Abstract
Background
To compare the dosimetric characteristics between volumetric modulated arc therapy (VMAT) and 9-field intensity-modulated radiation therapy (9F-IMRT) for cervical cancer patients with para-aortic lymph node (PALN) metastasis.
Methods
We selected 20 patients who had received extended-field radiotherapy for cervical cancer with PALN metastasis. IMRT and VMAT plans were compared in terms of target, organs at risk (OARs), homogeneity index (HI), conformity index (CI), the number of monitor units (MUs) and treatment time (s).
Results
The CI and HI of VMAT plans were superior to those of IMRT plans (P<0.05). As for OARs, the mean maximum doses (Dmean) to the kidneys in the VMAT plans were all lower than those in IMRT plans (P<0.001). V40, V50 of the rectum, and V40 of the bladder in VMAT plans involved fewer doses than IMRT plans (P<0.001). Compared with IMRT plans, VMAT reduced the average number of MUs by 51% and the average treatment time by 31%.
Conclusions
Both VMAT and IMRT plans can satisfy clinical dosimetric demands and protect OARs. VMAT has the best performance on CI and HI and can better protect the OARs. VMAT plans have fewer MUs and improve treatment efficiency.
Keywords: Cervical cancer, para-aortic lymph node metastasis (PALN metastasis), radiotherapy, intensity-modulated radiation therapy (IMRT), volumetric modulated arc therapy (VMAT)
Introduction
Cervical cancer, which is a serious threat to women’s life and health, is a common gynecological malignant cancer and currently ranks second in female cancer mortality rates. In addition, approximately 85% of cases occur in developing countries (1). Lymph node metastasis is the main pathway of cervical cancer metastasis. It generally proceeds from the primary tumor through the nearby lymphatic vessels and onwards to the uterus, obturator, and iliac and external iliac lymph nodes, finally metastasizing in the abdominal aortic lymph node (2). A study of the American Gynecologic Oncology Group (GOG) showed that 5% of the patients with stage Ib cervical cancer, 16% with stage II, and 25% with stage III had para-aortic lymph node (PALN) metastasis (3). PALN metastasis is one of the main prognostic factors for cervical cancer, and the PALN metastatic rate increases with the progression of disease stage (4). For the cervical cancer patients with PALN metastasis, extended-field radiotherapy should be considered (5). It is important for cervical cancer patients with PALN metastasis to choose an appropriate treatment plan.
Formerly, 3-dimensional conformal radiation therapy (3D-CRT) was the standard treatment for cervical cancer; however, this technique did not appreciably reduce radiation exposure to organs at risk (OARs) (6). The development of technology has led to the establishment of intensity-modulated radiation therapy IMRT (7), which can increase the gain ratio of radiotherapy and better protect the OARs (8-10). However, the treatment delivery time for IMRT is prolonged (9,10). Volumetric modulated arc therapy (VMAT) is a newer intensity-modulated arc therapy technique (11) that has been investigated in a variety of malignant tumors (12-14). Several studies on advanced cervical cancer have demonstrated reduced OAR doses with IMRT compared to 3D-CRT (15-17). There are also many studies that have focused on dosimetric differences between IMRT and VMAT in cervical cancer (18,19), but there are no reports comparing IMRT and VMAT in cervical cancer patients with PALN metastasis.
Thus, the current study was designed to compare the dose difference between IMRT and VMAT in the target area and in terms of organ dose. Additionally, it was designed to explore the optimal radiotherapy regimen for patients with cervical cancer with PALN metastasis.
Methods
Patient selection
A total of 20 patients who had received extended-field radiotherapy using the 9F-IMRT plan for cervical cancer with PALN metastasis were retrospectively selected for this study. The diagnosis of PALN metastasis was confirmed by PET-CT, which showed a standardized uptake value (SUV) ≥2.5, or lymph node diameter ≥10 mm. Every patient received concurrent chemotherapy with paclitaxel 135 mg/m2 and cisplatin 50 mg/m2. Patients were 39–72 years old, with a median age of 50.5 years. According to FIGO staging, 11 cases were stage II b, 9 cases were stage III b, and the pathological types were all squamous cell carcinoma. The maximum diameter of the abdominal aortic lymph nodes was 11–34 mm, and the average diameter was 15 mm.
