Abstract
The aim of this study was to evaluate the effectiveness of the McKenzie method compared to manual therapy in the management of patients with chronic low back pain (CLBP). Randomised controlled trials evaluating the McKenzie method in treating CLBP in adults compared to manual therapy (MT) were searched in MEDLINE, CINAHL, Cochrane Library, and PEDro. The primary outcomes were pain and disability. Five trials were eligible for inclusion in the review, of which, most had a score of 8 out of 11 on the PEDro scale. At 2-3 months, all studies reported significant improvement in the pain level in the McKenzie group, and more than that in the MT group. At 6 months, significant improvements had occurred in the disability index reported by two trials in the McKenzie group than the MT group. At 12 months follow-up, there were no significant differences in measures of LBP, but three studies reported that the McKenzie method group had a better disability level than the MT group. In patients with CLBP, many pain measures showed that the McKenzie method is a successful treatment to decrease pain in the short term, while the disability measures determined that the McKenzie method is better in enhancing function in the long term.
Keywords: Chronic Low Back Pain, Mckenzie Treatment, Physical Therapy, Manual Therapy, Disability
Introduction
Low back pain (LBP) is a leading cause of disability that affects a substantial number of people with a significant global burden to societies and economies[1]. Globally, LBP ranks within the top 10% of debilitating conditions that cause most disability-adjusted life years (DALYs)[2]. Although LBP is a non-malignant, often self-resolving condition, patients often seek therapeutic measures to reduce the severity of the symptoms experienced. Chronic LBP (CLBP) often leads to lifestyle changes and prolonged absences from work due to its physically limiting nature. The discomfort and inconvenience associated with CLBP necessitate its prompt treatment[3].
The appropriate management of CLBP is a complex issue and depends on multiple factors involving physicians, healthcare policy makers, and patients[4]. Currently, there is support for several prospective treatments[5], and the National Institute for Health and Care Excellence (NICE) guidelines[6] urge the early treatment and management of CLBP. NICE suggest that benefit can be gained by information, education and patient preferences, regular exercise and physical activity, assessing and imaging patients, a combination of physical and psychological treatments, manual physiotherapy, invasive measures, and referral for surgery.
McKenzie method has been recognized as one of effective methods for treating LBP. This has become the most popular, particularly among physiotherapists, clinically approved treatment for LBP; it is recommended by NICE as a structured exercise programme[7]-[9]. The McKenzie method of LBP treatment is explained by the principle that exercises that encourage disc centralisation should be promoted, and exercises that encourage disc peripheralisation should be avoided10. After initial assessments, patients are arranged into four groups: postures, derangements, dysfunctions, and the presence of any non-mechanical syndromes[10].
The use of manual therapy (MT) is also recommended by NICE for treating patients with LBP6. MT is a hands-on treatment that involves spinal manipulation and patient mobilisation[11]-[12]. The mobilisation entails low-velocity passive movements through a normal range of motion (ROM), whereas the spinal manipulation involves high velocity impulses and thrusts that are normally administered to synovial joints, beyond their normal ROM, which may lead to audible sounds[13]. This technique is often used by osteopaths, chiropractors, and manual therapists.
Personalised exercises pertaining to homogenous subgroups of CLBP identify MT alongside the McKenzie method. Notwithstanding this, it would seem the evidence relating to its efficiency is dubious[14]-[16]. However, it is unknown if the McKenzie method can provide similar or superior beneficial effects compared to MT for CLBP in terms of pain and disability. Thus, this review aimed to evaluate the efficacy of the McKenzie method in treating CLBP, by comparing it to the MT method.
Materials and methods
Protocol
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline was used to conduct this review.
Search methods
The following databases were searched up to May 2016: MEDLINE, PEDro, The Cochrane Library, and CINAHL. Search terms including McKenzie, manual therapy, back pain, mobilisation, traction, end-range exercises, mechanical diagnosis and therapy (MDT), manipulation, active range of motion (AROM) exercises were used. Regional variations in spelling (e.g. between US and British English) were accounted for, as were acronyms and abbreviated terms, when conducting the search. No language filters were applied. The references of the relevant papers found were also manually searched and reviewed to identify further potential sources of information.
