Abstract
Prematurity is associated with perinatal neuroinflammation and injury. Screening for genetic modulators in an LPS murine model of preterm birth revealed the upregulation of Nr4a1, an orphan nuclear transcription factor that is normally absent or limited in embryonic brains. Concurrently, Nr4a1 was downregulated with magnesium sulfate (MgSO4) and betamethasone (BMTZ) treatments administered to LPS exposed dams. To understand the role of Nr4a1 in perinatal brain injury, we compared the preterm neuroinflammatory response in Nr4a1 knockout (KO) versus wild type (wt) mice. Key inflammatory factors Il1b, Il6 and Tnf, and Iba1+ microglia were significantly lower in Nr4a1 KO versus wt brains exposed to LPS in utero. Treatment with MgSO4/BMTZ mitigated the neuroinflammatory process in wt but not Nr4a1 KO brains. These results correspond with a reduction in cerebral hemorrhage in wt but not mutant embryos from dams given MgSO4/BMTZ. Further analysis with Nr4a1-GFP-Cre × tdTomato loxP reporter mice revealed that the upregulation of Nr4a1 with perinatal neuroinflammation occurs in the cerebral vasculature. Altogether, this study implicates Nr4a1 in the developing vasculature as a potent mediator of neuroinflammatory brain injury that occurs with preterm birth. It is also possible that MgSO4/BMTZ mitigates this process by direct or indirect inhibition of Nr4a1.
Subject terms: Disease model, Cellular neuroscience
Introduction
Preterm delivery and the long-term impacts on the developing neonate remain a major concern for obstetric care in the United States. The rate of preterm birth in the United States continue to rise1. Though our understanding of preterm birth and the associated fetal complications continues to evolve, there is still much to address. The pathogenesis of preterm birth and its consequences is complex and multifactorial, likely resulting from numerous elements including intrauterine inflammation and dysregulation of fetal neurodevelopmental processes2,3.
Preterm delivery, particularly when earlier in gestation, is linked to a high prevalence of cognitive impairment, developmental delays, and central nervous system disorders, such as cerebral palsy (CP)4,5. Perinatal brain injury is thought to result from acute neuroinflammation, driven by an excess of cytokines and immunological responses2,6. Treatment aimed at reducing perinatal neuroinflammation includes magnesium sulfate (MgSO4), which is thought to reduce vascular instability, decrease pro-inflammatory cytokines, and/or prevent hypoxic injury and ischemia-induced tissue damage6. Although the underlying molecular mechanisms of MgSO4 remain poorly understood, antenatal use has been shown to decrease the incidence of CP. Several randomized controlled trials have demonstrated improved outcomes with MgSO4, particularly for preterm pregnancies treated before 32–34 weeks gestation7–12. However, the effectiveness of MgSO4 is not guaranteed with an estimated number needed to treat of 5613.
In conjunction with MgSO4, antenatal corticosteroids such as betamethasone (BMTZ), have also improved fetal outcomes. Trials using corticosteroids in preterm labor have demonstrated reductions in intracranial hemorrhage and cystic periventricular leukomalacia14,15. Corticosteroids are characteristically anti-inflammatory and may alleviate the fetal neuroinflammatory burden with prematurity. Analogous to MgSO4, the exact molecular mechanisms of corticosteroids remain unclear16. If the mechanisms of injury and the actions of these treatments are delineated, other interventions may be developed.
We sought to identify pro-inflammatory targets that are responsive to MgSO4 and BMTZ treatments. Using microarray screening, we identified the upregulation of Nr4a1 in a murine model of preterm labor. Nr4a1 is an orphan nuclear receptor, also known as Nur77, TR3, and NGFI-B, that has been implicated in a variety of immune responses and adult neuroinflammatory injury17–20. In the prenatal brain, Nr4a1 expression is limited and not required for normal development21–23. Based on these preliminary findings, we hypothesized that Nr4a1 plays an important role in perinatal brain injury and sought to characterize its role using mutant mouse models. Our primary objective was to evaluate the neuroinflammatory response of Nr4a1 knockout (KO) versus wild type (wt) mice. Additionally, we sought to evaluate the relationship between Nr4a1 KO and wt mice in conjunction with MgSO4 and BMTZ treatments. Finally, we used Cre-loxP fate mapping to identify the cellular expression of Nr4a1 that is upregulated in response to perinatal neuroinflammation.
Materials and methods
Animal models
All animal experiments and procedures were approved by the Institutional Animal Care and Use Committee. Animals were randomly selected to receive treatments in all experiments/groups and the data acquisition/analysis was performed blinded with coded samples. For the microarray screening, CD-1 mice were purchased from Charles River Laboratories (Wilmington, MA, USA) and on E15.5 received an intrauterine injection of 100 µl containing 100 µg lipopolysaccharide (LPS) from Escherichia coli O55:B5 (Sigma-Aldrich, St. Louis, MO, USA) or the vehicle (PBS)24. Mice were subsequently treated with normal saline (NS) or MgSO4/BMTZ, 30 min post-injection of LPS/PBS. MgSO4 and BMTZ treatments were administered subcutaneously as previously described25. Brains were harvested 6 h following the intrauterine injections and frozen immediately in liquid nitrogen for expression analysis. Sample sizes were estimated based on cytokine gene expression from previous studies26,27.
Nr4a1 KO and wt controls on a C57BL/6 background were acquired from The Jackson Laboratory (Bar Harbor, ME, USA)22. Once acclimated (2 weeks), males and females were paired by their respective genotypes: KO male with KO female and wt male with wt female. Pregnancy was confirmed by the presence of a vaginal plug at which time males were separated from the females. At E15.5, females received a 100 µl intrauterine injection of either the PBS vehicle or 250 µg of LPS. The higher LPS dose was chosen for this and subsequent experiments in order to evaluate a more severe neuroinflammatory response that has been reported for the C57BL/6 strain28. A second group of wt and Nr4a1 KO mice received LPS or PBS and subsequent treatment with MgSO4/BMTZ as previously described. Embryos were again collected 6 h following the intrauterine injections. In these experiments, brains were harvested from half of the embryos for expression analysis while the remainder were placed in formalin, cut sagittal and embedded in paraffin.
For fate mapping, Nr4a1-GFP-Cre recombinase and tdTomato loxP reporter mice were acquired from The Jackson Laboratory; strains C57BL/6-Tg(Nr4a1-EGFP/cre820Khog/J and B6.Cg-Gt(ROSA)26Sortm14(CAG-tdTomato)Hze/J respectively. The Nr4a1-GFP-Cre allele enables the expression of green fluorescent protein (GFP) and Cre simultaneously under the Nr4a1 promoter29. The tdTomato loxP allele (Ai14 variant) is irreversibly activated in the presence of Cre30. Offspring with both alleles were generated by mating Nr4a1-GFP-Cre males with tdTomato loxP females. Dams received a 100 µl intrauterine injection of either 250 µg LPS or the PBS vehicle. In these experiments, only LPS exposed mice received MgSO4/BMTZ. Six hours post-intrauterine injections, embryo brains were initially fixed by maternal cardiac perfusion. First, the right ventricle was punctured to permit drainage and then 10 ml PBS followed by 10 ml 4% formaldehyde were infused into the left ventricle31. Embryos were then placed in 5 ml 4% formaldehyde for an additional 2 h and then dehydrated with a sucrose gradient beginning with 10%, 20%, and then 30%, in which they were left overnight at 4 °C. The next day embryos were cut sagittal and frozen in optimal cutting temperature (OCT) compound.
Microarray
RNA isolation
While working on dry ice, individual CD-1 embryo brains were selected and transferred to a pre-chilled 2.0 ml tube containing one 5 mm stainless steel bead (Qiagen, Germantown, MD, USA). Once brains were transferred, 700 μl of QIAzol Lysis Reagent (Qiagen) was added to each sample. Samples were immediately homogenized using a TissueLyzer LT (Qiagen) for 5 min at 50 Hz, then placed at −80 °C until all samples were processed. RNA was extracted using the miRNeasy 96 kit (Qiagen), according to the manufacturer’s instructions. The quantity of RNA samples was evaluated with a multichannel Nanodrop 8000 spectrophotometer (Thermo Fisher, Waltham, MA, USA).
Gene array
With an input of 100 ng total RNA, hybridization-ready, fragmented, labeled, sense-stranded DNA targets were prepared using Affymetrix GeneChip® WT Plus Reagent Kit (Affymetrix, Santa Clara, CA, USA). We then prepared the labeled cDNA targets, trays, and arrays with the GeneTitan Hybridization, Wash and Stain Kit for WT array plates (Affymetrix). Samples were then applied to the Mouse Gene 2.1 ST 96 Array Plate and placed in the GeneTitan System (Affymetrix). These steps conformed to the manufacturer’s recommendations. Of the 96 arrays, 80 passed the GeneTitan scanning quality control which includes visual inspection and QC metrics provided by the Affymetrix Expression Console (hybridization control performance, labeling control performance, internal control gene performance, signal histogram, probe cell intensity, Pearson’s Correlation, and Spearman Rank Correlation). In order to verify the performance of the replicates, Pearson’s R2 was manually calculated for each set of replicates within each group. The 16 which did not meet criteria were repeated. All 16 repeats passed quality control and were included in the final analysis.
