Abstract
Nearly a quarter of families of children with need of subspecialty care report difficulty accessing that care. Telehealth is a method to overcome barriers to subspecialty care. However, improving access to subspecialty care through telehealth requires granular identification of specific subspecialty barriers and recognition of the strengths and limitations of each telehealth strategy for addressing identified barriers. Focusing on each sequential step in subspecialty referrals and potential associated barriers, we summarize specific telehealth and technology-enabled strategies to improve access to subspecialty care, including electronic consultations, live interactive telemedicine, store-and-forward telemedicine, tele-mentoring, patient portals, and remote patient monitoring. Intentionally selecting telehealth strategies to target specific subspecialty referral barriers may avoid risks from misapplication of telehealth, may more clearly elevate equitable access as an essential goal within telehealth initiatives, and may also lead to synergistic use of strategies that overcome sequential barriers.
Pediatric subspecialty referrals involve a series of steps, with breakdown in any of these processes impairing access to care.1-3 An ideal referral begins with an initial referral decision, followed by a pre-visit transfer of information. Appointment scheduling is then followed by the consultative visit itself. Optimal referrals then include post-consultative communication and finally ongoing integration of care between primary care, subspecialty care, and the patient and family.1-3
Several barriers to subspecialty care can impede these steps. Pediatric subspecialists are in limited supply and concentrated in urban areas,4-9 leading to excessive wait times for appointments10 and lengthy travel for consultative visits.5 Current systems are plagued by scheduling challenges for parents,3 incomplete information transfer for subspecialists,11-13 and difficulty tracking patient referrals for primary care physicians (PCPs).2,14 Wide variation in referral rates suggests inconsistent PCP referral thresholds and variable referral necessity,15 with potentially unnecessary referrals overburdening pediatric subspecialty departments and delaying the referrals in need of more timely care. The combined effect of these barriers is that nearly a quarter of families of children in need of subspecialty care report difficulty accessing that care.16 Specific populations such as rural children, underinsured children, and children in lower income families face multiple barriers, leading to important geographic and socioeconomic disparities in access and utilization.8,16
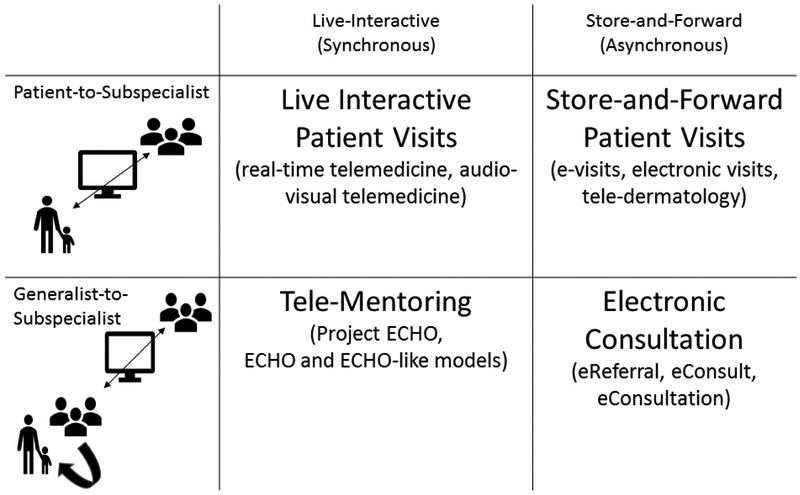
Telehealth is widely identified as a means for improving the ability of patients to access subspecialty care.17 Defined as the delivery of health services through telecommunication technology,18 telehealth encompasses a variety of models such as live-interactive telemedicine encounters, store-and-forward electronic consultations, and tele-mentoring (Figure), each of which can be used to improve connections between subspecialists, PCPs, and patients. But despite shared characteristics of using technology and addressing subspecialty care needs, these models are not interchangeable, yet telehealth is often discussed without adequate differentiation of its types, their purposes, and their limitations. As a result, enthusiasts and skeptics may both carry unrealistic expectations of telehealth, potentially leading to interventions that do not yield hoped-for results, evaluations that focus on inappropriate targets, or reimbursement decisions that miss opportunities to improve care through valuable but overlooked interventions. We aim to illustrate that telehealth is not a single strategy to improve access to subspecialty care, but rather a toolbox of potential tools to improve access, with the appropriateness of each tool depending on the specific barrier being addressed within subspecialty referral processes (Table).