Types of studies
The eligibility criteria for this study limited research data to randomised controlled trials (RCTs) that compared the relative efficacies of the McKenzie method and the MT method in treating CLBP among adults. All RCTs should clearly outline and use appropriate methods of randomisation (e.g. computer-generated random sequences). Quasi-randomised trials were excluded (e.g. randomisation by date of birth).
Types of participants
Participants involved in the trials included both male and female patients between the ages of 18 and 76 who had received therapy for CLBP. For the purposes of this study, CLBP was defined as LBP that had lasted for more than 12 weeks, during which time the patient had not been pain-free for more than 30 consecutive days[17]. Trials that omitted significant information, such as the duration of the patients’ symptoms, were excluded, as were trials that focussed on the primary prevention of CLBP. Trials in which patients differed in their presenting conditions (e.g. some patients having sub-acute LBP and some having CLBP) were only included if the CLBP patients were separated. Trials involving patients with specific underlying pathologies (e.g. spinal stenosis, scoliosis, radicular syndrome); pregnant patients; post-surgical (within 6 months) patients; patients with severe metabolic or cardiovascular disease; and patients with red flag symptoms for serious spinal pathology were also excluded.
Types of outcome measures
The primary outcome selected for this review was pain using the Numeric Pain Rating Scale (NPRS), Visual Analogue Scale (VAS), Symptom Bothersomeness Scale, and McGill Pain Questionnaire. Back function was also evaluated using the Roland Morris Disability Questionnaire (RMDQ) and the Oswestry Disability Index (ODI). These outcome measures were selected based on high levels of validity and reliability in measuring CLBP. The secondary outcomes comprised of general health status (e.g. SF-12), further visits to healthcare practitioners [e.g. the quantity of visits and dichotomous processes (yes/no)], return to work (e.g. return to work, number of days off work), and patient satisfaction [e.g. Patient Satisfaction Subscale (PSS)].
Data extraction
A standardised form was used to extract relevant data from articles. The following data was extracted: authors’ names, year of publication, setting, sample size, duration of intervention programme, outcome measures, type of intervention, baseline/pre and post values such as mean differences (MDs) or standardised mean differences (SMDs), and 95% confidence intervals (CIs). All pain, limitation of activity, and patient satisfaction scores were converted to a 0-100 scale.
Assessment of risk of bias
Issues regarding research bias and validity were evaluated. The PEDro scale was used to critically appraise the RCTs included in this study. The PEDro scale uses an 11-point scale with points awarded using yes/no responses to questions. It is an established means of assessing the methodological value of clinical trials[18] and evaluates the internal and external validity of clinical trials, also assessing the biases related to selection processes, detection, and performance.
Data analysis
Data analysis was performed with qualitative and quantitative methods based on PRISMA guidelines. I[2] statistics and the Chi[2] test were used to assess the statistical heterogeneity between the trials used in this study. I[2] statistics measure the degree of heterogeneity of trials, and the Chi[2] test reviews observable differences between trials and assesses whether these may be due to chance alone. Due to the clinical diversity of the trials studied, and the large variations in their methodologies, a meta-analysis was not performed.
Results
Search yield
A total of 203 articles were identified within the electronic databases, while 7 additional articles were identified through a manual bibliographic search. Duplicate citations were removed with the aid of the RefWorks citation manager programme yielding 95 non-duplicate articles. Another 74 articles were screened and excluded based on titles, 11 of which were reviewed and excluded based on the abstracts. After full-text records of the remaining 10 articles were reviewed, only 5 trials were eligible for inclusion in this review[19]-[23]. Figure 1 shows the flowchart of the search process.
Figure 1.
