Abstract
OBJECTIVE:
Evaluate the patterns of e-cigarette use and their association with smoking behavior.
MATERIALS AND METHODS:
We analyzed data from a population-based representative cohort of adult smokers who participated in the International Tobacco Control Policy Evaluation Surveys in Mexico. The analytic sample (n=760) was restricted to participants who were followed up from wave 6 (2012) to wave 7 (2014–2015). GEE models regressed e-cigarette use at follow-up and changes in cigarettes per day (CPD) between waves, on baseline sociodemographic variables, smoking status (daily, non-daily, quit), e-cigarette trial, and quit intentions.
RESULTS:
Smokers who were younger, had a higher income, and had tried e-cigarettes at baseline were more likely to be current e-cigarette users at follow-up. Ecigarette use at follow-up was not associated with a change in CPD over time.
CONCLUSIONS:
E-cigarette use does not appear to have promoted smoking cessation or reduction in this sample of Mexican smokers.
Keywords: Mexico, e-cigarettes, prospective study, smoking cessation
INTRODUCTION
E-cigarettes are battery operated devices which heat a solution that usually contains nicotine,1,2 and their use is taking off around the world.3–7 Some researchers have raised concerns that e-cigarette use may impede smoking cessation.8–12 However, most of the research on this topic has been conducted in high-income countries where e-cigarettes are legally available. In low- and middle-income countries, where cessation aids are not widely available and are rarely used, their impact may be especially important.13 This study aimed to understand the patterns of e-cigarette use among Mexican smokers, including the relationship between e-cigarette use and smoking behavior.
Studies on how e-cigarette use impacts smoking reduction and cessation have produced mixed results. Several longitudinal studies have found that e-cigarette use is associated with smoking reduction or cessation, 8–11 whereas other studies have detected no such association, 1,10,11,14 or have found that smokers who use e-cigarette are less likely to quit smoking than those who smoke cigarettes only.15–18 Indeed, according to a recent meta-analysis that included four longitudinal studies, the odds of quitting cigarettes was 28% lower among smokers who used e-cigarettes compared to those who were not using e-cigarettes.2 Still, other studies have found that the effectiveness of e-cigarette use for cessation depends on the type of e-cigarette device used and on the frequency of use.1,11,19 Nicotine delivery from cigarettes is more similar to that from e-cigarettes that have larger batteries and can be re-filled with fluids, compared to e-cigarette devices with smaller batteries that look like conventional cigarettes (i.e., with disposable, pre-filled cartridges).1, 20–22 E-cigarettes that better mimic nicotine delivery from combustible tobacco may have a greater potential for helping smokers quit combustible cigarettes.1
Study context
Since 2008, Mexico has prohibited the importation, distribution, advertising and sale of e-cigarettes.23 Nevertheless, there has been an increase in e-cigarette use over time. In 2012, 34% of Mexican adult smokers had heard of e-cigarettes, and 4% had tried them.24 By 2016, a national survey study found that 18% of adult smokers had tried e-cigarettes, and 5% were currently using them.25 In that survey, e-cigarette trial and current use were associated with being a current smoker, having a higher smoking frequency, being female, and having a higher socioeconomic status (i.e. income and education).1 However, to date there are no longitudinal studies of Mexican adults that have evaluated the predictors of e-cigarette use or its association with smoking reduction or cessation. In this study, we aim to evaluate the predictors of e-cigarette use in a population-based representative cohort of Mexican smokers. We will also evaluate the association between changes in the number of cigarettes smoked per day (from wave 6 to wave 7) and e-cigarette use at wave 7, as well as the relationship between planning to quit smoking at baseline and subsequent e-cigarette use. Since the relationship between e-cigarette use and smoking behaviors has been inconsistent in previous studies, we did not have an a priori hypothesized direction for this relationship.
MATERIALS AND METHODS
Design
We used data from waves 6 (2012) and 7 (2014–2015) of the International Tobacco Control Policy Evaluation Survey administered in Mexico (ITC-Mexico). ITCMexico is a population-based, representative cohort of adult smokers who reside in seven major Mexican cities (Mexico City, etc.) The initial data collection took place in 2006, using a stratified, multi-stage sampling scheme with face-to-face household interviews. At each wave, the sample is replenished in order to maintain sample size. A more detailed description of the sampling methodology can be found elsewhere.26–28 At entry into the cohort, eligible participants were aged 18 or more years, had smoked at least once during the previous week, and had smoked at least 100 cigarettes in their lifetime. Those who quit smoking over the study period were still surveyed and followed up. The data for wave 6 were collected between October and December, 2012, (N=2 129 participants) in seven Mexican cities. The data for wave 7 were collected between November 2014 and March, 2015, although only participants in 3 cities (Monterrey, Guadalajara and Mexico City; N=944 participants) were surveyed, due to resource constraints. The study protocol was approved by the IRB at the Mexican National Institute of Public Health.
