Abstract
Noninvasive biomarkers are clinically useful for evaluating liver fibrosis stage in patients with nonalcoholic fatty liver disease (NAFLD). The aim of the present study was to compare plasma proteins in patients with early nonalcoholic steatohepatitis (NASH) (F0-F1) versus NASH with significant/advanced fibrosis (F2–F4) to determine whether candidate proteins could be used as potential noninvasive biomarkers. Nineteen biopsy-proven NAFLD patients including ten early NASH patients and nine NASH patients with significant/advanced fibrosis were enrolled in the present study. High-resolution proteomics screening of plasma was performed with the SCIEX TripleTOF 5600 System. Proteins were quantified using two different software platforms, Progenesis Qi and Scaffold Q+, respectively. Progenesis Qi analysis resulted in the discovery of 277 proteins compared with 235 proteins in Scaffold Q+. Five consensus proteins (i.e. Complement component C7; α-2-macroglobulin; Complement component C8 γ chain; Fibulin-1; α-1-antichymotrypsin) were identified. Complement component C7 was three-fold higher in the NASH group with significant/advanced fibrosis (F2–F4) compared with the early NASH (F0-F1) group (q-value = 3.6E-6). Complement component C7 and Fibulin-1 are positively correlated with liver stiffness (P=0.000, P=0.002, respectively); whereas, Complement component C8 γ chain is negatively correlated (P=0.009). High levels of Complement C7 are associated with NASH with significant/advanced fibrosis and Complement C7 is a perfect classifier of patients included in this pilot study. Further studies will be needed in a larger validation cohort to confirm the utility of complement proteins as biomarkers or mechanistic determinants of NASH with significant/advanced fibrosis.
Keywords: Complement, Liver fibrosis, NAFLD, Noninvasive biomarker, Proteomics
Introduction
Nonalcoholic fatty liver disease (NAFLD), one of the most common liver diseases worldwide, can be categorized histologically into nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH) [1]. Accurately evaluating liver fibrosis stage in NAFLD patients is of importance for identifying those who may progress to liver cirrhosis and hepatocellular carcinoma. Although a liver biopsy is the gold standard for diagnosing and determining the stages of fibrosis, there is an urgent need to develop noninvasive methods [2–12], including imaging modalities [13–17], biomarkers [18–26], and artificial intelligence algorithms [27–32].
The purpose of the present study was to perform proteomic screening of plasma via SCIEX TripleTOF 5600 System [33–35] to identify potential noninvasive biomarkers in NAFLD patients with significant/advanced liver fibrosis.
Methods
Patients
Plasma samples were acquired through the ‘Prevalence and Risk Factors for NAFLD in patients with T2DM’ study conducted at the Royal London Hospital, Barts Health NHS Trust, United Kingdom (U.K.). The study was approved by the National Research Ethic Service (Reference 14/WA/1142) and carried out in accordance with the World Medical Association Declaration of Helsinki. Written informed consent was obtained from all participants.
Histological evaluation
All patients enrolled in the present study had undergone a percutaneous liver biopsy. Fibrosis stage was scored according to the Kleiner classification [36] on a 5-point scale (F0–F4).
Clinical and biochemical data
Relevant clinical data were recorded, including the patients’ age, sex, weight, and height. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Venous blood samples were collected in lithium-heparin tubes and plasma was stored at −80°C until analysis. Laboratory evaluation in all patients included measurement of the serum levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT). Liver stiffness for all patients were assessed by FibroScan.
Proteomics and data processing
Plasma was assayed for total protein (Bio-Rad Protein Assay) and 5 µl was digested with trypsin (1:10 ratio enzyme to protein) for 18 h at 37°C following following reduction and alkylation as we previously described [37]. Peptides were desalted using solid phase extraction cartridges (Strata-x, Phenomenex) and eluted sequentially in 25% acetonitrile/0.1% formic acid and 45% acetonitrile/0.1% formic acid. Each peptide fraction was diluted 1:4000 in 0.1% formic acid and 10 µl injected on to a 2-cm c18 trap column (Dionex pepmap100, Thermo Scientific). Peptides were separated on a c18 analytical column (15 cm × 75 µm, Dionex pepmap 100) for 60 min from 0.1% formic acid to 50% acetonitrile/0.1% formic acid. Data were acquired in IDA mode on a SCIEX 5600. Wiff files were uploaded to Progenesis Qi or converted into .MGFs for MASCOT searching (v2.4) against the human proteome database (SwissProt/UniProt; 2015) before being loaded to Scaffold Q+. Both Progenesis Qi and Scaffold Q+ were utilized to determine significant protein differences to construct a consensus differential protein list to reduce analytical bias of a single software platform. Proteomics data of the present study has been loaded into the ProteomeXchange database (Submission Reference No.: 1-20190126-112361).