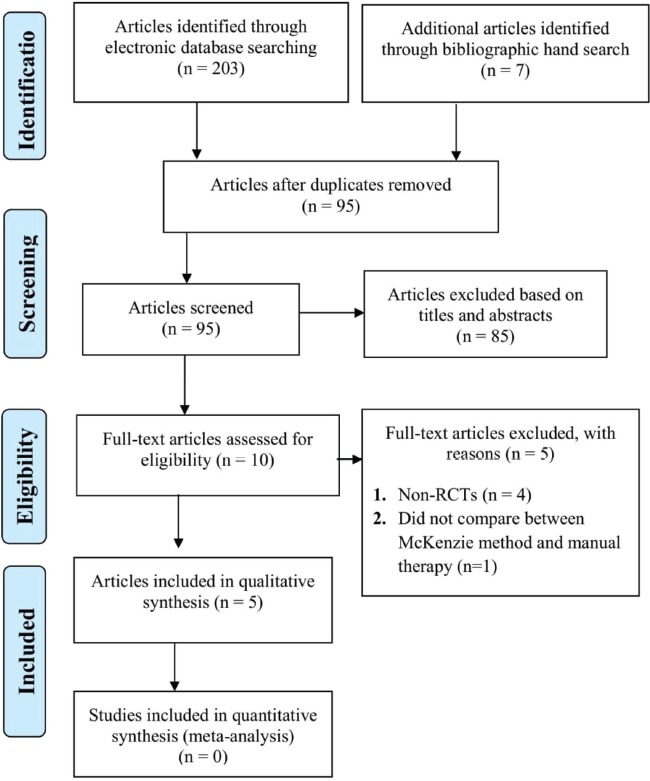
Flowchart of search process.
Characteristics of included studies
The main characteristics of the included studies are shown in Table 1. In total, 810 subjects were examined across the five studies. Across the studies, the mean number of participants was 162, the range of participants within the studies was 25-350, with 3 studies having relatively small sample sizes of 25, 90, and 97 subjects[21]-[23]. The small sample sizes affect the internal validity of the studies, reducing the value of their evidence. Smaller studies demonstrably have larger effect sizes, impacting their influence on the level of difference between the cohorts[24] and increasing the likelihood of type 2 errors (i.e. failing to detect a present effect). Therefore, there is a potential for publication bias, as studies producing insignificant results are unlikely to be published[25]. Most subjects across the five studies were employed and well-educated, 54.5% were male, and the mean age of participants was 41, with their ages ranging from 18 to 76 years.
Table 1.
Summary of included study characteristics.
| Study | Setting | Duration | Outcomes measured | Interventions |
|---|---|---|---|---|
| Cherkin et al.[19] | Primary care clinics | Pain longer than 7 days | Roland disability scale, bothersomeness at 4 and 12 weeks, 1 and 2 years, sought care at 2 years, quality of care at 4 weeks | 1. Physical therapy (N=129): McKenzie assessment, patients classified, treated accordingly 2. Chiropractic manipulation (N=119) and assessment: short lever high velocity thrust manipulations. Exercise sheet given 3. Educational booklet provided |
| Schenk et al.[22] | Setting not specified | LBP for 7 days but less than 7 weeks | Visual analogue scale (VAS), Oswestry scale at 3rd visit. | Standard protocol: Postural correction and 20 min x 3 visits, treadmill, 5 sets of 10 interventions 1. Exercise group (N=15): individual exercises based on assessment findings 2. Mobilisation group (N=10): passive movements based on the assessment findings |
| Paatelma et al.[21] | Occupational health care centre | LBP longer than 7 days | Roland Morris Disability questionnaire at baseline, and at 3, 6, and 12 months follow-up | 1.Orthopaedic manual therapy (N=45) 2. McKenzie method group (N=52) 3. “Advice only to be active” group |
| Kilpikoski et al.[23] | Hospital clinic | LBP longer than 7 days | Back and leg pain were assessed by VAS, disability with the Roland Morris questionnaire and functional status with an activities of daily living (ADL) index immediately after the treatment period, at 3, 6 and 12 months follow-up | 1.Orthopaedic manual therapy (N=42) 2. McKenzie method group (N=48) 3. “Advice only to be active” group |
| Petersen et al.[20] | Primary care clinics | LBP longer than 6 weeks | Main outcome: a reduction of at least 5 points or an absolute score below 5 points on the Roland Morris Questionnaire | Secondary outcomes were reduction in disability and pain, global perceived effect, general health, mental health, lost work time, and medical care utilisation 1. McKenzie treatment (N=175) 2. Spinal manipulation (N=175): all types of manual techniques including vertebral mobilisation and high velocity thrust as well as myofascial trigger-point massage were used |
Quality assessment
The quality assessment scores for the included studies are shown in Table 2. The median quality assessment sum score on the PEDro scale was 8, with a range of 6-8. Most of the studies had an 8 out of 11 PEDro score, while Schenk et al.[22] recorded the lowest PEDro score of 6. The most common methodological flaw present in all five trials was a failure to blind the patient (5 trials), the therapist (5 trials) and the assessor (5 trials). However, in Schenk et al.[22], the assessors were not blinded to concealed allocation. It is arguable though, that blinding would be difficult to achieve in a trial evaluating the McKenzie method versus MT. Failure to explicitly use an intention to treat analysis occurred in one of the five studies[22].
