Abstract
Objective
The relationship between bone graft technique and postoperative outcomes for minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) has not been well-defined. This study aims to determine the effect of iliac crest bone grafting (ICBG) on patient-reported outcomes (PROs) and complication rates following MIS TLIF.
Methods
Primary, single-level MIS TLIF patients were consecutively analyzed. Patients that prospectively received a percutaneous technique of ICBG were compared to patients that retrospectively received bone morphogenetic protein-2 (BMP-2). Complication rates were assessed perioperatively and up to 1 year postoperatively. Changes in Oswestry Disability Index (ODI), visual analogue scale (VAS) back, and VAS leg pain were compared. Rates of minimum clinically important difference (MCID) achievement at final follow-up for ODI, VAS back, and VAS leg scores were compared.
Results
One hundred forty-nine patients were included: 101 in the BMP-2 cohort and 48 in the ICBG cohort. The ICBG cohort demonstrated increases in intraoperative blood loss and shorter lengths of stay. ICBG patients also experienced longer operative times, though this did not reach statistical significance. No significant differences in complication or reoperation rates were identified. The ICBG cohort demonstrated greater improvements in VAS leg pain at 6-week and 12-week follow-up. No other significant differences in PROs or MCID achievement rates were identified.
Conclusion
Patients undergoing MIS TLIF with ICBG experienced clinically insignificant increases in intraoperative blood loss and did not experience increases in postoperative pain or disability. Complication and reoperation rates were similar between groups. These results suggest that ICBG is a safe option for MIS TLIF.
Keywords: Minimally invasive transforaminal lumbar interbody fusion, Iliac crest bone graft, Bone morphogenic protein-2, Oswestry Disability Index, Visual analogue scale, Minimum clinically important difference
INTRODUCTION
Minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) is a clinically effective surgical treatment for lumbar degenerative disease [1,2]. Since being introduced, technological advancements in instrumentation and bone grafting adjuncts have led to improved postoperative outcomes and patient satisfaction. However, the concern for pseudarthrosis remains significant, with reported rates ranging from 2.0%–40.0% following spinal fusion [3,4].
Although several advances have been made to improve fusion rates, bone grafting techniques remain a significant factor in achievement of arthrodesis. The iliac crest bone graft (ICBG) has been considered the “gold standard” grafting technique in lumbar fusion surgery. Autologous bone grafts, such as ICBG, provide an effective biological scaffold for bone growth due to the graft’s osteoconductive and osteoinductive properties [5]. Additionally, autologous graft adjuncts avoid the potential concerns of immunogenicity and disease transmission associated with alternative graft materials. However, morbidity associated with ICBG remains a concern. Postoperative donor site pain is the most common issue associated with ICBG and has been reported in 2.8% to 27.9% of patients [6,7]. ICBG techniques have also been associated with increased operative time and greater intraoperative blood loss [8]. In an effort to avoid these complications, alternative graft materials such as demineralized bone matrix, ceramics, and recombinant bone morphogenetic protein-2 (BMP-2) have been developed [9-11]. These graft alternatives have demonstrated similar rates of arthrodesis to autograft, but have also been associated with higher surgical costs and additional complications [9,12-15].
Previous studies have investigated differences in outcomes between patients undergoing lumbar fusion with ICBG and lumbar fusion with graft alternatives [16-18]. However, there is a paucity of literature in regard to differences in outcomes based on graft adjunct in the minimally invasive spine population. As such, the purpose of this study is to evaluate postoperative outcomes for patients undergoing MIS TLIF with ICBG or BMP-2.
MATERIALS AND METHODS
1. Patient Population
Following Institutional Review Board approval (ORA #15052601), all patients scheduled to undergo primary, 1-level MIS TLIF with ICBG by a single surgeon from 2016 to 2017 were considered for prospective inclusion in the ICBG cohort. A historical cohort of patients that underwent primary, 1-level MIS TLIF with BMP-2 from 2014 to 2016 was identified from a prospectively maintained database of patients treated by the same surgeon (ORA #14051301). All patients were treated for degenerative pathology. Patients were excluded if they were treated for non-degenerative pathology or had less than 6 months of follow-up data.