Statistical analysis
Statistical differences in Progenesis Qi were determined using ANOVA of log2 transformed data and P-values corrected for local false discovery rate (q-value). Proteins with q-values less than 0.05 were considered different. Statistical differences in Scaffold Q+ were determined using a t test of normalized spectral abundance factors (NSAF) as a comparison with Progenesis Qi results. NSAF values were not transformed for normality, nor were P-values adjusted for multiple comparisons. For statistically different proteins (Progenesis Qi), receiver operating characteristic (ROC) curves were created in Sigmaplot plotted using the data from Progenesis Qi, and the areas under the ROC curves (AUROCs) were calculated in order to represent classification performance. Correlation analysis was performed by using the Pearson’s correlation coefficient test in SPSS (IBM). Differences were considered to be statistically significant at P<0.05.
Results
Characteristics of NAFLD patients
A total of 19 biopsy-proven NAFLD patients were enrolled in the present study, including 10 early NASH patients and 9 NASH patients with significant/advanced fibrosis. The characteristics of the patients are summarized in Table 1. There were no significant differences in terms of sex, age, BMI, ALT, AST and smoking between the two groups. Patients with significant/advanced NASH fibrosis had elevated liver stiffness (P<0.001), Fibrosis-4 (FIB-4) score (P<0.01), and a higher prevalence of diabetes (P<0.001).
Table 1. Clinical characteristics of the patients enrolled in the study.
| Early NASH (F0-1) | Advanced NASH (F2–4) | P-value | |
|---|---|---|---|
| Sex (M/F) | (4/6) | (5/4) | 0.65 |
| Age (Mean [Range], Years) | 55.6 [35–70] | 58.4 [47–74] | 0.56 |
| BMI | 31 ± 4 | 32 ± 4 | 0.38 |
| Diabetes (No. Pts) | 1 | 9 | <0.001 |
| Stiffness (kPa) | 5.8 ±1.7 | 19.7 ± 9.8 | <0.001 |
| FIB4 | 1.1 ± 0.2 | 2.1 ±0.9 | <0.01 |
| ALT | 44 ± 34 | 65 ± 29 | 0.34 |
| AST | 34 ± 20 | 51 ± 19 | 0.14 |
| Smoker (%) | 90% | 89% | 1 |
Differentially abundant plasma proteins
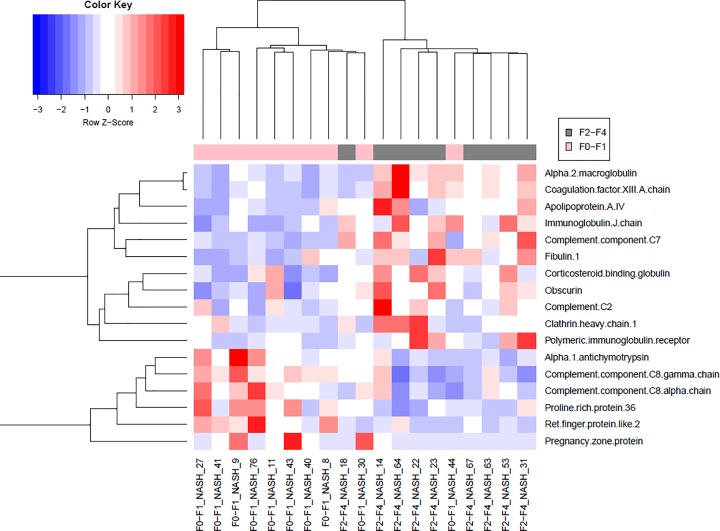