Gene array data analysis
We normalized arrays using an extension of the PLIER (Probe Logarithmic Intensity Error) algorithm, called the iterPLIER procedure, in the Affymetrix Expression Console. The iterPLIER (gene level) procedure discards feature sets that perform poorly, as described by Qu et al.32. We imported the resulting CHP files into Partek Genomics Suite version 6.12.0907 (St. Louis, Missouri, USA). Affymetrix library files included all available reference files related to MoGene-2_1-st. To determine differentially expressed genes, an analysis of variance (ANOVA) was conducted with contrasts. Gene lists were generated by applying a cutoff by Benjamini-Hochberg False Discovery Rate (FDR < 0.05)33,34.
qRT-PCR
E15.5 brains were snap frozen in liquid nitrogen and subsequently processed for gene expression analysis. Whole brains were homogenized and then RNA was extracted utilizing the RNeasy Lipid Tissue Kit (Qiagen), following the manufacturer instructions. First strand cDNA was then generated using the GoScript reverse transcription kit (Promega, Fitchburg, WI, USA). PCR reactions were conducted with SYBR Green on a Light Cycler 480 II system (both from Roche, Indianapolis, IN, USA). Reactions were performed in triplicate for each gene sample using the following conditions: 95 °C × 5 min, then 40 cycles at 95 °C × 10 s, 60 °C ×10 s, and 72 °C × 10 s. The relative expression of each respective target was calculated by ΔCt, normalizing to ribosomal protein 18 s35,36. Primer sequences for Foxd1 were generated using NCBI primer-BLAST37. With exceptions to 18 s and Foxd1, the majority of primers sequences were generated by the Harvard PrimerBank38. Primer sequences are detailed in Supplementary Table S1.
Histology
Sagittal sections from whole embryos placed in formalin or OCT were cut 8 µm thick. Formalin fixed paraffin embedded sections were cleared and used for Iba1 immunohistochemical staining. Antigen retrieval was performed using citrate buffer pH 6.0 (Vector Laboratories, Burlingame, CA, USA) for 25 min at 95 °C. Slides were blocked with biotin/streptavidin (Vector Laboratories) in accordance with the manufacturer’s instructions and then with 2.5% Horse serum (Vector Laboratories) for 1 h. Washes were performed with PBS + 0.05% Tween 20 and a polyclonal goat anti-Iba1 (Abcam ab107159, Burlingame, CA, USA) was added at 1:1000 overnight at 4 °C in PBS + 0.05% Tween 20 with 1% BSA. The next day, an anti-goat pre-diluted ready to use secondary (Vector Laboratories) was applied for 1 h, followed by DAB staining. Slides were counterstained with hematoxylin and Iba1+ cells were quantified within 20× fields of fetal brains using the ImageJ cell counter application. The mean number of Iba1+ cells was calculated relative to the dimensional area of our microscopes 20× objective (358 mm2). Paraffin slides were also cleared and stained with hematoxylin and eosin (H&E) to visualize pathology. The frequency of cerebral hemorrhage was counted, either present or absent from at least three fields for each brain39. Frozen slides were examined under fluorescence to identify GFP and tdTomato reporters. Sections were stained for GFP to enhance the signal40. For this a polyclonal chicken anti-GFP (Abcam ab13970) was added at 1:1000 for 1 h, followed by a donkey anti-chicken secondary conjugated to Alexa Fluor 488 (Jackson ImmunoResearch, West Grove, PA, USA), also at 1:1000 for 1 h. Tissues were counterstained with DAPI and biotinylated BS1 (Vector Laboratories) at 1:500 for 1 h and followed by streptavidin Alexa Fluor 647 (Jackson ImmunoResearch) at 1:1000 for 1 h. All images were captured on a Leica (Buffalo Grove, IL, USA) SP8 system with DFC7000 camera. The brightness and contrast for fluorescent images were adjusted evenly between experimental and control samples to reduce background.
Statistics
With exception to the aforementioned microarray analysis, gene expression comparisons were accomplished with either unpaired Student’s t-test or one-way ANOVA with and without Tukey’s post-hoc test. Categorical data (Figs. 5, 6) was analyzed by chi-squared test using the PBS or PBS + MgSO4/BMTZ control groups as the expected reference. These comparisons were conducted using either Excel (Microsoft, Redmond, WA, USA) or SPSS (IBM, Armonk, NY, USA). Graphs and tables were generated using Excel.
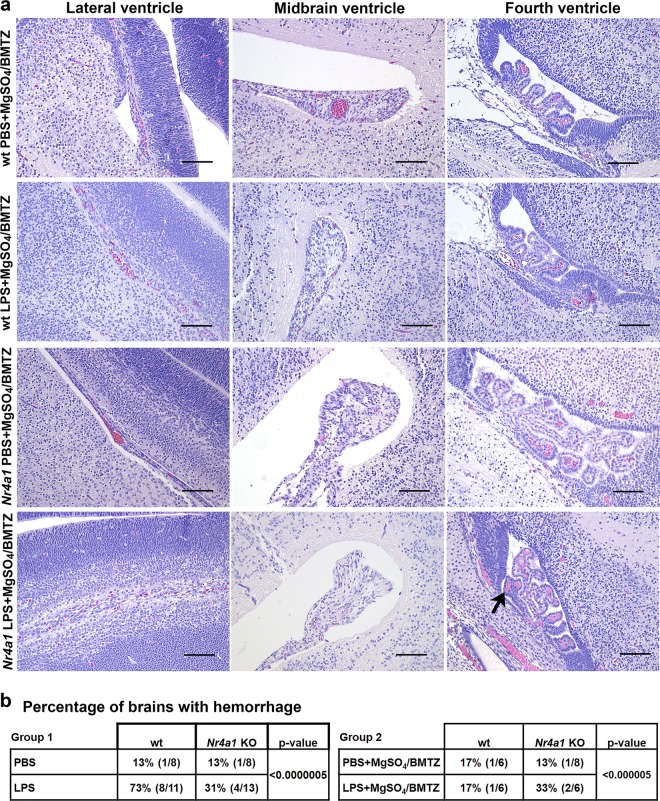
Fig. 5. Reductions of cerebral pathology in Nr4a1 KO embryos.
a Representative micrographs of hemorrhage (arrow), in respective areas for group 2 (PBS vs. LPS with MgSO4/BMTZ). Scale bars denote 100 µm. b The frequency of cerebral hemorrhage observed per condition for groups 1 and 2. The number of brains with hemorrhage vs. total examined is indicated in the brackets to the right of the percentages. P-values were generated by chi-squared test using the PBS or PBS + MgSO4/BMTZ controls as a reference.
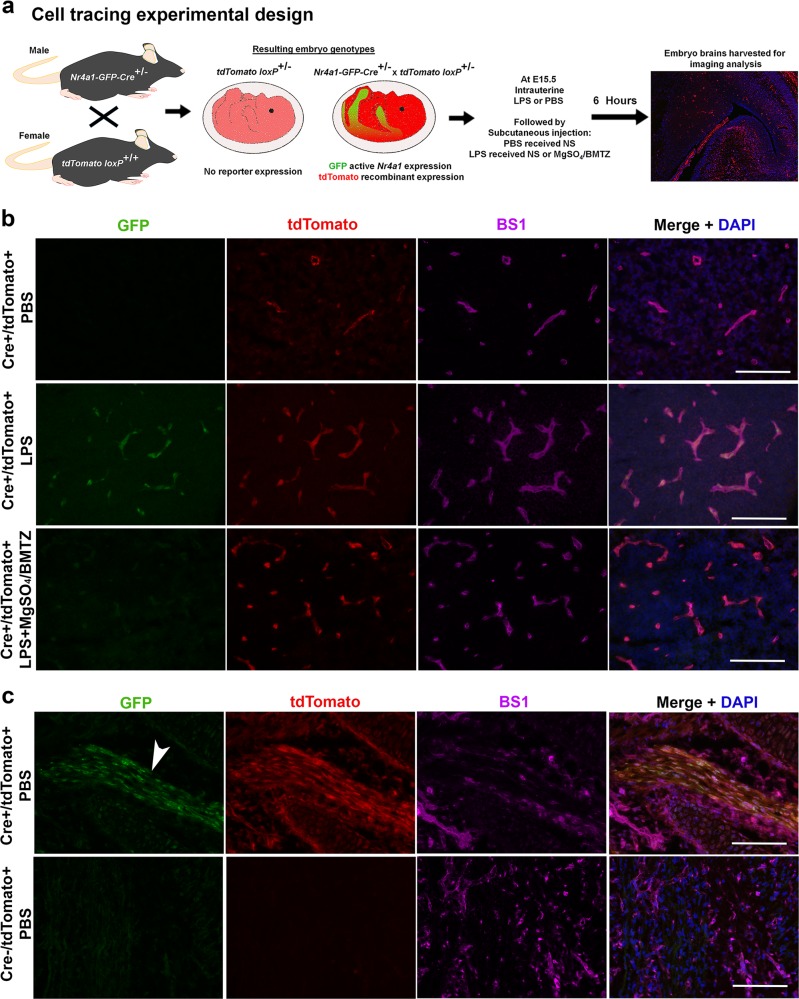
Fig. 6. Fate mapping Nr4a1 expression with perinatal neuroinflammation.