2. Surgical Technique
A standard MIS TLIF procedure was performed using a paramedian approach [19]. In the ICBG cohort, autologous bone graft was harvested from the iliac crest contralateral to the site of decompression using a minimally invasive technique [20]. For L5-S1 procedures, a single incision was utilized for ICBG harvest and MIS TLIF. For L4–5 procedures, a separate 14-mm incision was created over the posterior superior iliac spine (PSIS) to access the iliac crest. A high-speed burr was used to remove the cap of the PSIS through a tubular retractor. Approximately 45–50 mL of ICBG was obtained using a combination of curettes. After copious irrigation of the wound, adequate hemostasis was achieved using Gelfoam as well as a hemostatic matrix (FLOSEAL; Baxter, Deerfield, IL, USA), and 0 Vicryl was used to reapproximate the deep fascia. Surgical drainage was not placed in the harvest site. Following endplate preparation, the interbody device was packed with ICBG and the residual crest and local bone graft were packed around the device in the intervertebral site. The interbody devices utilized during our study period included the PEEK T-PAL Spacer System (DePuy Synthes, Raynham, MA, USA); the PEEK Concorde Bullet (DePuy Synthes); and the titanium expandable cage (ALTERA; Globus Medical, Audubon, PA, USA). For the BMP-2 cohort, the interbody device was packed with local bone graft, BMP-2 (extra small kit, 1.4 mL), and 15 mL of crushed allograft. The concentration of rhBMP-2 (Infuse; Medtronic, Fridley, MN, USA) utilized in our study was 0.75 mg/mL.
3. Data Collection
Patient demographic, comorbidity, and perioperative data were collected for each patient. Demographic and comorbidity information included age, sex, body mass index (BMI), smoking status, comorbidity burden, and preoperative pain. Of note, comorbidity burden was assessed using a modified Charlson comorbidity index (CCI) with the age component removed in order to evaluate age and comorbidity burden separately. Perioperative characteristics collected included operative time, estimated intraoperative blood loss, procedure level, and length of postoperative stay. Complications that occurred during the perioperative period and up to 1 year postoperatively were recorded.
Patient-reported outcome (PRO) questionnaires were completed preoperatively and at the 6-week, 12-week, 6-month, and 1-year postoperative time points. PRO measures included visual analogue scale (VAS) back pain, VAS leg pain, and Oswestry Disability Index (ODI). Achievement of minimum clinically important difference (MCID) for improvement in PROs at final follow-up was determined using values proposed by Copay et al. [21]. MCID cut-offs for VAS back, VAS leg, and ODI were set at -1.2, -1.6, and -12.8, respectively.
4. Statistical Analysis
Statistical analysis was performed using Stata ver. 13.0 (Stata-Corp LP, College Station, TX, USA). Demographic and perioperative characteristics were compared between ICBG and BMP-2 cohorts using chi-square analysis and independent t-tests for categorical and continuous variables, respectively. Complication and reoperation rates were assessed for the perioperative period and up to 1 year postoperatively using chi-square analysis. Postoperative changes in PROs were compared between cohorts using independent t-tests. Rates of MCID achievement at final follow-up for ODI, VAS back, and VAS leg scores were compared between groups using chi-square analysis. Statistical significance was set at p<0.05.
RESULTS
A total of 149 patients were included in this analysis, 101 (67.8%) in the BMP-2 cohort and 48 (32.2%) in the ICBG cohort. For the BMP-2 cohort, 122 patients had undergone the operation during the study period, but 21 patients were excluded from our study due to having follow-up periods shorter than 6 months. This resulted in 82.8% (101 of 122) of patients who received BMP-2 being included in our study. For the ICBG cohort, 57 patients had undergone the operation during the study period, but 48 patients were included in our study due to the rest having follow-up periods shorter than 6 months. This resulted in 84.2% (48 of 57) of patients who received ICBG being included in our study. Mean length of postoperative follow-up was 9.7 months (range, 6–12 months). Preoperative characteristics of the BMP-2 and ICBG cohorts are detailed in Table 1. There were no significant differences between groups with regard to age, sex, BMI, smoking status, comorbidity burden, or preoperative pain.
Table 1.
Baseline characteristics by bone graft type
| Characteristic | BMP-2 (n = 101) | ICBG (n = 48) | p-value† |
|---|---|---|---|
| Age (yr) | 51.9 ± 12.4 | 53.2 ± 10.7 | 0.524 |
| Sex | 0.069 | ||
| Female | 29 (28.7) | 21 (43.8) | |
| Male | 72 (71.3) | 27 (56.2) | |
| Body mass index | 0.511 | ||
| Nonobese (< 30 kg/m2) | 51 (50.5) | 27 (56.3) | |
| Obese (≥ 30 kg/m2) | 50 (49.5) | 21 (43.7) | |
| Smoking status | 0.302 | ||
| Nonsmoker | 84 (83.2) | 43 (89.6) | |
| Smoker | 17 (16.8) | 5 (10.4) | |
| Ageless CCI | 1.0 ± 1.2 | 0.9 ± 1.0 | 0.609 |
| Preoperative VAS pain | 6.9 ± 2.0 | 7.3 ± 1.8 | 0.229 |
Values are presented as mean±standard deviation or number (%).