Figure.
Telemedicine Strategies Categorized by Participants and Communication Method.
Table.
Referral Process Steps, Potential Barriers, and Potential Telehealth Strategies.
| Referral Step | Potential Barrier | Examples of Telehealth or Health Information Technology Strategies Addressing Barrier |
|---|---|---|
|
1. Referral Decision |
PCP uncertainty about need for referral or optimal referral | Electronic consultations Electronic messaging |
|
2. Pre-consultative communication |
Information not sent, not received, or not reviewed | Telehealth-enabled intake with nonphysician staff Electronic consultations |
|
3. Appointment Scheduling |
Scheduling process barriers | Electronically-transmitted referrals Patient portals |
| Lack of appointment availability (e.g., demand exceeds supply; excessive wait times) | Tele-Mentoring Electronic consultations |
|
| Difficulty tracking referrals | Electronically-transmitted referrals | |
|
4. Consultative Visit |
Geographic/travel barriers | Live interactive telemedicine Store-and-forward telemedicine |
| Need for urgent or immediate consultation | Live interactive telemedicine (on-demand) | |
| 5. Post-consultative communication | Patient-subspecialist communication barriers | Remote patient monitoring Patient portals |
| Generalist-subspecialist communication barriers | Electronic messaging Tele-Mentoring |
Subspecialty Referral Steps and Telehealth Applications
Referral decisions.
Families report that high-quality referral decisions incorporate shared decision making and specificity of decisions (for example, clear discussion of the expected outcome of the referral and, if relevant, the specific subspecialist to be seen).3 Barriers at this stage can include clinical uncertainty about the need for referral or uncertainty about the optimal subspecialist to meet the referral need.19 These uncertainties can, in turn, limit the ability to engage in shared decision making.3
Electronic consultations are a telehealth strategy well suited for targeting these barriers at the earliest part of the referral process (Table). Electronic consultations, also called eConsults or eReferrals in specific health care systems, use store-and-forward, asynchronous electronic documentation to facilitate communication between PCPs and subspecialists (Figure). Electronic consultations allow PCPs and subspecialists to discuss an individual patient’s subspecialty care needs, triage referral urgency, and coordinate interim evaluation and management.20,21 In some cases, electronic consultation may allow the PCP to manage the patient through this remote subspecialist guidance, thereby obviating the need for a subspecialty visit.22 When subspecialist visits are still needed, the back-and-forth text-based discussions with subspecialists can allow PCPs to address areas of clinical uncertainty, such that PCPs can then update families regarding expected visit outcomes, additional work-up to further inform the consultation, and specific preferred subspecialists. Through this patient-specific education, generalists may gain knowledge transferrable to future referral decisions as well.23 However, the electronic consultation process places additional administrative and clinical work on primary care clinicians,22 which may limit use or increase burn-out if not accompanied by adequate financial compensation or administrative time for this work. Electronic messaging, another technology-enabled tool, is an alternative strategy that can facilitate generalist-to-subspecialist communication around referral decisions, but in a less formalized manner than electronic consultations. These technology-enabled systems can complement other low-tech approaches to address uncertainty in referral decisions, such as referral guidelines.24 By addressing common PCP questions related to initial management and referral, referral guidelines can reduce variation in referrals and pre-emptively answer questions that might otherwise result in electronic consultation, electronic messaging, or telephone calls. Integrating such resources into electronic consultation systems,25 may reduce the volume and improve the efficiency of such systems.
Intake communication.
Families report that high-quality pediatric referral processes require that relevant information is both provided to and reviewed by the subspecialist in advance of the visit.3 For information from PCP records, shared electronic health records are a potential facilitator of information transfer from PCP to subspecialist. Barriers to this transfer of information include lack of interoperability between electronic records, barriers to paper record transfer, and lack of subspecialist time to review records prior to visits.1,3 For information to be obtained directly from families, intake communication can be limited by difficulty connecting by phone or mail with families.
In the process of informing referral decisions as discussed above, the exchange of information through electronic consultation has the potential to facilitate high-quality intake communication. Indeed, in one pediatric health system, electronic consultations were associated with improved PCP perceptions of pre-visit communication.26 However, in some systems, the patient may not necessarily be scheduled with the same subspecialist as the one participating in electronic consultation dialogues, requiring attention to how electronic consultation documentation is stored and made available to the treating subspecialist. The less formalized option of generalist-to-subspecialist electronic messaging for referral decisions also may not result in increasing information available to treating subspecialists unless systems are intentionally designed to allow this. However, shared electronic health records, electronic consultations, and electronic messaging each have the potential to enhance generalist-to-subspecialist pre-visit communication.
