Abstract
Objective
To analyze the relationship between age and perioperative complications of spine surgery in a Japanese cohort with the longest average life expectancy in the world.
Methods
Patients with spinal stenosis who underwent standard spine surgery without instrumented fusion were divided into 4 groups: adults (20–64 years), the young-old (65–74), the middle old (75–84), and the oldest-old (≥85). Data on medical complications, surgical complications, and deaths within 30 days of index surgery were compared across the groups. Risk factors for complications were identified through multivariate analysis.
Results
A total of 584 patients underwent 673 operations: 35% were performed on adult patients, 33% on the young-old, 27% on the middle old, and 5% on the oldest-old. The rates of total or [major] medical complications significantly increased with age (8% [0.8%], 11% [0.9%], 27% [3.9%], 45% [9.1%], respectively; p<0.001 [p=0.003]), whereas those of surgical complications did not differ (11%, 8.1%, 14%, 9.1%, respectively; p=0.25). Independent risk factors for medical complications were an age of 75 years or older (75–84: odds ratio [OR], 5.1; ≥85: OR, 6.2) and American Society of Anesthesiologists (ASA) physical status classification III (OR, 5.4). Two patients older than 85 years died from medical complications.
Conclusion
The complications of spine surgery increased in the middle and oldest-old patients because of medical complications; however, most were minor and treatable. Major complications were associated with preoperative medical comorbidities and their severities; therefore, most elderly patients with low ASA physical status classification (≤II) may benefit from spine surgery.
Keywords: Aging society, Perioperative complication, Medical complication, Surgical complication, Morbidity, Mortality
INTRODUCTION
Advances in medicine and medical services have increased the average life expectancy worldwide [1,2]. In Japan, the percentage of the population aged 65 years or older was 27.7% in 2017, which was the highest globally, and will reach 31.2% in 2030 [2]. Japan, therefore, has been facing the future of the world population aging. The prevalence of degenerative spinal diseases is expected to increase with population aging. Patient factors, particularly age, may have an impact on the rate of complications of spine surgery [3]. Improvements in the outcomes of spine surgery will contribute to a longer and better quality of life.
The relationship between age and the incidence of complications in patients undergoing spine surgery has been extensively examined; however, few studies have compared the incidence of complications among groups stratified by age [1,4-16]. A previous study focused on patients aged 65 years or older [6,17], while another study examined patients aged 75 years or older [9,13,15,16]. Most studies have failed to include patients older than 85 years. The majority of developed countries have set the age of retirement at 60 to 65 years; however, the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society declared that “75 is the new 65” based on data regarding the physical and mental health of the elderly [18]. Furthermore, the types of complications—medical or surgical—associated with poor outcomes currently remain unclear [10,12,19]. To clarify at which age complications of spine surgery begin to increase, and which types of complications are more likely to have an impact on outcomes, we performed an age-stratified analysis of Japanese patients, including those aged 85 or older, as Japan has the longest life expectancy in the world.
MATERIALS AND METHODS
1. Study Outcomes
The primary outcome was to clarify morbidity and mortality after standard spine surgery and potential risk factors for complications. The secondary outcome was to describe specific major complications that happened to octogenarians and nonagenarians after surgery.
2. Patient Selection
The study population consisted of consecutive patients older than 20 years with myelopathy or radiculopathy who underwent spine surgery without instrumented fusion between January 2008 and April 2018. Patients with spinal instability who required instrumented fusion surgery were excluded because those undergoing instrumented fusion surgery may be more likely to have complications than those undergoing decompression surgery alone. Patients with congenital, traumatic, infectious, neoplastic, and vascular lesions were also excluded.
3. Classification of Complications
Complications were classified as medical or surgical. Medical complications included stroke (intracranial hemorrhage, cerebral infarction, and transient ischemic attack), cardiac diseases (symptomatic angina, cardiac infarction, heart failure, and arterial embolism of lower extremities), respiratory diseases (pneumonia, atelectasis, and respiratory failure), digestive diseases (ileus and hepatic dysfunction), urological diseases (urinary tract infection and renal dysfunction), delirium, perioperative transfusion, and other diseases (drug allergy, gouty arthritis, electrolyte abnormalities, and parkinsonism). Surgical complications included deteriorated or new postoperative motor weakness, incidental durotomy, postoperative hematoma, wound infection and dehiscence, graft migration, insufficient decompression, laminectomy at the wrong level, and others (retained drain tube and head pin problems). Complications were considered to be major if they required invasive procedures (surgery, radiological interventions, and endoscopic procedures), necessitated management in the intensive care unit, resulted in a prolonged hospital stay of more than 2 weeks, or resulted in permanent morbidity.