BMP-2, bone morphogenetic protein-2; ICBG, iliac crest bone graft; CCI, Charlson comorbidity index; VAS, visual analogue scale.
p-values calculated using chi-square analysis for categorical variables and independent t-tests for continuous variables.
Table 2 compares perioperative characteristics and complication rates for the BMP-2 and ICBG cohorts. ICBG patients experienced a longer operative time compared to BMP-2 patients (119.2 minutes vs. 110.6 minutes, p=0.062); however, this did not reach statistical significance. The ICBG cohort demonstrated a greater estimated intraoperative blood loss (62.5 mL vs. 50.0 mL, p=0.026) though this was not clinically significant. No differences in operative level were observed between cohorts (p>0.05). Additionally, patients in the ICBG cohort had a significantly shorter length of stay (29.9 hours vs. 36.1 hours, p=0.043). No inpatient complications occurred in the ICBG group and 2 patients in the BMP-2 cohort experienced altered mental status, who were noted to experience transient, mild disorientation immediately following surgery while in the postanesthesia recovery setting. However, both patients quickly recovered and were discharged from the hospital on postoperative day 1 with otherwise no complications. The only observed surgical complication was a superficial wound infection at 6-week follow-up and occurred in the BMP-2 group. One patient in each cohort underwent a subsequent procedure in the first postoperative year. The BMP-2 patient received an L5-S1 anterior lumbar interbody fusion for adjacent segment disease 11 months following L4–5 MIS TLIF. The ICBG patient received an L2–3 lateral lumbar interbody fusion 8 months following an L4–5 MIS TLIF for unrelated pathology.
Table 2.
Operative characteristics and complication rates by bone graft type
| Variable | BMP-2 (n = 101) | ICBG (n = 48) | p-value† |
|---|---|---|---|
| Operative time (min) | 110.6 ± 25.6 | 119.2 ± 27.4 | 0.062 |
| Estimated blood loss (mL) | 50.1 ± 24.7 | 62.5 ± 42.3 | 0.026* |
| Operative level | 0.278 | ||
| L2–3 | 1 (1.0) | 0 (0) | |
| L3–4 | 6 (5.9) | 0 (0) | |
| L4–5 | 48 (47.5) | 22 (45.8) | |
| L5–S1 | 46 (45.5) | 26 (54.2) | |
| Length of hospital stay (hr) | 36.1 ± 17.4 | 29.9 ± 17.6 | 0.043* |
| Complications‡ | |||
| Inpatient | 2 (2.0) | 0 (0) | - |
| Postoperative | 1 (1) | 0 (0) | - |
| Reoperation§ | 1 (1) | 1 (2.1) | - |
Values are presented as mean±standard deviation or number (%).
BMP-2, bone morphogenetic protein-2; ICBG, iliac crest bone graft.
p<0.05, statistically significant differences.
p-values calculated using chi-square analysis (categorical) and independent t-tests (continuous).
Complications included altered mental status (n=2) and superficial wound infection at 6 weeks postoperative (n=1).
Reasons for reoperation included adjacent segment disease (n=1) and unrelated pathology (n=1).
Postoperative changes in PROs from preoperative values are described in Table 3. ICBG and BMP-2 patients demonstrated similar improvements in ODI and VAS back pain scores at all postoperative time points (Figs. 1, 2). The ICBG cohort reported significantly greater improvement in VAS leg pain at 6 weeks (-3.6 vs. -2.4, p=0.035) and 12 weeks (-4.3 vs. -2.9, p=0.014), but not at subsequent time points (Fig. 3). No differences in rates of MCID achievement for ODI, VAS back, or VAS leg were observed between groups at final follow-up (Table 4).
Table 3.
