Abstract
This systematic review aims to determine the effectiveness of proprioceptive neuromuscular facilitation (PNF) treatment techniques in adhesive capsulitis for decreasing pain and disability and increasing range of motion (ROM) and function. A thorough, computerized search was done using database search engines by two reviewers. After meticulous scrutiny and screening of 410 studies, according to the selection criteria, 10 full-text articles were included in the review and meta-analysis. All 10 studies had undergone a methodological quality assessment by the Physiotherapy Evidence Database Scale. Meta-analysis was done for external rotation, abduction ROM and pain. The most common PNF techniques used by most of the studies were, hold-relax and contract-relax in upper limb D2 flexion, abduction, and an external rotation pattern, while some studies used scapular PNF patterns. Among the 10 included studies, nine showed that the PNF group is superior in decreasing pain and reducing disability, increasing ROM, improving function. The meta-analysis also showed a significant effect size and that the PNF is superior than conventional physical therapy in decreasing pain, increasing external rotation, and abduction ROM
Keywords: Adhesive Capsulitis, Function, Pain, Proprioceptive Neuromuscular Facilitation, Range of Motion
Introduction
Adhesive Capsulitis (AC) is the most common disorder of the shoulder joint[1]. Currently, frozen shoulder and AC are the preferred terms and can be used interchangeably in clinical practice[2]. This condition is due to unknown etiology and is characterized by pain in the shoulder, which worsens at night, and a loss of range of motion (ROM) in all the three planes, but primarily in the abduction and external rotation of the shoulder[3]. Shoulder pain and stiffness contributes to severe disability[4]. Adhesive Capsulitis is generally classified into two categories: primary and secondary AC. Primary is associated with conditions such as, diabetes mellitus and thyroid disorders and secondary is due to shoulder injuries, rotator cuff tear, or post-surgical immobilization[5]. The condition occurs between the ages of 40-65 years and affects 3%-5% of the general population, 10-38% of patients with diabetes mellitus and thyroid disease[6].
Adhesive Capsulitis develops in four stages. Stage one is a painful stage, in which the patient develops gradual and insidious diffuse shoulder pain, which worsens at night and persists for less than three months and is associated with mild limitation of ROM. Stage two is a freezing stage, which is characterized by stiffness with significantly decreased active and passive ROM due to reduced capsular volume. This stage lasts for three to nine months. Stage three is the frozen stage, where the symptoms persist for 9-14 months and are characterized by shoulder stiffness and pain at the end of ROM or at night. Stage four is the thawing stage, in which ROM gradually improves due to capsular remodeling and is accompanied by minimal pain, which occurs between 15-24 months[7].
The management of Adhesive Capsulitis can either be conservative or surgical. Conservative treatment includes oral medications, intra-articular injections, and physical therapy. Studies have shown that most of the health professionals prefer conservative treatment with physiotherapy and analgesics for AC[7]. Studies have also demonstrated that rehabilitation is very effective in improving ROM and reducing pain, increasing function, followed by physical modalities[1]. Various physical therapy treatments commonly used in Adhesive Capsulits include, ice-pack, hot-pack, transcutaneous electrical nerve stimulation, and active and passive ROM exercises, joint mobilization techniques, proprioceptive neuromuscular facilitation (PNF), supervised home exercise programs, and Kinesio taping[8].
Kabat and Knott developed PNF treatment method in early 1950s[9]. The general exercises are performed as normal physiological joint movements in a single plane such as flextion (or) abduction (or) rotation. The concept of PNF is to enhance mobility, movement control, and joint coordination. This can be achieved by rotational diagonal patterns of movement through several stimuli and guidance provided by the therapist[10]. All the techniques of PNF are accomplished as per basic procedures, among them performing rotational patterns of movement is one of the chief component. Different techniques, such as rhythmic initiation, repeated contractions, rhythmic stabilization, combination of isotonics, dynamic reversals, hold-relax, and contract-relax can be applied to improve muscle strength and flexibility, respectively. Hold-relax, contract-relax techniques are based on the neurophysiology of reciprocal innervation, post-isometric relaxation (autogenic inhibition), and stress-relaxation[11].
There are studies about the application of PNF techniques in sports injuries, orthopedics[12], cardiorespiratory[13], and neurological conditions[14]. Recently, the application of these techniques in orthopedic conditions is evolving. However, studies have been conducted to find the effect of PNF treatment on Adhesive Capsulitis, however, there is conflicting evidence among them[9,15]. Even though some studies have recommended PNF, identifying which technique is better in treating AC is still debatable and needs to be answered.
Hence, the aim of the current paper is to review the effect of various PNF techniques applied to AC and to determine the effective treatment parameters. The other aim of the study is to conduct a meta-analysis to find out the effectiveness of PNF on improving shoulder external rotation and abduction ROM and reducing pain in AC.
Methodology
A thorough review was conducted by two reviewers on the PNF effect in AC using an electronic search strategy and other sources. Studies from 2000 to 2018 which are in English language were considered for the review.
Search methods
English database search engines, such as PUBMED, Google Scholar, PROQUEST, EBSCO HOST, MEDLINE, AC Digital Library, UpToDate, Saudi Digital Library, BMJ best practice, CINAHL, and Physiotherapy Evidence Database were used for the literature search. Some key words mentioned in the search strategy were AC, physical therapy, PNF, contract-relax, frozen shoulder, frozen shoulder contracture syndrome, stiff shoulder. We also conducted a literature search in other ways, like exploring the gray literature, hand searching for literature from the library, obtaining studies from the reference list of articles.