4. Statistical Analysis
Patient factors, surgical factors, complications, and deaths within 30 days of index surgery were retrospectively collected from patients’ medical records. To analyze the relationships between age and complications, patients were stratified into 4 groups: adults (20–64 years), young-old (65–74), middle old (75–84), and the oldest-old (≥85), and statistical data were compared across the 4 groups. The analysis of variance test was used for continuous variables and the chi-square test (or the Fisher exact test if there were fewer than 6 values for a given variable) for categorical variables. Surgical outcomes were assessed using the Wilcoxon signed-rank test. The secondary outcome was potential risk factors for complications. Patient and surgical factors were identified via univariate logistic regression analysis, from which variables with a p-value <0.05 were selected. Multivariate logistic regression analysis was then used to identify independent risk factors for complications after controlling simultaneously for potential confounders. IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA) was used for statistical analyses. Two-sided tests were used, with p-values <0.05 indicating statistical significance.
5. Ethics
This study protocol was approved by the Institutional Review Board of Tokyo Metropolitan Neurological Hospital, Japan (#24-4). Since this was a noninvasive study, written informed consent was not obtained. A public notice that provided information on this study was instead posted on our hospital website.
RESULTS
1. Patient Factors
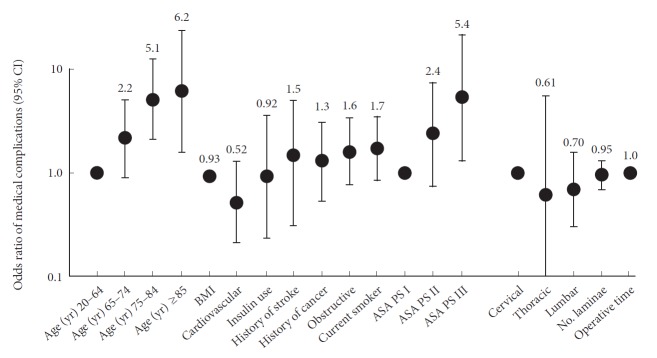
A total of 584 patients (mean, 70 years; range, 22–94 years) who underwent 673 operations were identified (Table 1). Adult patients accounted for one-third of our cohort, which was a similar proportion to those of young and middle old patients (Fig. 1). The oldest-old were also included in the present study. Medical comorbidities—hypertension, insulin use, hypercholesterolemia, obstructive pulmonary disease, malnutrition, cardiovascular diseases, urological diseases, involuntary movement disorder, and a previous history of cerebral stroke or cancer— and dependent status increased with age. The middle old and oldest-old groups had more preoperative comorbidities at baseline. Although the number of current smokers decreased with age, elderly patients were more likely to have obstructive pulmonary disease. As a result, the American Society of Anesthesiologists (ASA) physical status classification increased with age.
Table 1.
Baseline characteristics and comorbidities in 584 patients with spinal stenosis
| Variable | Age group (yr) |
p-value | |||
|---|---|---|---|---|---|
| 20–64 | 65–74 | 75–84 | ≥ 85 | ||
| No. of patients | 218 | 180 | 155 | 31 | |
| No. of surgeries | 237 | 222 | 181 | 33 | |
| Male sex (%) | 77 | 71 | 62 | 67 | 0.011* |
| Dependent status (mRS ≥ 3) | 30 | 39 | 50 | 67 | < 0.001* |
| Mean No. of medical comorbidities | 1.8 | 2.2 | 2.7 | 2.8 | < 0.001* |
| Hypertension | 29 | 51 | 62 | 70 | < 0.001* |
| Diabetes | 15 | 20 | 25 | 15 | 0.063 |
| Insulin use | 1 | 6 | 4 | 0 | 0.021* |
| Hypercholesterolemia | 18 | 19 | 29 | 27 | 0.028* |
| BMI (kg/m2), mean ± SD | 24 ± 4.4 | 24 ± 3.5 | 23 ± 3.5 | 22 ± 2.4 | 0.008* |
| BMI ≥ 25 kg/m2 | 37 | 37 | 27 | 9 | 0.002* |
| Current smoker | 26 | 14 | 10 | 3 | < 0.001* |
| Ex-smoker | 8 | 13 | 14 | 15 | 0.065 |
| Restrictive pulmonary disease | 11 | 9 | 14 | 9 | 0.53 |
| Obstructive pulmonary disease | 5 | 10 | 16 | 27 | < 0.001* |
| Hemoglobin (g/dL), mean ± SD | 13.9 ± 1.5 | 13.3 ± 1.3 | 12.8 ± 1.6 | 12.3 ± 1.3 | 0.28 |
| Malnutrition (Alb < 3.5 mg/dL) | 2 | 1 | 8 | 12 | < 0.001* |
| Infection | 5 | 9 | 6 | 3 | 0.40 |
| Cardiovascular disease | 5 | 12 | 20 | 27 | < 0.001* |
| Digestive disease | 8 | 10 | 12 | 18 | 0.21 |
| Urological disease | 3 | 7 | 15 | 12 | < 0.001* |
| Involuntary movement disorder | 11 | 8 | 2 | 3 | 0.001* |
| Parkinson disease | 6 | 9 | 3 | 3 | 0.098 |
| History of cerebral stroke | 2 | 5 | 9 | 18 | 0.001* |
| History of cancer | 2 | 7 | 10 | 24 | < 0.001* |
| Steroid use | 3 | 5 | 2 | 0 | 0.27 |
| ASA physical status classification | < 0.001* | ||||
| I | 32 | 15 | 7 | 3 | |
| II | 59 | 75 | 78 | 67 | |
| III | 9 | 10 | 15 | 30 | |
Values are presented as percentage unless otherwise indicated.