Change in patient-reported outcomes by bone graft type
| Variable | BMP-2 (n = 101) | ICBG (n = 48) | p-value† |
|---|---|---|---|
| VAS back | |||
| Preoperative | 6.2 ± 2.5 | 5.9 ± 2.7 | 0.432 |
| 6-Week Δ | -2.2 ± 2.8 | -2.2 ± 3.3 | 0.903 |
| 12-Week Δ | -2.7 ± 2.9 | -3.0 ± 2.5 | 0.555 |
| 6-Month Δ | -2.9 ± 3.1 | -2.8 ± 3.4 | 0.922 |
| 1-Year Δ | -3.2 ± 3.3 | -3.5 ± 3.5 | 0.677 |
| VAS leg | |||
| Preoperative | 5.3 ± 2.7 | 6.1 ± 2.9 | 0.090 |
| 6-Week Δ | -2.4 ± 3.4 | -3.6 ± 3.0 | 0.035* |
| 12-Week Δ | -2.9 ± 2.9 | -4.3 ± 2.9 | 0.014* |
| 6-Month Δ | -3.1 ± 3.0 | -4.0 ± 3.0 | 0.064 |
| 1-Year Δ | -3.2 ± 3.4 | -3.8 ± 3.7 | 0.476 |
| ODI | |||
| Preoperative | 41.0 ± 16.4 | 37.9 ± 17.0 | 0.281 |
| 6-Week Δ | -5.0 ± 19.6 | -8.2 ± 15.8 | 0.339 |
| 12-Week Δ | -12.0 ± 17.4 | -13.0 ± 15.7 | 0.768 |
| 6-Month Δ | -17.4 ± 19.7 | -18.0 ± 17.8 | 0.854 |
| 1-Year Δ | -19.2 ± 18.4 | -20.0 ± 19.1 | 0.843 |
Values are presented as mean±standard deviation.
BMP-2, bone morphogenetic protein-2; ICBG, iliac crest bone graft; VAS, visual analogue scale; ODI, Oswestry Disability Index.
Δ=postoperative ODI/VAS – preoperative ODI/VAS.
p<0.05, statistically significant differences.
p-values calculated using independent t-tests.
Fig. 1.
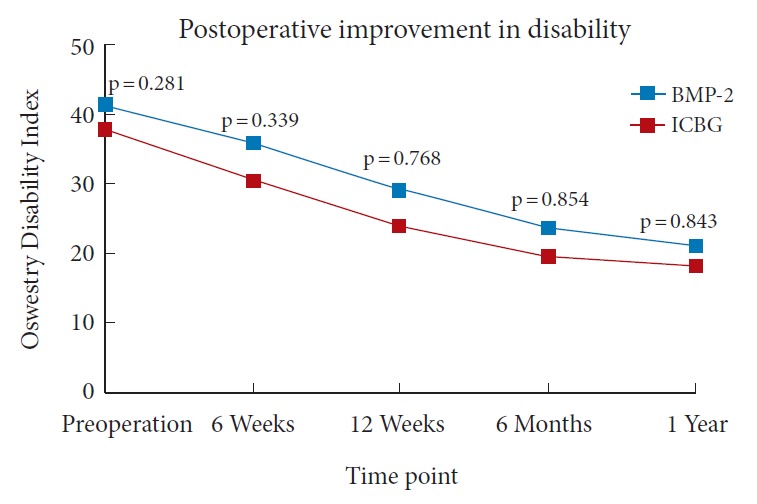
Line graph demonstrating Oswestry Disability Index scores preoperatively and up to 1 year postoperatively for ICBG and BMP-2 cohorts. BMP-2, bone morphogenetic protein-2; ICBG, iliac crest bone graft.
Fig. 2.
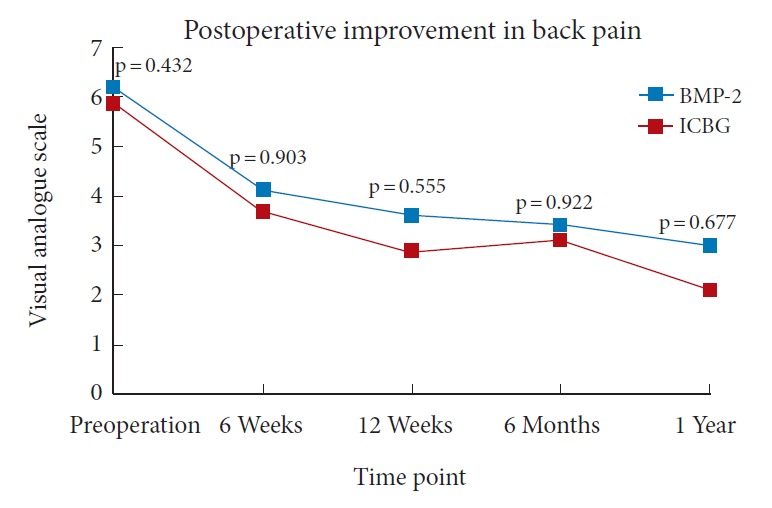
Line graph demonstrating visual analogue scale back pain scores preoperatively and up to 1 year postoperatively for ICBG and BMP-2 cohorts. BMP-2, bone morphogenetic protein-2; ICBG, iliac crest bone graft.
Fig. 3.