Sample
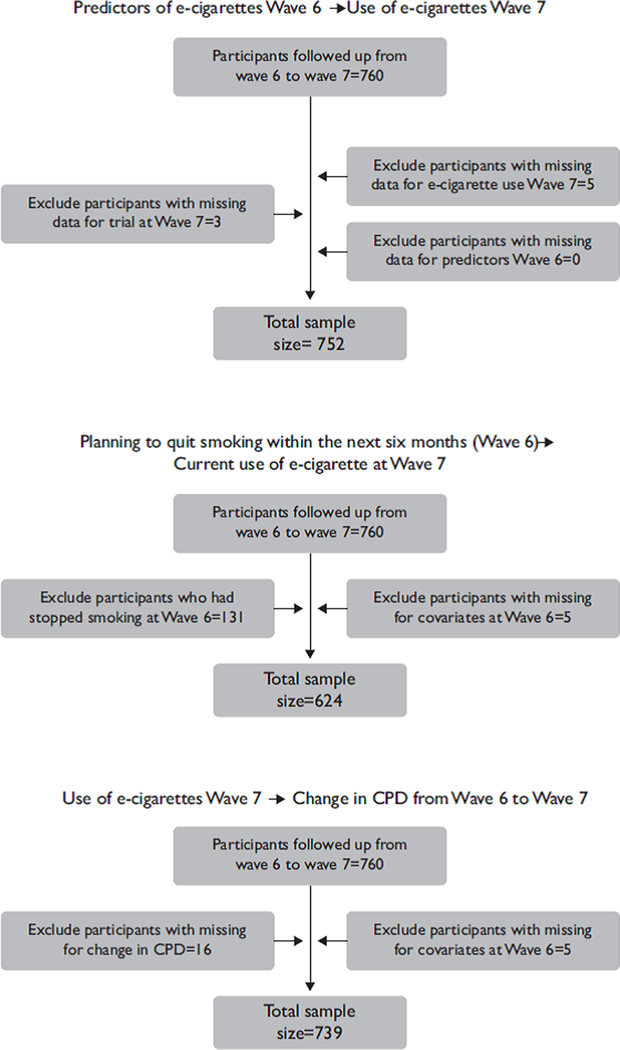
The analytic sample was restricted to wave six participants (N=992) from the three largest cities in Mexico (Monterrey, Guadalajara and Mexico City) who were followed up from wave 6 to wave 7 (N=760 participants). 23% of a total of 992 eligible participants from wave 6 (n=232) were excluded and were not followed up. After excluding those participants who had missing values for the exposure, outcome and covariates, the final study sample size for the analytic sample of predictors of e-cigarette use was 752 participants. The analytic sample for assessing the relationship between e-cigarette use at wave 7 and a change in the number of cigarettes smoked per day from wave 6 to wave 7 included 739 participants. The analytic sample for evaluating the association between planning to quit smoking at wave 6 and e-cigarette use at wave 7 (n=624) eliminated those who were not smoking at wave 6 because they were not asked questions about quit intentions (see figure 1 for determination of analytic samples).
Figure 1.
Sample flow chart (Mexico, 2012–2015)
Measures
E-cigarette variables.
After describing e-cigarettes to participants, e-cigarette trial was assessed by asking participants: “Have you ever tried an electronic cigarette?” (Yes/No). Current e-cigarette use was measured by asking participants who had ever tried e-cigarettes: “In the last six months, how often did you use an e-cigarette?” (response options: “Daily”, “Not daily but at least once a week”, “1–3 times per month”, “A few times in the last six months”, “Did not use in the last six months”). Participants were classified as either using e-cigarettes at least once in the last month (daily, weekly, 1–3 times per month) or not (other responses). For some analyses, e-cigarette use in the last six months (vs. not) was also derived from this question. Participants who had used e-cigarettes at least one to three times per month were asked what type of e-cigarette they were currently using most often (response options: “A disposable (non-rechargeable) e-cigarette”, “An e-cigarette kit that looks like a cigarette”, “An e-cigarette kit with cartridges that does not look like an e-cigarette”, “Don’t know”).