mRS, modified Rankin Scale; BMI, body mass index; SD, standard deviation; Alb, albumin; ASA, American Society of Anesthesiologists.
p<0.05, statistically significant differences.
Fig. 1.
Distribution of patients across age groups.
2. Surgical Factors
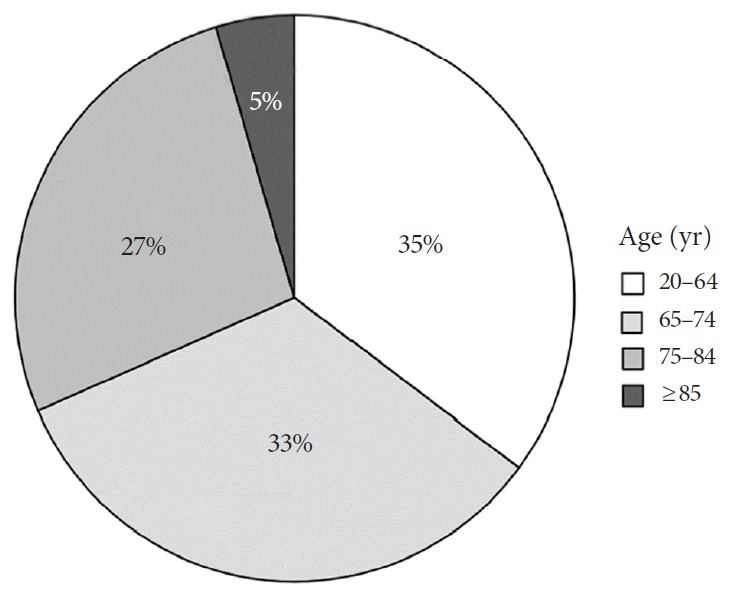
The patients included in this study underwent standard spine surgery in daily practice: laminectomy, laminoplasty, discectomy, foraminotomy, or anterior decompression and allograft fusion (Table 2). The cervical spine was the most common surgical site, followed by the lumbar and thoracic spine (56%, 38%, and 6%, respectively). Laminectomy and laminoplasty were the 2 most common surgical procedures (45% and 38%). The mean number of laminae (vertebrae) treated, the mean operative time, and mean operative blood loss decreased with age. During the median 15-month follow-up (range, 0–78 months), the frequency of independent status significantly increased after surgery regardless of age (Fig. 2) (p<0.001).
Table 2.