Selection of the studies
Studies which have included participants who are diagnosed with AC with pain and ROM as outcome measures were included. The encompassed studies should have used PNF alone or combined as the main treatment and compared to conventional physical therapy. The study design should be either randomized controlled trials (RCT) and quasi-experimental design
Studies with the diagnosis of shoulder impingement syndrome, rotator cuff tears, shoulder instability were excluded. Further studies which included subjects with shoulder pain due to neurological abnormalities (hemiplegia), disorders of bones such as fractures, osteoporosis, glenohumeral arthritis, and cervical pathology were omitted.
Data extraction
Data regarding the characteristics of studies, such as author, study design, interventions for experimental and control groups, details of the PNF intervention types, characteristics of the intervention, and treatment parameters were retrieved by the two reviewers. Mean and standard deviation of the outcome measures used in all the included studies was also extracted by the two reviewers. In the studies where there are no details of mean and standard deviation, reviewers personally communicated to the authors and gathered the data. The total number of participants, participants in each group, and participant characteristics (age, sex, and stage of AC) were also obtained by the two reviewers.
Methodological quality
The methodological quality of all the included studies was assessed by using a Physiotherapy Evidence Database Scale. If there was any disagreement among the reviewers, the opinion of a third reviewer was considered. The Physiotherapy Evidence Database Scale is an 11-item scale used to evaluate the quality of the RCTs of the physical therapy studies. This scale is based on the Delphi Consensus Technique. The total Physiotherapy Evidence Database scores for RCTs were ranged from 0-10. This range is further classified as 9-10 points (excellent), 6-8 points (good), 4-5 points (fair), 0-3 points (poor)[16,17].
Study selection for meta-analysis
Studies that evaluated pain on a continuous scale from 0 to 10, like the Visual Analog Scale (VAS) or the Shoulder Pain and Disability Index (SPADI), were included in this meta-analysis. ROM, which was measured in degrees of abduction and external rotation, were considered for the analysis.
Statistical analysis
We used SPSS version 21.0 for performing statistical analysis. For the meta-analysis of pain, abduction, and external rotation, the effect size was calculated by a correlation coefficient (r-value). Pre- and post-mean and standard deviation differences of experimental as well as control groups were used to calculate the effect size of each study. To produce a stabilized mean difference value, pre- and post-mean differences and standard deviation differences were averaged. For calculating the standard error, a stabilized mean difference value and a number of participating subjects were used. By using a stabilized mean difference value, a standard error, and 95% Confidence Interval (CI), we calculated the r-value.
Results
Results of search
After a thorough literature search through the electronic search engines mentioned in methods, a total of 410 citations were located. Out of the 410 citations, 182 citations were immediately removed, as they were duplicate records. After removing duplicate records atotal of 228 records remained. By screening abstracts from 228 records, 185 records were also excluded. A total of 43 full-text articles were examined for eligibility. Out of 43 articles, 33 studies were excluded for several reasons, including, those with PNF intervention in shoulder impingement syndrome (seven), three studies with hemiplegic shoulder, five studies on interventions in hemiplegic lower limb, one study with intervention in myofascial pain syndrome, three studies with supraspinatus tear, one study with shoulder surgery, one study including a heterogeneous group, one study gave PNF as adjunctive treatment, four studies on healthy population, two studies on knee joints, two studies on calcified tendinitis, one study without necessary data, one study was a case study, one study was in Korean language. Finally, a total of 10 studies were included for systematic review. The details of the included studies were shown in flowchart Figure 1.
Figure 1.
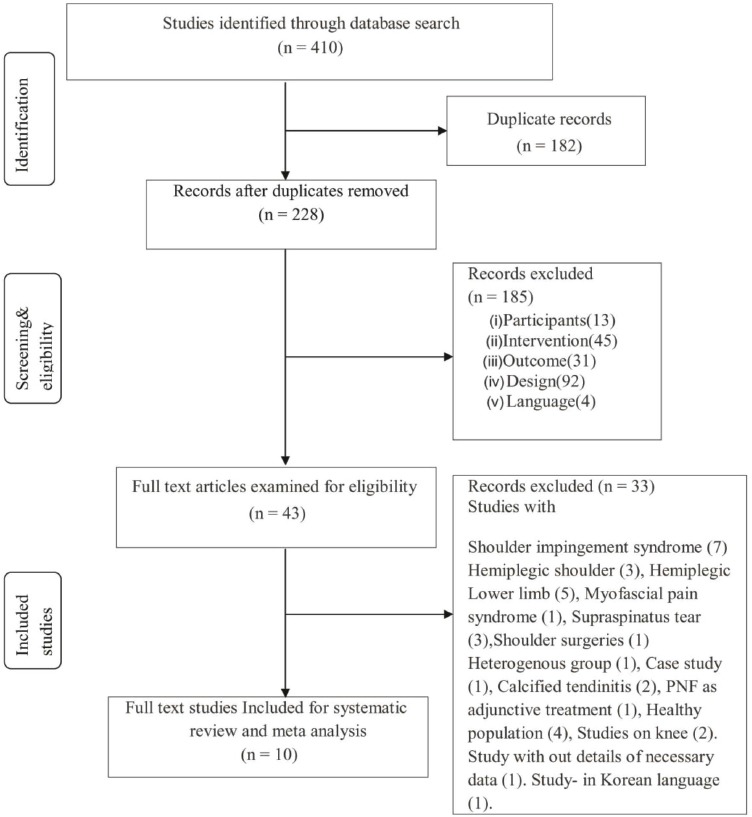
Flow diagram of search strategy, screening and included studies.
Methodological quality assessment
The Physiotherapy Evidence Database score of all the included studies are revealed in Table 1. Among the 10 studies, six studies were of good quality, two studies were of average quality, and two studies were of poor quality.
Table 1.
