Abstract
Congenital abnormalities of the kidney and urinary tract (CAKUT) are a highly diverse group of diseases that together belong to the most common abnormalities detected in the new-born child. Consistent with this diversity, CAKUT are caused by mutations in a large number of genes and present a wide spectrum of phenotypes. In this review, we will focus on duplex kidneys, a relatively frequent form of CAKUT that is often asymptomatic but predisposes to vesicoureteral reflux and hydronephrosis. We will summarise the molecular programs responsible for ureter induction, review the genes that have been identified as risk factors in duplex kidney formation and discuss molecular and cellular mechanisms that may lead to this malformation.
Keywords: CAKUT, kidney development, duplex systems, ureter budding
Introduction
The urinary tract, composed of the kidneys, ureters, bladder and urethra, represents the main excretory system of the mammalian organism. Development of the urinary system, made up of more than 40 different cell types, needs to proceed in a highly organised manner. Given this complexity, it is not surprising that mutations in developmental genes can lead to a wide variety of abnormalities that are usually grouped together as congenital abnormalities of the kidneys and urinary tract (CAKUT). Defects affecting the kidneys range from renal agenesis (a complete lack of kidney development) to hypoplasia (reduced size), dysplasia (abnormally developed tissue), cystic dysplasia, and terminal differentiation defects. Lower urinary tract malformations include vesicoureteral reflux (VUR), hypospadias (opening of the urethra at the lower side of the penis) and posterior urethral valves that often lead to outflow obstructions. Although individual malformations are considered rare diseases, CAKUT, taken together, have an incidence of about 3 to 6 in 1000 live births and thus belong to the most frequent abnormalities detected in the new-born child 1. An in-depth presentation of all subclasses and their aetiology would be far beyond the scope of this review and therefore interested readers are referred to other publications that present an overview of CAKUT phenotypes and the genetics underlying them 2– 6. Here, we will instead concentrate on duplex (or multiplex) kidneys, a very frequent subclass of CAKUT, which is often neglected in the literature.
Development of the urinary system
To understand the aetiology of duplex kidneys, it is important to consider how the urinary system forms. From a developmental point of view, the urogenital tract derives from two independent germ layers with kidneys and ureters arising from the intermediate mesoderm (IM) and the bladder and urethra developing from cloacal endoderm 7. Accordingly, malformations of the urinary system can be further classified into congenital abnormalities of the upper and lower urinary tract (and the latter are sometimes abbreviated as CALUT). Despite this developmental distinction, it should be noted that some authors group malformations of the ureter as part of congenital abnormalities of the lower urinary tract.
Kidney development in mammals commences with the formation of the nephric duct (ND) at the anterior (rostral) pole of the IM. As development proceeds, epithelial cells of the ND proliferate and actively migrate towards the caudal end of the nephrogenic cord 8– 10. Eventually, the ND fuses with the cloaca, a process that involves dedicated apoptosis and requires GATA3 and LHX1 as well as retinoic acid and RET and FGF signalling 9– 13.
As the ND elongates caudally, a series of tubules forms within the nephrogenic cord. The most anteriorly positioned pronephric tubules are considered an evolutionary remnant and are non-functional in mammals. Subsequently, a wave of mesonephric tubules develop that fall into two groups. While rostrally positioned tubules are connected to the ND and serve as an embryonic kidney, more caudally located tubules do not drain into the ND and are non-functional 14, 15. Both pronephros and mesonephros are transitory structures in the mammalian embryo and disappear (pronephros) or are remodelled (mesonephros) at later stages of development.
The metanephros represents the permanent kidney in mammals and develops at the most caudal position of the IM. Metanephros development is first detectable as a population of slightly condensed mesenchymal cells within the nephrogenic cord which express a set of molecular markers ( HOX11, SIX2, GDNF, EYA1) 15, 16. In normal development, signalling from the metanephric mesenchyme (MM) induces the formation and outgrowth of a single ureteric bud (UB) from the ND, which will invade the MM and undergo a first stereotypic dichotomous branching event (T-shaped ureter). The collecting duct system (ureteric tree) forms through further rounds of branching that often include tri-tips, which, however, eventually resolve into ureter bifurcations 17, 18. In return, signals released from the ureter will induce the MM to differentiate into nephrons, the functional units of the kidney. For further details on this process, we refer the reader to recent reviews 19– 22.
Development of the urinary system is not restricted to kidney formation but also involves extensive developmental remodelling of the lower tract. An excellent and detailed description of this complex process can be found in 7. In brief, the emerging UB is initially connected to the cloaca via the distal part of the ND, also termed the common nephric duct (CND). Downgrowth of the urorectal septum leads to a separation of the cloaca into a ventrally located urogenital sinus and a dorsally positioned anorectal sinus 7, 23– 25. The cranial urogenital sinus will further elongate to develop into the bladder, whereas its posterior portion will form the urethra. As development proceeds, apoptosis eliminates the CND, leading to the fusion of the ureter with the future bladder, thus creating the ureterovesical junction 26.