Surgical procedure-related variables in 673 spinal surgeries for spinal stenosis
| Variable | Age group (yr) |
p-value | |||
|---|---|---|---|---|---|
| 20–64 | 65–74 | 75–84 | ≥ 85 | ||
| No. of surgeries | 237 | 222 | 181 | 33 | |
| Spinal level | 0.001* | ||||
| Cervical | 66 | 50 | 49 | 61 | |
| Thoracic | 5 | 4 | 9 | 6 | |
| Lumbar | 29 | 45 | 43 | 33 | |
| Diagnosis | < 0.001* | ||||
| Degenerative stenosis | 52 | 67 | 75 | 79 | |
| Disc herniation | 23 | 15 | 6 | 9 | |
| OPLL | 14 | 6 | 8 | 3 | |
| OYL | 4 | 3 | 7 | 6 | |
| Spondylolisthesis | 1 | 3 | 3 | 0 | |
| Craniocervical stenosis | 1 | 1 | 0 | 3 | |
| Foraminal stenosis | 5 | 5 | 1 | 0 | |
| Surgical procedure | < 0.001* | ||||
| Anterior decompression & fusion | 12 | 5 | 1 | 3 | |
| Posterior approach | 88 | 95 | 99 | 97 | < 0.001* |
| Laminectomy | 24 | 45 | 67 | 79 | |
| Laminoplasty | 50 | 38 | 27 | 15 | |
| Discectomy | 10 | 8 | 4 | 3 | |
| Posterior foraminotomy | 3 | 4 | 1 | 0 | |
| No. of laminae (vertebrae) treated, mean ± SD | 2.9 ± 1.2 | 2.6 ± 1.0 | 2.7 ± 1.0 | 2.4 ± 0.7 | 0.017* |
| Operative time (min), mean ± SD | 305 ± 111 | 277 ± 100 | 263 ± 107 | 232 ± 76 | < 0.001* |
| Operative blood loss (mL), mean ± SD | 151 ± 223 | 139 ± 150 | 138 ± 148 | 113 ± 151 | 0.648 |
| Antibiotics use (day), mean ± SD | 2.5 ± 1.9 | 2.5 ± 1.5 | 2.5 ± 1.6 | 2.8 ± 4.2 | 0.903 |
Values are presented as percentage unless otherwise indicated.
OPLL, ossified longitudinal ligament; OYL, ossified yellow ligament; SD, standard deviation.
p<0.05, statistically significant differences.
Fig. 2.
The rate of independent status (modified Rankin Scale [mRS] ≤2). The values of the y-axis represent number of surgeries resulted in mRS≤2/total surgeries. The values were calculated on the basis of number of surgeries because some patients underwent independent multiple surgeries.
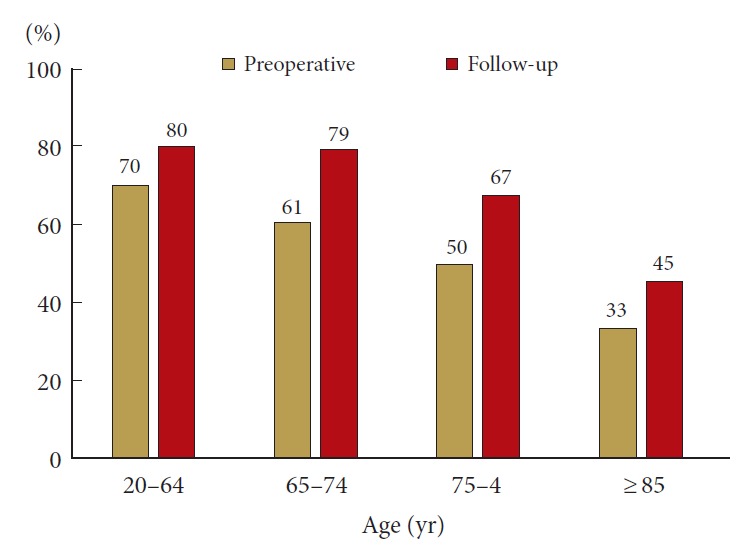
3. Complication Rates
The rate of medical complications was significantly higher in the middle and oldest-old than in adult patients (Fig. 3). In the middle old patients, delirium was the most common medical complication (14%), followed by digestive diseases (4.4%), perioperative transfusion (3.3%), and respiratory diseases (2.8%, Table 3). In the oldest-old patients, delirium was the most common medical complication (27%), followed by respiratory diseases (9.1%), cardiovascular diseases (9.1%), and stroke (6.1%). The rate of surgical complications did not significantly differ across the groups (Fig. 3). Total complications, including medical and surgical complications, increased in patients aged 75 years or older (Table 3).
Fig. 3.
The rates of complications. The values on the y-axis represent the complicated surgeries/total surgeries. Gray bars indicate the rates of major complications.
Table 3.