To overcome barriers to intake communication with families, live interactive telemedicine with non-physician staff is an innovative approach recently developed by an academic-community partnership.27 This group recognized that many families did not complete needed intake telephone calls after referral, and replaced these calls with a scheduled live interactive telehealth visit with the clinic case worker, during which the case worker reviewed insurance information, referral indication, and other eligibility information.27 This telehealth-enhanced referral process increased the proportion of children completing this intake step from 64% to 80%, and yielded higher family satisfaction with referral processes,27 suggesting utility in real-time audiovisual connection with non-physician staff as a strategy to improve intake communication with families.
Appointment scheduling.
In interviews about subspecialty referrals, families describe a range of difficulties with appointment scheduling, including uncertainty about processes and process reliability, difficulty obtaining a timely appointment that accommodates family obligations, and excessive amounts of time spent scheduling,3 PCPs also report difficulty tracking referrals through the scheduling process.2 Limited appointment availability, due to demand for subspecialty visits that exceeds the available supply, is a key barrier to scheduling. However, additional barriers relate to scheduling processes themselves, including complex telephone triage systems, confusing voicemail boxes, and overtasked office staff.3 Addressing scheduling barrier are an important but often overlooked step for promoting equitable access, as these barriers may be particularly insurmountable for individuals with low health literacy, low English proficiency, precarious employment, or complex custodial arrangements.
Scheduling processes.
One technology-enabled tool to improve scheduling processes themselves is electronically-transmitted referrals. With electronically-transmitted referrals, PCP referral orders are transmitted electronically to subspecialist clinic staff at the time of referral, triggering subspecialist staff to call the family to schedule the referral.28 Implementation of such electronically-transmitted referrals in one pediatric referral system resulted in increased appointment scheduling, increased visit attendance, and increased PCP satisfaction.14 However, even within such a system, disparities in scheduling persist by child race, child insurance type, and neighborhood socioeconomic circumstances,29 suggesting a need for additional targeted interventions to improve equitable access at this step. If designed to transmit information back to the PCP on scheduling outcome, electronically-transmitted referrals may also improve PCP referral tracking capabilities,14 thereby addressing another impediment to high-quality scheduling processes.
Patient portals, through which children or caregivers access the child’s health information online, may also improve scheduling processes, although in many systems patient portal functions are only be available after patients have established a relationship with a specific clinician. Among a sample of pregnant mothers, scheduling was identified as one of the more popular features of patient portals, although not all patient portal users were aware of this functionality.30 Among a sample of patient portal messages sent to pediatric surgical subspecialists, 42% of messages addressed appointments and scheduling, with many of these messages also addressing other clinical needs at the same time.31 However, use of patient portals remains low32 and differences exist in portal use by education level and by insurance.32 Adoption overall and within underserved populations needs to be addressed for portals to meaningfully contribute to addressing barriers within the scheduling process.
Appointment availability.
Appointment scheduling requires appointment availability, which is a barrier that may also be addressed by different telehealth-enabled strategies. One of these strategies is structured subspecialist tele-mentoring programs (e.g., Project ECHO™).33 Tele-mentoring programs schedule regular audio-visual conferences between subspecialists and PCPs to review case-based clinical management, supporting PCP-based care for current patients and enhancing PCP capacity to address future subspecialty care needs without subspecialist input (Figure).33 Two recent reviews of studies of tele-mentoring programs found that most studies focused on provider outcomes and many lacked adequate comparison groups, such that the impact of tele-mentoring programs on actual appointment demand and availability is currently unknown.34,35 While further studies are needed to understand these system-level impacts, a goal of tele-mentoring efforts remains to increase access to care by heightening the quality of PCP-delivered care and increasing the availability of subspecialty appointments.