Classification and epidemiology of duplex kidneys
Duplex systems can have a variety of phenotypes, and multiple classification systems have been proposed to categorise this pathology ( Figure 1) 27. In incomplete duplication, the two poles of a duplex kidney share the same ureteral orifice of the bladder. Such duplex kidneys with a bifid pelvis or ureter arise when an initially single UB bifurcates before it reaches the ampulla. This is likely caused by a premature first branching event that occurred before the ureter has reached the MM. Much more frequent are complete duplications, which occur when two UBs emerge from the ND. In most cases, the lower pole of the kidney is normal and the upper pole is abnormal 28, 29, an observation explained by the fact that the ectopic UB frequently emerges anteriorly to the position of the normal UB and drives the formation of the upper pole of a duplex kidney. Inverted Y-ureteral duplication is a rare condition in which two ureteral orifices drain from a single normal kidney. Inverted Y-ureteral duplication is believed to be caused by the merging of two independent UBs just before or as they reach the kidney anlagen 30. A very rare H-shaped ureter has also been reported 31. Although the vast majority of cases involve a simple duplication, multiplex ureters with up to six independent buds have also been described 32– 37. In some cases, the additional ureter or ureters are ectopic and fail to connect to the bladder or the kidney (blind ending ureter) 33.
Figure 1. Classification of duplex kidney anatomy.
Compared with a normal kidney ( a), complete duplication produces a duplex kidney with two poles that drain into two ureters ( b). Incomplete duplication leads to a Y-shaped ureter ( c). Blind ureters do not drain into the bladder ( d). In the rare case of inverted Y-ureteral duplication, two ureters fuse before entering the kidney ( e).
The aetiology of most duplex kidneys can be traced back to the very first induction steps of the ureter. In the majority of cases, an additional UB emerges in a rostral position to the normal outgrowth. By contrast, in adults, the upper (abnormal) kidney pole drains into the bladder at a site distal to the orifice of the lower kidney pole 38. This paradoxical phenomenon, known as the Weigert–Meyer rule 29, can be explained by the significant amount of remodelling occurring at the future ureter–bladder junction during development. Indeed, as apoptosis eliminates the CND, the ureter inserts into the developing bladder and moves upwards ( Figure 2) 7, 39– 41. An initially anteriorly positioned ureter thus ends up with a more distal insertion site in the bladder, a model that has been proposed by Mackie and Stephens 42. Correct positioning of the ureter into the bladder is important to allow formation of a normal trigone (the triangle formed by the two ureter orifices and the urethra) and prevent ureter reflux caused by a malfunctioning valve or a too-short ureter tunnel. Because the vast majority of duplex kidneys arise from an ectopic bud in a rostral position, it is usually the upper pole of the kidney that is affected by VUR and hydronephrosis.
Figure 2. Morphogenesis of duplex kidney.
Duplex kidneys form through the induction of two ureteric buds from the nephric duct that will invade the metanephric mesenchyme. Subsequently, apoptosis of the common nephric duct (CND) leads to the insertion of both ureters into the developing bladder with the orifice of the initially posteriorly positioned ureteric bud ending up in a superior position.
Estimates suggest a prevalence of duplex kidneys of between 0.2 and 2% in the general population, and females are affected twice as frequently as males 38, 43. The reasons for this sex bias are unknown. About 40% of patients with duplex kidneys have been reported to exhibit pathological manifestations 43. However, because duplex kidneys are frequently asymptomatic and therefore predominantly detected in patients who seek medical assistance, the actual percentage of patients with symptoms is likely to be lower. Symptoms associated with duplex kidneys can include pain, haematuria, dysuria and difficulty or abnormal frequency of micturition 38, 43. Specific manifestation of the pathology depends on the anatomy of each duplication event 44. Furthermore, duplex kidneys are linked to a number of renal disorders, including pelvi-calyceal dilatation, cortical scarring, VUR, hydronephrosis, ureterocoeles on the non-duplex side, caliculi or yo-yo reflux (in the incomplete duplication cases) 38, 43.
Molecular pathways controlling ureter induction
If duplex kidney formation is rooted in the formation of two ureteric tips, how can we explain the outgrowth of supernumerary buds on a molecular level? Interactions between MM and the ND are crucial to ensure the induction of the ureter from the ND, and a key pathway controlling this process is the GDNF/RET signalling axis ( Figure 3) 45. GDNF, a distant member of the transforming growth factor beta (TGFβ) superfamily of signalling molecules, is specifically expressed within the MM, whereas its cognate receptor RET is expressed along the entire length of the ND. Binding of GDNF to RET is greatly facilitated by the co-receptor GFRα1. The requirement for these genes in ureter outgrowth has been extensively demonstrated by using gene targeting in mice, and homozygous mutations in either of these genes leads to a failure of ureter induction and consequently renal agenesis 46– 50. Binding of GDNF to the receptor tyrosine kinase RET induces autophosphorylation and recruitment of the tyrosine phosphatase SHP2 51, 52, which results in the activation of several intracellular signalling cascades, including RAS/MAPK, PLCγ/Ca 2+, PI3K-AKT 53, and culminates in the transcriptional activation of a set of downstream target genes 54. Ureter branching appears to involve, in particular, the ERK/MAPK pathway, and mice lacking the kinases Mek1 and Mek2 fail to form a properly branched ureteric tree 55. Activated RET signalling induces not only proliferation but also cellular motility. Indeed, experiments in chimeric mice demonstrated that wild-type cells move towards the tip of the UB but that Ret mutant cells are left behind 56. This cellular sorting mechanism ensures a strong and directed response that, under normal circumstances, results in the outgrowth of a single UB.