Smoking-related variables
In order to examine smoking reduction we estimated the change in cigarettes per day (CPD) between wave 6 and wave 7. This variable was created by subtracting the CPD in wave 6 from the CPD in wave 7, assigning a value of 0 to those who had quit smoking at either wave. Therefore, negative values represented a reduction in CPD from wave 6 to wave 7, a positive value represented an increase in CPD, and a zero value represented no change over time. Planning to quit smoking within the next six months was measured by asking participants who smoked if they planned to quit “Within the next month”, “Within the next six months”, “Sometime in the future, beyond six months”, or “not planning to quit”. This variable was dichotomized into “Yes” (Plan to quit within the next six months or before) and “No” (other responses).29
Covariates
Several individual-level sociodemographic variables were examined as covariates, including age (18–29, 30–39, 40–54, 55 or older), sex, education (dichotomized into individuals that had a middle-school education or less, and those with high school education or more), and monthly household income (low=$5 000 MP or less; middle=$5 001-$8 000 MP; high=$8 000 MP or more; “Don’t know”). The categories used to model income and education were chosen to be as close to uniform as possible across categories, while preventing zero counts that might hinder convergence for models where the prevalence of the outcome was low. Finally, the smoking status was categorized as daily smokers, non-daily smokers and quitters.
Analysis
We used chi-squares to compare participants who were lost to follow-up to those who were not. Weighted generalized estimating equations (GEE) models with robust standard errors were used to account for the nested structure of the data due to the cluster sampling approach. All models were weighted to account for sample size at the city level in order to prevent the observations for the largest city (Mexico City) from overrepresenting those for the smaller cities (Monterrey and Guadalajara). The models estimated the associations between sociodemographic and tobacco-use variables at baseline and e-cigarette use at follow-up (last six month use); the association between e-cigarette use at follow-up and change in CPD over time (adjusting for covariates), and the association between planning to quit smoking at baseline and e-cigarette use at follow-up. All analyses were conducted using Stata 14.
RESULTS
Unweighted sample characteristics from wave 6 are presented on table I, including a comparison of participants who were followed-up from wave 6 to wave 7 with those who were not. More than half of the study participants who were followed-up were male and aged over 40 years. Moreover, 65% of respondents had a middle school education or less, and half of the participants had a low income. Approximately 61% of participants were daily smokers, and 22% were non-daily smokers. Daily smokers smoked an average of eight CPD, while non-daily smokers smoked an average of one CPD. Over 90% of the participants had not tried e-cigarettes, and only 12 participants reported using e-cigarettes at least once a month. Among past month e-cigarette users, one used a disposable (non-rechargeable) e-cigarette, four used an e-cigarette kit that looks like a cigarette, six used e-cigarettes with pre-filled cartridges (that did not look like a cigarette), and one respondent answered “Don’t know” (data not shown). Differences in sociodemographic characteristics between participants who were followed-up and those who were not followed-up were mostly not statistically significant; however, participants who were not followed-up were younger and had higher levels of education.
Table I.
Selected baseline characteristics of the Mexican smokers follow-up sample (México, 2012)
| Smokers followed-up (N=760) |
Smokers not followed- up (N=232) |
||
|---|---|---|---|
| Baseline variables | % (n) | % (n) | p-value* |
| Sex | |||
| Female | 46 (351) | 39 (92) | 0.08 |
| Male | 54 (409 | 61 (142) | |
| Age | |||
| 18–29 | 12 (88) | 17 (40) | 0.005 |
| 30–39 | 34 (255) | 41 (97) | |
| 40–54 | 32 (241) | 24 (56) | |
| 55+ | 23 (176) | 18 (41) | |
| Education | |||
| Middle school or less | 65 (496) | 47 (111) | <0.001 |
| High school or more | 35 (264) | 52 (121) | |
| Income | |||
| Low | 50 (383) | 47 (110) | 0.11 |
| Middle | 22 (169) | 23 (54) | |
| High | 15 (111) | 21 (49) | |
| Unknown | 13 (97) | 9 (21) | |
| Smoking status | |||
| Daily | 61 (464) | 62 (146) | 0.869 |
| Non-daily | 22 (164) | 21 (49) | |
| Quitters | 17 (132) | 17 (39) | |
| E-cigarettes trial | |||
| Yes | 6 (45) | 10 (23) | 0.091 |
| No | 94 (715) | 90 (210) | |
Chi-square test
E-cigarette use at follow-up
Participants with a high household income at baseline where morel likely to have used e-cigarettes in the last six months at follow-up, compared to participants with a low income (9 vs. 6% respectively; AOR=7.05, 95%IC 1.52–32.73; table II). Moreover, participants who had tried e-cigarettes at baseline were more likely to report using e-cigarettes in the last six months (20.45 vs. 3.25% respectively; AOR=7.22, 95%IC 2.26–22.51; table II) and in the last month (9.09 vs. 1.13% respectively; AOR=15.94, 95%IC 2.93–86.80; table II) at follow-up. Participants who were between 18–29 years old were more likely to have used e-cigarettes in the past month, compared to those who were 55 or older (5.85 vs. 0.6% respectively; AOR=10.28, 95%IC 1.14–92.44; table II).