Electronic consultations are another strategy that may also reduce subspecialty referrals and thereby increase appointment availability. In the process of addressing referral decisions, electronic consultations may allow subspecialists to guide PCPs in their care such that a subspecialty visit is not needed, potentially freeing appointments for more complex patients.36 In one pediatric study, up to 36% of electronic consultations were resolved without an in-person subspecialist visit.37 In another study where 25% of electronic consultations were resolved without an in-person visit, the median time from referral to appointment decreased by 17% after implementation.38 By providing PCPs with patient-specific education, the subspecialty interactions during electronic consultations may also gradually increase PCP capacity for subspecialty care, further reducing future demand for subspecialty appointments.22,23,36 Thus telehealth strategies may help address appointment scheduling barriers by focusing either on improving scheduling processes or increasing current or future appointment availability.
Visit Attendance.
Once scheduled, barriers to attending the consultative visit itself include geographic or travel barriers, scheduling conflicts, and insurance barriers.3,8 Even when visits occur, parents identify other potential barriers to high quality care, including inattention to comprehensive care needs, inattention to informational needs, limited shared decision making, or inadequate time with the subspecialist.3
Live interactive telemedicine visits (i.e. real-time audio-visual teleconferencing between physicians and patients, Figure) are optimal for targeting barriers to the consultative visit itself, particularly the travel and time barriers that arise when long distances or transportation difficulties separate patients from subspecialists.17,39 By overcoming geographic barriers, on-demand models of live interactive telemedicine can also facilitate rapid emergent consultations, such as pediatric critical care or neurology subspecialty consultations in rural emergency departments.40-42 In a recent national survey, 52 US telehealth programs reported providing 43 different pediatric clinical service lines with geographic coverage ranging from regionally to internationally.43 These programs identified multiple barriers to service expansion, including reimbursement issues, licensing/credentialing concerns, and barriers related to state regulations.43 Reimbursement for live interactive telemedicine visits can vary by state and by payer, and can vary within payer by specialty and by patient residence or physical location,44 such that actual out-of-pocket costs to patients or uncertainty about costs or reimbursement are a substantial barrier for both patients and clinicians. In addition to costs, families identified multiple key design elements (e.g., scheduling processes, appointment timeliness, subspecialist buy-in, continuity with known subspecialists) that may enhance family willingness to use telemedicine for pediatric subspecialty care in the context of an ongoing subspecialist relationship.45
Store-and-forward patient-to-subspecialist electronic visits (also called e-visits, or asynchronous telemedicine) can also allow patient and subspecialist to directly communicate, but via transmission of electronic text and images which are sent by the patient and later reviewed by the subspecialist (Figure). Store-and-forward visits could replace initial consultative visits, with new patients sending information and receiving diagnosis and treatment from the reviewing subspecialist, as seen in some teledermatology models.46 Alternatively, store-and-forward visits could replace ongoing maintenance visits with subspecialists. For example, a recent trial used store-and-forward virtual asthma visits for ongoing asthma management while reducing the frequency of in-person visits.47 As with live interactive telemedicine visits, state regulations and state Medicaid policy vary in their stances on whether store-and-forward visits can establish a doctor-patient relationship and in coverage for store-and-forward visits.44
Importantly, while live interactive telemedicine visits and store-and-forward electronic visits are a means of connecting patients with subspecialists, the primary factors determining the value of a telemedicine visit likely relate to the expertise of the treating clinician and the quality of the care delivered more than the use of technology itself. Key aspects, then, of subspecialty telemedicine encounters may include whether the subspecialist is known to the patient or has the potential for an ongoing relationship, whether records are integrated with existing patient electronic medical records, whether visits occur in the home or at a facility, whether peripheral devices (e.g., telestethoscopes) are available to facilitate virtual examination, and whether the subspecialist has appropriate pediatric-specific expertise. Thus while both live interactive telemedicine visits and store-and-forward electronic visits may facilitate care with increased convenience, reduced travel burden, and reduced opportunity costs, the value and quality of the visits may be determined by factors beyond the modality of care delivery – as is the case with in-person care as well.
Additionally, it is vital to recognize that telemedicine visits will not on their own address barriers related to upstream or downstream steps in referral processes, such as scheduling processes, appointment availability, or generalist-to-subspecialist communication.
Post-consultative communication and care integration.