Figure 3. Molecular interactions during kidney development.
GDNF-RET signalling is at the core of the signalling network in kidney development and is responsible for ureteric bud (UB) emergence. GDNF expression is positively modulated by factors expressed in metanephric mesenchyme (PAX2, EYA1 and SALL1) and negatively (probably in an indirect manner) by SOX11, FOXC1, FOXC2 and ROBO2 in anterior domains of the nephrogenic cord. Ectopic formation of the UB is prevented by the factors expressed in nephric duct (SLIT2, SPRY1 and GATA3) and in the enveloping mesenchyme (BMP4 and FAT4). Influence from other upstream factors leads to the formation of a complex regulatory landscape.
Factors regulating Gdnf expression
Given the crucial function of Gdnf in ureter induction, we need to consider how the expression of this gene is regulated. Activation of Gdnf in the mesenchyme relies on a set of transcription factors, including SALL1, PAX2 and EYA1. Deletion of either of these factors in mice leads to a lack of ureter induction and consequently to renal agenesis 57– 59 . Heterozygous mutations in each of these genes have been shown to be involved in CAKUT 5, 6, and SALL1, in particular, has also been linked to duplex kidney formation 60. In addition, Gdnf mRNA levels appear to be regulated post-transcriptionally via its 3’ untranslated region (UTR). Indeed, replacement with a heterologous UTR sequence resulted in increased Gdnf expression levels that were associated with ND remodelling defects independent of apoptosis 61.
In the mouse, Gdnf expression commences in rostral domains of the nephrogenic cord at embryonic day 9.5 (E9.5), about 1 day before ureter induction. The ND, however, does not respond to the GDNF signal in those anterior regions and this is likely to be due to two reasons: First, the anterior IM has relatively high levels of BMP signalling, which is known to suppress ureter branching (see the ‘Restricting Ret activation’ section below). Second, SLIT/ROBO signalling, a pathway that is known for its role in axon repulsion 62, appears to repulse Gdnf-expressing cells from the ND, thus causing a physical separation of these two structures in anterior regions 63. Robo2 knockout mice lack this separation and show ectopic buds along the entire length of the ND 64. The physical separation of ND and Gdnf-expressing cells may explain why in Foxc1, Foxc2 and Sox11 mouse mutants, which all display a dramatic expansion of Gdnf expression, the ND does not respond in the anterior domain 64– 66. Instead, only the region just rostrally to the normal site of induction responds by forming a second ureter. Mutations in ROBO2, SLIT2 and its associated GTPase-activating protein SRGAP2 are found in patients with VUR and duplex systems 67, 68.
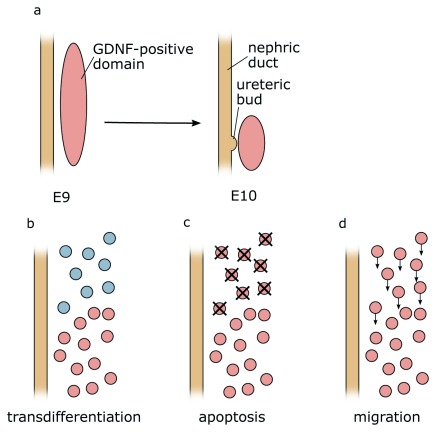
By the time of ureter induction (E10.5 in mice), mesenchymal cells that express Gdnf become restricted to the caudal part of the MM ( Figure 4). Three possible mechanisms for this restriction could be envisaged: (1) Active suppression of Gdnf expression in more rostral domains could occur. Since the expression of Foxc1 and Sox11 overlaps with the Gdnf domain, active suppression of the latter seems unlikely. (2) Gdnf-positive cells at the rostral end could undergo cell death. The pro- and mesonephros are known to be subject to massive apoptosis, although this seems to affect, in particular, the epithelial cells of tubules. However, preliminary data from our lab suggest that mesenchymal cells positioned just rostrally of the Gdnf-expressing domain also undergo apoptosis. (3) Finally, rostrally positioned Gdnf-positive cells may undergo directed migration towards the caudal end. The proposed distinct origin of ND and MM from the anterior and posterior IM, respectively, would argue against this possibility 16. However, Slit/Robo signalling and members of the SoxC class genes have been implicated in cell migration 62, 69. Perhaps Gdnf restriction is a combination of several mechanisms, including cell clearance through apoptosis and directed cell migration of anteriorly positioned Gdnf-positive cells. A careful analysis of mouse mutants showing an expansion of the Gdnf expression domain, perhaps coupled with live imaging in explant cultures, may help to address this open question.
Figure 4. Possible causes of caudal Gdnf domain restriction.
( a) At early stages during development, Gdnf expression can be found in rostral domains of the intermediate mesoderm but over time becomes caudally restricted. Three mechanisms could explain this observation: ( b) active suppression of Gdnf expression in more rostral domains ( c), apoptosis of Gdnf-expressing cells ( d), or migration of the cells towards the caudal end of the intermediate mesoderm. E, embryonic day.