Specific perioperative complications in 673 spinal stenosis surgeries
| Variable | Age group (yr) |
p-value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 20–64 |
65–74 |
75–84 |
≥ 85 |
Overall |
|||||||
| Total | Major | Total | Major | Total | Major | Total | Major | Total | Major | ||
| Medical complications | |||||||||||
| Delirium | 3.8 | 0 | 3.6 | 0 | 14 | 0.6 | 27 | 3.0 | 7.6 | 0.3 | < 0.001* |
| Respiratory | 0.8 | 0.4 | 2.7 | 0 | 2.8 | 1.1 | 9.1 | 6.1 | 2.4 | 0.7 | 0.029* |
| Urological | 0.8 | 0 | 2.3 | 0.5 | 2.2 | 1.1 | 3.0 | 0 | 1.8 | 0.4 | 0.58 |
| Digestive | 1.3 | 0.4 | 0 | 0 | 4.4 | 0.6 | 0 | 0 | 1.6 | 0.3 | 0.004* |
| Transfusion | 0 | 0 | 0.9 | 0 | 3.3 | 0 | 6.1 | 0 | 1.5 | 0 | 0.005* |
| Cardiovascular | 0 | 0 | 0.9 | 0 | 1.7 | 0 | 9.1 | 0 | 1.2 | 0 | < 0.001* |
| Stroke | 0 | 0 | 0.5 | 0.5 | 0.6 | 0.6 | 6.1 | 3.0 | 0.6 | 0.4 | < 0.001* |
| Drug allergy | 0.4 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0.3 | 0 | 0.82 |
| Gouty arthritis | 0.4 | 0 | 0 | 0 | 0.6 | 0 | 0 | 0 | 0.3 | 0 | 0.73 |
| Electrolyte abnormalities | 0 | 0 | 0.5 | 0 | 0.6 | 0 | 0 | 0 | 0.3 | 0 | 0.71 |
| Parkinsonism | 0.4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.1 | 0 | 0.61 |
| Surgical complications | |||||||||||
| Incidental durotomy | 2.5 | 0.4 | 2.7 | 0.5 | 9.4 | 0.6 | 0 | 0 | 4.3 | 0.4 | 0.001* |
| Neurological deficits | 2.5 | 0.4 | 2.7 | 1.4 | 2.8 | 1.7 | 6.1 | 0 | 2.8 | 1.0 | 0.76 |
| Fibrin glue use | 1.7 | 0 | 0.5 | 0 | 3.9 | 0 | 0 | 0 | 1.8 | 0 | 0.061 |
| Hematoma | 1.3 | 0.4 | 1.4 | 0.5 | 1.7 | 1.1 | 6.1 | 3.0 | 1.6 | 0.7 | 0.23 |
| Wound dehiscence | 1.7 | 0 | 0.9 | 0.5 | 0 | 0 | 0 | 0 | 0.9 | 0.1 | 0.31 |
| Deep infection | 0.4 | 0.4 | 0.9 | 0.5 | 0.6 | 0.6 | 0 | 0 | 0.6 | 0.4 | 0.88 |
| Graft sinking/migration | 1.3 | 0.4 | 0 | 0 | 0.6 | 0 | 0 | 0 | 0.6 | 0.1 | 0.34 |
| Insufficient decompression | 0.4 | 0.4 | 0 | 0 | 1.1 | 1.1 | 0 | 0 | 0.4 | 0.4 | 0.41 |
| Wrong level laminectomy | 0 | 0 | 0 | 0 | 1.1 | 0.6 | 0 | 0 | 0.3 | 0.1 | 0.14 |
| Retained drain tube | 0.4 | 1.0 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0.3 | 0.3 | 0.82 |
| Head pin problem | 0.4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.1 | 0 | 0.61 |
| Any complications | 18.1 | NA | 17.6 | NA | 36.5 | NA | 54.5 | NA | 24.7 | NA | < 0.001* |
| Any major complications | NA | 3.8 | NA | 4.5 | NA | 7.2 | NA | 15.2 | NA | 5.5 | 0.034* |
Values are presented as percentage.
NA, not available.
p<0.05, statistically significant differences.
4. Major Complications in the Oldest-Old
A total of 5 major complications, including 4 medical and 1 surgical complications, occurred in the oldest-old (Table 4). A major respiratory complication occurred in an 88-year-old male patient who underwent anterior decompression with allograft fusion for cervical disc herniation. He developed delirium that required sedation after surgery. Three days later, he developed severe aspiration pneumonia that required reintubation. After management in the intensive care unit, pneumonia improved and the patient eventually recovered to a normal lifestyle. Another major respiratory complication occurred in an 87-year-old male patient who underwent posterior cervical decompression. Before surgery, he developed aspiration pneumonia because of decreased respiratory function due to severe cervical spinal stenosis. After the improvement of pneumonia, he underwent surgery; however, aspiration pneumonia recurred. Despite the intensive management of pneumonia, he died 19 days after surgery.
Table 4.