Strategies to improve post-consultative communication and care integration between generalists, subspecialists, families, and patients include remote patient monitoring, electronic messaging, and patient portals. Remote patient monitoring enhances communication between families and subspecialists by assessing and transmitting clinical data for subspecialist review.48 Through ongoing collection of patient data via specialized digital devices or by patient report, remote patient monitoring facilitates more continuous care than traditionally provided by intermittent in-person subspecialist visits.48 Live-interactive telemedicine visits or store-and-forward telemedicine visits may also be used to enhance the frequency of communication or interval care with patients and families without adding the potential burden of additional in-person visits.47,49 E-mail and short message service texts between subspecialists, PCPs, and/or families may provide another less structured opportunity to enhance and integrate care between visits, although the convenience of these methods of communication must be tempered by concerns about data confidentiality and data integrity. Finally, patient portals can provide a platform for both patient data reporting and family-to-subspecialist electronic messages between visits, allowing enhanced communication on topics ranging from logistical to medical to social concerns.31
Value of Specificity in Telehealth Implementation
Overcoming Risks.
Each of these strategies offer opportunities to improve specific aspects of a complicated process, but they also carry potential risks and unintended consequences. In addition to concerns noted previously regarding specific strategies, general risks associated with telehealth remain salient (e.g., concerns about privacy, quality, and possible overutilization).39 The potential for some groups of patients to have inadequate access to or comfort with telehealth-enabled systems is another important consideration, lest telehealth systems perpetuate or exacerbate existing disparities. Additionally, strategies that enhance pre-visit or post-visit communication also alter physician workflow and scope of practice, potentially contributing to physician burn-out if associated issues of workload and reimbursement are not addressed.22
Beyond these concerns, additional specific risks arise if a strategy is implemented in hopes of improving a problem it does not target. In clinical and research settings, such misapplication could lead to missed opportunities to improve access, to wasted resources, and to negative evaluations. For example, the impact of an electronic consultation program may be limited in a system with persistent appointment scheduling barriers. Further, new systems may be blamed for old problems if an improvement in upstream referral processes unmasks or exacerbates downstream bottlenecks.
In the policy arena, a lack of appreciation of the differences between telehealth models may lead to policies and reimbursement schedules that preferentially incentivize one telehealth model despite the potential value of others. For example, fee-for-service reimbursement for live interactive telemedicine visits promotes a strategy that addresses geographic barriers, but has the potential to place additional visit demand on a finite number of subspecialists and inefficient scheduling systems, two different barriers which require different solutions.
Enhancing Equity.
Intentionally selecting telehealth strategies to target specific identified subspecialty referral barriers may also aid in centering health equity more clearly in telehealth initiatives. As highlighted within the discussion of specific strategies, many mechanisms could lead to unequal use of telehealth among patients. For example, differences in adoption of telehealth may be driven by disparities in access to technology (e.g., equipment; internet service50), varied personal preferences regarding technology (e.g., parent comfort with technology), or unequal financial access to telehealth due to state or insurer policy (e.g., coverage dictated by miles from care,44 which may not account for substantial travel barriers facing urban populations). Additionally, just as differences exist in which patients report being offered access to a patient portal,32 individual or systemic biases may influence who is offered the option of telehealth.
Naming the barrier to be addressed through telehealth implementation can more clearly guide implementation and evaluation to account for and overcome these additional barriers to achieve equitable access. First, by selecting a telehealth strategy in response to a specific referral barrier, subsequent implementation decisions can be guided by identification of which patient populations are disproportionately impacted by the identified barrier and by prioritizing representative family perspectives in design and implementation. Second, when specific referral barriers are clearly named as the impetus for telehealth programs, evaluation of these telehealth programs may focus more specifically on the degree to which barriers are removed and whether equity in access is achieved. Because average improvement in access can occur even as disparities widen, implementation of telehealth initiatives must intentionally target and actively assess equity, ideally by partnering with families to tailor strategies to those most in need of improved access.
Achieving Synergy.
Recognizing the strengths and limitations of each strategy also illuminates the potential synergy of using these strategies together to optimize sequential steps in the referral process. In such a system, the referral process could begin with an electronic consultation, allowing PCP and subspecialists to come to shared understanding of referral needs. The conclusion of this electronic consultation could then trigger an electronically-transmitted referral message to subspecialist office staff to facilitate patient scheduling. These processes could be integrated with the patient portal to allow families to track the “status” of their referral through this process. If determined to be appropriate through the prior electronic consultation dialogue, the option of a telemedicine visit could be offered in lieu of an in-person visit. Alternatively, if an in-person visit is required, the prior electronic consultation could allow coordination of any testing anticipated to be needed at the time of the visit. And after the consultative visit, the subspecialist could engage in three-way messaging with the PCP and patient via a patient portal, with the patient reporting follow-up data at regular intervals via the same portal. By comprehensively using this full set of tools to address each step in the referral process, the patient, PCP, and subspecialist would achieve more coordinated, continuous connected care, unimpeded by referral barriers.