a Experimental design for combining the Nr4a1-GFP-Cre and tdTomato loxP alleles in E15.5 embryos. Males heterozygous for Nr4a1-GFP-Cre were timed mated with females homozygous for tdTomato loxP to generate embryos that harbor both alleles at a 50% Mendelian frequency. For this comparison, tdTomato loxP mice were given intrauterine PBS and subcutaneous NS, LPS and NS or LPS and MgSO4/BMTZ. Embryo brains were harvested 6 h following injections for fluorescence microscopy. b Representative micrographs for each genotype portraying GFP (green), indicative of real-time Nr4a1 expression, and tdTomato (red), expressed irreversibly following Cre recombination. BS1 (magenta) was used to label the vasculature. Merged images combine all three channels with DAPI (blue). c Positive (skeletal muscle, arrowhead) and negative controls (Cre negative littermates) confirm the specificity of the Cre-loxP combination represented in (a). Scale bars denote 100 µm.
Results
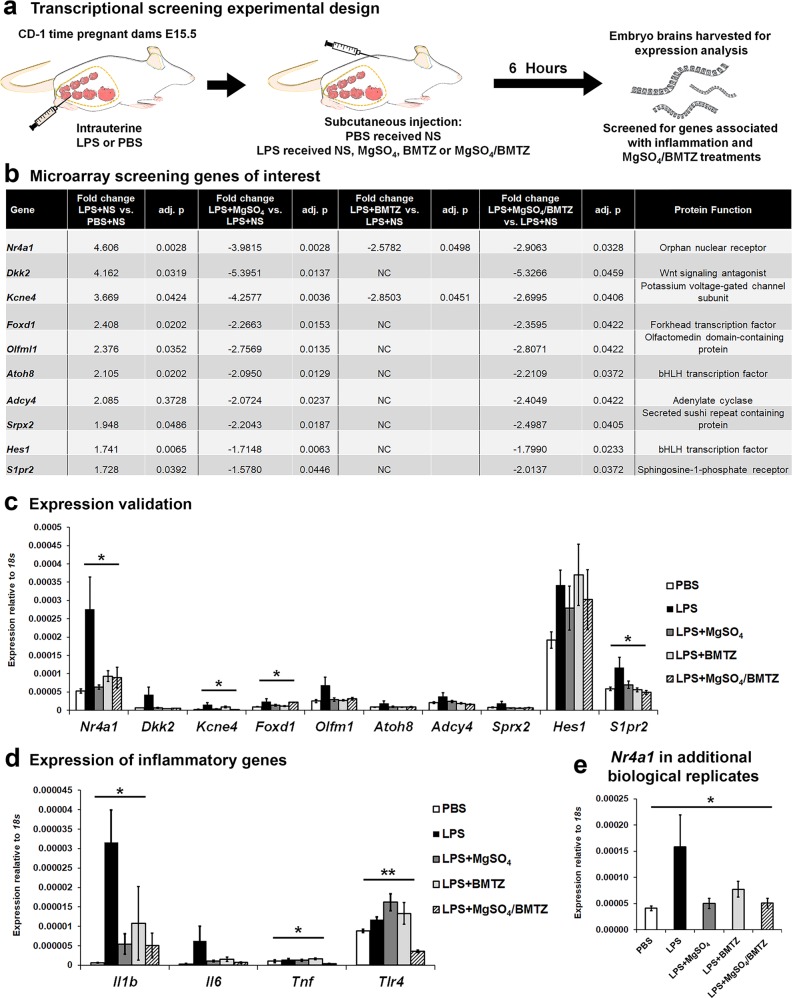
Nr4a1 expression is upregulated with perinatal neuroinflammation
To identify mediators of perinatal brain injury, we utilized microarray analysis to screen for inflammation-associated genes differentially expressed with LPS exposure and modulated by treatment with MgSO4, BMTZ, or the combination of MgSO4/BMTZ (Fig. 1a). The top ten genes upregulated with LPS injections and downregulated with at least one treatment were selected for further validation based on the degree of fold change and adjusted p-value. These genes included transcription factors (Nr4a1, Foxd1, Atoh8, Hes1), regulatory proteins (Dkk2, Olfml1, Srpx2, Kcne4), an enzyme (Adcy4) and a cell surface receptor (S1pr2) (Fig. 1b)41–50. Only Nr4a1, Kcne4, Foxd1, and S1pr2 were significantly higher with LPS and similar to controls with treatments by qRT-PCR (Fig. 1c). The observed changes corresponded with the significant upregulation of proinflammatory genes: Interleukin 1 beta (Il1b), Tumor necrosis factor (Tnf), and Toll-like receptor 4 (Tlr4) (Fig. 1d)26,51. Expression of Interleukin 6 (Il6) was also elevated with LPS, although not significantly. In comparison to LPS alone, treatment with any combination of MgSO4 and/or BMTZ resulted in lower expression of these inflammatory factors. Interestingly, we observed an increase of Tlr4 with LPS and either treatment administered individually. With the treatment combination, the expression of Tlr4 was similar to PBS controls. From this screening and validation, we identified Nr4a1 as the most prominent gene modulated by LPS and treatments. Validation in additional samples supported this result (Fig. 1e).
Fig. 1. Screening for inflammatory regulators reveals the upregulation of Nr4a1.
a CD-1 dams were randomized to receive an intrauterine injection of LPS or PBS at E15.5. Dams given LPS were randomized to receive subcutaneous injections of a combination of MgSO4 and/or BMTZ or the normal saline (NS) vehicle control. Mice that received PBS received NS. Brains were harvested for gene expression analysis 6 h following intrauterine injections. b The top genes upregulated with LPS and downregulated with treatment. Fold changes represent genes upregulated with LPS+NS groups vs. PBS+NS controls (column 2) and downregulated in LPS groups with MgSO4 (column 4), BMTZ (column 6), or the combination of MgSO4/BMTZ (column 8). Column 10 denotes a description of each gene. NC denotes no change. This comparison represents N = 4 embryo brains per condition, analyzed by microarray. c Validation by qRT-PCR in the same samples used for microarray analysis in b. d Expression of key inflammatory genes (Il1b, Il6, Tnf and Tlr4) by qRT-PCR, in the same samples assayed in b. e Additional embryo brains (total N = 8–9 per group) analyzed by qRT-PCR to confirm the upregulation of Nr4a1. *p < 0.05 and **p < 0.005 by one-way ANOVA. Error bars represent ±SEM.
Nr4a1 KO mice show significant reductions in perinatal neuroinflammation and injury
In order to assess whether Nr4a1 regulates perinatal neuroinflammatory injury, we compared KO mice versus wt controls. Second, we compared LPS injury in wt and KO mice with the administration of MgSO4 and BMTZ to evaluate if the protective effects of these treatments are related to Nr4a1. The therapies of both MgSO4 and BMTZ were chosen due to their effectiveness when given in combination versus individual administration (Fig. 1d, e). These experiments were split into two groups, one evaluating LPS alone and a second comparing treatments. Group 1 consisted of wt and Nr4a1 KO mice that received only LPS or PBS. Group 2 consisted of wt and Nr4a1 KO mice that received LPS or PBS and MgSO4/BMTZ treatment (Fig. 2a). Although MgSO4 and BMTZ are relatively safe, their administration in PBS controls was included to account for any effects that may occur in mutant mice.