Methodological quality of studies by physiotherapy evidence database scale.
| Author | Criteria | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total | Classification |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mahendran et al[19] | Yes | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 3 | Poor |
| Mehta et al[2] | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 5 | Average |
| Renjitha L[20] | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | Good |
| Kalasva N et al[23] | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | Good |
| Akbas et al[22] | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | Good |
| Kalita et al[31] | Yes | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 4 | Average |
| Ravichandran et al[21] | Yes | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 8 | Good |
| Pande et al[3] | Yes | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 7 | Good |
| Prasanna et al[18] | Yes | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 3 | Poor |
| Balci et al[4] | Yes | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Good |
Characteristics of the included studies
In this systematic review, reviewers included 10 eligible studies. The studies were conducted between the years 2013 to 2017. The number of subjects in each study varied between 24 to 60. All the studies had two comparison groups, except one in which there were three comparison groups[4]. Among the 10 studies, nine were RCTs and one was a quasi-experimental design[18]. The characteristics of the included studies in this systematic review were provided in Table 2.
Table 2.
Charactersistics of the studies Included in the review.
| Author, year | Total participants | Study Design | Type of intervention (Number of Subjects):-Intervention | PNF Technique (Dosage) | Treatment Frequency | Outcome (measures of assessment) | Conclusion |
|---|---|---|---|---|---|---|---|
| Mehta H, 2013[2] | 30 | RCT | PNF group: (15 Subjects): - PNF stretching by Hold-relax Control group: (15 Subjects): - Self-stretching. | Hold-Relax for internal rotators (6 Sec of isometric contraction with 10 seconds relaxation, 3 times repetition) | Once in a day 5 d/wk during 4 wks. | - Pain and Function (SPADI) - External rotation, and Abduction (ROM) |
Both groups are effective, but the PNF group is better than Control in improving ROM and decreasing pain and disability. |
| Mahendran P, 2013[19] | 30 | RCT | PNF group: (15 Subjects): - Contract-relax, joint mobilization, and moist heat Control group: (15 Subjects): - Mobilization and moist heat Codman’s exercises as the home program for both the groups | Contract-Relax in D2 Flexion Pattern for Adductors and internal rotators (10-15 times) | Once in a day 5 d/wk during 4 wks. | - Pain (VAS) - External rotation, and Abduction (ROM) |
PNF combined with joint mobilization is better at increasing ROM, and decreasing pain |
| Renjitha L, 2013[20] (Unpublished dissertation) | 50 | RCT | PNF group: (25 Subjects): - PNF contract-relax, coracohumeral ligament stretching and pendular exercises Control group: (25 Subjects): - Pendular exercises | PNF contract-relax for Internal rotators (7 Sec contraction and 15 Sec of relaxation in external rotation, 5 repetitions) Followed by facilitation of D2 Flexion patterns for 5 repetitions. | Once in a day 2 d/wk during 4 wks. | - Pain (VAS) - Pain, and Function (SPADI) - External rotation (ROM) |
The PNF treatment group is better than control in improving ROM of external rotation , function and decreasing pain |
| Kalasva NK, 2014[23] | 30 | RCT | PNF group: (15 Subjects): - myo facial release, Contract-relax PNF Control group: (15 Subjects): -Supine relaxed position for 10 minutes | PNF contract-relax to subscapularis and internal rotators (7 Sec of contraction and 15 Sec of relaxation in external rotation, 5 repetitions) Followed by facilitation of D2 Flexion patterns for 5 repetitions. | Single Session | - External rotation (ROM) | PNF in combination with myo fascial release is better at improving ROM than the control group |
| Kalita A, 2015[31] | 60 | RCT | PNF group: (30 Subjects): -Contract-relax, joint mobilization and pendular exercise. Control group: (30 Subjects): -Pendular exercise | Contract-Relax for internal rotators (7 Sec contraction and 15 Sec of relaxation in external rotation, 5 repetitions) Followed by facilitation of D2 Flexion patterns for 5 repetitions. | Once in a day 2 d/wk during 4 Wks | - Pain and Function (SPADI) - External rotation (ROM) |
Both groups are effective, but the PNF group is better than Control in improving ROM, function and decreasing pain. |
| Akbas E , 2015[22] | 36 | RCT | PNF group: (18 Subjects): -PNF hold relax in D2 Flexion Pattern, Scapular Anterior elevation, and Posterior Depression patterns, Ultrasound, and Hot pack Control group: (18 Subjects): -Ultrasound and Hot pack Wall and wand exercise as a home program for both the groups | Hold-relax (5-8 Sec isometric contraction for improving D2 flexion pattern) Repeated stretch techniques for anterior elevation and posterior depression scapular pattern | Once in a day 5 d/wk during 3 Wks | -Pain (VAS) - Pain and Function (SPADI) - External rotation, Internal Rotation, Abduction & Flexion (ROM) - postural deformities (Postural analysis by inspection) - Scapula evaluation (lateral scapular slide test) |
PNF group is better in improving ROM, function and decreasing pain |
| Ravichandran H, 2015[21] | 60 | RCT | PNF group: (30 Subjects): -D2 flexion and extension patterns Control group: (30 Subjects): -Muscle energy technique for Flexion, Extension, Abduction, External rotation and Internal Rotation) | D2 Flexion and Extension pattern (8 repetitions per set, 2 sets per session, 1 session per day Each repetition held for 5-10 Sec) | Once in a day 5 d/wk during 2 Wks | - Flexion, Extension, Abduction, External rotation and Internal Rotation (ROM) - Pain (Pennsylvania shoulder score first subset) |