Conclusion
In the swell of enthusiasm for telehealth, it is essential to be precise about the specific referral barriers each strategy addresses and does not address. As telehealth evidence and experience grows and as the logistical, technological, and financial barriers to use of telehealth subside, we have increasing opportunities to select from a range of telehealth tools when seeking to address specific referral barriers. In this evolving context, a comprehensive vision of the role of each telehealth strategy in improving access to pediatric subspecialty care is needed, such as that proposed here, so that implementation decisions can be made based on specific referral barriers and desired outcomes in order to optimize access to subspecialty care for all children.
What’s new: Addressing each sequential step and potential barrier in subspecialty referral processes, we discuss the abilities of specific telehealth and technology-enabled strategies to address specific components of access to subspecialty care, including electronic consultations, live-interactive telemedicine, store-and-forward telemedicine, and tele-mentoring.
Acknowledgments
Financial Support: Dr. Ray is supported by an NIH career development award (K23HD088642). The content and views are solely the responsibility and opinions of the author and do not necessarily represent the official views or policies of funders.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors have no conflicts of interest to report.
Financial Disclosures: The authors have no financial disclosures to report.
References
- 1.Institute for Healthcare Improvement / National Patient Safety Foundation. Closing the Loop; A Guide to Safer Ambulatory Refrrals in the EHR Era. Cambridge, Massachusetts: Institute for Healthcare Improvement;2017. [Google Scholar]
- 2.Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89(1):39–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ray KN, Ashcraft LE, Kahn JM, Mehrotra A, Miller E Family perspectives on high-quality pediatric subspecialty referrals. Acad Pediatr. 2016. August;16(6):594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayer ML. Are we there yet? Distance to care and relative supply among pediatric medical subspecialties. Pediatrics. 2006;118(6):2313–2321. [DOI] [PubMed] [Google Scholar]
- 5.Mayer ML. Disparities in geographic access to pediatric subspecialty care. Matern Child Health J. 2008;12(5):624–632. [DOI] [PubMed] [Google Scholar]
- 6.Mayer ML, Beil HA, von Allmen D. Distance to care and relative supply among pediatric surgical subspecialties. J Pediatr Surg. 2009;44(3):483–495. [DOI] [PubMed] [Google Scholar]
- 7.Basco WT, Rimsza ME. Pediatrician workforce policy statement. Pediatrics. 2013;132(2):390–397. [DOI] [PubMed] [Google Scholar]
- 8.Ray KN, Bogen DL, Bertolet M, Forrest CB, Mehrotra A. Supply and utilization of pediatric subspecialists in the US. Pediatrics. 2014;133(6):1061–1069. [DOI] [PubMed] [Google Scholar]
- 9.Ray K, Kahn J, Miller E, Mehrotra A. Use of adult-trained medical subspecialists by children seeking medical subspecialty care. Journal of Pediatrics. 2016. June 22 [Epub ahead of print];176:173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pletcher BA, Rimsza ME, Cull WL, Shipman SA, Shugerman RP, O'Connor KG. Primary care pediatricians' satisfaction with subspecialty care, perceived supply, and barriers to care. J Pediatr. 2010;156(6):1011–1015. [DOI] [PubMed] [Google Scholar]
- 11.Stille CJ, Primack WA, Savageau JA. Generalist-subspecialist communication for children with chronic conditions: a regional physician survey. Pediatrics. 2003;112(6 Pt 1):1314–1320. [DOI] [PubMed] [Google Scholar]
- 12.Stille CJ, McLaughlin TJ, Primack WA, Mazor KM, Wasserman RC. Determinants and impact of generalist-specialist communication about pediatric outpatient referrals. Pediatrics. 2006; 118(4): 1341–1349. [DOI] [PubMed] [Google Scholar]
- 13.Stille CJ, Primack WA, McLaughlin TJ, Wasserman RC. Parents as information intermediaries between primary care and specialty physicians. Pediatrics. 2007;120(6):1238–1246. [DOI] [PubMed] [Google Scholar]
- 14.Ray KN, Drnach M, Mehrotra A, Suresh S, Docimo SG. Impact of Implementation of Electronically Transmitted Referrals on Pediatric Subspecialty Visit Attendance. Acad Pediatr. 2018. May-Jun;18(4):409–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forrest CB, Majeed A, Weiner JP, Carroll K, Bindman AB. Referral of children to specialists in the United States and the United kingdom. Arch Pediatr Adolesc Med. 2003;157(3):279–285. [DOI] [PubMed] [Google Scholar]
- 16.Bethell CD, Kogan MD, Strickland BB, Schor EL, Robertson J, Newacheck PW. A national and state profile of leading health problems and health care quality for US children: key insurance disparities and across-state variations. Acad Pediatr. 2011;11(3 Suppl):S22–33. [DOI] [PubMed] [Google Scholar]
- 17.The Use of Telemedicine to Address Access and Physician Workforce Shortages. Pediatrics. 2015;136(1):202–209. [DOI] [PubMed] [Google Scholar]
- 18.Telehealth for Acute and Chronic Conditions. Effective Health Care Program https://effectivehealthcare.ahrq.gov/topics/telehealth-acute-chronic/research-protocol. Accessed April 18, 2019.