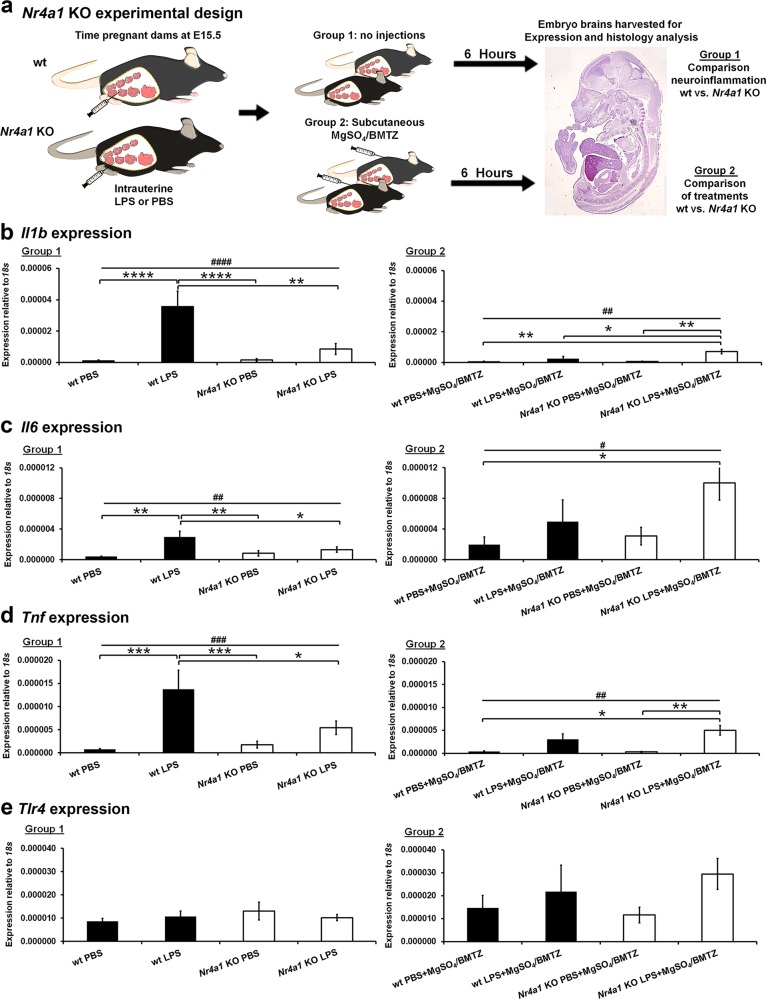
Fig. 2. Examination of perinatal inflammation in the absence of Nr4a1.
a Experimental design comparing wild type (wt) and Nr4a1 knockout (KO) dams exposed to perinatal neuroinflammation at E15.5. Two groups of animals were evaluated; one comparing only PBS vs. LPS and a second comparing PBS vs. LPS with subsequent treatments of MgSO4/BMTZ. Embryo brains were harvested for molecular analysis, at 6 h following intrauterine injections of PBS or LPS. b–e Expression analysis for principal inflammatory genes Il1b, Il6, Tnf, and Tlr4 was examined in E15.5 brains. This analyses represents per condition N = 13–17 brains for group 1 and N = 7–12 brains for group 2. #p < 0.05, ##p < 0.005, ###p < 0.0005 by one-way ANOVA and *p < 0.05, **p < 0.005, ***p < 0.0005, ****p < 0.00005 by Tukey’s post-hoc test. Error bars represent ± SEM.
Once more, to evaluate the perinatal neuroinflammatory response to LPS we examined the expression of Il1b, Il6, Tnf, and Tlr4 (Fig. 2b). Gene expression analysis by qRT-PCR revealed a robust upregulation of cytokines in wt versus Nr4a1 KO fetal brains with LPS. The expression of Il1b, Il6, and Tnf in the wt brains was significantly elevated in the LPS group as compared to the PBS control (Fig. 2b, d, Group 1). In the Nr4a1 KO brains, the expression of these cytokines was similar between PBS and LPS exposed animals. With the addition of MgSO4/BMTZ treatment, the wt inflammatory response was significantly lower than with LPS alone (Fig. 2b, d, Group 2). In contrast, the Nr4a1 KO mice exposed to LPS showed greater expression of Il1b with LPS in comparison to PBS controls versus wt brains. Expression of Il6 and Tnf cytokines was also higher in Nr4a1 KO brains exposed to LPS and MgSO4/BMTZ, but only between certain treatment groups (Fig. 2c, d, Group 2).
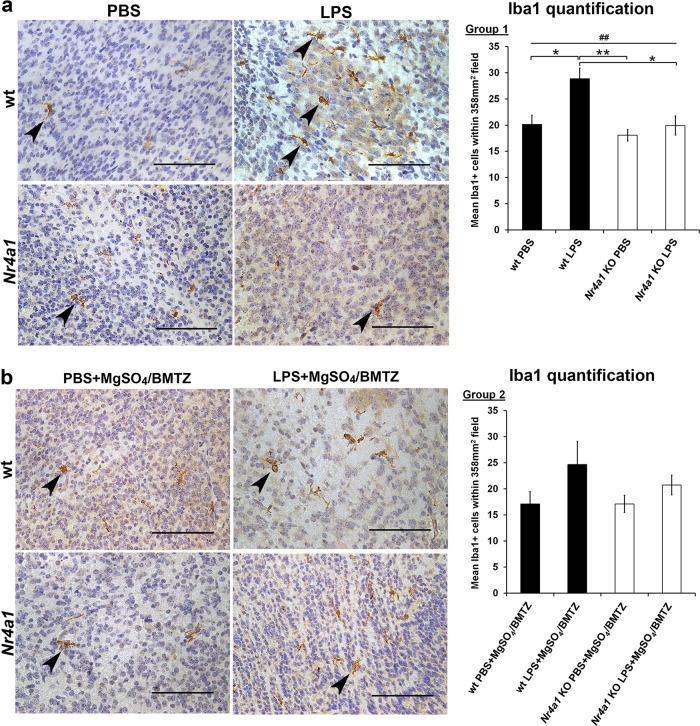
In addition to gene expression, we also compared the cellular response to neuroinflammation by quantifying the number of Iba1+ microglia. With LPS, a greater number of Iba1+ cells was observed in wt embryo brains (Fig. 3a)52,53. No difference was observed in the brains of Nr4a1 KO embryos with PBS or LPS exposure. With MgSO4/BMTZ treatment, the number of Iba1+ cells in wt brains was higher but not significantly with LPS vs. PBS controls (Fig. 3b). There was also no significant difference in Nr4a1 KO brains with MgSO4/BMTZ treatment.
Fig. 3. Microglial comparison between wt and Nr4a1 KO embryos.
E.15.5 brains from wt and Nr4a1 KO embryos were stained for Iba1 with DAB (brown). Sections were counterstained with hematoxylin to visualize nuclei in blue and high magnification micrographs (40×) depict Iba1+ microglia (arrowheads) between conditions. Cell quantifications graphed to the right were conducted at a lower magnification (20×) in order to reduce error. a Comparison and quantification of Iba1+ cells for group 1 (N = 6 brains per condition); wt and Nr4a1 KO animals were exposed to PBS or LPS. b Comparison and quantification for group 2 (N = 3 brains per condition); wt and Nr4a1 KO animals were exposed to PBS or LPS and MgSO4/BMTZ treatment. Scale bars denote 100 µm. ##p < 0.005 by one-way ANOVA and *p < 0.05, **p < 0.005, by Tukey’s post-hoc test. Error bars represent ± SEM.
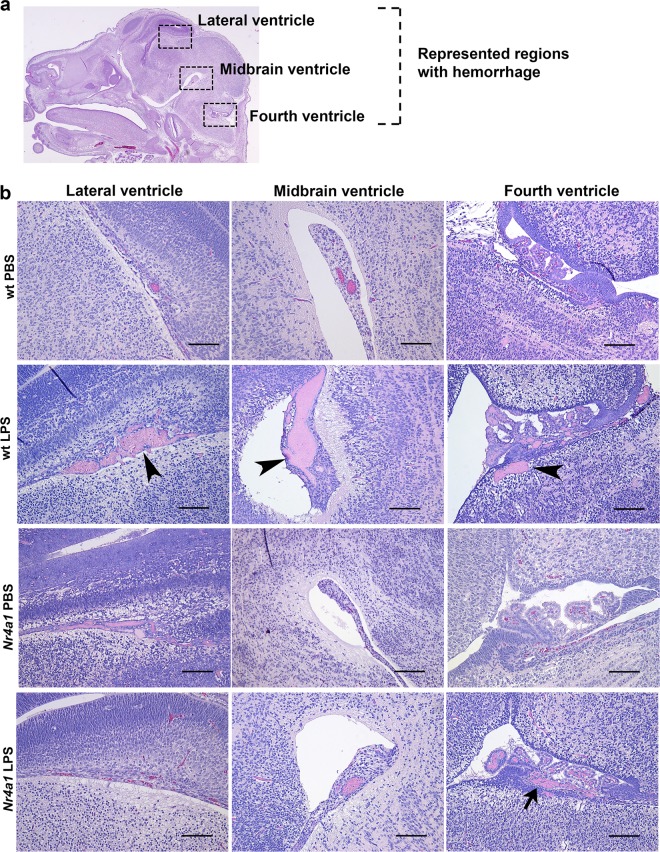
To gain more insight into the role of Nr4a1 in perinatal brain injury, we examined the histopathology in wt versus mutant embryo brains. Most obvious was cerebral hemorrhage, occurring predominantly in the lateral ventricle, midbrain, and fourth ventricle (Fig. 4a). This pathology was more pronounced in wt animals exposed to LPS in comparison to PBS controls and Nr4a1 KO brains (Fig. 4b). The frequency of hemorrhage in wt mice exposed to LPS diminished with MgSO4/BMTZ treatment (Fig. 5a). The frequency of hemorrhage was also significantly different between wt and mutant animals in both Groups 1 and 2 (Fig. 5b). Notably, the incidence of hemorrhage in Nr4a1 KO brains exposed to LPS and MgSO4/BMTZ was greater versus wt counterparts and similar to mutant mice that received only LPS.