Table II.
Weighted association between socio-demographic variables at baseline and use of e-cigarettes at follow-up (México, 2012–2015)
| E-cigarettes used in the last six months (N=752) | E-cigarettes used in the last month (N=752) | |||||
|---|---|---|---|---|---|---|
| Baseline Variables | % | OR CI 95% | AOR CI 95% | % | OR CI 95% | AOR CI 95% |
| Sex | ||||||
| Female | 4.6 | 1.2 (0.44, 3.32) | 1.1 (0.35, 3.70) | 2.0 | 1.2 (0.33, 4.52) | 1.4 (0.47, 4.66) |
| Male | 3.9 | 1.00 | 1.00 | 1.2 | 1.00 | 1.00 |
| Age | ||||||
| 18–29 | 6.9 | 2.0 (0.29, 14.84) | 2.0 (0.28, 15.38) | 5.8 | 12.7 (1.41, 114.47) | 10.2 (1.14, 92.44) |
| 30–39 | 5.2 | 2.5 (0.34, 18.61) | 2.1 (0.30, 15.84) | 0.8 | 1.8 (0.15, 22.42) | 1.4 (0.10, 23.05) |
| 40–54 | 4.6 | 1.4 (0.18, 10.86) | 0.9 (0.12, 7.53) | 1.7 | 5.0 (0.52, 50.01) | 4.6 (0.46, 47.38) |
| 55 and more | 1.2 | 1.00 | 1.00 | 0.6 | 1.00 | 1.00 |
| Education | ||||||
| Middle school or less | 2.4 | 1.00 | 1.00 | 1.4 | 1.00 | 1.00 |
| High school or more | 7.7 | 3.4 (1.19, 10.08) | 1.6 (0.52, 5.20) | 1.9 | 0.8 (0.23, 2.80) | 0.3 (0.06, 1.71) |
| Income | ||||||
| Low | 1.6 | 1.00 | 1.00 | 1.1 | 1.00 | 1.00 |
| Middle | 6.0 | 6.6 (1.54, 28.85) | 6.2(1.22, 31.65) | 2.4 | 5.0 (1.09, 23.47) | 5.6 (1.00, 31.40) |
| High | 8.1 | 8.9 (2.11, 38.00) | 7.0 (1.52, 32.73) | 0.9 | 1.6 (0.18, 15.19) | 1.9 (0.20, 19.11) |
| Unknown | 7.2 | 6.6 (1.50, 29.80) | 7.2 (1.63, 31.75) | 3.1 | 6.7 (1.38, 32.98) | 6.3 (1.06, 37.85) |
| Smoking status | ||||||
| Daily | 4.2 | 1.00 | 1.00 | 1.7 | 1.00 | 1.00 |
| Non-daily | 6.2 | 1.2 (0.39, 3.83) | 1.3 (0.40, 4.39) | 2.2 | 0.7 (0.20, 2.92) | 0.7 (0.18, 3.26) |
| Quitters | 2.4 | 0.8 (0.17, 4.54) | 1.3 (0.26, 6.75) | 0.6 | 0.2 (0.02, 1.73) | 1.3 (0.25, 7.00) |
| E-cigarette trial | ||||||
| No | 3.3 | 1.00 | 1.00 | 1.1 | 1.00 | 1.00 |
| Yes | 20.5 | 7.2 (2.36,22.51) | 7.2 (2.26, 23.04) | 9.1 | 10.4 (2.66, 40.83) | 15.9 (2.93, 86.80) |
In models with the analytic sample of participants who smoked at baseline, those who planned to quit smoking were not more likely to be using e-cigarettes in the month previous to the follow-up wave (1.9 vs. 1.6% respectively; AOR=1.30, 95% IC 0.23–7.41; table III).
Table III.