Pathways in nephric duct–specific activation
PAX2 not only is involved in the activation of GDNF but also is required for the expression of ND-specific genes. A key target appears to be the transcription factor GATA3, which in turn transcriptionally activates Ret. Tissue-specific knockout mice that lack Gata3 within the ND show an altered response to local growth factors (GDNF and FGF) and display premature cell differentiation and differential cell adhesion properties. As a result, cells with sufficient levels of GATA3 and RET segregate from GATA3-deficient cells and expand, forming ectopic buds and kidneys 70.
Beta-catenin, a multifunctional protein involved in cell–cell adhesion and transcriptional regulation, appears to be one of the factors involved in this growth. Conditional inactivation of β-catenin in the ND leads to a range of kidney defects, including duplex kidney formation 71. Molecular markers affected in these mutants were the transcription factors EMX2 and SOX9, both of which are known to be involved in ureter budding 72, 73. However, ectopic budding was observed only in cases where loss of β-catenin expression was mosaic 74. Hypoxia-induced reduction of β-catenin has also been shown to cause duplex kidneys amongst other CAKUT phenotypes 75. Beta-catenin action during kidney induction is mediated at least partly through the transcription factor GATA3 70.
Sox17 mutations have been identified in a cohort of human patients with CAKUT, including a duplicated pyeloureteral system. The authors demonstrated that the mutation influenced protein stability and reduced β-catenin activity 76. It is therefore possible that the mutated SOX17 protein leads to lower β-catenin and, in turn, reduced GATA3 levels.
In parallel to GATA3, LHX1 (LIM1) appears to be essential in permitting normal budding 77. Tissue-specific deletion of LIM1 in ND derivatives leads to renal hypoplasia and hydronephrosis and an impaired extension of the ND. Some conditional mutants of Lim1 also display incomplete duplication of kidney ureters where both poles of a duplex kidney merge before entering the bladder. This form of duplex kidney was traced back to the first UB branching event, where defective UB forms a Y-shaped rather than a T-shaped structure 9.
Restricting Ret activation
To limit ureter outgrowth to a single site, a series of negative regulators that suppress the RET signalling cascade are in place. BMP signalling, in particular, seems to be a suppressor of ureter outgrowth and branching, and heterozygous Bmp4 mutations in mice lead to a wide range of CAKUT phenotypes, including duplex kidneys 78. BMP and FGF signalling are known antagonists in epithelial branching of the lung 79 but also kidney development 80. Since FGF and RET receptors are receptor tyrosine kinases that use similar intracellular signal transduction pathways, we can reason that the antagonistic action of BMP acts in analogous fashion on RET signalling. To permit ureter outgrowth specifically at the site of the future kidney, MM cells express the BMP inhibitor Gremlin ( Grem1), which counteracts the BMP function 81. Heterozygous BMP4 and GREM1 mutations have both been identified in human patients with CAKUT 82, 83, although it is not clear whether variants in these genes also predispose to duplex kidney formation.
A number of other genes involved in duplex kidney formation appear to affect the BMP/Gremlin axis. Mutants for the intraflagellar transport proteins IFT25 or IFT27, which are believed to increase GLI3R, a repressor of SHH signalling, show a high penetrance of duplex kidney formation (~50%) 84. Similarly, constitutive expression of a truncation mutation in Gli3 ( Gli3 Δ699), which is found in Pallister–Hall syndrome and is likely to sensitise tissue for SHH signalling, causes CAKUT with duplex kidneys 85. The phenotype has been linked to an increased sensitivity of the ND by lowering BMP4 signalling.
Of interest, several genes that are implicated in the formation of cilia (for example, Cep290, Dync2h1, Tbc1d32 and Tmem67) have also been implicated in duplex kidney formation 86. The primary cilia is an organelle that has a key function in cellular signalling 87, and SHH signalling, in particular, is directly linked to this organelle. Because SHH signalling has been proposed to be involved in duplex kidney formation ( 88 and above), it is tempting to speculate that the above cilia-related genes also influence this pathway.
In addition to extracellular modulators, cytoplasmic antagonists exist to suppress ureter outgrowth. Most notably, Sprouty ( Spry1) suppresses MAPK signalling in the absence of GDNF, and inactivation in mice results in the formation of multiple UBs 89. Signalling through the angiotensin receptor appears to be important in suppressing Spry1 expression 90 but also in activating Ret expression, and Agtr2 knockout mice show a range of CAKUT phenotypes, including a duplex system 91. To date, no pathogenetic SPRY1 mutations have been identified in patients with CAKUT, and it is currently unclear to what extent this gene contributes to duplex kidney formation in human patients. Interestingly, in the absence of Spry1, GDNF signalling is no longer required for ureter induction, and Spry1 -/-/Gdnf -/- double knockout mice develop normal kidneys. In this context, FGF10, which normally plays only a minor role in kidney development, becomes indispensable for kidney induction, and triple mutants ( Fgf10 -/-/Spry1 -/-/Gdnf -/-) display renal agenesis 92. FGF signalling thus can be considered a reinforcing signal that contributes to enhanced epithelial growth and budding. FGF signalling serves as the main pathway in branching morphogenesis of other organs such as the lung 93, and we can speculate that GDNF/RET signalling has taken over the ancestral function of FGF in epithelial branching of the kidney.