Fig. 4. Comparison of cerebral pathology observed in wt and Nr4a1 KO embryos.
a H&E stained cross-section of an E15.5 brain, highlighting the regions (boxed areas) where injury in the form of hemorrhage was mainly observed. b Representative micrographs of hemorrhage in the respective areas described in a for group 1 (PBS vs. LPS). Hemorrhage was predominant in wt brains exposed to LPS (arrowheads) and to a lesser extent in Nr4a1 KO brains also exposed to LPS (arrow). Scale bars denote 100 µm.
Nr4a1 is upregulated by cerebral endothelial cells in response to neuroinflammation
To characterize the cellular expression of Nr4a1, we utilized Cre-loxP fate mapping with the Nr4a1-GFP-Cre model. In addition to Cre, this allele expresses GFP as an indicator of active Nr4a1 expression. To compare GFP and Cre labeling, tdTomato loxP females were mated with Nr4a1-GFP-Cre males and given intrauterine PBS, LPS or LPS and MgSO4/BMTZ at E15.5 (Fig. 6a). In brains of PBS controls, we observed tdTomato localized to the vasculature (Fig. 6b). LPS exposed animals had tdTomato and GFP, both appearing localized to the cerebral vasculature. Analogous to PBS controls, we observed only tdTomato in brains exposed to LPS and MgSO4/BMTZ. Staining with the lectin BS1 confirmed that GFP and tdTomato reporters localized to the vasculature31. Both GFP and tdTomato reporters were present in the developing skeletal muscle (Fig. 6c), corresponding to the known expression of Nr4a1 in myoblasts54. Concurrently, fluorescence for either reporter was absent in littermates negative for the Nr4a1-GFP-Cre allele.
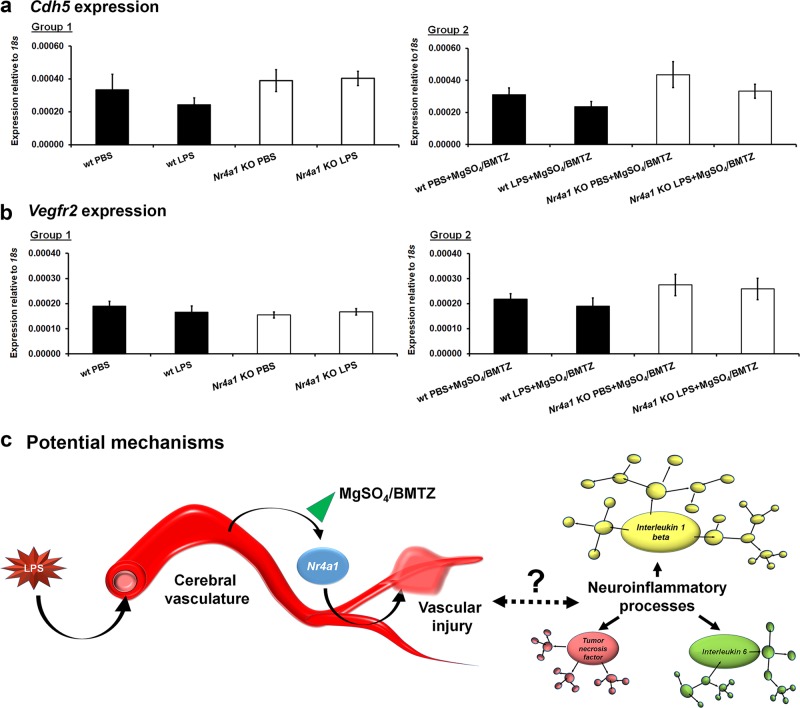
Based on the pattern of cellular expression we examined Nr4a1 KO versus wt brains (same samples used in Fig. 2) for differences in vascular genes, Cdhr5 and Vegfr2. Both genes are important for endothelial integrity and angiogenesis. Therefore a difference from PBS controls may reflect intrinsic differences in vascular development that may influence the outcomes observed in Nr4a1 KO brains with LPS exposure55,56. Secondarily, we sought to gain more insight into possible declines in endothelial cell integrity or number that may also occur with LPS. Expression analysis indicates no such differences even with MgSO4/BMTZ (Fig. 7a, b).
Fig. 7. Vascular gene expression in Nr4a1 KO embryos and summary of findings.
Embryonic brains from Fig. 2 were evaluated for the expression of a Cdh5 and b Vegfr2. No statistical significance by was noted by one-way ANOVA between wt and Nr4a1 KO animals or with MgSO4/BMTZ treatment. Error bars represent ±SEM. c Through undetermined interactions the expression of Nr4a1 with perinatal neuroinflammation results in vascular injury (hemorrhage). In turn, the neuroinflammatory process is activated directly or indirectly, as indicated by the upregulation of principal cytokines Il1b, Il6, and Tnf. This process appears blunted by MgSO4/BMTZ, which may be related to Nr4a1 suppression.
Discussion
We found that Nr4a1 is upregulated with neuroinflammation in a murine model of preterm labor. Treatments with MgSO4/BMTZ mitigated this response in wt animals. In contrast, Nr4a1 KO animals showed a reduction in neuroinflammation and brain injury. MgSO4/BMTZ did not alter inflammatory responses in mutant animals. Finally, using Cre-loxP fate mapping, we were able to identify that the inflammatory upregulation of Nr4a1 occurs in the vasculature of the fetal brain.
With normal brain development, Nr4a1 is limited or absent according to several lines of evidence21,22. In situ hybridization of fetal mouse brains show an absence of Nr4a1 until E18.5 (© 2015 Allen Institute for Brain Science, Allen Brain Atlas API; available from: http://developingmouse.brain-map.org/gene/show/15145). Within the context of preterm birth, Nr4a1 is upregulated with lung inflammation in premature sheep57. In addition, microarray analysis of fetal rat brains 4 h following LPS exposure reveals an increase of Nr4a1 expression (GEO accession GDS4429)23. This coincides with the significant increase of Nr4a1 that we observed at 6 h following LPS. Based on this pattern of upregulation with insult, downregulation with MgSO4/BMTZ treatments, and limited presence in brain development, we reasoned that Nr4a1 warranted further investigation. We took a genetic approach and used an established mutant mouse model with no known developmental phenotype22. The lack of differences between PBS controls (Figs. 2–5, 7a, b) support the notion that Nr4a1 ablation does not influence normal development. However, with the addition of an inflammatory instigator there are significant changes that may cause neurodevelopmental deficiencies noted in postnatal animals36.
Our study suggest Nr4a1 plays a prominent role in perinatal neuroinflammation and brain injury. Conversely, Nr4a1 has been implicated in both anti- and pro-inflammatory processes. Within the adult innate immune system and with metabolic disease, Nr4a1 plays an anti-inflammatory role58,59. The mechanisms by which Nr4a1 reduces inflammation have been noted to involve p38, NF-kB, and ISG12 depending on the context of disease, biological modeling, and analyses19,60,61. In- depth molecular examination suggests p38 counters Nr4a1 in suppressing NF-kB pro-inflammatory signaling19. Whereas comparisons of animal models reveals Nr4a1 deficient mutants exhibit greater inflammation in response to sepsis and higher mortality versus Isg12 deficient animals61. In the adult CNS, Nr4a1 is broadly expressed in brain tissue and involved in regulatory functions, specifically in microglia. In contrast to our results in embryonic brains, adult Nr4a1 KO mice show elevated autoimmune inflammatory responses by microglia and T-cells62–64.