Weighted association between intention to quit at baseline and use of e-cigarettes at follow-up (México, 2012–2015)
| Use of e-cigarettes in the last months (N=624) | ||||
|---|---|---|---|---|
| N | % | OR CI 95% | AOR CI 95% | |
| Plan to quit smoking in the next six months | ||||
| Yes | 2 | 1.87 | 1.06 (0.2–5.64) | 1.3 (0.23–7.41) |
| No/Don’t know | 8 | 1.55 | 1.00 | 1.00 |
| Sex | ||||
| Female | 5 | 1.77 | 0.75 (0.21–2.73) | |
| Male | 5 | 1.46 | 1.00 | |
| Age | ||||
| 18–29 | 5 | 3.55 | 7.83 (0.81–75.55) | |
| 30–39 | 1 | 0.67 | 0.98 (0.05–16.45) | |
| 40–50 | 3 | 2.01 | 6.32 (0.5–79.33) | |
| 55+ | 1 | 0.54 | 1.00 | |
| Education | ||||
| Middle school or less | 6 | 1.46 | 1.00 | |
| High school or more | 4 | 1.87 | 0.29 (0.06–1.36) | |
| Income | ||||
| Low | 1 | 0.83 | 1.00 | |
| Middle | 2 | 1.09 | 1.88 (0.13–27.27) | |
| High | 4 | 1.7 | 6.95 (0.61–78.62) | |
| unknown | 3 | 3.53 | 12.41 (0.99–155.57) | |
| Ever used e-cigarettes at baseline | ||||
| yes | 3 | 7.14 | 9.24 (2.02–42.2) | |
| No | 7 | 1.20 | 1.00 | |
Changes in smoking frequency
Participants who had used e-cigarettes in the past month at follow-up were not more likely to have either reduced or increased the number of cigarettes smoked per day since the previous wave (βadjusted =−0.58, 95%IC −3.25–2.10; table IV).
Table IV.
Weighted association between use of e-cigarettes and change in cigarette in one unit of cigarette per day (México, 2012–2015)
| Change in smoking
consumption (N=739) |
||
|---|---|---|
| β CI 95% | βadjusted CI 95% | |
| Use of e-cigarettes in the last month | ||
| Yes | −0.42 (−3.06, 2.23) | −0.58 (−3.25, 2.10) |
| No | ref | ref |
| Sex | ||
| Female | 0.15 (−0.69, 0.99) | |
| Male | ref | |
| Age | ||
| 18–29 | 1.32 (−0.32, 2.95) | |
| 30–39 | 0.32 (−1.07, 1.71) | |
| 40–50 | 0.35 (−0.91,1.62) | |
| 55 o more | ref | |
| Education | ||
| Middle school or less | ref | |
| High school or more | −0.28 (−1.24, 0.67) | |
| Income | ||
| Low | ref | |
| Middle | −0.12 (−1.30, 1.06) | |
| High | −0.62 (−1.67, 0.43) | |
| Unknown | −1.24 (−3.25, 0.78) | |
| Smoking status | ||
| Everyday | ref | |
| Non-daily | 1.34 (0.27, 2.40) | |
| Quitters* | 1.94 (1.21, 2.66) | |
Quitters where represented as zero cigarette per day. Negative values for change in smoking cessation represent a reduction in e-cigarette use from wave 6 to Wave 7.
DISCUSSION
Our study suggests that Mexican smokers who were younger and had a higher income at baseline were more likely to be current e-cigarette users at follow-up, which is consistent with a 2016 cross-sectional survey conducted in Mexico.25 Our study also found that trial of e-cigarette use at baseline was the strongest predictor of current e-cigarette use at follow-up, suggesting that those who were most interested in trying this innovative nicotine delivery device, even if it was illegal, were more likely to continue using it. Those who were e-cigarette users at follow-up were no more likely to increase or decrease CPD over time than those who did not currently use e-cigarettes at follow-up; these results are consistent with those of certain previous studies.1,10,11,14 However, other studies that have found that e-cigarette use is associated with CPD reduction and smoking cessation.8–11 A longitudinal study in Great Britain found that smokers who were daily e-cigarette users were more likely to achieve a 50% reduction in CPD, compared to smokers who did not use e-cigarettes.9 However, the same study found no significant CPD reduction among less frequent e-cigarette users compared to never e-cigarette.9 Due to the small number of daily e-cigarette users in our sample, we were unable to examine changes in CPD as a function of e-cigarette use intensity. As in other studies, it is possible that Mexican smokers use e-cigarettes in conjunction with conventional cigarettes rather than as an aid to quit smoking.30–32 Moreover, other observational studies suggest that the extent of CPD reduction among e-cigarette users is comparable to that among smokers who use nicotine replacement therapy (NRT).9,33 In this study, we were unable to evaluate associations between NRT use and changes in CPD, as NRT is not widely available, and its use is very low among smokers and recent quitters in Mexico (3.5% of 14.3 million in 2015).34
At baseline, our assessment of e-cigarette use behavior was limited to trial only. When we asked more detailed questions at follow-up, only a small percentage of our sample reported using e-cigarettes at least once in the last month (n=12), half of whom used e-cigarettes with pre-filled cartridges. This small sample size did not permit evaluation of the frequency of use or type of e-cigarette used, which previous studies suggest are critical considerations when assessing the impact of e-cigarettes on smoking reduction and cessation.1,20–22 Larger sample sizes that consider e-cigarette devices used and nicotine content will be necessary to determine whether e-cigarettes can effectively promote cessation among smokers who use the devices as an aid for quitting.1
Smokers who planned to quit smoking at baseline were not more likely to become current e-cigarette users at follow-up; hence, e-cigarette use may not be perceived as a viable smoking cessation aid within the context of Mexico. This result is consistent with a previous longitudinal study in the US.35 Mexicans may mainly experiment with e-cigarettes, substituting them for cigarettes in contexts where smoking is not allowed or is socially unacceptable. This orientation may change if e-cigarettes become legal, more widely available, and are accompanied by marketing and communication campaigns that encourage their use for harm reduction.