When compared with the muscle energy technique group, PNF technique was effective in restoring ROMof abduction, external rotation, internal rotation, function and relieving pain |
| Balci N, 2016[4] | 53 | RCT | PNF group: (18 Subjects): -Scapular PNF, hot pack, ultra sound and transcutaneous electrical nerve stimulation Control group: (17 Subjects): -Hot pack, ultra sound and transcutaneous electrical nerve stimulation Classic exercise group: (18 Subjects): -Stretching and strengthening exercise | PNF all scapular patterns with Rhythmic initiation and repeated contractions Technique. (20 repetitions with rest for 20 Sec for one hour) | Single session | - Pain (VAS) - Flexion, Abduction (ROM) - Scapular dyskinesis (Lateral scapular slide test) |
Pre and post all the 3 groups were shown significant differences. But between the groups, there was no statistically significant difference |
| Pande P, 2017[3] | 30 | RCT | PNF group: (15 Subjects): -PNF Hold-Relax and the ultrasound. Control group: (15 Subjects): -Mobilization and ultrasound | Hold-Relax for improving D2 Flexion pattern (10 Sec antagonist muscle contraction followed by voluntary relaxation) 5 times per session | Once in a day 3d /wk during4wks. | - Pain (VAS) - External rotation and Abduction (ROM) |
Both groups are effective, but the PNF group is better than Control in improving ROMand decreasing pain |
| Prasanna KJ, 2017[18] | 24 | Quasi-Experimental | PNF group: (12 Subjects): -Scapular PNF, wax therapy, stretching, and shoulder mobilization Control group: (12 Subjects): -Wax therapy, stretching, and shoulder mobilization | Scapular PNF in repeated contraction and rhythmic initiation in all patterns (20 repetitions with rest of 20 Sec between each repetition) | No details during 6 wks. | - Pain (VAS) - External rotation, Flexion and Abduction (ROM) - Scapular dyskinesia (Lateral scapular slide test) - Function (Simple shoulder test) |
Both groups are effective, but Scapular PNF group is better than Control. |
Note: wk=week, d=days; PNF: proprioceptive Neuromuscular Facilitation, ROM: Range of Motion, VAS: Visual Analog Scale, SPADI: Shoulder pain and Disability Index.
The age range of the participant in all the studies was ranging from 40 to70 years. Out of 10 studies, 7 studies included subjects who are in stage two of AC, but one study included subjects in the acute stage of AC[19] and two studies did not mention about the stage of AC[20,21].
Out of 10 studies, only two[2,21] used isolated PNF as an intervention in the experimental group. However, the remaining eight studies combined other physical therapy adjunctive treatments like joint mobilization, wax therapy, transcutaneous electrical nerve stimulation, ultra sound, moist heat, short wave diathermy, pendular exercise, myofascial release, and muscle energy techniques with the PNF techniques.
The PNF techniques used were the hold-relax and contract-relax for the adductors and internal rotators of the shoulder. Rhythmic initiation and repeated contractions for scapular patterns were other techniques used in some studies. The most common upper limb pattern facilitated was Diagonal 2 - flexion, abduction, and external rotation. Two studies used rhythmic initiation and repeated contractions for all scapular patterns. One study used rhythmic initiation for anterior elevation and posterior depression of scapular pattern[22]. In the experimental groups, for performing hold-relax and contract-relax, the duration of contraction was ranged from 5 to 10 seconds, while the time for relaxation ranged from 10 to 20 seconds. Number of the repetitions ranged between 3 to 20. The dosage of treatment per week ranged from 2 to 5 times per week. Total treatment duration ranged from 3 to 6 weeks, however, most of the studies preferred four weeks. Out of the 10 studies, only two studies were conducted as single treatment sessions[4,23]. However, one study did not mention the details of the sessions per week[18].
The treatments used in control group were self-stretching, joint mobilization, muscle energy technique, transcutaneous electrical nerve stimulation, ultra sound, wax, and moist heat. These treatments applied either individually (or) in combination. Pendular/Codman exercise wall and wand exercises had been given as a home program for both groups in some studies[19,22].
The common outcome measures used in the studies were ROM, pain, and functional performance. The pain was measured by VAS or SPADI or Pennsylvania shoulder score. Disability and function were evaluated by SPADI (or) a Simple Shoulder Test. Some studies used other outcome measures like the lateral scapular slide test[4,18,22] postural analysis[22]. ROM for shoulder flexion, abduction, external rotation, internal rotation, the extension was measured by using a goniometer in degrees.
Out of 10 studies, 9 concluded that both groups are effective in improving outcome measures, but PNF groups are superior and statistically significant in improving outcomes, except in one study by Balci et al.[4], which conducted a single session and demonstrated that there is no significant difference between groups, however, all the groups had shown significant differences after a single session of treatment interventions.
Meta-analysis of external rotation, abduction, and pain
The meta-analysis of external rotation, abduction ROM, and pain were performed by calculating the effect size of each study using the correlation coefficient r-value. The details of the included studies according to outcome variables for meta-anlaysis were shown in Table 3. A change in the external rotation range was obtained from nine studies. The effect size of the nine studies ranged from-0.12 to 0.90. The total effect size was 0.59, which shows very good results for PNF treatment compared to other treatments for improving external rotation ROM. The results of the analysis for external rotation ROM represented in the forest - plot (Figure 2). Effect size, lower limits, and upper limits of 95% CI are represented in Table 4.
Table 3.
