Abstract
Objective
The cervical spine consists of 4 typical and 3 atypical vertebrae. The uncinate process is one of the unique features of the cervical vertebrae. Uncinectomy and uncoforaminotomy are widely used to decompress the nerve in the intervertebral foramen and to remove osteophytes from the uncinate process. Morphometric analyses of the uncinate process help spine surgeons obtain a 3-dimensional orientation for approaching the cervical spine with minimal risk to the surrounding vascular and neural structures. This study aims to analyze the morphometry of uncinate process of cervical vertebrae with relevant to cervical spine surgery.
Methods
Eighty dry adult cervical vertebrae were studied, and 11 parameters were measured. Seven parameters were paired and 4 were unpaired.
Results
The height of the uncinate process progressively increased from C3 to C6 and decreased at C7. The length of the uncinate process increased from C3 to C6–7. The width was greatest at C6 and smallest at C3. The vertebral body width and anteroposterior diameter gradually increased from C3 to C7. The parameters of the lamina also increased from C3 to C7.
Conclusion
Precise knowledge about the cervical vertebrae is useful for diagnosing both common and uncommon causes of symptoms and for choosing an appropriate approach. Thus, it helps to increase the success rate of cervical surgery.
Keywords: Cervical vertebrae, Morphometry, Uncinate process
INTRODUCTION
The axial skeleton of neck comprises 7 cervical vertebrae. Out of which, 4 vertebrae (C3–6) are typical and 3 vertebrae (C1, C2, and C7) are atypical. Each typical vertebra consists of vertebral body and the neural arch formed by pedicles, articulating processes, laminae and spinous process.
Uncinate process is a bony projection, also known as “eminentia costaria, processus uncinatus,” present on the posterolateral margin of the superior surface of lower cervical vertebrae (C3–7) which encroach on the inferior surface of the above vertebra to form unco-vertebral joint (UVJ) or Luschka joint [1]. The UVJ forms the medial boundary of the vertebral foramen. The uncinate process was classified into 3 types based on the encroachment over adjacent intervertebral foramen. Type I – Uncinate process does not encroach upon the adjacent intervertebral foramen. Type II – encroach upon adjacent foramen without deformation. Type III – encroach upon adjacent foramen with deformation of uncinate process [2]. So, the type of uncinate process can also be an uncommon cause of radiculopathy. In such cases, it carries the importance during manipulation of uncinate process in spine procedure.
Morphological characteristics of cervical vertebrae are an important factor for maintaining the normal cervical lordosis and the mobility of the cervical column. Any change in morphometry which can be caused by trauma, pathological or space-occupying lesions, osteophyte formation, intervertebral disc herniation will lead to cervical instability, stenosis of the vertebral canal, compression of neurovascular structures, etc [3,4]. Study of morphology of cervical vertebra is important in spine-related surgeries like nerve decompression, transpedicular screws, plate fixation, uncinectomy, uncoforaminotomy to increase the success rate of these interventions for the above conditions [1-4]. Hence, we have undertaken the study to document the morphometry of uncinate process of cervical vertebrae along with some other parameters of cervical vertebrae.
MATERIALS AND METHODS
Eighty dry Indian adult human cervical vertebrae of age between 45–70 years with unknown sex were used for this study. Cervical vertebrae containing all the anatomical features were included in the study. Signs of fractured vertebrae, damaged vertebrae are excluded. Measurements were taken on the vertebrae between C3 and C7. All the linear parameters were precisely measured using digital vernier caliper (Mitutoyo absolute AOS digimatic caliper series 500) with 0.01-mm precision, after the identification of easily recognizable structures on each vertebra. Bony structures present on both sides were measured bilaterally. The measured data are grouped into 3 viz. uncinate process, lamina, and vertebral body. All the parameters were measured thrice by single investigator and its mean that the value was taken as final. All parameters were measured by the same observer and also by a second observer with an interval of 2 months in 20 cervical vertebrae to assess the inter and intraobserver variation using intraclass correlation coefficient was evaluated by SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA).