Specific complications in the oldest-old (≥85) patients
| Age (yr)/sex | ASA PS classification | Diagnosis | Procedure | Major complications | Minor complications | Outcome |
|---|---|---|---|---|---|---|
| 88/M | II | Cervical disc | ACDF | Aspiration pneumonia | Delirium | GR |
| 87/M | III | CS | Laminectomy | Aspiration pneumonia | Delirium | Dead |
| 92/F* | II | Thoracic OYL | Laminectomy | TIA | None | GR |
| 94/F* | III | LS | Laminectomy | Cerebral infarction | None | Dead |
| 86/M | III | Thoracic OYL | Laminectomy | Postoperative hematoma | None | GR |
| 87/M | II | CS | Laminoplasty | None | Delirium | GR |
| 88/M | II | CS | Laminectomy | None | Delirium | GR |
| 88/F | II | CS | Laminectomy | None | Delirium | GR |
| 88/M | II | LS | Laminectomy | None | Delirium | GR |
| 90/M | II | LS | Laminectomy | None | Delirium | GR |
| 85/F | II | LS | Laminectomy | None | Delirium | GR |
| 85/F | III | CS | Laminectomy | None | Delirium, transfusion | GR |
| 85/F | II | CS | Laminectomy | None | Arrhythmia | GR |
| 85/M | II | Lumbar disc | Laminectomy | None | Arrhythmia | GR |
| 88/M | III | LS | Laminectomy | None | High creatinine | GR |
| 88/F | III | CS | Laminectomy | None | Atelectasis, transfusion | GR |
| 87/F | II | CS | Laminectomy | None | Postoperative hematoma | GR |
| 89/M | II | CS | Laminectomy | None | Neurologic deficit | GR |
ASA PS, American Society of Anesthesiologists Physical Status; ACDF, anterior cervical decompression with allograft fusion; GR, good recovery; CS, cervical stenosis; OYL, ossified yellow ligament; TIA, transient ischemic attack; LS, lumbar stenosis.
These 2 cases represent 1 patient.
Two major cerebral embolic events occurred in 1 female patient who had been treated with anticoagulation therapy for atrial fibrillation. When she was 92 years old, she required thoracic decompression for thoracic spinal stenosis. Seven days after surgery, she experienced a transient ischemic attack, but recovered to a normal lifestyle. Two years after thoracic surgery, she required lumbar decompression surgery. She again developed acute cerebral infarction 2 days after surgery. Despite thrombolytic treatment, this patient died 9 days after surgery. For this patient, anticoagulation therapy was discontinued for 96 hours. During this period, heparin bridge therapy was performed. The cause of the embolic event may have been the discontinuation of anticoagulation therapy in the postoperative period. A major surgical complication occurred in an 86-year-old male patient who had been treated with anticoagulation therapy for atrial fibrillation. One day after thoracic decompression surgery, he developed postoperative symptomatic hematoma that required reoperation. For this patient, anticoagulation therapy was discontinued for 72 hours. During this period, heparin bridge therapy was performed. The cause of hematoma may have been a resumption of anticoagulation therapy in the immediate postoperative period.
As described above, 2 patients, one aged 87 years and the other aged 94 years, died because of medical complications; therefore, the mortality rate of the oldest-old was 5.6%.
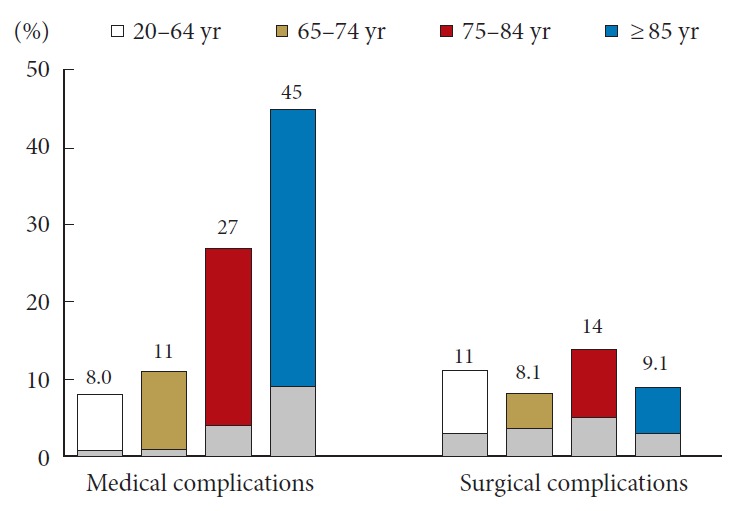
5. Multivariate Analysis of Risk Factors for Complications
Among the patient and surgical factors assessed for their relationships with medical complications after spine surgery, an age of 75 years or older (75–84 years: odds ratio [OR], 5.1; 95% confidence interval [CI], 2.1–13; ≥85 years: OR, 6.2; 95% CI, 1.6–24), ASA physical status classification III (OR, 5.4; 95% CI, 1.3–22) remained independent risk factors (Fig. 4).
Fig. 4.
Risk factors for medical complications. ASA PS, American Society of Anesthesiologists physical status; BMI, body mass index; CI, confidence interval.