CT simulation
Before the CT positioning was performed, the patients were required to empty their bowels and fill their bladders. All patients underwent CT scans in the supine position with a slice thickness of 3 mm, which is from the upper edge of T12 to 5 cm below the lower edge of the obturator foramen. After the simulation, the CT images were transferred into the Pinnacle treatment planning system (V9.2).
Delineation of target volumes and OARs
The target volumes were delineated by the same experienced radiation oncologist and radiologist (20). According to Report 83 by the International Commission on Radiation Units and Measurements (ICRU) (21), the clinical target volume (CTV) of extended-field radiotherapy for cervical cancer patients with PALN metastasis included the cervical mass, parametrial tissue, upper vagina, and uterus, along with the pelvic and PALNs of each patient. The planning target volume (PTV) was generated by adding 0.7 cm margins from the CTV in all directions except in the anterior and posterior directions (22) (Figure 1). The OARs included the kidneys, rectum, bladder, small intestine, pelvis, and bilateral femoral head.
Figure 1.
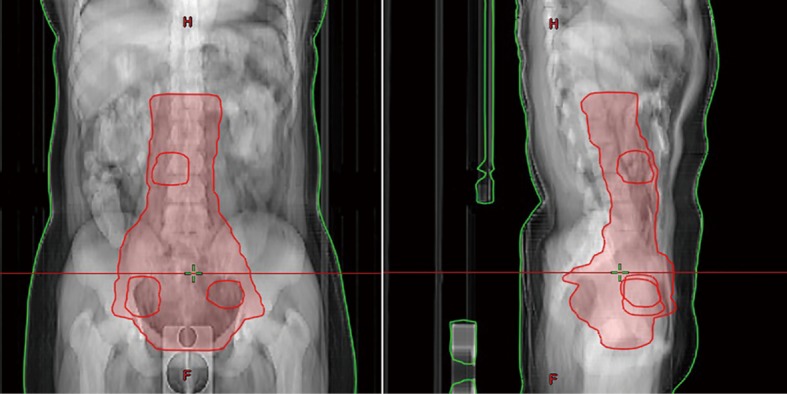
PTV of one cervical cancer patient with PALN metastasis. PTV, planning target volume; PALN, para-aortic lymph node.
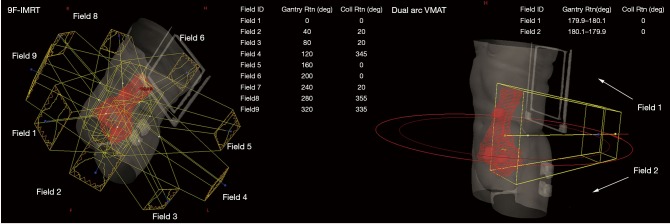
9F-IMRT planning for cervical cancer patients with PALN metastasis
9F-IMRT plans were designed with Elekta Medical Systems, with a 6-MV beam linear accelerator. A total of 9 fields were used to generate the plans. The gantry angles of each field were 40°, 80°, 120°, 160°, 200°, 240°, 280°, 320°, and 0° (Figure 2). The prescription doses were 50.4 Gy in 28 fractions (daily dose of 1.8 Gy). All 9F-IMRT plans were normalized to cover 95% of the PTV with 100% of the prescription dose. The mean dose (Dmean) to the kidneys was limited to <12 Gy. The V50 of the small bowel was limited to less than 10%. The V50 of the rectum was limited to less than 50%, the V50 of the bladder was limited to less than 30%, and the V50 of the femoral heads was limited to less than 5% (23,24).
Figure 2.
Beam-on fields of 9F-IMRT and beam-on fields of dual arc VMAT for one patient. 9F-IMRT, 9-field intensity-modulated radiation therapy; VMAT, volumetric modulated arc therapy.