Finally, tissue-specific knockout of Fat4 within the nephrogenic cord results in a duplex kidney phenotype that can be rescued by reducing the dose of GDNF ( Gdnf +/-). Recent molecular experiments demonstrated that FAT4 directly binds to RET and restricts its activity in the ND/UB by disrupting the formation of RET-GFRA1-GDNF complex 94, 95.
There are a number of other genes which have been shown to be implicated in duplex kidney formation but for which the molecular events leading to supernumerary buds are not well defined. Because in these cases the causative nature of mutations for duplex kidney formation is less established, we refrain from a mere listing of genes at this place. The interested reader is referred to Table 1 of genes involved, the associated phenotypes and corresponding references.
Table 1. Genes involved in duplex kidney formation.
| Group | Genotype | Mechanism | Reference |
|---|---|---|---|
| GDNF domain | |||
| Robo2 -/- | Abnormal
Gdnf expression domain
MM fails to separate from WD |
Grieshammer
et al.
64
Wainwright et al. 63 |
|
| Slit2 -/- | Abnormal Gdnf expression domain | Grieshammer et al. 64 | |
| Foxc1 -/- | MM fails to reduce in size | Kume
et al.
65
Komaki et al. 96 |
|
| Sox11 -/- | MM fails to reduce in size | Neirijnck et al. 66 | |
| Increased
sensitivity of WD |
|||
| Bmp4 +/- | Lack of inhibition of WNT11, a target of GDNF | Miyazaki
et al.
78
Michos et al. 81 |
|
| Ift25 -/-, Ift27 -/- | Increased sensitivity of WD through Gremlin-BMP4
cascade |
Desai et al. 84 | |
| Gli3 Δ699/Δ699 | Increased sensitivity of WD through Gremlin-BMP4
cascade |
Blake et al. 85 | |
| Agtr2 -/Y | Disrupted renin-angiotensin signalling leads to aberrant
UB morphogenesis |
Nishimura
et al.
91
Yosypiv et al. 90 |
|
| p53 -/-, p53 UB-/- | Increased response of WD to GDNF signal. Two ureters
fuse in the later development and resemble a bifurcation |
Saifudeen
et al.
97
El-dahr et al. 98 |
|
| Fat4 -/- Fjx1 -/- | Premature branching with incomplete duplication due
to overactive GDNF-RET signalling |
Saburi
et al.
94
Zhang et al. 95 |
|
| Hoxb7-Cre β-catenin -/c | Ectopic activation of UB branching pathway in WD | Marose et al. 74 | |
| Spry1 -/- | Increased sensitivity of WD to GDNF-RET signalling | Basson et al. 89 | |
| Gata3ND -/- | The entire length on WD is covered by ectopic UBs,
most of which subsequently regress |
Grote et al. 70 | |
| Cell polarity
defect |
|||
| T-Cre Wnt5af l/Δ | Double UB, abnormal morphology of posterior WD,
defects in IM morphogenesis |
Yun et al. 99 | |
| Ror2 -/- | Similar to Wnt5a phenotype | Yun et al. 99 | |
| Cell adhesion
defect |
|||
| L1 -/Y | Either incomplete or complete duplication. Double UB
on WD or accessory budding from the main ureter |
Debiec et al. 100 | |
| Unknown | |||
| Pax2 +/- | Premature branching with incomplete duplication,
linked with inactivation of GDNF expression |
Brophy et al. 101 | |
| Pax2-Cre Lim1 Δ/Δ | WD fails to extend caudally; UB is absent or Y-shaped | Pedersen et al. 9 | |
|
Cc2d2a, Mks1,
Cep290, Dync2h1, Tbc1d32, Tmem67 |
Duplex kidney as a part of a ciliopathy phenotype | San agustin et al. 86 | |
| Sox17 Y259N/+ | Duplicated pyeloureteral collecting system | Gimelli et al. 76 | |
| Nfia -/- | Partial ureteral duplication | Lu et al. 102 | |
| Adamts18 -/- | Complete ureteral duplication, increased nephron
endowment |
Rutledge et al. 103 |
Conclusions and perspectives
As we have seen, the seemingly simple event of ureteric budding is a highly complicated and stringently controlled process that employs both positive and negative feedback loops. As such, the fact that a large number of genes are involved in duplex kidney formation is not surprising, and future analyses are likely to identify many more factors involved in these abnormalities. However, the incomplete penetrance of phenotypes and the multigenic basis of this malformation make the confirmation of mutations as being disease-causing increasingly difficult. Indeed, our own unpublished data suggest that duplex kidney phenotypes can be highly genetic background–dependent, indicating the presence of modifier genes. Moreover, intergenic/regulatory mutations or epigenetic mechanisms that affect gene expression levels rather than protein function are likely to contribute to disease. Finally, we should keep in mind that, despite a large degree of conservation, mice and humans show significant differences on a developmental and molecular level 104– 106. Findings in knockout mice are therefore only indicative and should not be directly extrapolated to human patients. Future research should also address the disparity in the frequency of duplex kidneys occurring in men and women. In the long run, the integration of a large amount of whole genome sequencing data coupled with a better understanding of how gene regulation is achieved will be required to corroborate the involvement of genomic changes and predict the phenotypic outcome in duplex kidneys.