Of the factors assessed for their relationships with major medical complications, insulin use (OR, 20; 95% CI, 1.8–221), and a history of cerebral stroke (OR, 11; 95% CI, 1.3–89) remained as independent risk factors.
DISCUSSION
In the present study, we found that perioperative complications of spine surgery were significantly more common in the middle old (75–84 years) and oldest-old patients (≥85 years), but not in the young-old patients (65–74 years), because of medical complications. Our results support the redefinition of the concept of elderly, “75 is the new 65”, by the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society.
Furthermore, we found that most of the medical complications were minor and treatable, although the middle old and oldest-old patients were 5- and 6-fold, respectively, more likely to develop medical complications than adult patients (20–64 years). Major complications were a reflection of an exacerbation of pre-existing disease, rather than new occurrence of disease. Baseline health status, ASA physical status classification, was driving the risk for complications rather than age alone.
Numerous studies of the complications of spine surgery in elderly patients have been conducted; however, most studies have failed to include patients older than 85 years [1,4,13-16,5-12]. Murphy et al. [14] reported the complications of lumbar decompression surgery in elderly patients stratified by age. They concluded that patients aged 65 or older were more likely to develop minor complications (surgical and urinary tract infections) and not to be discharged home than those younger than 65 years; however, there were no significant differences in the rates of major complications across the groups. The difference between our results and previous findings may be explained by the fact that our study included markedly older patients, including those aged 85 or older, a choice that was made because Japan is experiencing the highest rate of population aging worldwide [2].
Attention should be paid to the fact that the most common medical complication in those aged 85 or older was delirium (27%), which was sometimes associated with sedation and respiratory complications. A multicenter, randomized, placebo-controlled trial recently reported that ramelteon showed preventive effects on delirium, with a relative risk of 0.09 in patients in intensive care units [20]. Nightly administration of ramelteon to elderly patients may provide protection against delirium in patients who have undergone spine surgery. Anticoagulation therapy in elderly patients undergoing elective spine surgery is also a critical issue. Despite the increasing use of oral anticoagulants, guidelines for their perioperative use in spine decompression surgery are still lacking. In our case series, the 94-year-old patient who had been treated with anticoagulation therapy developed acute cerebral infarction, possibly because of the discontinuation of anticoagulation therapy during surgery. The 86-year-old patient, however, developed a postoperative symptomatic hematoma because of the resumption of anticoagulation therapy just after surgery. A large-scale study of perioperative anticoagulant use has been recently reported: the report’s conclusions were that anticoagulant resumption >72 hours postoperatively may increase risk of thromboembolic events, and that a short preoperative anticoagulant discontinuation time (<24 hours) may be justified [21].
The primary limitation of the present study is that it was a retrospective, single-institution analysis. A prospective, multiinstitutional, international study is needed to resolve this limitation. Various surgical methods were included from the cervical to lumber regions in the present study because we’d like to discuss about complications associated with all kinds of standard spine surgery in daily clinical practice. To minimize statistical errors, surgical confounders were adjusted by multivariate analysis. We consider the present results to be beneficial for determining possible risks in elderly patients after spine surgery in a large number of institutions in the world.
CONCLUSION
Among elderly patients, including those aged 85 years or older, perioperative complications of spine surgery were more common in middle (75–84) and oldest-old (≥85) patients, but not in young-old patients (65–74). This increase was associated with medical, but not surgical complications; however, most of the medical complications were minor and treatable. Major complications were associated with preoperative medical comorbidities and their severities, rather than new occurrence of disease; therefore, most elderly patients with low ASA physical status classification (≤II) may benefit from spine surgery.
Acknowledgments
Portions of this work were presented in abstract form at the 77th Annual Meeting of the Japan Neurosurgical Society, held in Sendai, Japan, on October 10–12, 2018.
Footnotes
The authors have nothing to disclose.