Studies included for meta-analysis according to outcome variables.
| Author of the study & Year | Exteranl Rotation ROM | Abduction ROM | Pain |
|---|---|---|---|
| Mahendran et al[19], 2013 | ✓ | ✓ | ✓ |
| Mehtha et al[2], 2013 | ✓ | ✓ | ✓ |
| Renjitha L[20], 2013 | ✓ | ✗ | ✓ |
| Kalasva et al[23], 2014 | ✓ | ✗ | ✗ |
| Akbas et al[22], 2015 | ✓ | ✓ | ✓ |
| Kalitaet al[31], 2015 | ✓ | ✗ | ✓ |
| Ravichandran et al[21], 2015 | ✓ | ✓ | ✗ |
| Balci etal[4], 2106 | ✗ | ✓ | ✓ |
| Pande et al[3], 2017 | ✓ | ✓ | ✓ |
| Prasanna et al[18], 2017 | ✓ | ✓ | ✓ |
Figure 2.
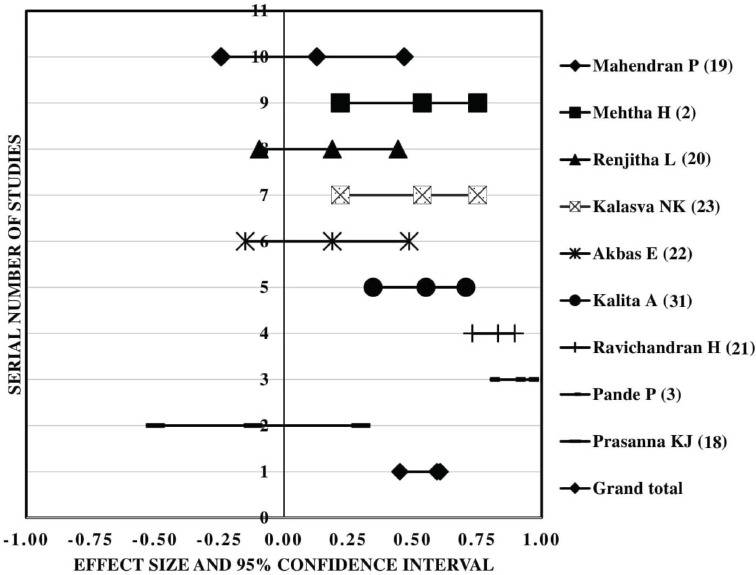
Forest plot of external rotation range of motion.
Table 4.
Effect size values of the external rotation range of motion.
| Author of the study | No of Subjects | Effect Size | Standard Error | 95% CI (Lower) | 95% CI (Upper) | p-value |
|---|---|---|---|---|---|---|
| Mahendran et al[19] | 30.00 | 0.13 | 0.19 | -0.24 | 0.47 | 0.072 |
| Mehtha et al[2] | 30.00 | 0.54 | 0.19 | 0.22 | 0.75 | 0.000 |
| Renjitha L[20] | 50.00 | 0.19 | 0.15 | -0.10 | 0.44 | 0.007 |
| Kalasva et al[23] | 30.00 | 0.54 | 0.19 | 0.22 | 0.75 | <0.05 |
| Akbas et al[22] | 36.00 | 0.19 | 0.17 | -0.15 | 0.49 | 0.161 |
| Kalitaet al[31] | 60.00 | 0.55 | 0.13 | 0.35 | 0.71 | 0.000 |
| Ravichandran et al[21] | 60.00 | 0.83 | 0.13 | 0.73 | 0.90 | 0.000 |
| Pande et al[3] | 30.00 | 0.90 | 0.19 | 0.80 | 0.95 | 0.011 |
| Prasanna et al[18] | 24.00 | -0.12 | 0.22 | -0.50 | 0.30 | <0.05 |
| Grand Total | 350.00 | 0.59 | 0.06 | 0.45 | 0.61 | 0.000 |
An effect size of pain was calculated from eight studies. The effect size of the studies ranged from -0.31 to -0.87. Total effect size is -0.57, which shows the good effect of PNF treatment in reducing pain compared to other treatments. The results of the analysis are represented in the forest-plot (Figure 3). Effect size, upper and lower limits of 95% CI are represented in Table 5.
Figure 3.
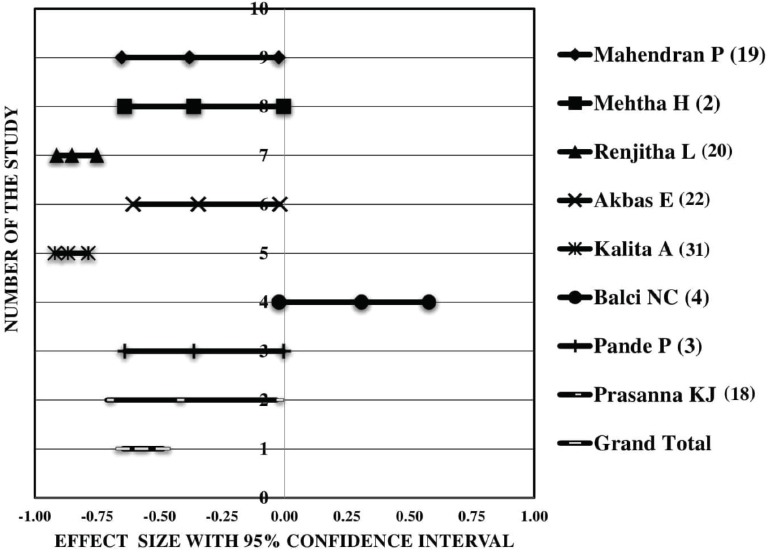
Forest plot of pain.
Table 5.