- 19.Porras-Javier L, Bromley E, Lopez M, Coker TR. Challenges to Effective Primary Care-Specialty Communication and Coordination in the Mental Health Referral and Care Process for Publicly Insured Children. J Behav Health Serv Res. 2018;45(4):668–677. [DOI] [PubMed] [Google Scholar]
- 20.Chen AH, Murphy EJ, Yee HF Jr. eReferral--a new model for integrated care. N Engl J Med. 2013;368(26):2450–2453. [DOI] [PubMed] [Google Scholar]
- 21.Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: A systematic review and narrative synthesis. J Telemed Telecare. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee MS, Ray KN, Mehrotra A, Giboney P, Yee HF Jr., Barnett ML. Primary Care Practitioners' Perceptions of Electronic Consult Systems: A Qualitative Analysis. JAMA Intern Med. 2018;178(6):782–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwok J, Olayiwola JN, Knox M, Murphy EJ, Tuot DS. Electronic consultation system demonstrates educational benefit for primary care providers. J Telemed Telecare. 2017:1357633X17711822. [DOI] [PubMed] [Google Scholar]
- 24.Cornell E, Chandhok L, Rubin K. Implementation of referral guidelines at the interface between pediatric primary and subspecialty care. Healthc (Amst). 2015;3(2):74–79. [DOI] [PubMed] [Google Scholar]
- 25.Soni SM, Giboney P, Yee HF Jr. Development and Implementation of Expected Practices to Reduce Inappropriate Variations in Clinical Practice. JAMA. 2016;315(20):2163–2164. [DOI] [PubMed] [Google Scholar]
- 26.Rea CJ, Wenren LM, Tran KD, et al. Shared Care: Using an Electronic Consult Form to Facilitate Primary Care Provider-Specialty Care Coordination. Acad Pediatr. 2018;18(7):797–804. [DOI] [PubMed] [Google Scholar]
- 27.Coker TR, Porras-Javier L, Zhang L, et al. A Telehealth-Enhanced Referral Process in Pediatric Primary Care: A Cluster Randomized Trial. Pediatrics. 2019; 143(3). [DOI] [PubMed] [Google Scholar]
- 28.Barnett ML, Mehrotra A, Frolkis JP, et al. Implementation Science Workshop: Implementation of an Electronic Referral System in a Large Academic Medical Center. J Gen Intern Med. 2016;31(3):343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bohnhoff JC, Taormina JM, Ferrante L, Wolfson D, Ray KN. Unscheduled referrals and unattended appointments after pediatric subspecialty referral. . Under review. [DOI] [PubMed] [Google Scholar]
- 30.Kim J, Mathews H, Cortright LM, Zeng X, Newton E. Factors Affecting Patient Portal Use Among Low-Income Pregnant Women: Mixed-Methods Pilot Study. JMIR Form Res. 2018;2(1):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riera KM, Robinson JR, Van Arendonk KJ, Jackson GP. Care Delivered by Pediatric Surgical Specialties Through Patient Portal Messaging. J Surg Res. 2019;234:231–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anthony DL, Campos-Castillo C, Lim PS. Who Isn't Using Patient Portals And Why? Evidence And Implications From A National Sample Of US Adults. Health Aff (Millwood). 2018;37(12):1948–1954. [DOI] [PubMed] [Google Scholar]
- 33.Arora S, Kalishman S, Dion D, et al. Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Aff (Millwood). 2011;30(6):1176–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fischer SH, Rose AJ, McBain RK, Faherty LJ, Sousa J, Martineau M. Evaluation of technology-enabled collaborative learning and capacity building models: materials for a report to Congress. . Santa Monica, CA: RAND Corporation;2019. [Google Scholar]