REFERENCES
- 1.Gerhardt J, Bette S, Janssen I, et al. Is eighty the new sixty? Outcomes and complications after lumbar decompression surgery in elderly patients over 80 years of age. World Neurosurg. 2018;112:e555–60. doi: 10.1016/j.wneu.2018.01.082. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Health Labour and Welfare . Annual health, labour and welfare report 2017 [Internet] Tokyo: Ministry of Health Labour and Welfare; 2017. [cited 2019 May 5]. https://www.mhlw.go.jp/english/wp/wp-hw11/index.html. [Google Scholar]
- 3.Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakashima H, Tetreault LA, Nagoshi N, et al. Does age affect surgical outcomes in patients with degenerative cervical myelopathy? Results from the prospective multicenter AOSpine International study on 479 patients. J Neurol Neurosurg Psychiatry. 2016;87:734–40. doi: 10.1136/jnnp-2015-311074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lau D, Osorio JA, Deviren V, et al. The relationship of older age and perioperative outcomes following thoracolumbar three-column osteotomy for adult spinal deformity: an analysis of 300 consecutive cases. J Neurosurg Spine. 2018;28:593–606. doi: 10.3171/2017.10.SPINE17374. [DOI] [PubMed] [Google Scholar]
- 6.Cassinelli EH, Eubanks J, Vogt M, et al. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976) 2007;32:230–5. doi: 10.1097/01.brs.0000251918.19508.b3. [DOI] [PubMed] [Google Scholar]
- 7.Arvind V, Kim JS, Oermann EK, et al. Predicting surgical complications in adult patients undergoing anterior cervical discectomy and fusion using machine learning. Neurospine. 2018;15:329–37. doi: 10.14245/ns.1836248.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung SK, Kim KT, Kim YB. Surgical complications of transforaminal lumbar interbody fusion in elderly patients. Korean J Spine. 2010;7:167–72. [Google Scholar]
- 9.Khashan M, Lidar Z, Salame K, et al. Minimally invasive spinal decompression in patients older than 75 years of age: perioperative risks, complications, and clinical outcomes compared with patients younger than 45 years of age. World Neurosurg. 2016;89:337–42. doi: 10.1016/j.wneu.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Purvis TE, De la Garza Ramos R, Sankey EW, et al. In-hospital medical complications after non-operative and operative treatment of thoracolumbar fractures in patients over 75 years of age. J Clin Neurosci. 2018;50:83–7. doi: 10.1016/j.jocn.2018.01.061. [DOI] [PubMed] [Google Scholar]
- 11.Takai K, Matsumoto T, Yabusaki H, et al. Surgical complications associated with spinal decompression surgery in a Japanese cohort. J Clin Neurosci. 2016;26:110–15. doi: 10.1016/j.jocn.2015.06.029. [DOI] [PubMed] [Google Scholar]
- 12.Lee MJ, Hacquebord J, Varshney A, et al. Risk factors for medical complication after lumbar spine surgery: a multivariate analysis of 767 patients. Spine (Phila Pa 1976) 2011;36:1801–6. doi: 10.1097/brs.0b013e318219d28d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vitaz TW, Raque GH, Shields CB, et al. Surgical treatment of lumbar spinal stenosis in patients older than 75 years of age. J Neurosurg. 1999;91(Spine 2):181–5. doi: 10.3171/spi.1999.91.2.0181. [DOI] [PubMed] [Google Scholar]
- 14.Murphy ME, Gilder H, Maloney PR, et al. Lumbar decompression in the elderly: increased age as a risk factor for complications and nonhome discharge. J Neurosurg Spine. 2017;26:353–62. doi: 10.3171/2016.8.SPINE16616. [DOI] [PubMed] [Google Scholar]
- 15.Wang MY, Green BA, Shah S, et al. Complications associated with lumbar stenosis surgery in patients older than 75 years of age. Neurosurg Focus. 2003;14:e7. doi: 10.3171/foc.2003.14.2.8. [DOI] [PubMed] [Google Scholar]
- 16.Acosta FL, McClendon J, O’Shaughnessy BA, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: complications and predictive factors. J Neurosurg Spine. 2011;15:667–74. doi: 10.3171/2011.7.SPINE10640. [DOI] [PubMed] [Google Scholar]
- 17.De la Garza-Ramos R, Goodwin CR, Abu-Bonsrah N, et al. Prolonged length of stay after posterior surgery for cervical spondylotic myelopathy in patients over 65years of age. J Clin Neurosci. 2016;31:137–41. doi: 10.1016/j.jocn.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 18.Ouchi Y, Rakugi H, Arai H, et al. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr Gerontol Int. 2017;17:1045–7. doi: 10.1111/ggi.13118. [DOI] [PubMed] [Google Scholar]
- 19.Landriel Ibañez FA, Hem S, Ajler P, et al. A new classification of complications in neurosurgery. World Neurosurg. 2011;75:709–15. doi: 10.1016/j.wneu.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Hatta K, Kishi Y, Wada K, et al. Preventive effects of ramelteon on delirium. JAMA Psychiatry. 2014;71:397–403. doi: 10.1001/jamapsychiatry.2013.3320. [DOI] [PubMed] [Google Scholar]
- 21.Croci DM, Dalolio M, Guzman R, et al. Direct oral anticoagulants in patients undergoing spine surgery. World Neurosurg. 2019;125:e1034–41. doi: 10.1016/j.wneu.2019.01.236. [DOI] [PubMed] [Google Scholar]