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Satu Kuure, Helsinki Institute of Life Science / STEMM Research Program, Faculty of Medicine, University of Helsinki, Helsinki, Finland
Norman D Rosenblum, Department of Paediatrics, The Hospital for Sick Children, Toronto, Canada
Funding Statement
This work was supported by the La Ligue Contre le Cancer.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; peer review: 2 approved]
References
- 1. Queisser-Luft A, Stolz G, Wiesel A, et al. : Malformations in newborn: results based on 30,940 infants and fetuses from the Mainz congenital birth defect monitoring system (1990-1998). Arch Gynecol Obstet. 2002;266(3):163–7. 10.1007/s00404-001-0265-4 [DOI] [PubMed] [Google Scholar]
- 2. Capone VP, Morello W, Taroni F, et al. : Genetics of Congenital Anomalies of the Kidney and Urinary Tract: The Current State of Play. Int J Mol Sci. 2017;18(4):pii: E796. 10.3390/ijms18040796 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 3. Jain S, Chen F: Developmental pathology of congenital kidney and urinary tract anomalies. Clin Kidney J. 2018;12(3):382–99. 10.1093/ckj/sfy112 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 4. Schedl A: Renal abnormalities and their developmental origin. Nat Rev Genet. 2007;8(10):791–802. 10.1038/nrg2205 [DOI] [PubMed] [Google Scholar]
- 5. Nicolaou N, Renkema KY, Bongers EM, et al. : Genetic, environmental, and epigenetic factors involved in CAKUT. Nat Rev Nephrol. 2015;11(12):720–31. 10.1038/nrneph.2015.140 [DOI] [PubMed] [Google Scholar]
- 6. van der Ven AT, Vivante A, Hildebrandt F: Novel Insights into the Pathogenesis of Monogenic Congenital Anomalies of the Kidney and Urinary Tract. J Am Soc Nephrol. 2018;29(1):36–50. 10.1681/ASN.2017050561 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 7. Georgas KM, Armstrong J, Keast JR, et al. : An illustrated anatomical ontology of the developing mouse lower urogenital tract. Development. 2015;142(10):1893–908. 10.1242/dev.117903 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 8. Grote D, Souabni A, Busslinger M, et al. : Pax 2/8-regulated Gata 3 expression is necessary for morphogenesis and guidance of the nephric duct in the developing kidney. Development. 2006;133(1):53–61. 10.1242/dev.02184 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 9. Pedersen A, Skjong C, Shawlot W: Lim 1 is required for nephric duct extension and ureteric bud morphogenesis. Dev Biol. 2005;288(2):571–81. 10.1016/j.ydbio.2005.09.027 [DOI] [PubMed] [Google Scholar]
- 10. Attia L, Schneider J, Yelin R, et al. : Collective cell migration of the nephric duct requires FGF signaling. Dev Dyn. 2015;244(2):157–67. 10.1002/dvdy.24241 [DOI] [PubMed] [Google Scholar]
- 11. Walker KA, Sims-Lucas S, Di Giovanni VE, et al. : Deletion of fibroblast growth factor receptor 2 from the peri-wolffian duct stroma leads to ureteric induction abnormalities and vesicoureteral reflux. PLoS One. 2013;8(2):e56062. 10.1371/journal.pone.0056062 [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 12. Chia I, Grote D, Marcotte M, et al. : Nephric duct insertion is a crucial step in urinary tract maturation that is regulated by a Gata3-Raldh2-Ret molecular network in mice. Development. 2011;138(10):2089–97. 10.1242/dev.056838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoshi M, Reginensi A, Joens MS, et al. : Reciprocal Spatiotemporally Controlled Apoptosis Regulates Wolffian Duct Cloaca Fusion. J Am Soc Nephrol. 2018;29(3):775–783. 10.1681/ASN.2017040380 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 14. Sainio K, Hellstedt P, Kreidberg JA, et al. : Differential regulation of two sets of mesonephric tubules by WT-1. Development. 1997;124(7):1293–9. [DOI] [PubMed] [Google Scholar]
- 15. Mugford JW, Sipilä P, Kobayashi A, et al. : Hoxd11 specifies a program of metanephric kidney development within the intermediate mesoderm of the mouse embryo. Dev Biol. 2008;319(2):396–405. 10.1016/j.ydbio.2008.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Taguchi A, Kaku Y, Ohmori T, et al. : Redefining the in vivo origin of metanephric nephron progenitors enables generation of complex kidney structures from pluripotent stem cells. Cell Stem Cell. 2014;14(1):53–67. 10.1016/j.stem.2013.11.010 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 17. Lefevre JG, Short KM, Lamberton TO, et al. : Branching morphogenesis in the developing kidney is governed by rules that pattern the ureteric tree. Development. 2017;144(23):4377–85. 10.1242/dev.153874 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 18. Short KM, Combes AN, Lefevre J, et al. : Global quantification of tissue dynamics in the developing mouse kidney. Dev Cell. 2014;29(2):188–202. 10.1016/j.devcel.2014.02.017 [DOI] [PubMed] [Google Scholar]