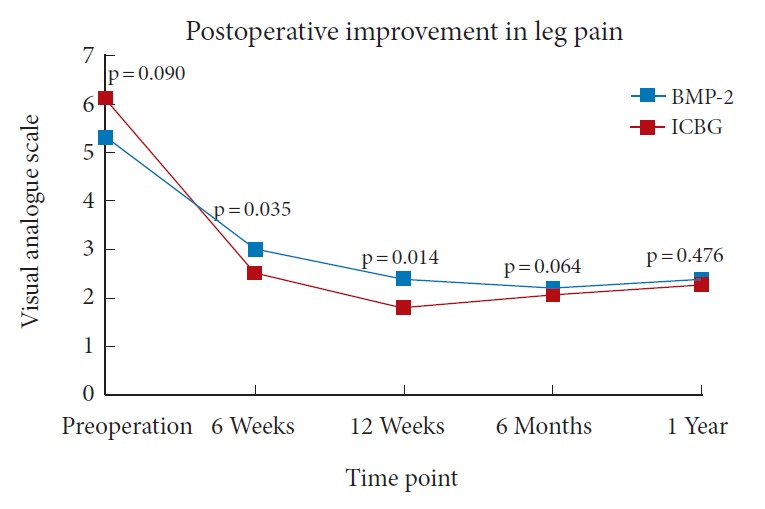
Line graph demonstrating visual analogue scale leg pain scores preoperatively and up to 1 year postoperatively for ICBG and BMP-2 cohorts. BMP-2, bone morphogenetic protein-2; ICBG, iliac crest bone graft.
Table 4.
Achievement of minimum clinically important difference at final follow-up
| Variable | BMP-2 (n = 101) | ICBG (n = 48) | p-value† |
|---|---|---|---|
| VAS back | 72 (71.3) | 33 (68.8) | 0.751 |
| VAS leg | 63 (62.4) | 31 (64.6) | 0.794 |
| ODI | 60 (59.4) | 30 (62.5) | 0.718 |
Values are presented as number (%).
BMP-2, bone morphogenetic protein-2; ICBG, iliac crest bone graft; VAS, visual analogue scale; ODI, Oswestry Disability Index.
p-values calculated using chi-square analysis.
DISCUSSION
ICBG is an effective graft option for lumbar fusion procedures. However, concerns exist regarding postoperative donor site pain and morbidity associated with ICBG techniques [22,23]. While previous studies have investigated the relationship between bone graft technique and lumbar fusion outcomes [24-26], the effect of ICBG using a minimally invasive technique on postoperative outcomes following MIS TLIF has not been well-defined.
In the present study, use of ICBG was associated with small increases in estimated intraoperative blood loss of 12 mL and shorter postoperative hospital stay of 6 hours. Low complication rates were demonstrated for both ICBG and BMP-2 cohorts during the inpatient stay and first postoperative year. Only one patient required a reoperation related to the index procedure and this occurred in the BMP-2 cohort. Finally, postoperative improvements in PROs were comparable among patients receiving ICBG or BMP-2 during MIS TLIF.
Minimally invasive ICBG harvesting was not associated with an increased complication rate in the present study, without complications identified in this cohort. This complication rate is lower than demonstrated in previous studies within the spine literature. Among patients undergoing MIS TLIF with ICBG, reported complication rates range from 5.0%–16.66% [17,27-30], with the most common complications being iliac crest bone infections and superficial wound infections. A systematic review performed by Tuchman et al. [18] investigated the efficacy of ICBG in lumbar fusions compared to allograft or local autograft. A total of 6 studies were identified comparing outcomes between ICBG and non-ICBG cohorts. Although complications were reported inconsistently across included studies, no differences in infection, dural tear, pedicle screw misplacement, or instrumentation failure rates were observed between treatment groups. However, donor site-specific complications, including donor site pain, hematoma/seroma, and sensory loss, were reported to occur more frequently in ICBG cohorts. When comparing use of ICBG to BMP in lumbar fusion patients, the literature has reported similar rates of perioperative complications (23% for each, p=0.771) but higher rates of donor site complications (7% vs. 0%, p=0.001) and complications requiring surgical treatment (20% vs. 12%, p=0.006), among ICBG cohorts [25]. The present study did not identify an increased complication rate among ICBG patients or any reported donor site complications, which suggests that the use of minimally invasive techniques for ICBG harvesting may limit the morbidity previously associated with the procedure.
Postoperative improvement in PROs is a primary focus after spinal procedures such as MIS TLIF. This is magnified with the use of ICBG, as donor site harvesting is thought to lead to increased pain and disability. This study demonstrated that patients receiving ICBG do not experience inferior outcomes with respect to ODI and VAS back and leg pain. In fact, ICBG patients may experience greater improvements in VAS leg pain during the first several months of recovery. One possible explanation for this finding may be the development of postoperative radiculitis from BMP use, leading to comparatively less improvement in leg pain in the BMP cohort [13,31,32].