Table 2.
Methodological quality of included trials.
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cherkin et al.[19] | + | + | + | + | - | - | - | + | + | + | + | 8 |
| Schenk et al.[22] | + | + | - | + | - | - | - | + | - | + | + | 6 |
| Paatelma et al.[21] | + | + | + | + | - | - | - | + | + | + | + | 8 |
| Kilpikoski et al.[23] | + | + | + | + | - | - | - | + | + | + | + | 8 |
| Petersen et al.[20] | + | + | + | + | - | - | - | + | + | + | + | 8 |
PEDro items: 1 Eligibility criteria; 2 Random allocation; 3 Concealed allocation; 4 Comparability at baseline; 5 Patient blinding; 6 Therapist blinding; 7 Assessor blinding; 8 At least 85% follow-up; 9 Intention to treat analysis; 10 Between-group statistical comparisons; 11 Point measures and measures of variability.
Treatment efficacy
The outcome variables at the different follow-up points, as well as the sizes of the effects of the trials and pooled results are depicted in Table 3. At baseline, pain, disability and functional status were at the same level across the groups. Immediately after the treatment period, Schenk et al.[22] and Kilpikoski et al.[23] found that the McKenzie group had a significantly greater decrease in pain level (p=0.01; p=0.001, respectively), and significantly greater improvements in the Roland Disability scores (p=0.03)[22]. At 2-3 months, all studies reported significant improvements in level of pain, reported in the McKenzie group to a greater extent than the MT group. According to Petersen et al.[20], there were some differences in the Roland Disability scores in the McKenzie intervention group, beyond those reported in the MT group (p=0.022).
Table 3.
McKenzie vs. manual therapy.