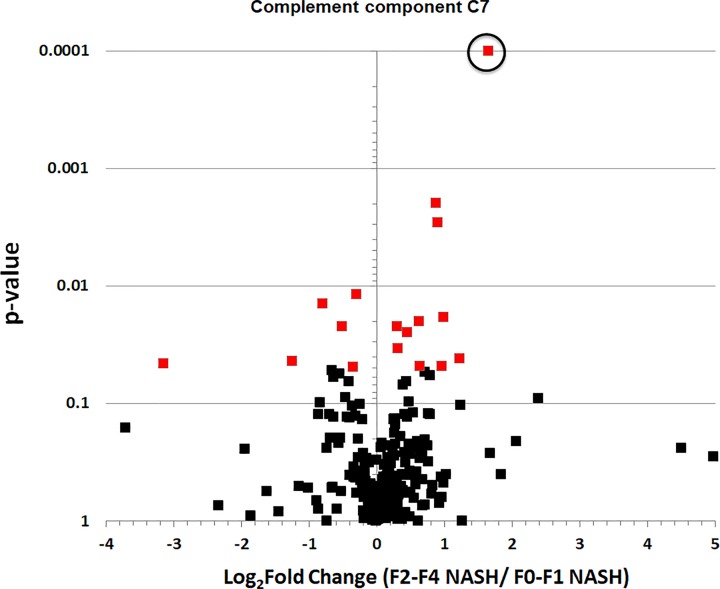
Progenesis Qi workflow analysis resulted in the discovery of 277 proteins compared with 235 proteins in Scaffold Q+ workflow. Five consensus proteins (i.e. Complement component C7; α-2-macroglobulin; Complement component C8 γ chain; Fibulin-1; α-1-antichymotrypsin) were shown in Table 2. Hierarchal clustering of 17 significantly different proteins from the Progenesis Qi workflow was utilized to group patients using an average (UPGMA) agglomeration method in R Studio. Color intensity indicates standard deviations from the mean (Z-score) in a positive (red) or negative (blue) direction (Figure 1). The volcano plot (log2 fold change vs. P-value) displays all proteins identified in the Progenesis Qi analysis (Figure 2). Complement component C7 was three-fold higher (log2 = 1.65) in the NASH group (F2–F4) with significant/advanced fibrosis compared with the early NASH (F0-F1) group (q-value = 3.6E-6).
Table 2. Identification of five consensus proteins via Progenesis Qi and Scaffold Q+ analysis in NASH patients with significant/advanced fibrosis versus early NASH patients.
| Protein name | Progenesis Qi (total proteins = 277) | Scaffold Q (total proteins = 235) |
|---|---|---|
| Complement component C7 |  |
 |
| α-2-macroglobulin |  |
 |
| Complement component C8 γ chain |  |
 |
| Fibulin-1 OS = Homo sapiens |  |
 |
| α-1-antichymotrypsin |  |
 |
Figure 1. Hierarchal clustering heat map of significant plasma proteins as discovered by Progenesis Qi analysis.
Hierarchal clustering of 17 significantly different proteins was utilized to group patients using an average (UPGMA) agglomeration method in R Studio. Color intensity indicates standard deviations from the mean (Z-score) in a positive (red) or negative (blue) direction.
Figure 2. The volcano plot of all proteins identified in the Progenesis Qi analysis.
Complement C7 was circled above and was three-fold higher (log2 = 1.65) in the NASH group with significant/advanced fibrosis (F2–F4) compared with the early NASH (F0-F1) group (actual q-value = 3.6E-6, but was changed to 0.0001 for display purposes).