Similar outcomes have been reported in a meta-analysis by Noshchenko et al. [25] comparing the use of ICBG and BMP in lumbar fusion procedures. After pooling data from 8 eligible studies, no significant differences in postoperative improvement for ODI, VAS back, or VAS leg pain scores were identified between ICBG and BMP cohorts. Interestingly, donor site pain was reported to occur in 49% of patients at 24-month follow-up. However, it is important to note that subsequent reports have suggested that donor pain is overreported in the literature [6,33,34]. While donor site pain was not explicitly assessed in the present study, anecdotally, no patients reported donor site pain at their follow-up clinic visits. This supports the idea that donor site pain may be overreported within the literature. Furthermore, the use of minimally invasive approaches for ICBG harvesting may play a role in limiting donor site pain. Continued investigation into true rates of donor site pain associated with various ICBG harvesting techniques is necessary. Nonetheless, the comparable improvements in pain and disability, combined with reported cost advantages and enhanced arthrodesis rates, makes ICBG an effective option for patients undergoing MIS TLIF.
A major limitation of the present study is that achievement of arthrodesis was not evaluated. This analysis instead aimed to focus on PROs with the use of minimally invasive surgical techniques. Moreover, fusion rates in the comparison of BMP-2 versus ICBG have been discussed extensively within previous literature regarding lumbar spine fusion procedures [24-26,35,36]. For instance, in a multicenter, randomized prospective study of patients undergoing posterior lumbar interbody fusion for degenerative disc disease, Haid et al. [37] found statistically insignificant differences in fusion rates between the BMP-2 and ICBG groups. Another investigation conducted by Katayama et al. [38] assessing patients undergoing posterolateral lumbar fusion who concurrently received ICBG and BMP-2 on either side demonstrated there was no statistically significant difference in the fusion rate at 2 years following surgery (82% vs. 91%). Finally, in a meta-analysis of 13 randomized controlled trials and 31 cohort studies, Fu et al. [35] concluded that BMP-2 and ICBG were similar in attaining successful fusion rates, which ranged from 77% to 93% at the 2-year postoperative timepoint in both cohorts. These findings from the literature, along with the results we demonstrated in our study regarding the comparable perioperative outcomes, complication rates, and PROs between BMP-2 and ICBG demonstrate that ICBG may be a safe and effective option. Further studies will need to be conducted in order to include long-term fusion rates as evaluated by radiographic results in patients after undergoing MIS TLIF.
This study has additional limitations. First, all patients were treated by a single surgeon at a single institution, which may limit the generalizability of these results to a broader, more diverse patient population. Second, the data we analyzed in our study may not follow a normal distribution, such as the ODI, VAS, and CCI scores. In these cases, other methods of statistical analysis such as the Mann-Whitney U-test can be utilized. Nevertheless, the t-test is commonly employed in the spine literature for PROs. Third, the incidence of donor site pain was not specifically evaluated in this patient population. While no patients in this cohort reported pain at the donor site at their postoperative clinic visits, more work is needed to determine the true rates of donor site pain associated with minimally invasive ICBG harvesting techniques. Finally, some patients may have been treated for complications outside of the institution in which this study was performed. As such, the complication rates may be slightly underestimated in this analysis. However, we believe that our practice is relatively closed and the incidence of unreported complications to be relatively low.
CONCLUSION
Patients undergoing MIS TLIF with ICBG experienced clinically insignificant increases in estimated intraoperative blood loss as compared to those receiving BMP-2. Use of ICBG was not associated with an increased complication rate. Additionally, ICBG patients did not experience increases in postoperative pain or disability compared to BMP-2 patients. These results, coupled with the advantages in arthrodesis promotion and cost savings, suggest that the use of ICBG is a safe and effective option for patients undergoing MIS TLIF. Additional investigation is needed to determine long-term outcomes and rates of donor site pain for patients undergoing MIS TLIF with ICBG.
Footnotes
The authors have nothing to disclose.