- 35.Zhou C, Crawford A, Serhal E, Kurdyak P, Sockalingam S. The Impact of Project ECHO on Participant and Patient Outcomes: A Systematic Review. Acad Med. 2016;91(10):1439–1461. [DOI] [PubMed] [Google Scholar]
- 36.Liddy C, Moroz I, Mihan A, Nawar N, Keely E. A Systematic Review of Asynchronous, Provider-to-Provider, Electronic Consultation Services to Improve Access to Specialty Care Available Worldwide. Telemed J E Health. 2019;25(3):184–198. [DOI] [PubMed] [Google Scholar]
- 37.Lai L, Liddy C, Keely E, et al. The impact of electronic consultation on a Canadian tertiary care pediatric specialty referral system: A prospective single-center observational study. PLoS One. 2018;13(1):e0190247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnett ML, Yee HF Jr., Mehrotra A, Giboney P Los Angeles Safety-Net Program eConsult System Was Rapidly Adopted And Decreased Wait Times To See Specialists. Health Aff (Millwood). 2017;36(3):492–499. [DOI] [PubMed] [Google Scholar]
- 39.Kahn JM. Virtual visits--confronting the challenges of telemedicine. N Engl J Med. 2015;372(18):1684–1685. [DOI] [PubMed] [Google Scholar]
- 40.Dharmar M, Romano PS, Kuppermann N, et al. Impact of critical care telemedicine consultations on children in rural emergency departments. Crit Care Med. 2013;41(10):2388–2395. [DOI] [PubMed] [Google Scholar]
- 41.Demaerschalk BM, Berg J, Chong BW, et al. American Telemedicine Association: Telestroke Guidelines. Telemed J E Health. 2017;23(5):376–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dayal P, Hojman NM, Kissee JL, et al. Impact of Telemedicine on Severity of Illness and Outcomes Among Children Transferred From Referring Emergency Departments to a Children's Hospital PICU. Pediatr Crit Care Med. 2016;17(6):516–521. [DOI] [PubMed] [Google Scholar]
- 43.Olson CA, McSwain SD, Curfman AL, Chuo J. The Current Pediatric Telehealth Landscape. Pediatrics. 2018;141(3). [DOI] [PubMed] [Google Scholar]
- 44.Center for Connected Health Policy. State telehealth laws and Medicaid program policies: a comprehensive scan of the 50 states and District of Columbia. . 2018; https://www.cchpca.org/telehealth-policy/state-telehealth-laws-and-reimbursement-policies-report. Accessed May 8, 2019.
- 45.Ray KN, Ashcraft LE, Mehrotra A, Miller E, Kahn JM. Family Perspectives on Telemedicine for Pediatric Subspecialty Care. Telemed J E Health. 2017;23(10):852–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O'Connor DM, Jew OS, Perman MJ, Castelo-Soccio LA, Winston FK, McMahon PJ. Diagnostic Accuracy of Pediatric Teledermatology Using Parent-Submitted Photographs: A Randomized Clinical Trial. JAMA Dermatol. 2017;153(12):1243–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van den Wijngaart LS, Roukema J, Boehmer ALM, et al. A virtual asthma clinic for children: fewer routine outpatient visits, same asthma control. Eur Respir J. 2017;50(4). [DOI] [PubMed] [Google Scholar]
- 48.Totten AM, Womack DM, Eden KB, et al. In: Telehealth: Mapping the Evidence for Patient Outcomes From Systematic Reviews. Rockville (MD)2016. [PubMed] [Google Scholar]
- 49.Willard A, Brown E, Masten M, et al. Complex Surgical Infants Benefit From Postdischarge Telemedicine Visits. Adv Neonatal Care. 2018;18(1):22–30. [DOI] [PubMed] [Google Scholar]
- 50.Drake C, Zhang Y, Chaiyachati KH, Polsky D. The Limitations of Poor Broadband Internet Access for Telemedicine Use in Rural America: An Observational Study. Ann Intern Med. 2019. [DOI] [PubMed] [Google Scholar]