| Study | Duration | Quantitative Results | |||
|---|---|---|---|---|---|
| Outcomes | (Mean, 95% CI) | p-value | |||
| McKenzie | Manual Therapy | ||||
| Cherkin et al.[19] | Baseline | VAS | 6.0(5.6-6.5) | 5.5 (5.1–5.8) | 0.04 |
| RMDQ | 12.2 (11.2–13.1) | 12.1 (11.2–13.1) | 0.83 | ||
| 1 month | VAS | 2.3 (1.9–2. 8) | 1.9 (1.5–2.2) | 0.007 | |
| RMDQ | 4.1 (3.3–4.9) | 3.7 (2.9–4.5) | 0.25 | ||
| 3 months | VAS | 2.7 (2.2–3.2) | 2.0 (1.6–2.4) | 0.02 | |
| RMDQ | 3.1 (2.4–3.9) | 4.1 (3.2–5.0) | 0.15 | ||
| Schenk et al.[22] | Baseline | VAS | 3.9 | 3.8 | 0.852 |
| ODI | 27.40 | 29.5 | 0.70 | ||
| Immediately after the 3rd visit | VAS | -2.1 | -3.0 | 0.037 | |
| ODI | -9.06 | -6.20 | 0.047 | ||
| Paatelma et al.[21] | Baseline | VAS | 32 | 35 | NA |
| RMDQ | 9 | 9 | NA | ||
| 3 months | VAS | 10 (-20–6) | 18 (-14–12) | 0.389 | |
| RMDQ | 2 (-4–2) | 1 (-4–3) | 0.751 | ||
| 6 months | VAS | 10 (-27– -4) | 14 (-22–2) | 0.009 | |
| RMDQ | 0 (-7– -1) | 1 (-6–0) | 0.003 | ||
| 12 months | VAS | 8 (-17–9) | 11(-17–9) | 0.732 | |
| RMDQ | 1 (-6–0) | 0 (-6–0) | 0.028 | ||
| Kilpikoski et al.[23] | Baseline | VAS | 31 | 35 | NA |
| RMDQ | 9 | 9 | NA | ||
| Immediately after treatment | VAS | 16 (-14–1) | 22 (-14–1) | 0.125 | |
| RMDQ | 1 (-4–0) | 3 (-4–0) | 0.145 | ||
| At 6 months visit | VAS | 10 (-11–1) | 14 (-11–1) | 0.164 | |
| RMDQ | 0 (-3–0) | 1 (-3–0) | 0.028 | ||
| 12 months | VAS | 8 (-10–8) | 11 (-10–8) | 0.920 | |
| RMDQ | 1 (-3–1) | 0 (-3–1) | 0.318 | ||
| Petersen et al.[20] | Immediately after treatment | VAS | 15.3 (-1.2–4.4) | 13.8 (-1.2–4.4) | 0.271 |
| RMDQ | 6.5 (-0.6–2) | 5.8 (-0.6–2) | 0.268 | ||
| 2 months | VAS | 14.4 (-1.3–4.1) | 13 (-1.3–4.1) | 0.309 | |
| RMDQ | 6.7 (0.2–2.8) | 5.2 (0.2–2.8) | 0.022 | ||
| 12 months | VAS | 15 (-0.2–5.8) | 12.2 (-0.2–5.8) | 0.063 | |
| RMDQ | 7.1 (0.2–2.9) | 5.6 (0.2–2.9) | 0.030 | ||
VAS Visual Analogue Scale, RMDQ Roland Morris Disability Questionnaire, ODI Oswestry Disability Index.
At the six month follow-up, significant improvements were observed in the disability index reported by Kilpikoski et al.[23] and Paatelma et al.[21] in the McKenzie group (p<0.028; p<0.05, respectively), beyond improvements seen in the MT group, with no differences between the groups in LBP. At the 12-month follow-up, there were no significant differences between groups in LBP, but it was reported[19]-[21] that the McKenzie method group had a better disability level than the MT group (p=0.05, p=0.028, p=0.030, respectively).
Discussion
The objective of this review was to evaluate current evidence for the efficacy of the McKenzie method in treating CLBP in adults in comparison to MT. Five studies met the inclusion criteria. During the first six months, all studies reported significant improvement in pain level in the McKenzie group, beyond those reported in the MT group. Most trials found no improvement in the disability level, except in the trial by Petersen et al.[20], who reported differences in disability improvement for those receiving the McKenzie intervention (p=0.022). These results support the findings of previous studies. At the six-month follow-up, two trials[21,23] reported that the McKenzie method was a successful treatment to improve disability level (p<0.05, p<0.028, respectively), but Schenk et al.[22] reported significant differences in LBP for the McKenzie group (p=0.037). At the 12-month point/mark, there were no significant differences between groups in LBP, but most studies[19]-[21] reported that the McKenzie method group had a better disability level than the MT group (p=0.05, p=0.028, p=0.030, respectively).