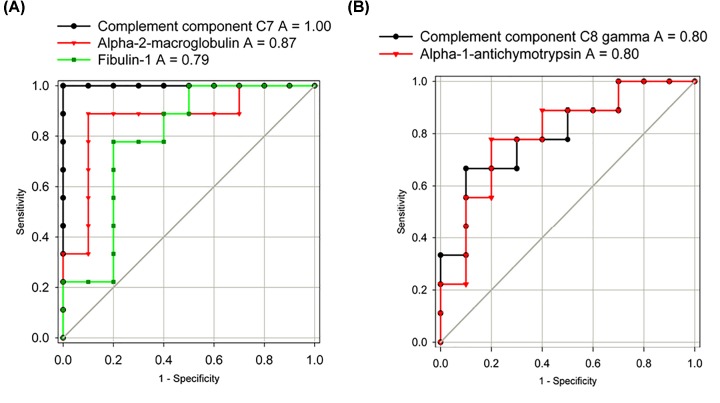
ROC curves
Classification performance was estimated using AUROCs for the five consensus different proteins identified. As shown in Figure 3A, the AUROCs for those proteins elevated in NASH patients with significant/advanced fibrosis (F2–F4) are 1.00 (Complement component C7), 0.87 (α-2-macroglobulin), and 0.79 (Fibulin-1), respectively. As shown in Figure 3B, the AUROCs for those proteins reduced in NASH patients with significant/advanced fibrosis (F2–F4) are both 0.80 (Complement component C8 γ chain; α-1-antichymotrypsin).
Figure 3. Classification performance estimated using ROC curve for the five consensus differential plasma proteins.
(A) Proteins elevated in the NASH patients with significant/advanced fibrosis (F2–F4). (B) Proteins lower in the NASH patients with significant/advanced fibrosis (F2–F4). Abbreviation: AUC, area under the curve. All areas have a P-value <0.03.
Correlation analysis
As shown in Table 3, Complement component C7 and Fibulin-1 are positively correlated with liver stiffness (P=0.000, P=0.002, respectively); whereas, Complement component C8 γ chain is negatively correlated (P=0.009). Moreover, Complement C7 and α-2-macroglobulin were positively correlated with FIB-4 (P=0.031, P=0.042, respectively) while Complement component C8 γ chain was negatively correlated with FIB-4 (P=0.013). Interestingly, Complement component C7 also positively correlated with HBA1c (P=0.045) while γ-1-antichymotrypsin is negatively correlated with ALT (P=0.036).
Table 3. Pearson’s r correlation analysis of five consensus differential plasma proteins.
| Stiffness | Complement C7 | α-2- macroglobulin | Complement C8 γ chain | Fibulin-1 | α-1-antichymotrypsin | ||
|---|---|---|---|---|---|---|---|
| Stiffness | Pearson correlation | - | 0.740† | 0.407 | −0.584† | 0.657† | −0.453 |
| Sig. (two-tailed) | - | 0.000 | 0.084 | 0.009 | 0.002 | 0.051 | |
| n | - | 19 | 19 | 19 | 19 | 19 | |
| FIB-4 | Pearson correlation | 0.502 | 0.556* | 0.530* | −0.623* | 0.297 | −0.330 |
| Sig. (two-tailed) | 0.056 | 0.031 | 0.042 | 0.013 | 0.282 | 0.230 | |
| n | 15 | 15 | 15 | 15 | 15 | 15 | |
| ALT | Pearson correlation | 0.126 | 0.037 | 0.185 | −0.459 | 0.320 | −0.511* |
| Sig. (two-tailed) | 0.629 | 0.887 | 0.477 | 0.064 | 0.210 | 0.036 | |
| n | 17 | 17 | 17 | 17 | 17 | 17 | |
| HBA1c | Pearson correlation | 0.539 | 0.613* | 0.438 | −0.077 | 0.010 | 0.068 |
| Sig. (two-tailed) | 0.087 | 0.045 | 0.178 | 0.821 | 0.977 | 0.843 | |
| n | 11 | 11 | 11 | 11 | 11 | 11 | |
| BMI | Pearson Correlation | 0.277 | 0.228 | 0.264 | −0.167 | 0.267 | 0.072 |
| Sig. (two-tailed) | 0.251 | 0.347 | 0.274 | 0.494 | 0.270 | 0.770 | |
| N | 19 | 19 | 19 | 19 | 19 | 19 |
Correlation is significant at the 0.05 level (two-tailed).
Correlation is significant at the 0.01 level (two-tailed).
Discussion
The present study showed for the first time that Complement C7 and C8 γ chain and Fibulin-1 significantly correlate with liver stiffness. Moreover, Complement C7 acted as a potential biomarker to identify those NASH patients with significant/advanced liver fibrosis.