VMAT planning for cervical cancer patients with PALN metastasis
The prescription dose for the VMAT plans was the same as the 9F-IMRT plans (50.4 Gy in 28 fractions). The VMAT plans were performed using two coplanar arcs (clockwise rotation from 181° to 179° and counterclockwise rotation from 179° to 181°) (Figure 2). The 6-MV photon beam of Elekta Medical Systems was used. The VMAT plans were optimized in the Pinnacle treatment system (V9.2) by following the RTOG 0724 protocol, the same as for the 9F-IMRT planning (22). After dose calculation, all VMAT plans were normalized to cover 95% of the target volume, with 100% of the prescription dose.
Plan evaluation
ICRU 83 states that the quality of the radiotherapy program should be assessed by the target index (conformity index, CI) and the homogeneity index (HI).
| [1] |
| [2] |
Description: TVRI is the target volume of the prescription dose line, TV is the target volume, VRI is the total volume of the prescription dose line, D2% represents the approximate maximum dose, D98% represents the approximate minimum dose, and D50% is the median dose. The CI value is between 0 and 1, and the larger CI values indicate a better dose of coverage in the target. Additionally, the lower the HI value is, the better the dose uniformity of the target (21).
Monitor unit (MU) and treatment time
Statistical analysis of MU was performed, and the treatment time of the two radiotherapy techniques was recorded (treatment time is the time taken for the first irradiation field to reach the end of treatment after completion of position and position verification).
Statistical analysis
SPSS 20.0 (IBM Corp, Armonk, NY, USA) statistical software was used to analyze the measurement data with ±s, between the two groups using the t-test. A P value <0.05 was considered a difference in statistical significance.
Results
Comparison of dose distribution
As shown in Figure 3, the dark yellow kidney volume was less than 1,200 cGy. Additionally, Figure 3 shows that the kidneys on the 9F-IMRT and dual arc VMAT plans are well protected, but the dual arc VMAT plans could achieve a better dose distribution of the target. At the same time, the bladder and rectum doses in the dual arc VMAT were typically less than 9F-IMRT. Therefore, the OARs and the PTV dose-volume histogram (DVH) of the dual arc VMAT plan was superior to the 9F-IMRT plan.
Figure 3.
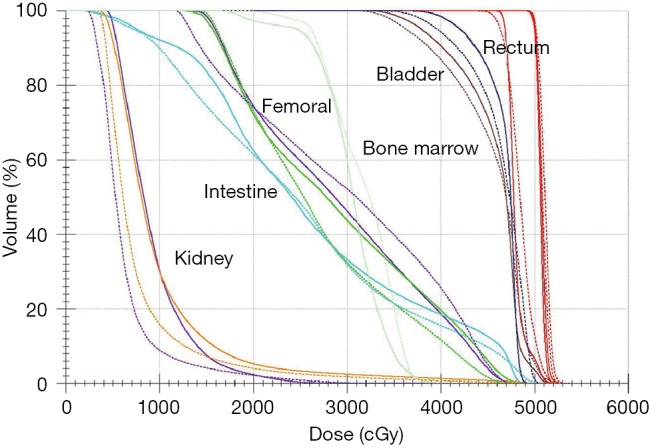
Comparison of DVH between dual arc VMAT and 9F-IMRT plans (the curve with represents the 9F-IMRT plan, and the curve with represents the dual arc VMAT plan). DVH, dose-volume histogram; 9F-IMRT, 9-field intensity-modulated radiation therapy; VMAT, volumetric modulated arc therapy.
Dosimetric comparison
Table 1 shows that the dose received by the target volume, D2% and D98% of the PTV in dual arc VMAT, was better than that in the 9F-IMRT plan, which was a statistically significant difference (P<0.01). The PTV volume receiving 95% and 105% of the prescription dose in dual arc VMAT was better than that in the 9F-IMRT plan, which was also a statistically significant difference (P<0.001). The CI for PTV was better in dual arc VMAT than in 9F-IMRT, while the HI for PTV in dual arc VMAT was lower than that in 9F-IMRT, which was a statistically significant difference (P<0.05).