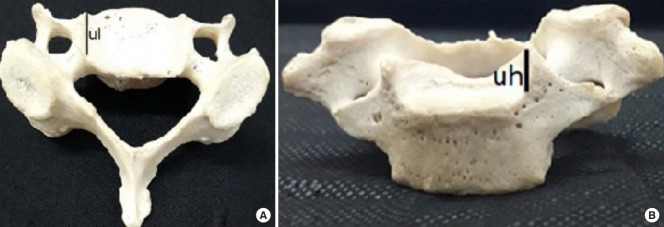
The following parameters were evaluated for C3–7 vertebrae (Fig. 1).
Fig. 1.
C3–7 cervical vertebrae.
1. Uncinate Process
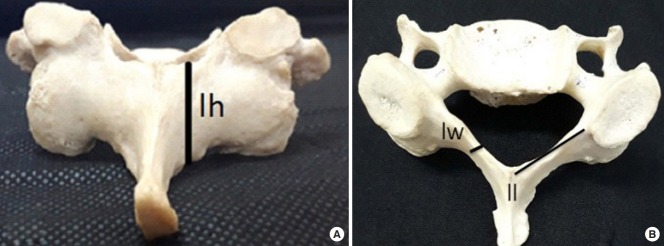
The measurements are (1) height – from the superior margin of the cervical vertebra to the tip of uncinate process (Fig. 2B); (2) width – transverse length of the uncinate process near its base; (3) length – from the anterior end to posterior end of the uncinate process near its base (Fig. 2A); (4) distance between the uncinate processes near its tip; (5) intervertebral foramen – distance between the uncinate process tip and lateral edge of lamina (medial to the superior articulating process).
Fig. 2.
(A, B) Measurements of uncinate process. ul, uncinate process length; uh, uncinate process height.
2. Vertebral Body
The measurements are (1) anteroposterior diameter – from the middle of the anterior margin to the middle of the posterior margin in the superior surface of the vertebral body (Fig. 3B) and (2) transverse diameter – at the level of the transverse process (Fig. 3A).
Fig. 3.
(A, B) Measurements of vertebral body. ap, anteroposterior diameter of vertebral body; vw, vertebral body width.
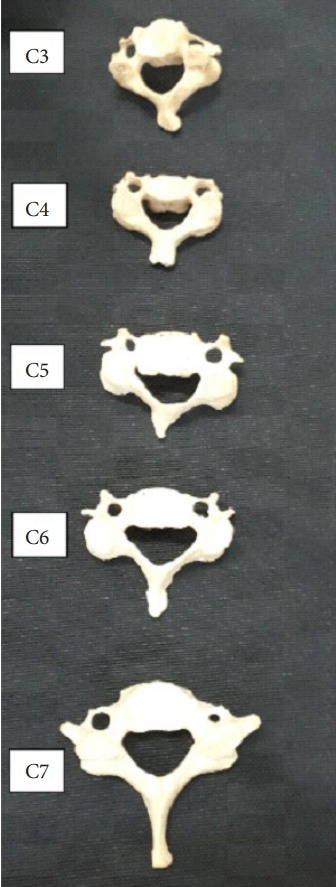
3. Lamina
The measurements are (1) length – at the superior border of lamina (Fig. 4B), (2) width – in the middle of the lamina (Fig. 4B), (3) height – from superior border to inferior border in the middle of the lamina (Fig. 4A), and (4) distance between the lateral ends of the lamina of both sides.
Fig. 4.
(A, B) Measurements of lamina: lw, lamina width; ll, lamina length; lh, lamina height.
RESULTS
Eighty dry cervical vertebrae have been studied. There is no significant difference between the right and the left of the vertebral processes.
Table 1 and Fig. 5 show the results of uncinate process parameters.
Table 1.