The range of the median quality assessment sum scores for the trials using the PEDro scale was 6-8, and the mean was 8. The lack of patient, therapist, and assessor blinding was the most common methodological flaw. However, in the study performed by Schenk et al.[22], the assessors were not blinded to concealed allocation, which introduced the possibility of selection bias. It should be mentioned, however, that blinding is not always possible in clinical trials, especially physiotherapist-blinding in clinical trials regarding physiotherapeutic treatments. Therefore, the methodological quality of the trials should not be considered as significantly downgraded due to this limitation. Blinding is much more difficult to conduct in non-pharmacological treatment studies than it is in pharmacological treatment studies[26]. Assessor blinding, however, is possible in these studies, and it especially significant when considering the subjective nature of clinical examinations (e.g. assessing flexibility, strength, and palpation) performed without an awareness of the allocated groups of subjects. Assessor blinding is promoted, as it reduces the potential for bias within the study[27]. Additionally, the relatively small sample size of three of the included studies (25, 90 and 97 subjects)[21]-[23] was attributable to the internal validity of the studies, reducing the value of their evidence. Smaller studies demonstrably have larger effect sizes, impacting their influence on the level of difference between the cohorts[24] and increasing the likelihood of type 2 errors. Therefore, there is a potential for publication bias, as studies producing insignificant results are unlikely to be published[25].
The study by Schenk et al.[22] reported the lowest scores on the PEDro scale. Despite this, the results were limited in their generalisability because their disability ratings were perceived to be high, especially for those subjects within the mobilisation groups of the Oswestry Index (at the baseline). This high baseline score has the potential to result in intervention bias. In addition, the study was performed in a single outpatient clinic, with subjects from a small population, and a single therapist, potentially affecting its reliability as evidence. Finally, there was also a lack of sufficient information regarding the treatment procedures in both groups, again, potentially resulting in intervention bias. A couple of studies[20,21] reported a large withdrawal rate, which was often due to patients’ disappointment at the lack of discernible benefit from the treatment, sometimes, they were practitioner-determined withdrawals. Additionally, type II errors (i.e. failing to detect a present effect) were made more probable as the sample sizes were small for three-arm trials. The sample size was also not calculated prior to analysis, however, the power analysis identified that the F-test noted differences between the groups. These differences were equal to those that were implied by the sample difference, heightening the probability of type 2 errors occurring. Cherkin et al.[19] used a single healthcare provider, which lowered the generalisability of their results. This could explain the absence of standardisation within the study and has the potential to lead to transfer and performance bias.
Despite these limitations, many strengths exist within the studies. One such strength is that within the studies, patients suffering from centralised pain were accurately selected. Another strength was that the therapists providing the treatment were experienced and competent in delivering both the orthopaedic MT and the McKenzie methods of treatment. Additionally, the VAS and RMDQ measurement tools have been reviewed as being sufficiently valid, justifying their use within the trials[28,29].
The evidence presented here supporting the effectiveness of McKenzie therapy in reducing pain and disability in patients with CLBP compared to MT is in accordance with a systematic review by Clare et al.[30]. In their study, the authors evaluated six RCTs that investigated the efficacy of McKenzie therapy in the treatment of back and neck pain. The results of this review show that for LBP patients, McKenzie therapy does result in a greater decrease in pain and disability in the short term to a greater extent than other standard therapies including MT. However, this review is constrained by several limitations. Firstly, the quality of the included trials was not restricted based on a minimum score but instead aimed to look at the relationship between trial quality and outcome because so few studies were included. Furthermore, in considering the individual quality items, it is evident that most included studies scored poorly on the validated quality items (randomisation, concealed allocation, blinding). It is hard to achieve therapist and patient blinding in trials of McKenzie therapy, blinding of assessors should be achievable. Concealed allocation is also achieved relatively easily, e.g. through the use of sealed opaque envelopes containing the allocation codes. In addition, no distinction was made in the studies reviewed between patients with back pain only and those with pain radiating into the lower limb.