Table 1. Dosimetric parameters comparison between 9F-IMRT and dual arc VMAT.
| Item | VMAT | IMRT | t | P |
|---|---|---|---|---|
| D2% (Gy) | 50.4±1.9 | 53.1±3.7 | 3.055 | 0.007 |
| D50% (Gy) | 47.2±0.8 | 46.9±0.9 | −0.943 | 0.358 |
| D98% (Gy) | 46.7±1.8 | 45.3±0.9 | −3.161 | 0.005 |
| V95% | 98.7±0.9 | 97.7±0.8 | −3.759 | 0.001 |
| V105% | 55.3±3.0 | 51.2±0.5 | −5.855 | <0.001 |
| HI | 0.08±0.03 | 0.10±0.03 | 2.262 | 0.036 |
| CI | 0.84±0.08 | 0.77±0.11 | −2.657 | 0.016 |
D2%, the approximate maximum dose; D50%, the median dose; D98%, the approximate minimum dose; V95%, volume receiving 95% of the prescription dose; V105%, volume receiving 105% of the prescription dose; HI, homogeneity index; CI, conformity index. IMRT, intensity modulated radiation therapy; VMAT, volumetric modulated arc therapy. When 9F-IMRT vs. VMAT, P<0.05.
Comparison of the irradiation dose of OARs
As for the OARs, the mean doses (Dmean) of the kidneys in the dual arc VMAT plans were all lower than those in the 9F-IMRT plans (P<0.001). The V40 and V50 of the rectum and V40 of the bladder in the dual arc VMAT plans carried fewer doses than IMRT (P<0.001). However, the V10, V20, and V30 of the rectum, V10, V20, V30, and V50 of the bladder,V10, V20, V30, V40, and V50 of the small intestine, and V10, V20, V30, V40, and V50 of the femoral heads all appeared the same as in the 9F-IMRT plans (P>0.05) (Table 2).
Table 2. Comparison of dose parameters for OARs between 9F-IMRT and dual arc VMAT.
| OAR | Dose of volume | VMAT | IMRT | t | P |
|---|---|---|---|---|---|
| Rectum | V10 Gy (%) | 98.2±1.3 | 97.9±1.2 | −0.943 | 0.358 |
| V20 Gy (%) | 97.5±0.7 | 97.7±0.4 | 0.887 | 0.386 | |
| V30 Gy (%) | 90.8±1.4 | 91.4±1.2 | 1.429 | 0.169 | |
| V40 Gy (%) | 48.6±3.7 | 60.8±4.4 | 12.087 | <0.001 | |
| V50 Gy (%) | 42.7±1.7 | 37.1±1.2 | 15.582 | <0.001 | |
| Bladder | V10 Gy (%) | 100±0.0 | 100±0.0 | 0.000 | 1.000 |
| V20 Gy (%) | 98.3±0.5 | 98.1±0.6 | −1.418 | 0.172 | |
| V30 Gy (%) | 76.7±2.9 | 76.3±2.8 | −0.568 | 0.577 | |
| V40 Gy (%) | 45.8±4.2 | 47.6±6.2 | 2.720 | 0.014 | |
| V50 Gy (%) | 25.7±2.2 | 25.4±2.5 | −0.419 | 0.680 | |
| Intestine | V10 Gy (%) | 81.8±1.1 | 81.1±1.6 | −1.530 | 0.143 |
| V20 Gy (%) | 55.5±2.2 | 57.7±5.9 | 1.721 | 0.101 | |
| V30 Gy (%) | 35.3±3.3 | 39.3±8.2 | 1.998 | 0.06 | |
| V40 Gy (%) | 23.7±3.5 | 25.9±7.1 | 1.676 | 0.110 | |
| V50 Gy (%) | 6.2±0.4 | 6.3±0.3 | 2.012 | 0.059 | |
| Femoral | V10 Gy (%) | 91.8±2.5 | 92.6±1.1 | 1.423 | 0.171 |
| V20 Gy (%) | 80.4±4.7 | 81.7±5.1 | 1.004 | 0.328 | |
| V30 Gy (%) | 49.2±4.6 | 48.7±4.5 | −0.626 | 0.539 | |
| V40 Gy (%) | 30.1±1.6 | 30.7±0.8 | 1.513 | 0.147 | |
| V50 Gy (%) | 3.4±0.6 | 3.2±0.5 | −1.674 | 0.111 | |
| Kidney-L | Mean (Gy) | 8.6±1.2 | 10.6±1.1 | 9.721 | <0.001 |
| Kidney-R | Mean (Gy) | 8.4±1.3 | 10.6±0.9 | 5.741 | <0.001 |
VxGy, volume receiving at least X Gy dose; IMRT, intensity modulated radiation therapy; VMAT, volumetric modulated arc therapy. When 9F-IMRT vs. VMAT, P<0.05.