Parameters of uncinate process in mm
| Cervical vertebra | Height (mm) |
Length (mm) |
Width (mm) |
Distance between the tip of both uncinate process (mm) | Distance between uncinate tip and lamina near the medial end of the superior facet (IVF) (mm) |
||||
|---|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | Right | Left | ||
| C3 | 4.34 ± 1.04 | 3.82 ± 0.85 | 9.93 ± 1.41 | 10.21 ± 1.25 | 2.60 ± 0.53 | 2.51 ± 0.57 | 18.73 ± 1.24 | 11.57 ± 1.70 | 11.23 ± 1.71 |
| C4 | 4.55 ± 1.28 | 4.19 ± 1.09 | 10.39 ± 1.54 | 10.95 ± 1.66 | 2.77 ± 0.85 | 2.77 ± 1.00 | 19.68 ± 1.55 | 12.35 ± 2.39 | 11.72 ± 2.42 |
| C5 | 4.79 ± 2.02 | 4.44 ± 1.38 | 10.99 ± 2.25 | 11.32 ± 2.63 | 2.72 ± 0.69 | 2.79 ± 0.51 | 21.08 ± 2.88 | 11.44 ± 1.32 | 10.86 ± 1.22 |
| C6 | 5.31 ± 1.30 | 5.38 ± 1.18 | 12.00 ± 2.84 | 12.50 ± 2.86 | 2.96 ± 0.78 | 2.82 ± 0.71 | 22.26 ± 2.33 | 11.44 ± 1.71 | 10.79 ± 2.21 |
| C7 | 5.13 ± 1.15 | 5.41 ± 1.58 | 12.27 ± 2.72 | 11.71 ± 2.57 | 2.86 ± 0.60 | 2.78 ± 0.41 | 22.45 ± 2.15 | 10.63 ± 1.55 | 9.75 ± 1.26 |
Values are presented as mean±standard deviation.
IVF, intervertebral foramen.
Fig. 5.
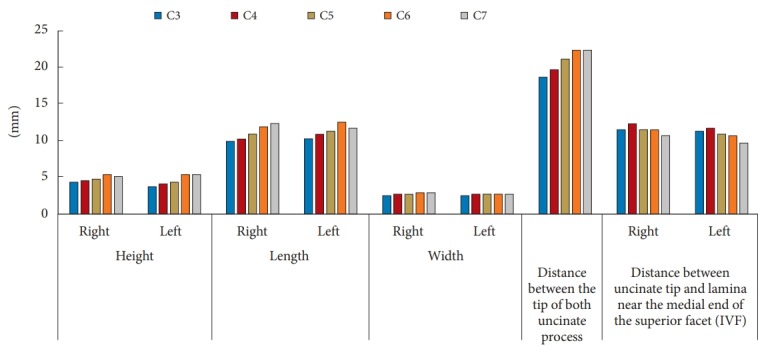
Bar diagram showing the results of uncinate process. IVF, intervertebral foramen.
1. Uncinate Process
The maximum and minimum height of the uncinate process measured at C6–7 (5.31–5.41 mm) vertebrae and C3 (4.08 mm) respectively. The maximum and minimum length of the uncinate process measured at C6–7 (12.27–12.50) and C3 (10.07 mm) vertebra respectively. The width of the uncinate process is maximum at C6 (2.89 mm) and minimum at C3 (2.55 mm) vertebral level. The maximum and minimum distance between the tips of the uncinate process measured at C7 (22.45 mm) and C3 (18.73) vertebra respectively. The maximum and minimum distance between the tip of uncinate process and the lamina (i.e., the intervertebral foramen) is measured at C4 (10.19 mm) and C7 (10.19 mm) respectively.
Prevalence of type I uncinate process (Fig. 6A) was 60%; type II uncinate process (Fig. 6B) was 40% and there was no type III uncinate process.
Fig. 6.
Types I (A) and II (B) uncinate process. UP, uncinate process.
2. Vertebral Body
The anteroposterior diameter and the width of the vertebral body are maximum in C7 (15.17 mm) vertebra and minimum in C3 (12.19 mm) vertebra. There is a gradual increase in the size of the vertebral body from C3 to C7 level (Table 2).
Table 2.
Parameters of vertebral body in mm
| Cervical vertebra | Anteroposterior diameter (mm) | Width (mm) |
|---|---|---|
| C3 | 12.94 ± 1.52 | 18.93 ± 0.99 |
| C4 | 13.96 ± 1.48 | 20.32 ± 1.90 |
| C5 | 13.78 ± 1.90 | 20.80 ± 1.87 |
| C6 | 14.96 ± 2.02 | 21.74 ± 3.77 |
| C7 | 15.70 ± 2.43 | 22.59 ± 3.55 |
Values are presented as mean±standard deviation.