In addition to the anti-inflammatory responses, there are numerous biological processes whereby Nr4a1 is pro-inflammatory. Nr4a receptors are expressed in several immune cells to include activated macrophages20. Within the context of LPS stimulation, Nr4a1 can also promote macrophage NF-kB signaling65. Other studies have indicated that Nr4a1 does not alter immune cell responses but instead antagonizes endothelial responses to inflammation66. In regards to the CNS, Nr4a1 has been implicated in adult brain injury to promote neuroinflammation and cell death17,18. Although these studies did not link the cerebral vasculature to Nr4a1 signaling, it is important to note that trauma was modeled by inducing subarachnoid hemorrhage. In regard to a role within the vasculature, various modalities have implicated Nr4a1 in regulating endothelial cell inflammation, leakiness, permeability and dysfunction40,66–68. Such studies reinforce that Nr4a1 is dispensable for homeostasis but is important in a pathological state. This pattern of Nr4a1 necessity makes it an ideal target for disease, since ablation in normal processes may not result in deleterious side effects.
In this study, the absence of Nr4a1 in KO mice resulted in a significant reduction of principal pro-inflammatory markers in the E15.5 pup brains. This evidence provides a basis for the role of Nr4a1 in regulating bacteria initiated perinatal neuroinflammation. It is possible that Nr4a1 promotes an increase in cytokine expression from an inflammatory insult, as displayed by the effect of LPS in the wt mice. In comparing the LPS treatment groups of the wt and the Nr4a1 KO, the treatment of MgSO4/BMTZ did not appear to decrease the level of inflammatory cytokine expression. This may be explained by a potential mechanism related to Nr4a1 signaling that is essential for the neuroprotective actions of MgSO4/BMTZ. Alternatively, in Nr4a1 KO animals inflammation may be reduced to a threshold whereby the treatments are no longer effective. We additionally recognize that by using MgSO4/BMTZ in combination (a clinically relevant approach), our results cannot be attributed to one of the two medications.
The upregulation of pro-inflammatory genes with LPS exposure corresponds with a greater number of microglia in wt brains. Treatment with MgSO4/BMTZ mitigated the increase of microglia in wt embryos that was observed with LPS alone. In mutant embryos exposed to LPS, the number of microglia did not elevate or correlate with increases in pro-inflammatory gene expression. In response to inflammatory stimuli such as LPS, microglia produce cytokines including IL-1β69. It is possible that the microglial inflammatory response is restricted in mutant embryos, resulting in significantly lower levels of cytokine expression vs. wt animals. Alternatively, other cell population’s upregulate cytokines independent of the mutant status but to a limited degree as compared to microglia.
To further characterize the role of Nr4a1 in perinatal brain injury, we examined the histopathology of the embryo brains. Cerebral hemorrhage was notable in wt versus Nr4a1 KO brains with LPS. MgSO4/BMTZ mitigated the frequency of hemorrhage in wt brains but had no effect in KO animals. These results correspond with the pathological findings in humans, whereby the incidence of intraventricular hemorrhage is greater with prematurity and reduced by corticosteroids70–72. The mechanisms of perinatal hemorrhage within the context of preterm labor are not clear. Our examination of key vascular genes suggests that cerebral hemorrhage is not a result of endothelial cell decline (Fig. 7a, b). Both MgSO4 and corticosteroids are known to relax the vasculature73,74. However, it is unclear whether vasodilation or other responses invoked by MgSO4 and/or BMTZ confer neuroprotection. Our results suggest a possible role of Nr4a1 with regard to MgSO4/BMTZ and the cerebral vasculature. This is supported by the upregulation of Nr4a1 in vessels observed with Cre-loxP fate mapping.
Whether Nr4a1 signaling directly or indirectly influences the perinatal inflammatory response remains a question. Given that Nr4a1 is expressed in the vasculature, we suspect that it is mediating inflammation as summarized in Fig. 7c. One of the principal inflammatory markers, Il1b, was intimately affected by the knockout status and the treatment group. This suggests that Il1b expression is modulated by Nr4a1. However, it is unclear whether the upregulation of inflammatory cytokines by Nr4a1 is direct or indirect. Vascular cells are known to express interleukin receptors and respond to inflammatory cytokines75. Therefore, it is likely that perinatal vascular cells interact with immune cells, but are not the main source of inflammatory cytokines.
Our study’s strengths include the use of multiple murine models including outbred CD1, inbred C57BL/6 and Nr4a1 KO mice, to support our findings. Furthermore, several assays and validation experiments were conducted including the use of Cre-loxP mutants that not only substantiated the upregulation of Nr4a1 with neuroinflammation but also implicated the vasculature. Finally, the comparison of MgSO4/BMTZ provides additional insight into the mechanisms of neuroprotection and the role of Nr4a1.
The primary limitation of our study is the reliance on a mouse model of preterm labor. The mechanisms of preterm labor in humans are complex and difficult to translate. Therefore, we used an inflammation-based model which has been well described in the literature. Although other exposure modalities using live bacteria exist, we used the in utero LPS approach to examine specific inflammatory components of brain injury to evaluate potential mechanisms of MgSO4/BMTZ neuroprotection2,51,76.
A second limitation is the use of the microarray only for screening genes but not for functional analysis. This is due to the low number of genes that were validated; only four of our top ten were significant by qRT-PCR (Fig. 1c). Based on the high level of false positives, we deemed the microarray unsuitable for making interpretations regarding the status of the transcriptome.
A third limitation is that we could not establish a clear link between Nr4a1 and its mechanism of action. We suspect that the mechanisms of Nr4a1 are directly related to the vasculature and the pathology of hemorrhage. However, we could not pinpoint the role of Nr4a1 to specific pathways within the neuroinflammatory milieu. We observed that Nr4a1 is re-expressed in the context of neuroinflammation but the exact timing and reason for expression earlier in development also remain unclear. Finally, the etiology of preterm labor in humans is multifactorial and our observations may represent only one of many pathways that govern neuroinflammation and/or MgSO4/BMTZ neuroprotection77.
In closing, we have identified Nr4a1 as a potent mediator of perinatal neuroinflammation and direct or indirect target of MgSO4/BMTZ treatments. Nr4a1 expression was upregulated in the fetal brain vasculature and linked to cerebral hemorrhage. The lack of Nr4a1 in normal brains presents an opportunity to target neuroinflammation, potentially with few developmental side effects. Based on these findings, additional studies are warranted to better understand the role of the vasculature and Nr4a1 signaling within the context of preterm labor.
Supplementary information
Acknowledgements
Funding for this research was provided by the U.S. Air Force SG5 award program and by Madigan Army Medical Center. We are also grateful for the support from the Madigan Laboratory Animal Resource Service, in particular by Joanna Dandeneau.
Competing interests
Authors S.M.E., A.S.T., P.G.N., and N.I. have filed a provisional patent related to the targeting of Nr4a1 for reducing neuroinflammation with preterm labor. The authors have not received any monetary benefits for this filing or have any conflicts of interest regarding this research study to declare. Funding agencies had no influence on the bearing of this study.
Disclaimer
Some authors are federal employees or members of the armed forces. The views expressed are those of the authors and do not reflect the official policy or position of the U.S. Army Medical Department, Department of the Army, Department of Defense or the U.S. Government. Animals involved in this study were maintained in accordance with the ‘Guide for the Care and Use of Laboratory Animals’ published by the National Research Council/Institute of Laboratory Animal Research (ILAR).
Footnotes
Edited by B. Joseph
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information accompanies this paper at (10.1038/s41419-019-2196-7).