The complement system, a phylogenetically ancient makeup of the humoral system, consisting of a cascade of proteases and soluble factors, plays a vital role in innate immune [38]. The role of complement in liver diseases is less well characterized. The complement components C3 and C5 were reported to be associated with NAFLD [39–41] and C5 had a causal role in liver fibrogenesis [42]. There are strong and persistent stimuli for complement activation in NAFLD through multiple pathways, including the classical pathway and the lectin pathway [43], as well as the alternative pathway [44]. The complement component 7 (C7) is a terminal component of the complement cascade. The role C7 plays in the pathogenesis and progression of NAFLD are largely unknown. Our results showed that C7 was three-fold higher in the NASH group with significant/advanced fibrosis (F2–F4) compared with the early NASH (F0-F1) group, consistent with previous studies [45], suggesting C7 might be an important contributor in the pathogenesis of NAFLD. The exact mechanisms of C7 in the progress of NAFLD need to be further elucidated.
One limitation of our pilot study is the relatively small number of patients. Nevertheless, the sample numbers were sufficient to show significant differences in plasma proteins between early NASH and NASH with significant/advanced fibrosis in a conceptual approach.
In summary, the present study demonstrated that Complement C7 and C8 γ chain as well as Fibulin-1 significantly correlated with liver stiffness. Elevated levels of Complement C7 were detected in NASH patients with significant/advanced fibrosis and were a perfect classifier for patients included in this pilot study. Further studies in a larger validation cohort will be needed to confirm the utility of complement proteins as potential biomarkers or mechanistic determinants of progressive NASH.
Perspectives
Accurately evaluating liver fibrosis stage in NAFLD is important because it enables the identification of those most likely to progress to liver cirrhosis and hepatocellular carcinoma. Although a liver biopsy remains the current gold standard for diagnosis and staging of liver disease, it is invasive, costly, and with inherent risks; hence there is an urgent need to develop noninvasive methods.
Proteomic screening of plasma via SCIEX TripleTOF 5600 System identified potential noninvasive biomarkers of NAFLD patients with significant/advanced liver fibrosis. Complement components C7 and C8 γ chain, and Fibulin-1 significantly correlated with liver stiffness.
In this pilot, high levels of Complement C7 were associated with NASH with significant/advanced fibrosis and Complement C7 is a perfect classifier of patients with NASH.
Abbreviations
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- AUROC
area under the ROC curve
- BMI
body mass index
- FIB-4
Fibrosis-4
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- NSAF
normalized spectral abundance factor
- ROC
receiver operating characteristic
Contributor Information
Michael G. Janech, Email: janechmg@cofc.edu.
Wing-Kin Syn, Email: synw@musc.edu.
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
This work was supported in part by the Office of Naval Research [grant number N000141410361 (to M.G.J.)]; the Division of Gastroenterology and Hepatology and Division of Nephrology Funds [(to W.-K.S.), (to M.G.J.)]; the Ralph H. Johnson VAMC [(to W.-K.S.)]; and the Diabetes Research and Wellness Fund [(to W.A. and W.-K.S.)].
Author Contribution
W.-K.S. and M.G.J. conceived and designed the study. W.H., M.G.J., P.S., A.B., W.-K.S. performed data collection and analysis, and contributed to drafting of the manuscript. S.S. and W.A. provided technical and material support. W.H., M.G.J., W.A. and W.-K.S. contributed to critical revision of the manuscript. All authors approved the final version of the manuscript.