REFERENCES
- 1.Ahn J, Tabaraee E, Singh K. Minimally invasive transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2015;28:222–5. doi: 10.1097/BSD.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 2.Holly LT, Schwender JD, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006;20:E6. doi: 10.3171/foc.2006.20.3.7. [DOI] [PubMed] [Google Scholar]
- 3.Kornblum MB, Fischgrund JS, Herkowitz HN, et al. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine (Phila Pa 1976) 2004;29:726–33. doi: 10.1097/01.brs.0000119398.22620.92. [DOI] [PubMed] [Google Scholar]
- 4.Galimberti F, Lubelski D, Healy AT, et al. A systematic review of lumbar fusion rates with and without the use of rh-BMP-2. Spine (Phila Pa 1976) 2015;40:1132–9. doi: 10.1097/BRS.0000000000000971. [DOI] [PubMed] [Google Scholar]
- 5.Simon SR. Orthopaedic basic science. Rosemont (IL): American Academy of Orthopaedic; 1994. [Google Scholar]
- 6.Howard JM, Glassman SD, Carreon LY. Posterior iliac crest pain after posterolateral fusion with or without iliac crest graft harvest. Spine J. 2011;11:534–7. doi: 10.1016/j.spinee.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Myeroff C, Archdeacon M. Autogenous bone graft: donor sites and techniques. J Bone Joint Surg Am. 2011;93:2227–36. doi: 10.2106/JBJS.J.01513. [DOI] [PubMed] [Google Scholar]
- 8.Radcliff K, Hwang R, Hilibrand A, et al. The effect of iliac crest autograft on the outcome of fusion in the setting of degenerative spondylolisthesis: a subgroup analysis of the Spine Patient Outcomes Research Trial (SPORT) J Bone Joint Surg Am. 2012;94:1685–92. doi: 10.2106/JBJS.K.00952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mannion RJ, Nowitzke AM, Wood MJ. Promoting fusion in minimally invasive lumbar interbody stabilization with low-dose bone morphogenic protein-2--but what is the cost? Spine J. 2011;11:527–33. doi: 10.1016/j.spinee.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Dimitriou R, Mataliotakis GI, Angoules AG, et al. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury. 2011;42 Suppl 2:S3–15. doi: 10.1016/j.injury.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Grabowski G, Cornett CA. Bone graft and bone graft substitutes in spine surgery: current concepts and controversies. J Am Acad Orthop Surg. 2013;21:51–60. doi: 10.5435/JAAOS-21-01-51. [DOI] [PubMed] [Google Scholar]
- 12.Alvin MD, Derakhshan A, Lubelski D, et al. Cost-utility analysis of 1- and 2-level dorsal lumbar fusions with and without recombinant human bone morphogenic protein-2 at 1-year follow-up. Clin Spine Surg. 2016;29:E28–33. doi: 10.1097/BSD.0000000000000079. [DOI] [PubMed] [Google Scholar]
- 13.Muchow RD, Hsu WK, Anderson PA. Histopathologic inflammatory response induced by recombinant bone morphogenetic protein-2 causing radiculopathy after transforaminal lumbar interbody fusion. Spine J. 2010;10:e1–6. doi: 10.1016/j.spinee.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 14.Park JH, Bae YK, Suh SW, et al. Efficacy of cortico/cancellous composite allograft in treatment of cervical spondylosis. Medicine (Baltimore) 2017;96:e7803. doi: 10.1097/MD.0000000000007803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Than KD, Rahman SU, McKeever PE, et al. Symptomatic calcified perineural cyst after use of bone morphogenetic protein in transforaminal lumbar interbody fusion: a case report. Spine J. 2013;13:e31–35. doi: 10.1016/j.spinee.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann MF, Jones CB, Sietsema DL. Adjuncts in posterior lumbar spine fusion: comparison of complications and efficacy. Arch Orthop Trauma Surg. 2012;132:1105–10. doi: 10.1007/s00402-012-1529-0. [DOI] [PubMed] [Google Scholar]
- 17.Parajón A, Alimi M, Navarro-Ramirez R, et al. Minimally invasive transforaminal lumbar interbody fusion: meta-analysis of the fusion rates. what is the optimal graft material? Neurosurgery. 2017;81:958–71. doi: 10.1093/neuros/nyx141. [DOI] [PubMed] [Google Scholar]
- 18.Tuchman A, Brodke DS, Youssef JA, et al. Iliac crest bone graft versus local autograft or allograft for lumbar spinal fusion: a systematic review. Global Spine J. 2016;6:592–606. doi: 10.1055/s-0035-1570749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1:2–18. doi: 10.3978/j.issn.2414-469X.2015.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lopez GD, Hijji FY, Narain AS, et al. Iliac crest bone graft: a minimally invasive harvesting technique. Clin Spine Surg. 2017;30:439–41. doi: 10.1097/BSD.0000000000000556. [DOI] [PubMed] [Google Scholar]