- 19. McMahon AP: Development of the Mammalian Kidney. Curr Top Dev Biol. 2016;117:31–64. 10.1016/bs.ctdb.2015.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. O'Brien LL: Nephron progenitor cell commitment: Striking the right balance. Semin Cell Dev Biol. 2019;91:94–103. 10.1016/j.semcdb.2018.07.017 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 21. Kurtzeborn K, Cebrian C, Kuure S: Regulation of Renal Differentiation by Trophic Factors. Front Physiol. 2018;9:1588. 10.3389/fphys.2018.01588 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 22. Oxburgh L: Kidney Nephron Determination. Annu Rev Cell Dev Biol. 2018;34:427–50. 10.1146/annurev-cellbio-100616-060647 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 23. Huang YC, Chen F, Li X: Clarification of mammalian cloacal morphogenesis using high-resolution episcopic microscopy. Dev Biol. 2016;409(1):106–13. 10.1016/j.ydbio.2015.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Matsumaru D, Murashima A, Fukushima J, et al. : Systematic stereoscopic analyses for cloacal development: The origin of anorectal malformations. Sci Rep. 2015;5:13943. 10.1038/srep13943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kruepunga N, Hikspoors JPJM, Mekonen HK, et al. : The development of the cloaca in the human embryo. J Anat. 2018;233(6):724–39. 10.1111/joa.12882 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 26. Liaw A, Cunha GR, Shen J, et al. : Development of the human bladder and ureterovesical junction. Differentiation. 2018;103:66–73. 10.1016/j.diff.2018.08.004 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 27. Glassberg KI, Braren V, Duckett JW, et al. : Suggested Terminology for Duplex Systems, Ectopic Ureters and Ureteroceles. J Urol. 1984;132(6):1153–4. 10.1016/s0022-5347(17)50072-5 [DOI] [PubMed] [Google Scholar]
- 28. Zissin R, Apter S, Yaffe D, et al. : Renal duplication with associated complications in adults: CT findings in 26 cases. Clin Radiol. 2001;56(1):58–63. 10.1053/crad.2000.0639 [DOI] [PubMed] [Google Scholar]
- 29. Weigert C: Ueber einige Bildungsfehler der Ureteren. Virchows Arch. 1877;70(4):490–501. 10.1007/BF01935232 [DOI] [Google Scholar]
- 30. Britt DB, Borden TA, Woodhead DM: Inverted Y Ureteral Duplication with a Blind-Ending Branch. J Urol. 1972;108(3):387–8. 10.1016/s0022-5347(17)60749-3 [DOI] [PubMed] [Google Scholar]
- 31. Akbulut F, Savun M, Ucpinar B, et al. : Duplicated Renal System with H Shaped Ureter: An Extraordinary Anomaly. Case Rep Urol. 2016;2016:4062515. 10.1155/2016/4062515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Begg RC: Sextuplicitas Renum: A Case of Six Functioning Kidneys and Ureters in an Adult Female. J Urol. 1953;70(5):686–93. 10.1016/s0022-5347(17)67969-2 [DOI] [PubMed] [Google Scholar]
- 33. Senel U, Tanriverdi HI, Ozmen Z, et al. : Ectopic Ureter Accompanied by Duplicated Ureter: Three Cases. J Clin Diagn Res. 2015;9(9):PD10–2. 10.7860/JCDR/2015/13933.6446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lopes RI, Lopes RN, Filho CMB: Ureteral quadruplication with contralateral triplicate ureter. J Urol. 2001;166(3):979–80. 10.1016/S0022-5347(05)65878-8 [DOI] [PubMed] [Google Scholar]
- 35. Kudela G, Koszutski T, Mikosinski M, et al. : Ureteral triplication--report of four cases. Eur J Pediatr Surg. 2006;16(4):279–81. 10.1055/s-2006-924338 [DOI] [PubMed] [Google Scholar]
- 36. Bolkier M, Moskovitz B, Ginesin Y, et al. : Incomplete quadruplication of urinary tract with contralateral agenesis of the kidney. Eur Urol. 1991;19(3):267–8. 10.1159/000473636 [DOI] [PubMed] [Google Scholar]
- 37. Jurkiewicz B, Ząbkowski T, Shevchuk D: Ureteral quintuplication with renal atrophy in an infant after the 1986 Chernobyl nuclear disaster. Urology. 2014;83(1):211–3. 10.1016/j.urology.2013.07.031 [DOI] [PubMed] [Google Scholar]
- 38. Privett JTJ, Jeans WD, Roylance J: The incidence and importance of renal duplication. Clin Radiol. 1976;27(4):521–30. 10.1016/s0009-9260(76)80121-3 [DOI] [PubMed] [Google Scholar]
- 39. Batourina E, Choi C, Paragas N, et al. : Distal ureter morphogenesis depends on epithelial cell remodeling mediated by vitamin A and Ret. Nat Genet. 2002;32(1):109–15. 10.1038/ng952 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 40. Uetani N, Bertozzi K, Chagnon MJ, et al. : Maturation of ureter-bladder connection in mice is controlled by LAR family receptor protein tyrosine phosphatases. J Clin Invest. 2009;119(4):924–35. 10.1172/JCI37196 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 41. Batourina E, Tsai S, Lambert S, et al. : Apoptosis induced by vitamin A signaling is crucial for connecting the ureters to the bladder. Nat Genet. 2005;37(10):1082–9. 10.1038/ng1645 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 42. Mackie GG, Stephens FD: Duplex kidneys: a correlation of renal dysplasia with position of the ureteral orifice. J Urol. 1975;114(2):274–80. 10.1016/s0022-5347(17)67007-1 [DOI] [PubMed] [Google Scholar]