Meta-analysis of pain and total effect size, upper and lower limits of 95% CI.
| Author of the study | No of Subjects | Effect Size | Standard Error | 95% CI (Lower) | 95% CI (Upper) | p-value |
|---|---|---|---|---|---|---|
| Mahendran et al[19] | 30 | -0.38 | 0.19 | -0.65 | -0.02 | 0.028 |
| Mehtha et al[2] | 30 | -0.36 | 0.19 | -0.64 | 0.00 | <0.05 |
| RenjithaLet al[20] | 50 | -0.85 | 0.15 | -0.91 | -0.75 | 0.000 |
| Akbas et al[22] | 36 | -0.35 | 0.17 | -0.61 | -0.02 | 0.048 |
| Kalitaet al[31] | 60 | -0.87 | 0.13 | -0.92 | -0.79 | 0.000 |
| Balci et al[4] | 36 | 0.31 | 0.17 | -0.02 | 0.58 | >0.05 |
| Pande et al[3] | 30 | -0.36 | 0.19 | -0.64 | 0.00 | 0.004 |
| Prasanna et al[18] | 24 | -0.43 | 0.22 | -0.71 | -0.03 | <0.05 |
| Grand total | 296 | -0.57 | 0.06 | -0.65 | -0.49 | 0.000 |
A change in abduction was obtained from seven studies. The effect size of the seven studies ranged from -0.02 to 0.62. The total effect size of analysis is 0.41, which shows PNF treatment is good in improving abduction ROM when compared to other treatments. The results of the analysis represented on the forest-plot (Figure 4). Effect sizes, upper and lower limits of 95%CI are represented in Table 6.
Figure 4.
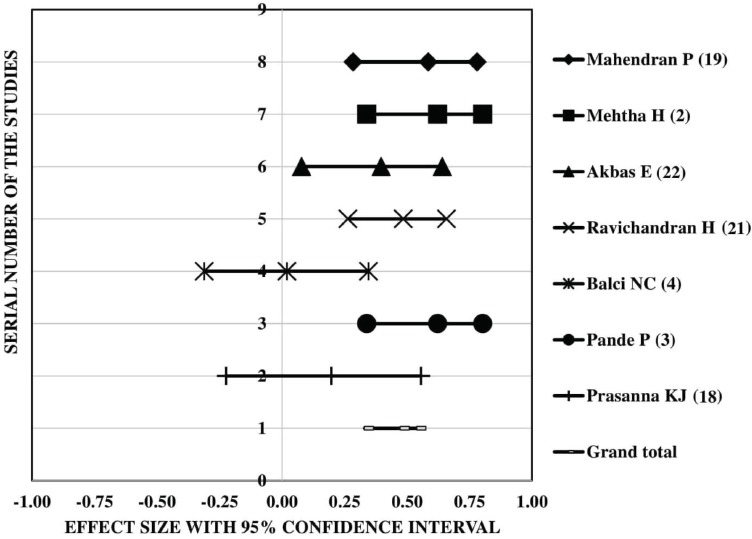
Forest plot of abduction range of motion.
Table 6.
Meta-analysis of abduction and total effect size, upper and lower limits of 95%CI.
| Author of the study | No of Subjects | Effect Size | Standard Error | 95% CI (Lower) | 95% CI (Upper) | p-value |
|---|---|---|---|---|---|---|
| Mahendran et al[19] | 30.00 | 0.58 | 0.67 | 0.28 | 0.78 | <0.001 |
| Mehtha et al[2] | 30.00 | 0.62 | 0.73 | 0.34 | 0.80 | 0.000 |
| Akbas et al[22] | 36.00 | 0.40 | 0.42 | 0.08 | 0.64 | 0.006 |
| Ravichandran et al[21] | 60.00 | 0.49 | 0.53 | 0.26 | 0.66 | 0.000 |
| Balci et al[4] | 36.00 | -0.02 | 0.02 | -0.35 | 0.31 | >0.05 |
| Pande et al[3] | 30.00 | 0.62 | 0.73 | 0.34 | 0.80 | 0.001 |
| Prasanna et al[18] | 24.00 | -0.20 | 0.20 | -0.56 | 0.22 | <0.05 |
| Grand Total | 246.00 | 0.41 | 0.07 | 0.29 | 0.51 | 0.000 |
Discussion
There are two main objectives for this study. One is to perform a systematic review to find the effect of various PNF techniques applied to AC and to determine the effective treatment parameters. The second objective of this study is to conduct a meta-analysis to find out the effectiveness of PNF on improving shoulder external rotation and abduction ROM and reducing pain in AC. The results of the systematic review had shown that, the most common PNF techniques which were shown to be effective in AC were hold and contract relax in uppper limib patterns. These techniques were given once in a day, 2-5 times per week for a total of 3-4 weeks duration. The results of meta-analysis had shown that PNF techniques are effective in reducing pain, increasing external rotation and abduction ROM in Adhesive Capsulitis when given alone or in combination with the other physical therapy interventions.
A recent systematic review conducted by Wanderely et al.[24] also showed similar results like our review that ROM could be improved without any adverse effects in PNF groups better than other conventional groups. They compared the effect of PNF to other stretching modalities on ROM and adverse effects in 1,864 healthy young adults in 46 studies. The PNF techniques used in their studies are hold-relax and contract-relax. These PNF interventions were compared with muscle stretching exercise and soft tissue mobilization techniques. The Wanderely review also demonstrated a significant difference in improving ROM in PNF groups compared to the control groups without any adverse effects.
In AC limitations in the ROM can be attributed to the capsular pattern of restriction i.e. greater limitation in the external rotation than abduction[25]. The anterior rotator cuff (Subscapularis) and internal rotators contraction will restrict the external rotation ROM. As external rotation is required during elevation, flexion and abduction of shoulder, any restriction of external rotation further limits in abduction and flexion ROM[26]. Most of the authors applied hold-relax or contract-relax techniques to these reflex guarding muscles like internal rotators and adductors in upper limb D2 flexion, abduction and external rotation pattern.