Limitations
This study has several limitations. For instance, our relatively small sample size and associated statistical power may account for the null results around e-cigarette use and CPD reduction, and for the low precision of estimates (e.g. large confidence intervals). However, some previous studies that have found positive and significant associations between e-cigarette use and smoking reduction and cessation have utilized smaller sample sizes (n=367, n=477).8 Moreover, in this study we were unable to systematically evaluate e-cigarette related factors (e.g. type of e-cigarette used, nicotine content, frequency of e-cigarette use) that appear to be important when accounting for smoking cessation and reduction. Although the follow-up survey assessed e-cigarette frequency, we were unable to analyze this variable in any detail due to a small sample size for daily and weekly e-cigarette users. The insufficient sample size also meant that we were unable to examine smoking cessation outcomes (quit attempts, successful quitting). To better assess these outcomes, future studies should consider using different sampling methods (e.g. oversampling e-cigarette users) or more controlled study designs (i.e. randomized clinical trials). Furthermore, the two year period between survey waves may have missed some important e-cigarette use and may be too long to examine its effectiveness for smoking cessation. Results from this study may not be generalizable to the Mexican population, as data were only collected from three cities (i.e. Mexico City, Guadalajara and Monterrey). Nonetheless, these cities are the largest in Mexico and represent a significant proportion of the population. Finally, differential follow-up may have introduced selection bias into the study, as participants who were lost to follow-up were younger and had higher education than those who were successfully followed up. However, this does not appear to be great cause of concern, given that we found no other significant differences between the analytic sample and those lost to follow-up, and our analyses adjusted for age, education and other key variables that might bias results.
Conclusions
This is the first longitudinal study in Latin America to evaluate e-cigarette use and its association with smoking reduction and cessation intentions; in it, we found no evidence that e-cigarette use promotes cessation or harm reduction among Mexican smokers. Despite banning the importation, distribution, marketing and sale of e-cigarettes, there are currently no restrictions regarding the use of e-cigarettes in smoke-free places,25 and e-cigarettes appear to be widely available to both adults and adolescents.36 Indeed, e-cigarettes can be easily acquired at supermarkets, which suggests a poor enforcement of the ban.4 Moreover, as the e-cigarette market is rapidly evolving, data from this study (2015) may not adequately represent current patterns of e-cigarette use among Mexican adults who smoke. Likewise, future legalization of e-cigarette products may change e-cigarette consumption patterns, including their relationship with smoking cessation. Even if e-cigarettes may help smokers quit smoking, they may also promote the use of nicotine products among Mexican adolescents, among whom those at a relatively low risk appear interested in trying e-cigarettes36,37 and are likely to progress to conventional smoking after e-cigarette trial,38 as found in US studies.39 Thus, policy makers need to carefully consider both the potential benefits and the potential harm of e-cigarette use for public health. In the end, this study suggests that e-cigarettes may not promote smoking reduction or cessation, and that it may be important to improve the enforcement of bans on e-cigarette marketing and clarify that smoke-free bans also apply to e-cigarette use, as recommended by the WHO.40
Acknowledgments
FUNDING
This research was supported by a grant from the Fogarty International Center and the National Cancer Institute of the United States National Institutes of Health (R01 TW010652). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of conflict of interests. The authors declare that they have no conflict of interests.