3. Lamina
The height, length, and width of the lamina are maximum in C7 (11.98, 14.99, and 3.13 mm, respectively) and minimum in the C3 (9.45, 13.31, and 2.39 mm, respectively) vertebra. The distance between the lateral ends of the lamina is increasing from C3 (20.26 mm) to C7 (22.80 mm) cervical vertebrae (Table 3).
Table 3.
Parameters of lamina in mm
| Cervical vertebra | Height (mm) |
Length (mm) |
Width (mm) |
Between the lateral ends of the lamina (mm) | |||
|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | ||
| C3 | 9.43 ± 1.36 | 9.47 ± 1.18 | 13.50 ± 1.39 | 13.11 ± 1.46 | 2.39 ± 0.95 | 2.39 ± 0.78 | 20.26 ± 1.23 |
| C4 | 10.25 ± 1.15 | 10.57 ± 0.90 | 13.91 ± 1.45 | 13.74 ± 1.95 | 2.79 ± 1.04 | 2.83 ± 1.20 | 20.34 ± 1.52 |
| C5 | 10.49 ± 2.03 | 10.39 ± 2.46 | 14.15 ± 1.82 | 14.11 ± 1.56 | 2.83 ± 0.70 | 2.83 ± 0.82 | 21.01 ± 2.14 |
| C6 | 11.47 ± 1.60 | 11.73 ± 1.98 | 14.22 ± 1.78 | 14.61 ± 1.76 | 2.87 ± 0.94 | 2.92 ± 0.86 | 21.47 ± 1.57 |
| C7 | 11.76 ± 1.93 | 12.19 ± 2.25 | 15.38 ± 2.15 | 14.61 ± 1.74 | 3.06 ± 1.07 | 3.20 ± 1.06 | 22.80 ± 1.99 |
Values are presented as mean±standard deviation.
The mean inter- and intraobserver reliability showed “good” results (intraclass coefficient, 0.658 and 0.741, respectively) for the parameters of uncinate process, vertebral body, and lamina of cervical spine.
DISCUSSION
Cervical vertebrae and the uncinate process can be approached anteriorly, posteriorly, and posterolaterally. Morphometry of the cervical vertebrae is useful in increasing the success rate of surgery as well as to reduce the complications. Each approach has its own merits and demerits. But the posterior approach for nerve decompression offers less operative time and better prognosis postoperatively [5].
1. Uncinate Process
Uncinate process is a bony projection, in the superior surface of the vertebral body, which forms the uncovertebral joint with the body of the cervical vertebra above and also forms the medial margin of the intervertebral foramen [1,6,7]. Uncinectomy and uncoforaminotomy are the procedures to treat vertebral artery narrowing or cervical nerve irritation. Making window for the nerve root decompression, during the surgery, depends on the height and width of uncinate process [6]. The average height of the uncinate process is gradually increasing from C3 to C6 (4.08 mm at C3 and 5.35 mm at C6) then it starts decreasing (5.27 mm at C7). The height of uncinate process of the present study correlates with Kim et al.[8] and Lu et al. [6]. The uncinate process is narrowest at C3 (2.55 mm) comparable with other studies, but it is widest in C6 (2.89 mm). The average width is significantly low compared to other studies. Tables 4, 5, and Fig. 7 show the comparison of height and width of the uncinate process with previous studies respectively. The decrease in the height of the uncinate process in the lower cervical vertebra is one of the anatomical reasons for the cervical nerve root compression since it forms the medial boundary of intervertebral foramen which prevents the posterolateral disc herniation. Intervertebral disc herniation is more common in C7 level also emphasize the importance of height of the uncovertebral joint [7].
Table 4.