The improvements in opposite ROM are ascribed to the principle of autogenic inhibition or post-isometric relaxation[11]. The authors applied these techniques with six to seven seconds of contraction followed by relaxation 15 seconds in external rotation and repeated five times, which may have influenced the relaxation of internal rotators and subscapularis muscles by autogenic inhibition. After application of techniques, the authors facilitated the upper limb D2 flexion, abduction, and external rotation patterns that could be facilitated abductors and external rotator muscles and gained ROM in external rotation, abduction.
While performing PNF techniques the process of autogenic inhibition (or) post-isometric relaxation stimulates the golgi tendon organs, when a targeted muscle is maximally contracted which in turn sends the inhibitory impulse through Ib afferent nerve fibers to the inhibitory interneurons in the spinal cord. These inhibitory interneurons further inhibit the alpha motor neuron of the same muscle to relax. This theory explains the possibility of relaxation in the inhibiting muscle during the contract-relax and hold-relax techniques of PNF[27].
Following PNF stretching the opposite muscles are contracted actively by the descending input from higher centers. This contraction of opposite muscles facilitates Ia afferent fibers which in turn excite the Ia inhibitory interneuron in the spinal cord which has got an inhibitory effect on the alpha motor neuron of the targeted muscle. This mechanism is known as reciprocal inhibition through which targeted muscle, which is causing the restriction will relax & elongate more[28]. During PNF stretching the targeted muscle is held in a stretch position in the opposite action, this will overcome the resistance produced by viscous material in musculotendinous unit for elongation. This increase in the length of musculotendinous unit is due to a property called creep. This whole mechanism is known as stress-relaxation by which muscular tendinous unit also elongates in the targeted muscle[27].
The probable mechanism of reducing pain in PNF techniques could be explained by the gate control theory. During PNF activities the afferent inputs from the muscle spindles, joints, tendons, and capsule could inhibit the pain transmission at the dorsal grey horn laminae of the spinal cord as proposed by pain gate theory[27]. There is the existence of alterations of scapular kinematics in patients with AC. Which in turn affects the normal scapula-humeral rhythm and restriction of shoulder elevation[29]. The altered scapular kinematics can restrict scapular depression, downward rotation, anterior tilt, posterior tilt, external rotation, and causes excessive upward rotation. Downward rotation & depression restricted due to the tightness of upper trapezius, rhomboids, and superior capsule. Restriction of scapular posterior tilt is because of the tightness of lower serratus anterior, pectoralis minor and anterior capsule[30]. Studies that have applied scapular patterns combined with upper limb D2 flexion, abduction, external rotation shown effective in improving ROM possibly due to correction in the scapular kinematic pattern.
The limitations of the current review were combining RCTs with one quasi-experimental study, combining single-session studies with multiple session studies, and combining various methods of PNF treatments. The future RCTs should take care of the following aspects like: 1) methodological quality of the studies should follow the Physiotherapy Evidence Database guidelines, 2) incorporate adherence in their studies, 3) consider other quantitative outcome measures like scapular kinematics, muscle strength, movement analysis and quality of life, 4) experimental group should be having only PNF treatment rather than combining with conventional physical therapy. Future reviews should try to combine a single type of studies, isolated techniques of PNF, long-term follow-up to see the effectiveness on AC.
Conclusion
Among the 10 included studies, nine showed that the PNF is superior than conventional physical therapy in decreasing pain, increasing ROM, improving function, and reducing disability. In the meta-analysis also, the PNF group showed superior improvements than the control groups, with an effect size of 0.59, 0.41, and -0.57 for shoulder external rotation, abduction, and pain, respectively. The contract and hold relax techniques of PNF applied in upper limb patterns were shown to be effective in decreasing pain and increasing ROM and function in subjects with Adhesive Capsulitis.
Acknowledgements
We sincerely thank the Deanship of Scientific Research, King Khalid University, Abha, Kingdom of Saudi Arabia for funding this research project numbered R.G.P.1/133/40.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1:180–189. doi: 10.1007/s12178-008-9031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta H, Joshi P, Trambadia H. Effectiveness of pnf stretching and self stretching in Patients with adhesive capsulitis-a comparative study. Indian J Physiother Occup Ther. 2013;7(1):47–52. [Google Scholar]
- 3.Pande P, Arora B, Rishi P. Effect of pnf and joint mobilization along with ultrasound on abduction and external rotation range of motion and pain in patients with frozen shoulder. Int J yoga Physiother Phys Edu. 2017;2(4):64–67. [Google Scholar]
- 4.Balcı NC, Yuruk ZO, Zeybek A, et al. Acute effect of scapular proprioceptive neuromuscular facilitation (PNF) techniques and classic exercises in adhesive capsulitis:a randomized controlled trial. J Phys Ther Sci. 2016;28:1219–1227. doi: 10.1589/jpts.28.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan HBY, Pua PY, How CH. Physical therapy in the management of frozen shoulder. Singapore Med J. 2017;58(12):685–689. doi: 10.11622/smedj.2017107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelley MJ, Mcclure PW, Leggin BG. Frozen shoulder:evidence and a proposed model guiding rehabilitation. J Orthop Sport Phys Ther. 2009;39(2):135–148. doi: 10.2519/jospt.2009.2916. [DOI] [PubMed] [Google Scholar]