The present systematic review differs from that of Clare et al.[30] in evaluating a variety of conservative interventions used for managing CLBP. Despite Clare et al.[30] including two studies[19,22] and reporting the same outcomes as the present review, the allocation of studies by active intervention differed. More specifically, the current study compared McKenzie therapy with MT in managing CLBP, while Clare et al.[30] investigated the efficacy of the McKenzie method for whole spinal pain in comparison to no treatment, sham treatment, or another treatment such as MT. Therefore, the present review is strengthened by being fully focussed on CLBP using McKenzie and manual therapy only without any other interventions and outcomes. Secondly, the present review utilised only high quality RCTs as determined using the PEDro scoring system (the lowest score was 6), while Clare et al.30 included trials which were not set for a minimum score, instead investigating the relationship between trial quality and outcome (the lowest score was 4).
The conclusions based upon this systematic review’s evidence remain unclear due to certain limitations. Firstly, only five RCTs were included within this study, and the RCTs were, themselves, not especially/particularly large-scale, which may prompt a lack of generalisability of the results found. This review only focused on studies that compared McKenzie method compared to MT alone. Additionally, the aforementioned limitations of the included studies further detract from the value of the evidence contained herein, though, as mentioned earlier, some of these limitations were necessary, considering the nature of the treatments involved. Due to the significant clinical and statistical differences (e.g. variations in the cohorts assessed, variations of the protocols used, and variations in the definitions used to assess output measures) across the included studies, a meta-analysis was not performed in this review. Another limitation of this review was that only studies published in the English language were included.
Conclusion
This review found that a group of selected measures of pain demonstrated that the McKenzie method was effective in the pain reduction in CLBP patients in the short term. Disability measures showed that the McKenzie method was better than the MT method at improving long term patient functionality. Due to a lack of available long term data regarding LBP treatments, it is difficult to establish any firm conclusions regarding the effect of treatments on factors other than pain and disability. Most studies included in this review were conducted without assessor- and therapist-blinding, therefore, the reliability of these studies is limited, although the importance of having blinding should not be overstated. Additionally, some of the sample sizes of the studies were too small to be generalised, making recommendation of the treatments assessed difficult to promote as routine clinical practice. It is evident that there is a dearth of methodologically sound and reliable RCTs in this area. The objective, therefore, for future research in this field, is to devise a question to guide research along a path (delineated with milestones), with an approved methodology, that would ultimately lead to more widely accepted conclusions.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Vos T, Flaxman A, Naghavi M, Lozano R, Michaud C. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010:a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tveito TH, Eriksen HR. United Kingdom back pain exercise and manipulation (UK BEAM) trial:is manipulation the most cost effective addition to “best care”? BMJ. 2005;330(7492):674. doi: 10.1136/bmj.330.7492.674-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haldeman S, Dagenais S. A supermarket approach to the evidence-informed management of chronic low back pain. Spine J. 2008;8(1):1–7. doi: 10.1016/j.spinee.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 5.Chou R, Loeser JD, Owens DK, Rosenquist RW. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain:an evidence-based clinical practice guideline from the American Pain Society. Spine. 2009;34(10):1066–77. doi: 10.1097/BRS.0b013e3181a1390d. [DOI] [PubMed] [Google Scholar]
- 6.NICE Guidelines. Low back pain and sciatica in over 16s:assessment and management NICE guideline. 2016 [Google Scholar]
- 7.Battié MC, Cherkin DC, Dunn R, Ciol MA, Wheeler KJ. Managing low back pain:attitudes and treatment preferences of physical therapists. Phys Ther. 1994;74(3):219–26. doi: 10.1093/ptj/74.3.219. [DOI] [PubMed] [Google Scholar]