Comparison of MUs and treatment time
To evaluate the performance of dual arc VMAT and 9F-IMRT plans, the MU and treatment time were compared between the two plans and listed in Table 3. For the 20 patients, compared with 9F-IMRT, the dual arc VMAT plans reduced the average number of MUs by 51% (812.5±218.1 vs. 1,670.7±182.2). Compared with 9F-IMRT, the dual arc VMAT plans reduced the mean delivery time by 31% (298.4±43.1 vs. 431.8±36.7 s). Therefore, the dual arc VMAT plans reduced MU and treatment time, which means it had better treatment efficiency.
Table 3. Comparison of MU and treatment time between 9F-IMRT and dual arc VMAT.
| Item | VMAT | IMRT | t | P |
|---|---|---|---|---|
| MUs | 812.5±218.1 | 1,670.7±182.2 | 16.628 | <0.001 |
| Time (s) | 298.4±43.1 | 431.8±36.7 | 12.664 | <0.001 |
IMRT, intensity modulated radiation therapy; VMAT, volumetric modulated arc therapy. When 9F-IMRT vs. VMAT, P<0.05.
Discussion
Radiotherapy for cervical cancer was initially 2-dimensional whole pelvic radiotherapy (WPRT), which is associated with severe short- and long-term side effects. In recent years, with the continued improvement of radiotherapy technology, 3-dimensional conformal radiotherapy (3D-CRT) and fixed-field intensity-modulated radiotherapy (IMRT) have been extensively applied in the treatment of cervical cancer (25,26). IMRT possesses obvious superiorities over 3D-CRT technology because the dose distribution is more reasonable. In addition, IMRT can reduce the number of organs and normal tissues at risk, including the kidneys, rectum, bladder, and small intestine. Consequently, it can alleviate adverse reactions, thus improving the radiotherapy efficacy for cervical cancer (18,27). However, IMRT technology is associated with certain drawbacks, mainly in its efficiency (28).
Research has been carried out concerning dosimetric differences in radiotherapy using VMAT or IMRT for treating cervical cancer. Huang et al. (29) evaluated the dose distribution between VMAT and 7F-IMRT in 13 cervical cancer patients and found that VMAT regimen showed marked advantages over 7-IMRT in terms of target region dose homogeneity and protection of endangered organs. Meanwhile, Nguyen et al. (30) also found that, compared with a conventional IMRT regimen, VMAT could achieve a highly conformal target region dose distribution and greater protection of normal tissues.
IMRT-dominated radiotherapy remains the major PALN radiotherapy for cervical cancer. Osborne et al. (31) reported that using extended-field radiation therapy for patients with cervical cancer with PALN metastasis improved patient’s condition in concurrence with advances in treatment. Portelance et al. (32) reported that, compared with 3D-CRT, IMRT reduces small bowel, rectum, and bladder doses in patients with cervical cancer receiving pelvic and para-aortic irradiation. However, there is no research or report that compares IMRT and VMAT treatment plans for cervical cancer patients with PALN metastasis.
This study compared the dosimetric difference and the dosimetric parameters in 20 cervical cancer patients with PALN metastasis between 9F-IMRT and VMAT plans. The results in the current study indicate that the target region doses in both regimens can satisfy the dosimetric requirement. In terms of the target homogeneity and CI, the VMAT plan was superior to the 9F-IMRT plan, and the calculated treatment time of the 9F-IMRT was longer than that of the VMAT plan (431.8±36.7 vs. 298.4±43.1 s). VMAT can reduce the patient’s discomfort caused by maintaining the same posture for a long time, reduce the errors caused by the body position during the treatment, and improve the accuracy of the treatment. The 9F-IMRT plans are delivered with the static IMRT technique, which needs more time to rotate the gantry and to move the MLCs between each beam-on (33). The 9F-IMRT plan has a disadvantage of relatively longer treatment times compared to VMAT; however, the expected real treatment time seems to be tolerable in the clinic.