References
- 1.Martin, J. A. & Osterman, M. J. K. Describing the Increase in Preterm Births in the United States, 2014–2016. NCHS Data Brief, 1–8 (2018). [PubMed]
- 2.Burd I, Balakrishnan B, Kannan S. Models of fetal brain injury, intrauterine inflammation, and preterm birth. Am. J. Reprod. Immunol. 2012;67:287–294. doi: 10.1111/j.1600-0897.2012.01110.x. [DOI] [PubMed] [Google Scholar]
- 3.Yoon BH, et al. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am. J. Obstet. Gynecol. 2000;182:675–681. doi: 10.1067/mob.2000.104207. [DOI] [PubMed] [Google Scholar]
- 4.Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR. Neurologic and developmental disability after extremely preterm birth. EPICure Study Group. N. Engl. J. Med. 2000;343:378–384. doi: 10.1056/NEJM200008103430601. [DOI] [PubMed] [Google Scholar]
- 5.Marlow N, Wolke D, Bracewell MA, Samara M, Group EPS. Neurologic and developmental disability at six years of age after extremely preterm birth. N. Engl. J. Med. 2005;352:9–19. doi: 10.1056/NEJMoa041367. [DOI] [PubMed] [Google Scholar]
- 6.Pierre WC, et al. Neonatal microglia: the cornerstone of brain fate. Brain, Behav., Immun. 2017;59:333–345. doi: 10.1016/j.bbi.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 7.Rouse DJ, et al. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N. Engl. J. Med. 2008;359:895–905. doi: 10.1056/NEJMoa0801187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rouse DJ, Hirtz D. Eunice Kennedy Shriver National Institute of Child, H. & Human Development Maternal-Fetal Medicine Units, N. What we learned about the role of antenatal magnesium sulfate for the prevention of cerebral palsy. Semin. Perinatol. 2016;40:303–306. doi: 10.1053/j.semperi.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crowther CA, Hiller JE, Doyle LW, Haslam RR, Australasian Collaborative Trial of Magnesium Sulphate Collaborative, G. Effect of magnesium sulfate given for neuroprotection before preterm birth: a randomized controlled trial. JAMA. 2003;290:2669–2676. doi: 10.1001/jama.290.20.2669. [DOI] [PubMed] [Google Scholar]
- 10.Marret S, et al. Magnesium sulphate given before very-preterm birth to protect infant brain: the randomised controlled PREMAG trial*. BJOG. 2007;114:310–318. doi: 10.1111/j.1471-0528.2006.01162.x. [DOI] [PubMed] [Google Scholar]
- 11.Mittendorf R, et al. Association between the use of antenatal magnesium sulfate in preterm labor and adverse health outcomes in infants. Am. J. Obstet. Gynecol. 2002;186:1111–1118. doi: 10.1067/mob.2002.123544. [DOI] [PubMed] [Google Scholar]
- 12.Conde-Agudelo A, Romero R. Antenatal magnesium sulfate for the prevention of cerebral palsy in preterm infants less than 34 weeks' gestation: a systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2009;200:595–609. doi: 10.1016/j.ajog.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Costantine, M. M. & Weiner, S. J. Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Effects of antenatal exposure to magnesium sulfate on neuroprotection and mortality in preterm infants: a meta-analysis. Obstet. Gynecol.114, 354–364 (2009). [DOI] [PMC free article] [PubMed]
- 14.Baud O, et al. Antenatal glucocorticoid treatment and cystic periventricular leukomalacia in very premature infants. N. Engl. J. Med. 1999;341:1190–1196. doi: 10.1056/NEJM199910143411604. [DOI] [PubMed] [Google Scholar]
- 15.Crowley P, Chalmers I, Keirse MJ. The effects of corticosteroid administration before preterm delivery: an overview of the evidence from controlled trials. Br. J. Obstet. Gynaecol. 1990;97:11–25. doi: 10.1111/j.1471-0528.1990.tb01711.x. [DOI] [PubMed] [Google Scholar]
- 16.Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol. Cell. Endocrinol. 2011;335:2–13. doi: 10.1016/j.mce.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dai Y, et al. Cyclosporin A ameliorates early brain injury after subarachnoid hemorrhage through inhibition of a Nur77 dependent apoptosis pathway. Brain Res. 2014;1556:67–76. doi: 10.1016/j.brainres.2014.01.052. [DOI] [PubMed] [Google Scholar]
- 18.Dai Y, et al. Nuclear receptor nur77 promotes cerebral cell apoptosis and induces early brain injury after experimental subarachnoid hemorrhage in rats. J. Neurosci. Res. 2014;92:1110–1121. doi: 10.1002/jnr.23392. [DOI] [PubMed] [Google Scholar]
- 19.Li L, et al. Impeding the interaction between Nur77 and p38 reduces LPS-induced inflammation. Nat. Chem. Biol. 2015;11:339–346. doi: 10.1038/nchembio.1788. [DOI] [PubMed] [Google Scholar]
- 20.Pei L, Castrillo A, Chen M, Hoffmann A, Tontonoz P. Induction of NR4A orphan nuclear receptor expression in macrophages in response to inflammatory stimuli. J. Biol. Chem. 2005;280:29256–29262. doi: 10.1074/jbc.M502606200. [DOI] [PubMed] [Google Scholar]
- 21.Zetterstrom RH, Williams R, Perlmann T, Olson L. Cellular expression of the immediate early transcription factors Nurr1 and NGFI-B suggests a gene regulatory role in several brain regions including the nigrostriatal dopamine system. Brain Res. Mol. Brain Res. 1996;41:111–120. doi: 10.1016/0169-328X(96)00074-5. [DOI] [PubMed] [Google Scholar]
- 22.Lee SL, et al. Unimpaired thymic and peripheral T cell death in mice lacking the nuclear receptor NGFI-B (Nur77) Science. 1995;269:532–535. doi: 10.1126/science.7624775. [DOI] [PubMed] [Google Scholar]
- 23.Oskvig DB, Elkahloun AG, Johnson KR, Phillips TM, Herkenham M. Maternal immune activation by LPS selectively alters specific gene expression profiles of interneuron migration and oxidative stress in the fetus without triggering a fetal immune response. Brain, Behav., Immun. 2012;26:623–634. doi: 10.1016/j.bbi.2012.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elovitz MA, Wang Z, Chien EK, Rychlik DF, Phillippe M. A new model for inflammation-induced preterm birth: the role of platelet-activating factor and Toll-like receptor-4. Am. J. Pathol. 2003;163:2103–2111. doi: 10.1016/S0002-9440(10)63567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hallak M. Effect of parenteral magnesium sulfate administration on excitatory amino acid receptors in the rat brain. Magnes. Res. 1998;11:117–131. [PubMed] [Google Scholar]
- 26.Burd I, Breen K, Friedman A, Chai J, Elovitz MA. Magnesium sulfate reduces inflammation-associated brain injury in fetal mice. Am. J. Obstet. Gynecol. 2010;202:292 e291–299. doi: 10.1016/j.ajog.2010.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nadeau-Vallee M, et al. Novel noncompetitive IL-1 receptor-biased ligand prevents infection- and inflammation-induced preterm birth. J. Immunol. 2015;195:3402–3415. doi: 10.4049/jimmunol.1500758. [DOI] [PubMed] [Google Scholar]
- 28.Wang X, et al. Disruption of interleukin-18, but not interleukin-1, increases vulnerability to preterm delivery and fetal mortality after intrauterine inflammation. Am. J. Pathol. 2006;169:967–976. doi: 10.2353/ajpath.2006.050207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moran AE, et al. T cell receptor signal strength in Treg and iNKT cell development demonstrated by a novel fluorescent reporter mouse. J. Exp. Med. 2011;208:1279–1289. doi: 10.1084/jem.20110308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Madisen L, et al. A robust and high-throughput Cre reporting and characterization system for the whole mouse brain. Nat. Neurosci. 2010;13:133–140. doi: 10.1038/nn.2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ieronimakis N, et al. Coronary adventitial cells are linked to perivascular cardiac fibrosis via TGFbeta1 signaling in the mdx mouse model of Duchenne muscular dystrophy. J. Mol. Cell. Cardiol. 2013;63:122–134. doi: 10.1016/j.yjmcc.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qu Y, He F, Chen Y. Different effects of the probe summarization algorithms PLIER and RMA on high-level analysis of Affymetrix exon arrays. BMC Bioinforma. 2010;11:211. doi: 10.1186/1471-2105-11-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hochberg Y, Benjamini Y. More powerful procedures for multiple significance testing. Stat. Med. 1990;9:811–818. doi: 10.1002/sim.4780090710. [DOI] [PubMed] [Google Scholar]
- 34.Reiner A, Yekutieli D, Benjamini Y. Identifying differentially expressed genes using false discovery rate controlling procedures. Bioinformatics. 2003;19:368–375. doi: 10.1093/bioinformatics/btf877. [DOI] [PubMed] [Google Scholar]