- 21.Copay AG, Glassman SD, Subach BR, et al. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008;8:968–74. doi: 10.1016/j.spinee.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Robertson PA, Wray AC. Natural history of posterior iliac crest bone graft donation for spinal surgery: a prospective analysis of morbidity. Spine (Phila Pa 1976) 2001;26:1473–6. doi: 10.1097/00007632-200107010-00018. [DOI] [PubMed] [Google Scholar]
- 23.Heary RF, Schlenk RP, Sacchieri TA, et al. Persistent iliac crest donor site pain: independent outcome assessment. Neurosurgery. 2002;50:510–6. doi: 10.1097/00006123-200203000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Zhang H, Wang F, Ding L, et al. A meta analysis of lumbar spinal fusion surgery using bone morphogenetic proteins and autologous iliac crest bone graft. PLoS One. 2014;9:e97049. doi: 10.1371/journal.pone.0097049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noshchenko A, Hoffecker L, Lindley EM, et al. Perioperative and long-term clinical outcomes for bone morphogenetic protein versus iliac crest bone graft for lumbar fusion in degenerative disk disease: systematic review with meta-analysis. J Spinal Disord Tech. 2014;27:117–35. doi: 10.1097/01.bsd.0000446752.34233.ca. [DOI] [PubMed] [Google Scholar]
- 26.Chen Z, Ba G, Shen T, et al. Recombinant human bone morphogenetic protein-2 versus autogenous iliac crest bone graft for lumbar fusion: a meta-analysis of ten randomized controlled trials. Arch Orthop Trauma Surg. 2012;132:1725–40. doi: 10.1007/s00402-012-1607-3. [DOI] [PubMed] [Google Scholar]
- 27.Peng CW, Yue WM, Poh SY, et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009;34:1385–9. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 28.Shunwu F, Xing Z, Fengdong Z, et al. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976) 2010;35:1615–20. doi: 10.1097/BRS.0b013e3181c70fe3. [DOI] [PubMed] [Google Scholar]
- 29.Seng C, Siddiqui MA, Wong KP, et al. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: a matched-pair comparison study. Spine (Phila Pa 1976) 2013;38:2049–55. doi: 10.1097/BRS.0b013e3182a8212d. [DOI] [PubMed] [Google Scholar]
- 30.Jang JS, Lee SH. Minimally invasive transforaminal lumbar interbody fusion with ipsilateral pedicle screw and contralateral facet screw fixation. J Neurosurg Spine. 2005;3:218–23. doi: 10.3171/spi.2005.3.3.0218. [DOI] [PubMed] [Google Scholar]
- 31.Rowan FE, O'Malley N, Poynton A. RhBMP-2 use in lumbar fusion surgery is associated with transient immediate post-operative leg pain. Eur Spine J. 2012;21:1331–7. doi: 10.1007/s00586-011-2113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Owens K, Glassman SD, Howard JM, et al. Perioperative complications with rhBMP-2 in transforaminal lumbar interbody fusion. Eur Spine J. 2011;20:612–7. doi: 10.1007/s00586-010-1494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pirris SM, Nottmeier EW, Kimes S, et al. A retrospective study of iliac crest bone grafting techniques with allograft reconstruction: do patients even know which iliac crest was harvested? Clinical article. J Neurosurg Spine. 2014;21:595–600. doi: 10.3171/2014.6.SPINE13902. [DOI] [PubMed] [Google Scholar]
- 34.Delawi D, Dhert WJ, Castelein RM, et al. The incidence of donor site pain after bone graft harvesting from the posterior iliac crest may be overestimated: a study on spine fracture patients. Spine (Phila Pa 1976) 2007;32:1865–8. doi: 10.1097/BRS.0b013e318107674e. [DOI] [PubMed] [Google Scholar]
- 35.Fu R, Selph S, McDonagh M, et al. Effectiveness and harms of recombinant human bone morphogenetic protein-2 in spine fusion: a systematic review and meta-analysis. Ann Intern Med. 2013;158:890–902. doi: 10.7326/0003-4819-158-12-201306180-00006. [DOI] [PubMed] [Google Scholar]
- 36.Ye F, Zeng Z, Wang J, et al. Comparison of the use of rhBMP-7 versus iliac crest autograft in single-level lumbar fusion: a meta-analysis of randomized controlled trials. J Bone Miner Metab. 2018;36:119–27. doi: 10.1007/s00774-017-0821-z. [DOI] [PubMed] [Google Scholar]
- 37.Haid RW, Jr, Branch CL, Jr, Alexander JT, et al. Posterior lumbar interbody fusion using recombinant human bone morphogenetic protein type 2 with cylindrical interbody cages. Spine J. 2004;4:527–38. doi: 10.1016/j.spinee.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 38.Katayama Y, Matsuyama Y, Yoshihara H, et al. Clinical and radiographic outcomes of posterolateral lumbar spine fusion in humans using recombinant human bone morphogenetic protein-2: an average five-year follow-up study. Int Orthop. 2009;33:1061–7. doi: 10.1007/s00264-008-0600-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