Comparison of the average height of uncinate process (UP)
| Study | Specimen | Average height (mm) of UP |
||||
|---|---|---|---|---|---|---|
| C3 | C4 | C5 | C6 | C7 | ||
| Kim et al., [8] (2012) | Cadaveric | 5.72 | 6.68 | 7.10 | 6.81 | 5.96 |
| Lu et al., [6] (1998) | Dry bone | 5.05 | 5.55 | 5.57 | 6.35 | 5.16 |
| Lee et al., [11] (2012) | Dry bone | 5.30 | 5.25 | 5.90 | 5.14 | 4.65 |
| Tubbs et al., [2] (2012) | Dry bone | 4.80 | 5.00 | 4.90 | 5.10 | 4.90 |
| Uğur et al., [1] (2000) | Dry bone | 4.94 | 5.62 | 5.70 | 6.30 | 6.60 |
| Kocabiyik et al., [9] (2017) | Dry bone | 6.40 | 7.44 | 6.50 | 7.23 | 6.25 |
| Present study (2018) | Dry bone | 4.08 | 4.37 | 4.60 | 5.35 | 5.27 |
Table 5.
Comparison of the width (mm) of the uncinate process
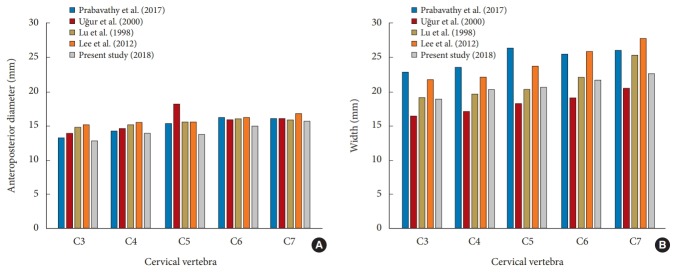
Fig. 7.
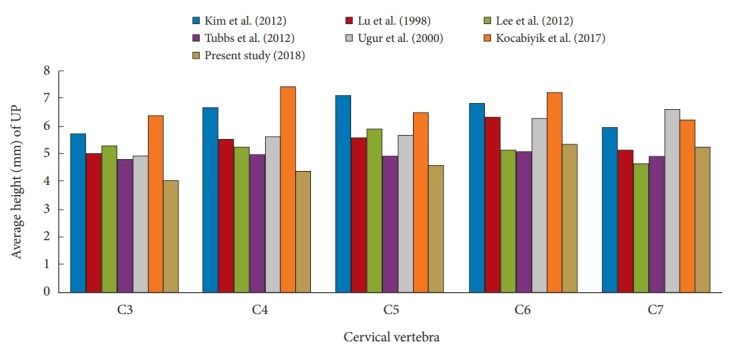
Bar diagram representing the comparison of uncinate process with previous studies. UP, uncinate process.
Apart from height and width of uncinate process, the type of uncinate process also important in diagnosing and choosing the interventions therapeutically. Because, alteration in normal shape of uncinate process may cause narrowing of vertebral foramen without any underlying pathology.
The distance between the tips of the uncinate process is gradually increasing from C3 (18.73 mm) to C7 (22.45 mm). The length of the uncinate process is increasing from C3 to C6–7 level. Therefore, the use of fixed values to approach the uncinate process through anteriorly may not be appropriate for all the vertebral levels. It may lead to inadequate decompression of the cervical spinal nerves [6,9].
Intervertebral foramen is a space between the posterior part of the uncinate process and the lamina facet junction. The average intervertebral foramen is minimum at C7 level (10.63± 1.55 mm on right and 9.75± 1.26 mm on left) and maximum at C4 level (12.35± 2.39 mm on right and 11.72 ± 2.42 mm on left) and correlates well with Uğur et al. [1]. Narrowing of intervertebral foramen leads to radiculopathy, spondylosis, cervical spondylotic myelopathy and narrowing of the radicular artery [6,7]. It can be caused by osteophytes from the uncinate process, intervertebral disc herniation, degeneration of joints, ligamentum flavum thickening, and bulging of the posterior vertebral ligament [7]. The surgical procedures to treat the above are anterior cervical discectomy and fusion, posterior cervical laminoforaminotomy, anterior cervical foraminotomy [2,5].