Compared with the 9F-IMRT plan, the VMAT plan proved to be superior in the protection of OARs, because it reduced the irradiation dose they received. When a dose comparison of the kidneys was calculated, the observed mean dose for the kidneys in the VMAT plan was smaller than that in the 9F-IMRT plan, which could provide better protection for the kidneys. Meanwhile, V40 and V50 of the rectum and V40 of the bladder in the VMAT plans carried a smaller dose than that in the 9F-IMRT plan. VMAT was more conducive to the protection of normal tissues in the radiation field and in further reducing the adverse reactions patients experience during and after radiotherapy. In addition, the VMAT plan had lower MU than that of the 9F-IMRT plan, and the results are consistent with those in the international literature (34,35). Nevertheless, research results may be different in practical work, which can be attributed to the differences in planning systems such as single- or double-arc, radiation energy, optimization algorithm, and control of plan quality by operators. Therefore, a good VMAT plan needs to effectively control various influencing factors in the clinical environment and reduce unnecessary errors so as to obtain the optimization of the radiotherapy plan. For the same case, it requires a longer time to design a plan for VMAT in contrast with IMRT to meet the clinical requirements.
Conclusions
In summary, both plans could meet the requirements of OAR protection in cervical cancer patients with PALN metastasis. The VMAT plan is more ideal than 9F-IMRT plan in terms of target region conformity and can better protect OARs like the kidneys, rectum, and small intestine. In addition, VMAT contributes to reducing the exposure time and lowering the number of errors induced by position and organ movement during exposure. Therefore, the VMAT plan is a superior radiotherapy technique to 9F-IMRT plan in the radiotherapy treatment for cervical cancer patients with PALN metastasis.
Acknowledgments
Funding: The present work was supported by the Six Summit Investigator Grant of Jiangsu Province (2016-WSW-020) and National Natural Science Foundation of China (81802598 and 81872485).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study is a retrospective analysis, only analyzing the patient’s clinical data, not involving patient’s privacy and treatment, so there is no informed consent was signed.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Bray F, Ren JS, Masuyer E, et al. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer 2013;132:1133-45. 10.1002/ijc.27711 [DOI] [PubMed] [Google Scholar]
- 2.McMahon CJ, Rofsky NM, Pedrosa I. Lymphatic metastases from pelvic tumors: anatomic classification, characterization, and staging. Radiology 2010;254:31-46. 10.1148/radiol.2541090361 [DOI] [PubMed] [Google Scholar]
- 3.Whitney CW, Sause W, Bundy BN, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol 1999;17:1339-48. 10.1200/JCO.1999.17.5.1339 [DOI] [PubMed] [Google Scholar]
- 4.Song S, Kim JY, Kim YJ, et al. The size of the metastatic lymph node is an independent prognostic factor for the patients with cervical cancer treated by definitive radiotherapy. Radiother Oncol 2013;108:168-73. 10.1016/j.radonc.2013.04.015 [DOI] [PubMed] [Google Scholar]
- 5.Oh J, Seol KH, Lee HJ, et al. Prophylactic extended-field irradiation with concurrent chemotherapy for pelvic lymph node-positive cervical cancer. Radiat Oncol J 2017;35:349-58. 10.3857/roj.2017.00367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang B, Zhu L, Cheng H, et al. Dosimetric comparison of intensity modulated radiotherapy and three-dimensional conformal radiotherapy in patients with gynecologic malignancies: a systematic review and meta-analysis. Radiat Oncol 2012;7:197. 10.1186/1748-717X-7-197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bucci MK, Bevan A, Roach M, 3rd.Advances in radiation therapy: conventional to 3D, to IMRT, to 4D, and beyond. CA Cancer J Clin 2005;55:117-34. 10.3322/canjclin.55.2.117 [DOI] [PubMed] [Google Scholar]