- 8.Foster NE, Thompson KA, Baxter GD, Allen JM. Management of nonspecific low back pain by physiotherapists in Britain and Ireland. A descriptive questionnaire of current clinical practice. Spine. 1999;24(13):1332–42. doi: 10.1097/00007632-199907010-00011. [DOI] [PubMed] [Google Scholar]
- 9.Gracey JH, McDonough SM, Baxter GD. Physiotherapy management of low back pain:a survey of current practice in northern Ireland. Spine. 2002;27(4):406–11. doi: 10.1097/00007632-200202150-00017. [DOI] [PubMed] [Google Scholar]
- 10.McKenzie R, May S. The Lumbar Spine:Mechanical Diagnosis and Therapy. 2nd Ed. New Zealand: Spinal Publications; 2003. [Google Scholar]
- 11.Cherkin DC, Sherman KJ, Deyo RA, Shekelle PG. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain. Ann Intern Med. 2003;138(11):898–906. doi: 10.7326/0003-4819-138-11-200306030-00011. [DOI] [PubMed] [Google Scholar]
- 12.Assendelft WJJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. Cochrane database Syst Rev. 2004;(1):CD000447. doi: 10.1002/14651858.CD000447.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Sandoz R. The significance of the manipulative crack and of other articular noises. Ann Swiss Chiro Assoc. 1969;4:47–68. [Google Scholar]
- 14.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4 European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(2):192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain:a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. [DOI] [PubMed] [Google Scholar]
- 16.Machado L, Maher C, Herbert R, Clare H. The effectiveness of the McKenzie method in addition to first-line care for acute low back pain:a randomized controlled trial. BMC Med. 2010;8(1):10. doi: 10.1186/1741-7015-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Vet HC, Heymans M, Dunn K, Pope D. Episodes of low back pain:a proposal for uniform definitions to be used in research. Spine. 2002;27(21):2409–16. doi: 10.1097/01.BRS.0000030307.34002.BE. [DOI] [PubMed] [Google Scholar]
- 18.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials:a demographic study. Aust J Physiother. 2009;55(2):129–33. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 19.Cherkin DC, Deyo R a, Battié M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339(15):1021–9. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 20.Petersen T, Larsen K, Nordsteen J, Olsen S, Fournier G. The McKenzie Method Compared With Manipulation When Used Adjunctive to Information and Advice in Low Back Pain Patients Presenting With Centralization or Peripheralization. Spine. 2011;36(24):1999–2010. doi: 10.1097/BRS.0b013e318201ee8e. [DOI] [PubMed] [Google Scholar]
- 21.Paatelma M, Kilpikoski S, Simonen R. Orthopaedic manual therapy, McKenzie method or advice only for low back pain in working adults:A randomized controlled trial with one year follow-up. J Rehabil Med. 2008;40(10):858–63. doi: 10.2340/16501977-0262. [DOI] [PubMed] [Google Scholar]
- 22.Schenk RJ, Jozefczyk C, Kopf A. A Randomized Trial Comparing Interventions in Patients with Lumbar Posterior Derangement. J Man Manip Ther. 2003;11(2):95–102. [Google Scholar]
- 23.Kilpikoski S, Alen M, Paatelma M, Simonen R, Heinonen A, Videman T. Outcome comparison among working adults with centralizing low back pain:Secondary analysis of a randomized controlled trial with 1-year follow-up. Adv Physiother. 2009;11(4):210–7. [Google Scholar]
- 24.Sterne J, Gavaghan D, Egger M. Publication and related bias in meta-analysis:power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–29. doi: 10.1016/s0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- 25.Slavin R, Smith D. The Relationship Between Sample Sizes and Effect Sizes in Systematic Reviews in Education. Educ Eval Policy Anal. 2009;31(4):500–6. [Google Scholar]
- 26.Boutron I, Tubach F, Giraudeau B, Ravaud P. Blinding was judged more difficult to achieve and maintain in nonpharmacologic than pharmacologic trials. J Clin Epidemiol. 2004;57(6):543–50. doi: 10.1016/j.jclinepi.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 27.Portney LG, Watkins MP. Foundations of clinical research:applications to practice. 3rd ed. Prentice Hall; 2008. [Google Scholar]
- 28.Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2(2):175–84. [PubMed] [Google Scholar]
- 29.Roland M, Morris R. A study of the natural history of back pain. Part I:development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8(2):141–4. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50(4):209–16. doi: 10.1016/s0004-9514(14)60110-0. [DOI] [PubMed] [Google Scholar]