2. Vertebral Body
The posture of the cervical spine depends on the integrity of the vertebra. Any change in the anatomy and its function may cause clinical symptoms due to stenosis, degenerative disease. Anteroposteriorly the diameter of the vertebral body is maximum in C7 (15.70 mm) and minimum in C3 (12.94 mm). The width is gradually increasing from C3 (18.93 mm) to C7 (22.59 mm). There is no significant difference with the previous studies. Table 6 and Fig. 8 shows the comparison of vertebral body dimensions with previous studies. Dimensions of the vertebral body are an important factor in planning the cervical spine surgeries like anterior fixation of bicortical screws, plate fixation in cervical reconstructive surgery [3,4,10]. The vertebral body is also taking part in the uncovertebral joint. Osteophyte removal from this joint, with or without bone graft between the adjacent vertebrae can be approached medially or laterally. Burring of the vertebral body in the lateral part helps to preserve intervertebral disc and maintain the segment functionally mobile. But the combined anterolateral approach eliminates the need of arthrodesis in uncosectomy and uncoforaminotomy without much risk to the adjacent vessels and nerves [6].
Table 6.
Comparison of parameters of vertebral body
| Study | Anteroposterior diameter (mm) |
Width (mm) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| C3 | C4 | C5 | C6 | C7 | C3 | C4 | C5 | C6 | C7 | |
| Mahto and omar [4] (2015) | 13.60 | 14.40 | 15.20 | 15.80 | - | 22.80 | 23.60 | 26.40 | 25.20 | - |
| Prabavathy et al. [3] (2017) | 13.18 | 14.40 | 15.40 | 16.34 | 16.12 | 22.80 | 23.54 | 26.46 | 25.42 | 26.12 |
| Uğur et al. [1] (2000) | 14.00 | 14.70 | 18.30 | 15.90 | 16.10 | 16.50 | 17.10 | 18.30 | 19.20 | 20.60 |
| Lu et al. [6] (1998) | 14.80 | 15.30 | 15.50 | 16.10 | 15.90 | 19.20 | 19.70 | 20.30 | 22.20 | 25.40 |
| Lee et al. [11] (2012) | 15.20 | 15.60 | 15.60 | 16.20 | 16.90 | 21.80 | 22.10 | 23.70 | 25.80 | 27.80 |
| Present study (2018) | 12.94 | 13.96 | 13.78 | 14.96 | 15.70 | 18.93 | 20.32 | 20.80 | 21.74 | 22.59 |
Fig. 8.
Bar chart representing the comparison of parameters of vertebral body with previous studies: anteroposterior diameter (A) and width (B).
3. Lamina
Cervical spondylotic myelopathy due to a tumor of the spinal medulla, posterior longitudinal ligament ossification can be treated surgically by cervical laminoplasty. The height of the lamina of cervical vertebra decreases from C3 to C5 and starts increasing at C6 level [10,11]. In the present study, the height and the distance between the lateral ends of the lamina are gradually increasing from C3 to C7 vertebrae correlates with Prabavathy et al. [3]. Stability of the cervical spine can be maintained by C7 lamina also [3,10]. The length of the lamina correlates with Prabavathy et al. [3]. The width of lamina shows various results compared to the present study. The increase in the width and the interlaminar distance can be due to the normal cervical enlargement of the spinal cord [10]. Table 7 shows the comparison of parameters of lamina with previous studies.
Table 7.
Comparison of parameters of the lamina
| Vertebra | Height (mm) |
Length (mm) |
Width (mm) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C3 | C4 | C5 | C6 | C7 | C3 | C4 | C5 | C6 | C7 | C3 | C4 | C5 | C6 | C7 | |
| Lee et al. [11] (2012) | 11.70 | 11.40 | 11.30 | 13.10 | 15.30 | 13.90 | 14.80 | 15.30 | 14.70 | 13.20 | 3.70 | 2.90 | 2.60 | 3.30 | 5.00 |
| Prabavathy et al. [3] (2017) | 8.20 | 9.34 | 11.56 | 12.56 | 13.52 | 22.58 | 22.72 | 23.2 | 23.74 | 24.08 | - | - | - | - | - |
| Bazaldua et al. [10] (2011) | 12.27 | 11.37 | 11.27 | 12.24 | 14.31 | - | - | - | - | - | 15.67 | 18.37 | 19.32 | 18.69 | 18.19 |
| Present study (2018) | 9.45 | 10.41 | 10.44 | 11.60 | 11.97 | 13.31 | 13.82 | 14.13 | 14.41 | 14.86 | 2.39 | 2.81 | 2.83 | 2.89 | 3.13 |
Overall, most of the parameters are less in our studies. Morphological dimensions of the cervical vertebra may be an evidence that the guidelines used in diagnosis and treatment of the cervical spine-related conditions can vary in Indian populations, mainly in surgeries using therapeutic instruments near the region of neurovascular structures.