References
- 1.Chalasani N., Younossi Z., Lavine J.E., Charlton M., Cusi K., Rinella M. et al. (2018) The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67, 328–357 10.1002/hep.29367 [DOI] [PubMed] [Google Scholar]
- 2.Brunt E.M., Wong V.W., Nobili V., Day C.P., Sookoian S., Maher J.J. et al. (2015) Nonalcoholic fatty liver disease. Nat. Rev. Dis. Primers 1, 15080 10.1038/nrdp.2015.80 [DOI] [PubMed] [Google Scholar]
- 3.Rinella M.E. (2015) Nonalcoholic fatty liver disease: a systematic review. JAMA 313, 2263–2273 10.1001/jama.2015.5370 [DOI] [PubMed] [Google Scholar]
- 4.Cheah M.C., McCullough A.J. and Goh G.B. (2017) Current modalities of fibrosis assessment in non-alcoholic fatty liver disease. J. Clin. Transl. Hepatol. 5, 261–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tapper E.B. and Lok A.S. (2017) Use of liver imaging and biopsy in clinical practice. N. Engl. J. Med. 377, 756–768 10.1056/NEJMra1610570 [DOI] [PubMed] [Google Scholar]
- 6.Bellan M., Castello L.M. and Pirisi M. (2018) Candidate biomarkers of liver fibrosis: a concise, pathophysiology-oriented review. J. Clin. Transl. Hepatol. 6, 317–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schuppan D., Surabattula R. and Wang X.Y. (2018) Determinants of fibrosis progression and regression in NASH. J. Hepatol. 68, 238–250 10.1016/j.jhep.2017.11.012 [DOI] [PubMed] [Google Scholar]
- 8.Tsai E. and Lee T.P. (2018) Diagnosis and evaluation of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis, including noninvasive biomarkers and transient elastography. Clin. Liver Dis. 22, 73–92 10.1016/j.cld.2017.08.004 [DOI] [PubMed] [Google Scholar]
- 9.Vilar-Gomez E. and Chalasani N. (2018) Non-invasive assessment of non-alcoholic fatty liver disease: clinical prediction rules and blood-based biomarkers. J. Hepatol. 68, 305–315 10.1016/j.jhep.2017.11.013 [DOI] [PubMed] [Google Scholar]
- 10.Wong V.W., Adams L.A., de Lédinghen V., Wong G.L. and Sookoian S. (2018) Noninvasive biomarkers in NAFLD and NASH - current progress and future promise. Nat. Rev. Gastroenterol. Hepatol. 15, 461–478 10.1038/s41575-018-0014-9 [DOI] [PubMed] [Google Scholar]
- 11.Yoneda M., Imajo K., Takahashi H., Ogawa Y., Eguchi Y., Sumida Y. et al. (2018) Clinical strategy of diagnosing and following patients with nonalcoholic fatty liver disease based on invasive and noninvasive methods. J. Gastroenterol. 53, 181–196 10.1007/s00535-017-1414-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Younossi Z.M., Loomba R., Anstee Q.M., Rinella M.E., Bugianesi E., Marchesini G. et al. (2018) Diagnostic modalities for nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, and associated fibrosis. Hepatology 68, 349–360 10.1002/hep.29721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim D., Kim W.R., Talwalkar J.A., Kim H.J. and Ehman R.L. (2013) Advanced fibrosis in nonalcoholic fatty liver disease: noninvasive assessment with MR elastography. Radiology 268, 411–419 10.1148/radiol.13121193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loomba R., Wolfson T., Ang B., Hooker J., Behling C., Peterson M. et al. (2014) Magnetic resonance elastography predicts advanced fibrosis in patients with nonalcoholic fatty liver disease: a prospective study. Hepatology 60, 1920–1928 10.1002/hep.27362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cassinotto C., Boursier J., de Lédinghen V., Lebigot J., Lapuyade B., Cales P. et al. (2016) Liver stiffness in nonalcoholic fatty liver disease: a comparison of supersonic shear imaging, FibroScan, and ARFI with liver biopsy. Hepatology 63, 1817–1827 10.1002/hep.28394 [DOI] [PubMed] [Google Scholar]