- 7.Georgiannos D, Markopoulos G, Devetzi E, et al. Adhesive capsulitis of the shoulder is there consensus regarding the treatment?a comprehensive review. Open Orthop J. 2017;28(11):65–76. doi: 10.2174/1874325001711010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alptekin H, Aydın T, İflazoğlu E. Evaluating the effectiveness of frozen shoulder treatment on the right and left sides. J Phys. 2016;28(1):207–212. doi: 10.1589/jpts.28.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee BK. Effects of the combined PNF and deep breathing exercises on the rom and the vas score of a frozen shoulder patient:single case study. J Exerc Rehabil. 2015;11(5):276–281. doi: 10.12965/jer.150229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mavromoustakos S, Beneka A, Malliou V, Adamidis A, Kellis E, Kagiaoglou A. Effects of a 6-week proprioceptive neuromuscular facilitation intervention on pain and disability in individuals with chronic low back pain. PANR Journal. 2015 [Google Scholar]
- 11.Adler SS, Beckers D, Buck M. Pnf in practice:an illustrated guide. 3rd ed. Germany: Springer; 2008. [Google Scholar]
- 12.Maicki T, Bilski J, Szczygiel E, et al. Pnf and manual therapy treatment results of patients with cervical spine osteoarthritis. J Back Musculoskelet Rehabil. 2017;30(5):1095–1101. doi: 10.3233/BMR-169718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paulraj M, Shristhudhi S, Supriya K, et al. Effectiveness of pnf of respiration to improve the exercise capacity in patients with copd:a pilot study. Int J World Res. 2017;1(35):1–6. [Google Scholar]
- 14.Mann DK, Raja NAR, Bhardwaj N, et al. Effect of Proprioceptive neuromuscular facilitation in hemiplegic gait a randomized trial of 4 Weeks and a follow up after 2 Weeks. Indian J Physiother Occup Ther - An Int J. 2013;7(3):59–64. [Google Scholar]
- 15.Das M, Vadivelan K, and Sivakumar VPR. Effectiveness of subscapularis soft tissue mobilization versus proprioceptive neuromuscular facilitation on glenohumeral external rotation in periarthritis shoulder. International Journal of Current Research. 2017;9(12):63484–9. [Google Scholar]
- 16.Foley NC, Bhogal SK, Teasell RW, et al. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys Ther. 2016;86:817–824. [PubMed] [Google Scholar]
- 17.Teasell R, Foley N, Salter K, et al. The stroke rehabilitation evidence-based review. 17th ed. Ottawa, Ontario, Canada: Canadian Stroke Network; 2016. [Google Scholar]
- 18.Prasanna KJ, Rajeswari R, Vpr S. Effectiveness of scapular proprioceptive neuromuscular facilitation (pnf) techniques in adhesive capsulitis of the Shoulder Joint. J Physiother Res. 2017;1(2):9. [Google Scholar]
- 19.Mahendran P, Chetia D. Combined effects of joint mobilization with proprioceptive neuromuscular facilitation in Subjects with adhesive capsulitis of shoulder. J CAR Institute of Med Sci. 2013;6(1):5–11. [Google Scholar]
- 20.Renjitha L. The Effects of additional propriceptive neuromusculer facilitation over conventional therapy in Patients with adhesive capsulitis [Internet] Rajiv Gandhi University of Health Sciences 2013. Available from: http://52.172.27.147:8080/jspui/bitstream/123456789/9106/1/Renjitha.l-MPT.pdf .
- 21.Ravichandran H, Balamurugan J. Effect of proprioceptive neuromuscular facilitation stretch and muscle energy technique in the management of adhesive capsulitis of the shoulder. Saudi J Sport Med. 2015;15(2):170–175. [Google Scholar]
- 22.Akbaş E, Güneri S, Taş S, et al. The effects of additional proprioceptive neuromuscular facilitation over conventional therapy in patients with adhesive capsulitis. Fiz Rehabil. 2015;26(2):78–85. [Google Scholar]
- 23.Kalasva NK, Shukla YU. To study the immediate effect of myofascial release with proprioceptive neuromuscular facilitation for Subscapularis on Glenohumeral External Rotation in shoulder periarthritis - an interventional study. Indian J Phys Ther. 2014;2(2):30–33. [Google Scholar]
- 24.Wanderley D, Lemos A, Moretti E, et al. Efficacy of proprioceptive neuromuscular facilitation compared to other stretching modalities in range of motion gain in young healthy adults:a systematic review. Physiother Theory Pract. 2018:1–21. doi: 10.1080/09593985.2018.1440677. [DOI] [PubMed] [Google Scholar]
- 25.Lee SY, Lee KJ, Kim W, et al. Relationships between capsular stiffness and clinical features in adhesive capsulitis of the shoulder. PM R. 2015;7(12):1226–34. doi: 10.1016/j.pmrj.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 26.Hollmann L, Halaki M, Kamper SJ, et al. Does muscle guarding play a role in range of motion loss in patients with frozen shoulder? Musculoskelet Sci Pract. 2018;37:64–68. doi: 10.1016/j.msksp.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Hindle K, Whitcomb T, Briggs W, et al. Proprioceptive neuromuscular facilitation (pnf):its mechanisms and effects on range of motion and muscular function. J Hum Kinet. 2012;31(1):105–113. doi: 10.2478/v10078-012-0011-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharman MJ, Cresswell AG, Riek S, et al. Proprioceptive neuromuscular facilitation stretching mechanisms andclinical implications. Sports Med. 2006;36(11):929–939. doi: 10.2165/00007256-200636110-00002. [DOI] [PubMed] [Google Scholar]
- 29.Ludewig PM, Jonathan F, Reynolds P. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sport Phys Ther. 2009;39(2):90–104. doi: 10.2519/jospt.2009.2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Endo K, Hamada J, Suzuki K, et al. Does scapular motion regress with aging and is it restricted in patients with idiopathic frozen shoulder? Open Orthop J. 2016;10(16):80–88. doi: 10.2174/1874325001610010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalita A, Milton A. The combined effectiveness of glenohumeral end-range mobilization and contract-relax technique for glenohumeral internal rotators in subjects with adhesive capsulitis. Int J Physiother. 2015;2(5):691–697. [Google Scholar]