- 8.Randall ME, Ibbott GS. Intensity-modulated radiation therapy for gynecologic cancers: pitfalls hazards, and cautions to be considered. Semin Radiat Oncol 2006;16:138-43. 10.1016/j.semradonc.2006.02.002 [DOI] [PubMed] [Google Scholar]
- 9.van Rij CM, Oughlane-Heemsbergen WD, Ackerstaff AH, et al. Parotid gland sparing IMRT for head and neck cancer improves xerostomia related quality of life. Radiat Oncol 2008;3:41. 10.1186/1748-717X-3-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korreman S, Rasch C, McNair H, et al. The European Society of Therapeutic Radiology and Oncology-European Institute of Radiotherapy (ESTRO-EIR) report on 3D CT-based in-room image guidance systems: a practical and technical review and guide. Radiother Oncol 2010;94:129-44. 10.1016/j.radonc.2010.01.004 [DOI] [PubMed] [Google Scholar]
- 11.Otto K.Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys 2008;35:310-7. 10.1118/1.2818738 [DOI] [PubMed] [Google Scholar]
- 12.Teoh M, Clark CH, Wood K, et al. Volumetric modulated arc therapy: a review of current literature and clinical use in practice. Br J Radiol 2011;84:967-96. 10.1259/bjr/22373346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yin L, Wu H, Gong J, et al. Volumetric-modulated arc therapy vs. c-IMRT in esophageal cancer: a treatment planning comparison. World J Gastroenterol 2012;18:5266-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quan EM, Li X, Li Y, et al. A comprehensive comparison of IMRT and VMAT plan quality for prostate cancer treatment. Int J Radiat Oncol Biol Phys 2012;83:1169-78. 10.1016/j.ijrobp.2011.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahamad A, D'Souza W, Salehpour M, et al. Intensity-modulated radiation therapy after hysterectomy: comparison with conventional treatment and sensitivity of the normal-tissue-sparing effect to margin size. Int J Radiat Oncol Biol Phys 2005;62:1117-24. 10.1016/j.ijrobp.2004.12.029 [DOI] [PubMed] [Google Scholar]
- 16.Heron DE, Gerszten K, Selvaraj RN, et al. Conventional 3D conformal versus intensity-modulated radiotherapy for the adjuvant treatment of gynecologic malignancies: a comparative dosimetric study of dose-volume histograms. Gynecol Oncol 2003;91:39-45. 10.1016/S0090-8258(03)00461-X [DOI] [PubMed] [Google Scholar]
- 17.van de Bunt L, van der Heide UA, Ketelaars M, et al. Conventional, conformal, and intensity-modulated radiation therapy treatment planning of external beam radiotherapy for cervical cancer: The impact of tumor regression. Int J Radiat Oncol Biol Phys 2006;64:189-96. 10.1016/j.ijrobp.2005.04.025 [DOI] [PubMed] [Google Scholar]
- 18.Cozzi L, Dinshaw KA, Shrivastava SK, et al. A treatment planning study comparing volumetric arc modulation with RapidArc and fixed field IMRT for cervix uteri radiotherapy. Radiother Oncol 2008;89:180-91. 10.1016/j.radonc.2008.06.013 [DOI] [PubMed] [Google Scholar]
- 19.Park JM, Park SY, Kim JI, et al. A comparison of treatment plan quality between Tri-Co-60 intensity modulated radiation therapy and volumetric modulated arc therapy for cervical cancer. Phys Med 2017;40:11-6. 10.1016/j.ejmp.2017.06.018 [DOI] [PubMed] [Google Scholar]
- 20.Taylor A, Rockall AG, Reznek RH, et al. Mapping pelvic lymph nodes: guidelines for delineation in intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 2005;63:1604-12. 10.1016/j.ijrobp.2005.05.062 [DOI] [PubMed] [Google Scholar]
- 21.Duthoy W, De Gersem W, Vergote K, et al. Whole abdominopelvic radiotherapy (WAPRT) using intensity-modulated arc therapy (IMAT): first clinical experience. Int J Radiat Oncol Biol Phys 2003;57:1019-32. 10.1016/S0360-3016(03)00663-1 [DOI] [PubMed] [Google Scholar]