- 16.Tapper E.B., Challies T., Nasser I., Afdhal N.H. and Lai M. (2016) The performance of vibration controlled transient elastography in a US cohort of patients with nonalcoholic fatty liver disease. Am. J. Gastroenterol. 111, 677–684 10.1038/ajg.2016.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tapper E.B. and Loomba R. (2018) Noninvasive imaging biomarker assessment of liver fibrosis by elastography in NAFLD. Nat. Rev. Gastroenterol. Hepatol. 15, 274–282 10.1038/nrgastro.2018.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoneda M., Fujii H., Sumida Y., Hyogo H., Itoh Y., Ono M. et al. (2011) Platelet count for predicting fibrosis in nonalcoholic fatty liver disease. J. Gastroenterol. 46, 1300–1306 10.1007/s00535-011-0436-4 [DOI] [PubMed] [Google Scholar]
- 19.Hashiba M., Ono M., Hyogo H., Ikeda Y., Masuda K., Yoshioka R. et al. (2013) Glycemic variability is an independent predictive factor for development of hepatic fibrosis in nonalcoholic fatty liver disease. PLoS ONE 8, e76161, 10.1371/journal.pone.0076161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tokushige K., Hashimoto E., Kodama K., Tobari M., Matsushita N., Kogiso T. et al. (2013) Serum metabolomic profile and potential biomarkers for severity of fibrosis in nonalcoholic fatty liver disease. J. Gastroenterol. 48, 1392–1400 10.1007/s00535-013-0766-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abe M., Miyake T., Kuno A., Imai Y., Sawai Y., Hino K. et al. (2015) Association between Wisteria floribunda agglutinin-positive Mac-2 binding protein and the fibrosis stage of non-alcoholic fatty liver disease. J. Gastroenterol. 50, 776–784 10.1007/s00535-014-1007-2 [DOI] [PubMed] [Google Scholar]
- 22.Kamada Y., Ono M., Hyogo H., Fujii H., Sumida Y., Yamada M. et al. (2017) Use of Mac-2 binding protein as a biomarker for nonalcoholic fatty liver disease diagnosis. Hepatol. Commun. 1, 780–791 10.1002/hep4.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cansanção K., Silva Monteiro L., Carvalho Leite N., Dávalos A., Tavares do Carmo M.D.G. and Arantes Ferreira Peres W. (2018) Advanced liver fibrosis is independently associated with palmitic acid and insulin levels in patients with non-alcoholic fatty liver disease. Nutrients 10, pii: E1586 10.3390/nu10111586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glass O., Henao R., Patel K., Guy C.D., Gruss H.J., Syn W.K. et al. (2018) Serum interleukin-8, osteopontin, and monocyte chemoattractant protein 1 are associated with hepatic fibrosis in patients with nonalcoholic fatty liver disease. Hepatol. Commun. 2, 1344–1355 10.1002/hep4.1237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koo B.K., Um S.H., Seo D.S., Joo S.K., Bae J.M., Park J.H. et al. (2018) Growth differentiation factor 15 predicts advanced fibrosis in biopsy-proven non-alcoholic fatty liver disease. Liver Int. 38, 695–705 10.1111/liv.13587 [DOI] [PubMed] [Google Scholar]
- 26.Luther J., Gala M.K., Borren N., Masia R., Goodman R.P., Moeller I.H. et al. (2018) Hepatic connexin 32 associates with nonalcoholic fatty liver disease severity. Hepatol. Commun. 2, 786–797 10.1002/hep4.1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Angulo P., Hui J.M., Marchesini G., Bugianesi E., George J., Farrell G.C. et al. (2007) The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 45, 846–854 10.1002/hep.21496 [DOI] [PubMed] [Google Scholar]
- 28.Shah A.G., Lydecker A., Murray K., Tetri B.N., Contos M.J., Sanyal A.J. et al. (2009) Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 7, 1104–1112 10.1016/j.cgh.2009.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ishiba H., Sumida Y., Tanaka S., Yoneda M., Hyogo H., Ono M. et al. (2018) The novel cutoff points for the FIB4 index categorized by age increase the diagnostic accuracy in NAFLD: a multi-center study. J Gastroenterol. 53, 1216–1224 10.1007/s00535-018-1474-y [DOI] [PubMed] [Google Scholar]
- 30.Loomba R., Jain A., Diehl A.M., Guy C.D., Portenier D., Sudan R. et al. (2019) Validation of serum test for advanced liver fibrosis in patients with nonalcoholic steatohepatitis. Clin. Gastroenterol. Hepatol. 17, 1867–1876 [DOI] [PubMed] [Google Scholar]