REFERENCES
- 1.Hitchman SC, Brose LS, Brown J, Robson D, McNeill A. Associations between e-cigarette type, frequency of use, and quitting smoking: findings from a longitudinal online panel survey in Great Britain. Nicotine Tob Res. 2015;17(10):1187–94. 10.1093/ntr/ntv078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–28. 10.1016/S2213-2600(15)00521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, et al. Electronic cigarettes a policy statement from the American Heart Association. Circulation. 2014;130(16):1418–36. 10.1161/CIR.0000000000000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Research and Markets. Global E and T- Vapor Market, Analysis and Forecast (2017–2025) (Focus on Product Segments, Distribution Channels and Country Analysis) [cited March 16, 2019]. Available from: https://www.researchandmarkets.com/reports/4471809/global-e-cigarette-and-t-vapormarket-analysis#pos-1
- 5.Sommer I, Griebler U, Mahlknecht P, Thaler K, Bouskill K, Gartlehner G, Mendis S. Socioeconomic inequalities in non-communicable diseases and their risk factors: an overview of systematic reviews. BMC Public Health.2015;15(1):914 10.1186/s12889-015-2227-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Headley D Hyperactivity in e-cigarettes but are we heading east … or west? 2014. June 26 In: Euromonitor Blog [internet] c2018 [about 5 screens]. Available from: http://blog.euromonitor.com/2014/06/hyperactivity-in-e-cigarettes-but-are-we-heading-eastor-west.html [Google Scholar]
- 7.Evans P E-Cigarette Makers Face Rise of Counterfeits. The Wall Street Journal. 2015. February 20 Available from: http://www.wsj.com/articles/ecigarette-makers-face-rise-of-counterfeits-1424441348 [Google Scholar]
- 8.Etter JF, Bullen C. A longitudinal study of electronic cigarette users. Addict Behav. 2014;39(2):491–4. 10.1016/j.addbeh.2013.10.028 [DOI] [PubMed] [Google Scholar]
- 9.Brose LS, Hitchman SC, Brown J, West R, McNeill A. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110(7):1160–8. 10.1111/add.12917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adkison SE, O’Connor RJ, Bansal-Travers M, Hyland A, Borland R, Yong HH, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. Am J Prev Med. 2013;44(3):207–15. 10.1016/j.amepre.2012.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berry KM, Reynolds LM, Collins JM, Siegel MB, Fetterman JL, Hamburg NM, et al. E-cigarette initiation and associated changes in smoking cessation and reduction: the Population Assessment of Tobacco and Health Study, 2013–2015. Tob Control 2018. 10.1136/tobaccocontrol-2017-054108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samet JM. A global health perspective on the future of tobacco control. Salud Publica Mex. 2012;54:264–69. 10.1590/S0036-36342012000300008 [DOI] [PubMed] [Google Scholar]
- 13.Blanco A, Sandoval RC, Martínez-López L, Caixeta R. Diez años del Convenio Marco de la OMS para el Control del Tabaco: avances en las Américas. Salud Publica Mex. 2017;59:117–25. 10.21149/8682 [DOI] [PubMed] [Google Scholar]
- 14.Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Intern Med. 2014;174(5):812–3. 10.1001/jamainternmed.2014.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vickerman KA, Carpenter KM, Altman T, Nash CM, Zbikowski SM. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15(10):1787–91. 10.1093/ntr/ntt061 [DOI] [PubMed] [Google Scholar]
- 16.Borderud SP, Li Y, Burkhalter JE, Sheffer CE, Ostroff JS. Electronic cigarette use among patients with cancer: characteristics of electronic cigarette users and their smoking cessation outcomes. Cancer. 2014;120(22):3527–35. 10.1002/cncr.28811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Delaimy WK, Myers MG, Leas EC, Strong DR, Hofstetter CR. Ecigarette use in the past and quitting behavior in the future: a population-based study. Am J Public Health. 2015;105(6):1213–9. 10.2105/AJPH.2014.302482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sutfin EL, Reboussin BA, Debinski B, Wagoner KG, John Spangler J, Wolfson M. The impact of trying electronic cigarettes on cigarette smoking by college students: a prospective analysis. Am J Public Health. 2015;105(8):e83–e89. 10.2105/AJPH.2015.302707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine Tob Res. 2014;17(2):127–33. 10.1093/ntr/ntu200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farsalinos KE, Spyrou A, Tsimopoulou K, Stefopoulos C, Romagna G, Voudris V. Nicotine absorption from electronic cigarette use: comparison between first and new-generation devices. Sci Rep. 2014;4:4133 10.1038/srep04133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. Washington, DC: The National Academies Press, 2018. 10.17226/24952 [DOI] [PubMed] [Google Scholar]