- 22.Lim K, Small W, Jr, Portelance L, et al. Consensus guidelines for delineation of clinical target volume for intensity-modulated pelvic radiotherapy for the definitive treatment of cervix cancer. Int J Radiat Oncol Biol Phys 2011;79:348-55. 10.1016/j.ijrobp.2009.10.075 [DOI] [PubMed] [Google Scholar]
- 23.Gaffney D, Mundt A, Schwarz J, et al. Advances in clinical research in gynecologic radiation oncology: an RTOG symposium. Int J Gynecol Cancer 2012;22:667-74. 10.1097/IGC.0b013e31824771fb [DOI] [PubMed] [Google Scholar]
- 24.Kavanagh BD, Pan CC, Dawson LA, et al. Radiation dose-volume effects in the stomach and small bowel. Int J Radiat Oncol Biol Phys 2010;76:S101-7. 10.1016/j.ijrobp.2009.05.071 [DOI] [PubMed] [Google Scholar]
- 25.Erpolat OP, Alco G, Caglar HB, et al. Comparison of hematologic toxicity between 3DCRT and IMRT planning in cervical cancer patients after concurrent chemoradiotherapy: a national multi-center study. Eur J Gynaecol Oncol 2014;35:62-6. [PubMed] [Google Scholar]
- 26.Yu C, Zhu W, Ji Y, et al. A comparative study of intensity-modulated radiotherapy and standard radiation field with concurrent chemotherapy for local advanced cervical cancer. Eur J Gynaecol Oncol 2015;36:278-82. [PubMed] [Google Scholar]
- 27.Renard-Oldrini S, Brunaud C, Huger S, et al. Dosimetric comparison between the intensity modulated radiotherapy with fixed field and Rapid Arc of cervix cancer. Cancer Radiother 2012;16:209-14. 10.1016/j.canrad.2012.02.002 [DOI] [PubMed] [Google Scholar]
- 28.Lesnock JL, Farris C, Beriwal S, et al. Upfront treatment of locally advanced cervical cancer with intensity modulated radiation therapy compared to four field radiation therapy: a cost-effectiveness analysis. Gynecol Oncol 2013;129:574-9. 10.1016/j.ygyno.2013.02.012 [DOI] [PubMed] [Google Scholar]
- 29.Huang B, Fang Z, Huang Y, et al. A dosimetric analysis of volumetric-modulated arc radiotherapy with jaw width restriction vs 7 field intensity-modulated radiotherapy for definitive treatment of cervical cancer. Br J Radiol 2014;87:20140183. 10.1259/bjr.20140183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen K, Cummings D, Lanza VC, et al. A dosimetric comparative study: volumetric modulated arc therapy vs intensity-modulated radiation therapy in the treatment of nasal cavity carcinomas. Med Dosim 2013;38:225-32. 10.1016/j.meddos.2013.01.006 [DOI] [PubMed] [Google Scholar]
- 31.Osborne EM, Klopp AH, Jhingran A, et al. Impact of treatment year on survival and adverse effects in patients with cervical cancer and paraortic lymph node metastases treated with definitive extended-field radiation therapy. Pract Radiat Oncol 2017;7:e165-73. 10.1016/j.prro.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 32.Portelance L, Chao KS, Grigsby PW, et al. Intensity-modulated radiation therapy (IMRT) reduces small bowel, rectum, and bladder doses in patients with cervical cancer receiving pelvic and para-aortic irradiation. Int J Radiat Oncol Biol Phys 2001;51:261-6. 10.1016/S0360-3016(01)01664-9 [DOI] [PubMed] [Google Scholar]
- 33.Mutic S, Dempsey JF. The ViewRay system: magnetic resonance-guided and controlled radiotherapy. Semin Radiat Oncol 2014;24:196-9. 10.1016/j.semradonc.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 34.Guy JB, Falk AT, Auberdiac P, et al. Dosimetric study of volumetric arc modulation with RapidArc and intensity-modulated radiotherapy in patients with cervical cancer and comparison with 3-dimensional conformal technique for definitive radiotherapy in patients with cervical cancer. Med Dosim 2016;41:9-14. 10.1016/j.meddos.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 35.Wild E, Bangert M, Nill S, et al. Noncoplanar VMAT for nasopharyngeal tumors: Plan quality versus treatment time. Med Phys 2015;42:2157-68. 10.1118/1.4914863 [DOI] [PubMed] [Google Scholar]