- 31.Patel Y.A., Gifford E.J., Glass L.M., Turner M.J., Han B., Moylan C.A. et al. (2018) Identifying nonalcoholic fatty liver disease advanced fibrosis in the veterans health administration. Dig. Dis. Sci. 63, 2259–2266 10.1007/s10620-018-5123-3 [DOI] [PubMed] [Google Scholar]
- 32.Polyzos S.A., Slavakis A., Koumerkeridis G., Katsinelos P. and Kountouras J. (2019) Noninvasive liver fibrosis tests in patients with nonalcoholic fatty liver disease: an external validation cohort. Horm. Metab. Res. 51, 134–140 [DOI] [PubMed] [Google Scholar]
- 33.Andrews G.L., Simons B.L., Young J.B., Hawkridge A.M. and Muddiman D.C. (2011) Performance characteristics of a new hybrid quadrupole time-of-flight tandem mass spectrometer (TripleTOF 5600). Anal. Chem. 83, 5442–5446 10.1021/ac200812d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dillen L., Cools W., Vereyken L., Lorreyne W., Huybrechts T., de Vries R. et al. (2012) Comparison of triple quadrupole and high-resolution TOF-MS for quantification of peptides. Bioanalysis 4, 565–579 10.4155/bio.12.3 [DOI] [PubMed] [Google Scholar]
- 35.Jones K.A., Kim P.D., Patel B.B., Kelsen S.G., Braverman A., Swinton D.J. et al. (2013) Immunodepletion plasma proteomics by tripleTOF 5600 and Orbitrap elite/LTQ-Orbitrap Velos/Q exactive mass spectrometers. J. Proteome Res. 12, 4351–4365 10.1021/pr400307u [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kleiner D.E., Brunt E.M., Van Natta M., Behling C., Contos M.J., Cummings O.W. et al. (2005) Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41, 1313–1321 10.1002/hep.20701 [DOI] [PubMed] [Google Scholar]
- 37.Sobolesky P., Parry C., Boxall B., Wells R., Venn-Watson S. and Janech M.G. (2016) Proteomic analysis of non-depleted serum proteins from bottlenose dolphins uncovers a high Vanin-1 phenotype. Sci. Rep. 6, 33879 10.1038/srep33879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Phieler J., Garcia-Martin R., Lambris J.D. and Chavakis T. (2013) The role of the complement system in metabolic organs and metabolic diseases. Semin. Immunol. 25, 47–53 10.1016/j.smim.2013.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xin Y.N., Geng N., Lin Z.H., Cui Y.Z., Duan H.P., Zhang M. et al. (2014) Serum complement C3f and fibrinopeptide A are potential novel diagnostic biomarkers for non-alcoholic fatty liver disease: a study in Qingdao Twins. PLoS ONE 9, e108132 10.1371/journal.pone.0108132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu C., Chen Y., Xu L., Miao M., Li Y. and Yu C. (2016) Serum complement C3 levels are associated with nonalcoholic fatty liver disease independently of metabolic features in Chinese population. Sci. Rep. 6, 23279 10.1038/srep23279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hu W., Wang M., Yin C., Li S., Liu Y. and Xiao Y. (2018) Serum complement factor 5a levels are associated with nonalcoholic fatty liver disease in obese children. Acta Paediatr. 107, 322–327 10.1111/apa.14106 [DOI] [PubMed] [Google Scholar]
- 42.Hillebrandt S., Wasmuth H.E., Weiskirchen R., Hellerbrand C., Keppeler H., Werth A. et al. (2005) Complement factor 5 is a quantitative trait gene that modifies liver fibrogenesis in mice and humans. Nat. Genet. 37, 835–843 10.1038/ng1599 [DOI] [PubMed] [Google Scholar]
- 43.Rensen S.S., Slaats Y., Driessen A., Peutz-Kootstra C.J., Nijhuis J., Steffensen R. et al. (2009) Activation of the complement system in human nonalcoholic fatty liver disease. Hepatology 50, 1809–1817 10.1002/hep.23228 [DOI] [PubMed] [Google Scholar]
- 44.Segers F.M., Verdam F.J., de Jonge C., Boonen B., Driessen A., Shiri-Sverdlov R. et al. (2014) Complement alternative pathway activation in human nonalcoholic steatohepatitis. PLoS ONE 9, e110053 10.1371/journal.pone.0110053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bell L.N., Theodorakis J.L., Vuppalanchi R., Saxena R., Bemis K.G., Wang M. et al. (2010) Serum proteomics and biomarker discovery across the spectrum of nonalcoholic fatty liver disease. Hepatology 51, 111–120 10.1002/hep.23271 [DOI] [PMC free article] [PubMed] [Google Scholar]