- 35.Au CG, et al. Increased connective tissue growth factor associated with cardiac fibrosis in the mdx mouse model of dystrophic cardiomyopathy. Int. J. Exp. Pathol. 2011;92:57–65. doi: 10.1111/j.1365-2613.2010.00750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thagard AS, et al. Long-term impact of intrauterine neuroinflammation and treatment with magnesium sulphate and betamethasone: Sex-specific differences in a preterm labor murine model. Sci. Rep. 2017;7:17883. doi: 10.1038/s41598-017-18197-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ye J, et al. Primer-BLAST: a tool to design target-specific primers for polymerase chain reaction. BMC Bioinforma. 2012;13:134. doi: 10.1186/1471-2105-13-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang X, Spandidos A, Wang H, Seed B. PrimerBank: a PCR primer database for quantitative gene expression analysis, 2012 update. Nucleic Acids Res. 2012;40:D1144–1149. doi: 10.1093/nar/gkr1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Winkler DT, et al. Spontaneous hemorrhagic stroke in a mouse model of cerebral amyloid angiopathy. J. Neurosci. 2001;21:1619–1627. doi: 10.1523/JNEUROSCI.21-05-01619.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goddard LM, et al. Progesterone receptor in the vascular endothelium triggers physiological uterine permeability preimplantation. Cell. 2014;156:549–562. doi: 10.1016/j.cell.2013.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martinez-Gonzalez J, Badimon L. The NR4A subfamily of nuclear receptors: new early genes regulated by growth factors in vascular cells. Cardiovascular Res. 2005;65:609–618. doi: 10.1016/j.cardiores.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 42.Quintero-Ronderos P, Laissue P. The multisystemic functions of FOXD1 in development and disease. J. Mol. Med. 2018;96:725–739. doi: 10.1007/s00109-018-1665-2. [DOI] [PubMed] [Google Scholar]
- 43.Chen J, et al. Diversification and molecular evolution of ATOH8, a gene encoding a bHLH transcription factor. PloS ONE. 2011;6:e23005. doi: 10.1371/journal.pone.0023005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kageyama R, Shimojo H, Ohtsuka T. Dynamic control of neural stem cells by bHLH factors. Neurosci. Res. 2019;138:12–18. doi: 10.1016/j.neures.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 45.Krupnik VE, et al. Functional and structural diversity of the human Dickkopf gene family. Gene. 1999;238:301–313. doi: 10.1016/S0378-1119(99)00365-0. [DOI] [PubMed] [Google Scholar]
- 46.Anholt RR. Olfactomedin proteins: central players in development and disease. Front. cell developmental Biol. 2014;2:6. doi: 10.3389/fcell.2014.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sia GM, Clem RL, Huganir RL. The human language-associated gene SRPX2 regulates synapse formation and vocalization in mice. Science. 2013;342:987–991. doi: 10.1126/science.1245079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grunnet M, et al. KCNE4 is an inhibitory subunit to Kv1.1 and Kv1.3 potassium channels. Biophysical J. 2003;85:1525–1537. doi: 10.1016/S0006-3495(03)74585-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rui X, Tsao J, Scheys JO, Hammer GD, Schimmer BP. Contributions of specificity protein-1 and steroidogenic factor 1 to Adcy4 expression in Y1 mouse adrenal cells. Endocrinology. 2008;149:3668–3678. doi: 10.1210/en.2008-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Blaho VA, Hla T. An update on the biology of sphingosine 1-phosphate receptors. J. lipid Res. 2014;55:1596–1608. doi: 10.1194/jlr.R046300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Burd I, et al. Inflammation-induced preterm birth alters neuronal morphology in the mouse fetal brain. J. Neurosci. Res. 2010;88:1872–1881. doi: 10.1002/jnr.22368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lei J, et al. Maternal dendrimer-based therapy for inflammation-induced preterm birth and perinatal brain injury. Sci. Rep. 2017;7:6106. doi: 10.1038/s41598-017-06113-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eloundou SN, et al. Placental malperfusion in response to intrauterine inflammation and its connection to fetal sequelae. PloS one. 2019;14:e0214951. doi: 10.1371/journal.pone.0214951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tontonoz P, et al. The orphan nuclear receptor Nur77 is a determinant of myofiber size and muscle mass in mice. Mol. Cell. Biol. 2015;35:1125–1138. doi: 10.1128/MCB.00715-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vestweber D. VE-cadherin: the major endothelial adhesion molecule controlling cellular junctions and blood vessel formation. Arterioscler Thromb. Vasc. Biol. 2008;28:223–232. doi: 10.1161/ATVBAHA.107.158014. [DOI] [PubMed] [Google Scholar]
- 56.Lafuente JV, Argandona EG, Mitre B. VEGFR-2 expression in brain injury: its distribution related to brain-blood barrier markers. J. Neural Transm. (Vienna) 2006;113:487–496. doi: 10.1007/s00702-005-0407-0. [DOI] [PubMed] [Google Scholar]
- 57.Hillman NH, Kemp MW, Noble PB, Kallapur SG, Jobe AH. Sustained inflation at birth did not protect preterm fetal sheep from lung injury. Am. J. Physiol. Lung Cell. Mol. Physiol. 2013;305:L446–453. doi: 10.1152/ajplung.00162.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hanna RN, et al. NR4A1 (Nur77) deletion polarizes macrophages toward an inflammatory phenotype and increases atherosclerosis. Circ. Res. 2012;110:416–427. doi: 10.1161/CIRCRESAHA.111.253377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Koenis DS, et al. Nuclear receptor Nur77 limits the macrophage inflammatory response through transcriptional reprogramming of mitochondrial. Metab. Cell Rep. 2018;24:2127–2140 e2127. doi: 10.1016/j.celrep.2018.07.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Popichak KA, et al. Compensatory expression of Nur77 and Nurr1 regulates NF-kappaB-dependent inflammatory signaling in astrocytes. Mol. Pharmacol. 2018;94:1174–1186. doi: 10.1124/mol.118.112631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Uhrin P, Perkmann T, Binder B, Schabbauer G. ISG12 is a critical modulator of innate immune responses in murine models of sepsis. Immunobiology. 2013;218:1207–1216. doi: 10.1016/j.imbio.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rothe T, et al. The nuclear receptor Nr4a1 Acts as a Microglia Rheostat and Serves as a Therapeutic Target in Autoimmune-Driven Central Nervous System Inflammation. J. Immunol. 2017;198:3878–3885. doi: 10.4049/jimmunol.1600638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liebmann M, et al. Nur77 serves as a molecular brake of the metabolic switch during T cell activation to restrict autoimmunity. Proc. Natl Acad. Sci. USA. 2018;115:E8017–E8026. doi: 10.1073/pnas.1721049115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shaked I, et al. Transcription factor Nr4a1 couples sympathetic and inflammatory cues in CNS-recruited macrophages to limit neuroinflammation. Nat. Immunol. 2015;16:1228–1234. doi: 10.1038/ni.3321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pei L, Castrillo A, Tontonoz P. Regulation of macrophage inflammatory gene expression by the orphan nuclear receptor Nur77. Mol. Endocrinol. 2006;20:786–794. doi: 10.1210/me.2005-0331. [DOI] [PubMed] [Google Scholar]
- 66.Hamers AA, et al. Limited role of nuclear receptor Nur77 in Escherichia coli-induced peritonitis. Infect. Immun. 2014;82:253–264. doi: 10.1128/IAI.00721-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhou H, et al. NR4A1 aggravates the cardiac microvascular ischemia reperfusion injury through suppressing FUNDC1-mediated mitophagy and promoting Mff-required mitochondrial fission by CK2alpha. Basic Res. Cardiol. 2018;113:23. doi: 10.1007/s00395-018-0682-1. [DOI] [PubMed] [Google Scholar]
- 68.You B, Jiang YY, Chen S, Yan G, Sun J. The orphan nuclear receptor Nur77 suppresses endothelial cell activation through induction of IkappaBalpha expression. Circ. Res. 2009;104:742–749. doi: 10.1161/CIRCRESAHA.108.192286. [DOI] [PubMed] [Google Scholar]
- 69.Cunningham CL, Martinez-Cerdeno V, Noctor SC. Microglia regulate the number of neural precursor cells in the developing cerebral cortex. J. Neurosci. 2013;33:4216–4233. doi: 10.1523/JNEUROSCI.3441-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Canterino JC, et al. Antenatal steroids and neonatal periventricular leukomalacia. Obstet. Gynecol. 2001;97:135–139. doi: 10.1016/s0029-7844(00)01124-8. [DOI] [PubMed] [Google Scholar]
- 71.Canterino JC, et al. Maternal magnesium sulfate and the development of neonatal periventricular leucomalacia and intraventricular hemorrhage. Obstet. Gynecol. 1999;93:396–402. doi: 10.1016/s0029-7844(98)00455-4. [DOI] [PubMed] [Google Scholar]
- 72.Pinto Cardoso G, et al. Association of intraventricular hemorrhage and death with tocolytic exposure in preterm infants. JAMA Netw. Open. 2018;1:e182355. doi: 10.1001/jamanetworkopen.2018.2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tang, J. et al. Magnesium sulfate-mediated vascular relaxation and calcium channel activity in placental vessels different from nonplacental vessels. J. Am. Heart Assoc.7, 10.1161/JAHA.118.009896 (2018). [DOI] [PMC free article] [PubMed]
- 74.Deruelle P, et al. Effects of antenatal glucocorticoids on pulmonary vascular reactivity in the ovine fetus. Am. J. Obstet. Gynecol. 2003;189:208–215. doi: 10.1067/mob.2003.444. [DOI] [PubMed] [Google Scholar]
- 75.Wong ML, et al. IL-1 beta, IL-1 receptor type I and iNOS gene expression in rat brain vasculature and perivascular areas. Neuroreport. 1996;7:2445–2448. doi: 10.1097/00001756-199611040-00008. [DOI] [PubMed] [Google Scholar]
- 76.Burd I, et al. Beyond white matter damage: fetal neuronal injury in a mouse model of preterm birth. Am. J. Obstet. Gynecol. 2009;201:279 e271–278. doi: 10.1016/j.ajog.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.