- 22.Lopez AA, Hiler MM, Soule EK, Ramôa CP, Karaoghlanian NV, Lipato T, et al. Effects of electronic cigarette liquid nicotine concentration on plasma nicotine and puff topography in tobacco cigarette smokers: a preliminary report. Nicotine Tob Res. 2015;18(5):720–3. 10.1093/ntr/ntv182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Congreso General de los Estados Unidos Mexicanos. Ley General para el Control del Tabaco. México, 2007. Salud Publica Mex; 2008;50(suppl 3):s405–13. [PubMed] [Google Scholar]
- 24.Gravely S, Fong GT, Cummings KM, Yan M, Quah A, Borland R, et al. Awareness, trial, and current use of electronic cigarettes in 10 countries: Findings from the ITC project. Int J Environ Res Public Health. 2014;11(11):11691–704. 10.3390/ijerph111111691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zavala-Arciniega L, Reynales-Shigematsu LM, Lozano P, Rodríguez-Andrade MÁ, Arillo-Santillán E, Thrasher JF. Patterns of awareness and use of electronic cigarettes in Mexico, a middle-income country that bans them: Results from a 2016 national survey. Prev Med. 2018;116:211–8. 10.1016/j.ypmed.2018.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fleischer NL, Thrasher JF, de Miera-Juárez BS, Reynales-Shigematsu LM, Arillo-Santillán E, Osman A, et al. Neighbourhood deprivation and smoking and quit behaviour among smokers in Mexico: findings from the ITC Mexico Survey. Tob Control. 2015;24(suppl 3):iii56–63. 10.1136/tobaccocontrol-2013-051495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lozano P, Thrasher JF, Forthofer M, Hardin J, Reynales-Shigematsu LM, Arillo-Santillán E, Fleischer NL. The role of social norms and socioeconomic status in smoking-related stigma among smokers in Mexico and Uruguay. Critical Public Health. 2018:1–13. 10.1080/09581596.2018.1440070 [DOI] [Google Scholar]
- 28.Thrasher J, Pérez-Hernández R, Arillo-Santillán E, Barrientos-Gutiérrez I. Hacia el consumo informado de tabaco en México: Efecto de las advertencias en población fumadora. Salud Publica Mex. 2012;54(3):242–53. [PMC free article] [PubMed] [Google Scholar]
- 29.Stewart B, Wild CP. World cancer report 2014. Geneva: World Health Organization/International Agency for Research on Cancer, 2015. [Google Scholar]
- 30.Zhu SH, Gamst A, Lee M, Cummins S, Yin L, Zoref L. The use and perception of electronic cigarettes and snus among the US population. PLoS One. 2013;8(10):e79332. 10.1371/journal.pone.0079332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Furlow B US government warns against long-term dual use of conventional and e-cigarettes. Lancet Respir Med. 2015;3(5):345 10.1016/S2213-2600(15)00138-1 [DOI] [PubMed] [Google Scholar]
- 32.Rutten LJF, Blake KD, Agunwamba AA, Grana RA, Wilson PM, Ebbert JO, et al. Use of e-cigarettes among current smokers: associations among reasons for use, quit intentions, and current tobacco use. Nicotine Tob Res. 2015;17(10):1228–34. 10.1093/ntr/ntv003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beard E, McNeill A, Aveyard P, Fidler J, Michie S, West R. Association between use of nicotine replacement therapy for harm reduction and smoking cessation: a prospective study of English smokers. Tob Control. 2013;22(2):118–22. 10.1136/tobaccocontrol-2011-050007 [DOI] [PubMed] [Google Scholar]
- 34.Pan American Health Organization, Instituto Nacional de Salud Pública. Global Adult Tobacco Survey. Mexico 2015. Cuernavaca, Mexico: INPS/PAHO, 2017. [Google Scholar]
- 35.Regan AK, Promoff G, Dube SR, Arrazola R. Electronic nicotine delivery systems: adult use and awareness of the ‘e-cigarette’in the USA. Tob Control. 2013;22(1):19–23. [DOI] [PubMed] [Google Scholar]
- 36.Thrasher JF, Abad-Vivero EN, Barrientos-Gutíerrez I, Pérez-Hernández R, Reynales-Shigematsu LM, Mejía R, et al. Prevalence and correlates of e-cigarette perceptions and trial among early adolescents in Mexico. J Adolesc Health. 2016;58(3):358–65. 10.1016/j.jadohealth.2015.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morello P, Pérez A, Braun SN, Thrasher JF, Barrientos I, Arillo-Santillán E, Mejía R. Smoking susceptibility as a predictive measure of cigarette and e-cigarette use among early adolescents. Salud Publica Mex. 2018;60(4):423–31. 10.21149/9193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lozano P, Barrientos-Gutierrez I, Arillo-Santillan E, Morello P, Mejia R, Sargent JD, Thrasher JF. A longitudinal study of electronic cigarette use and onset of conventional cigarette smoking and marijuana use among Mexican adolescents. Drug Alcohol Depend. 2017;180:427–30. 10.1016/j.drugalcdep.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: A systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–97. 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization Electronic nicotine delivery systems and electronic non-nicotine delivery systems (ENDS/ENNDS). Delhi: WHO, 2016. [Google Scholar]