CONCLUSION
The precise knowledge about the uncinate process and the anatomy of the cervical vertebrae help to choose the appropriate surgical approach, depth of approach and the appropriate size of the instruments used for reconstructive procedures, while managing the spinal pathologies. It can act as an important guide to avoid various complications during and after the surgical procedures. These may help to promote the prognosis and reduce the postoperative complication. It may give some contribution to achieve the complete success rate in cervical spine surgeries.
Footnotes
The authors have nothing to disclose.
REFERENCES
- 1.Uğur HC, Uz A, Attar A, et al. Anatomical projection of the cervical uncinate process in ventral, ventrolateral, and posterior decompressive surgery. J Neurosurg. 2000;93(2 Suppl):248–51. doi: 10.3171/spi.2000.93.2.0248. [DOI] [PubMed] [Google Scholar]
- 2.Tubbs RS, Rompala OJ, Verma K, et al. Analysis of the uncinate processes of the cervical spine: an anatomical study. J Neurosurg Spine. 2012;16:402–7. doi: 10.3171/2011.12.SPINE11541. [DOI] [PubMed] [Google Scholar]
- 3.Prabavathy G, Philip XC, Arthi G, et al. Morphometric study of cervical vertebrae C3-C7 in South Indian population – a clinico-anatomical approach. Ital J Anat Embryol. 2017;122:49–57. [Google Scholar]
- 4.Omar S. Clinico-anatomical approach for instrumentation of the cervical spine: A morphometric study on typical cervical vertebrae. Int J Sci Study. 2015;3:143–5. [Google Scholar]
- 5.Bhaganagare AS, Nagesh SA, Shrihari BG, et al. Management of cervical monoradiculopathy due to prolapsed intervertebral disc, an institutional experience. J Craniovertebr Junction Spine. 2017;8:132–5. doi: 10.4103/jcvjs.JCVJS_2_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu J, Ebraheim NA, Yang H, et al. Cervical uncinate process: an anatomic study for anterior decompression of the cervical spine. Surg Radiol Anat. 1998;20:249–52. doi: 10.1007/BF01628483. [DOI] [PubMed] [Google Scholar]
- 7.Hartman J. Anatomy and clinical significance of the uncinate process and uncovertebral joint: a comprehensive review. Clin Anat. 2014;27:431–40. doi: 10.1002/ca.22317. [DOI] [PubMed] [Google Scholar]
- 8.Kim SH, Lee JH, Kim JH, et al. Anatomical morphometric study of the cervical uncinate process and surrounding structures. J Korean Neurosurg Soc. 2012;52:300–5. doi: 10.3340/jkns.2012.52.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kocabiyik N, Ercikti N, Tunali S. Morphometric analysis of the uncinate processes of the cervical vertebrae. Folia Morphol (Warsz) 2017;76:440–5. doi: 10.5603/FM.a2017.0010. [DOI] [PubMed] [Google Scholar]
- 10.Bazaldua CJJ, González LA, Gómez SA, et al. Morphometric study of cervical vertebrae C3-C7 in a population from northeastern Mexico. Int J Morpho. 2011;29:325–30. [Google Scholar]
- 11.Lee TH, Kim SJ, Chung IH. Morphometrical study of uncinate processes and vertebral body of cervical spine. J Korean Neurosurg Soc. 2012;51:247–52. doi: 10.3340/jkns.2012.51.5.247. [DOI] [PMC free article] [PubMed] [Google Scholar]