- 43. Doery AJ, Ang E, Ditchfield MR: Duplex kidney: not just a drooping lily. J Med Imaging Radiat Oncol. 2015;59(2):149–53. 10.1111/1754-9485.12285 [DOI] [PubMed] [Google Scholar]
- 44. Didier RA, Chow JS, Kwatra NS, et al. : The duplicated collecting system of the urinary tract: embryology, imaging appearances and clinical considerations. Pediatr Radiol. 2017;47(11):1526–38. 10.1007/s00247-017-3904-z [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 45. Davis TK, Hoshi M, Jain S: To bud or not to bud: the RET perspective in CAKUT. Pediatr Nephrol. 2014;29(4):597–608. 10.1007/s00467-013-2606-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schuchardt A, D'Agati V, Larsson-Blomberg L, et al. : Defects in the kidney and enteric nervous system of mice lacking the tyrosine kinase receptor Ret. Nature. 1994;367(6461):380–3. 10.1038/367380a0 [DOI] [PubMed] [Google Scholar]
- 47. Sánchez MP, Silos-Santiago I, Frisén J, et al. : Renal agenesis and the absence of enteric neurons in mice lacking GDNF. Nature. 1996;382(6586):70–3. 10.1038/382070a0 [DOI] [PubMed] [Google Scholar]
- 48. Pichel JG, Shen L, Sheng HZ, et al. : Defects in enteric innervation and kidney development in mice lacking GDNF. Nature. 1996;382(6586):73–6. 10.1038/382073a0 [DOI] [PubMed] [Google Scholar]
- 49. Moore MW, Klein RD, Fariñas I, et al. : Renal and neuronal abnormalities in mice lacking GDNF. Nature. 1996;382(6586):76–9. 10.1038/382076a0 [DOI] [PubMed] [Google Scholar]
- 50. Cacalano G, Fariñas I, Wang LC, et al. : GFRalpha1 is an essential receptor component for GDNF in the developing nervous system and kidney. Neuron. 1998;21(1):53–62. 10.1016/s0896-6273(00)80514-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Willecke R, Heuberger J, Grossmann K, et al. : The tyrosine phosphatase Shp2 acts downstream of GDNF/Ret in branching morphogenesis of the developing mouse kidney. Dev Biol. 2011;360(2):310–7. 10.1016/j.ydbio.2011.09.029 [DOI] [PubMed] [Google Scholar]
- 52. Perrinjaquet M, Vilar M, Ibáñez CF: Protein-tyrosine phosphatase SHP2 contributes to GDNF neurotrophic activity through direct binding to phospho-Tyr 687 in the RET receptor tyrosine kinase. J Biol Chem. 2010;285(41):31867–75. 10.1074/jbc.M110.144923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Takahashi M: The GDNF/RET signaling pathway and human diseases. Cytokine Growth Factor Rev. 2001;12(4):361–73. 10.1016/s1359-6101(01)00012-0 [DOI] [PubMed] [Google Scholar]
- 54. Lu BC, Cebrian C, Chi X, et al. : Etv4 and Etv5 are required downstream of GDNF and Ret for kidney branching morphogenesis. Nat Genet. 2009;41(12):1295–302. 10.1038/ng.476 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 55. Ihermann-Hella A, Lume M, Miinalainen IJ, et al. : Mitogen-activated protein kinase (MAPK) pathway regulates branching by remodeling epithelial cell adhesion. PLoS Genet. 2014;10(3):e1004193. 10.1371/journal.pgen.1004193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chi X, Michos O, Shakya R, et al. : Ret-dependent cell rearrangements in the Wolffian duct epithelium initiate ureteric bud morphogenesis. Dev Cell. 2009;17(2):199–209. 10.1016/j.devcel.2009.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 57. Torres M, Gómez-Pardo E, Dressler GR, et al. : Pax-2 controls multiple steps of urogenital development. Development. 1995;121(12):4057–65. [DOI] [PubMed] [Google Scholar]
- 58. Kiefer SM, Robbins L, Stumpff KM, et al. : Sall1-dependent signals affect Wnt signaling and ureter tip fate to initiate kidney development. Development. 2010;137(18):3099–106. 10.1242/dev.037812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Xu PX, Adams J, Peters H, et al. : Eya1-deficient mice lack ears and kidneys and show abnormal apoptosis of organ primordia. Nat Genet. 1999;23(1):113–7. 10.1038/12722 [DOI] [PubMed] [Google Scholar]
- 60. Hwang DY, Dworschak GC, Kohl S, et al. : Mutations in 12 known dominant disease-causing genes clarify many congenital anomalies of the kidney and urinary tract. Kidney Int. 2014;85(6):1429–33. 10.1038/ki.2013.508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Li H, Jakobson M, Ola R, et al. : Development of the urogenital system is regulated via the 3'UTR of GDNF. Sci Rep. 2019;9(1):5302. 10.1038/s41598-019-40457-1 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 62. Blockus H, Chédotal A: Slit-Robo signaling. Development. 2016;143(17):3037–44. 10.1242/dev.132829 [DOI] [PubMed] [Google Scholar]
- 63. Wainwright EN, Wilhelm D, Combes AN, et al. : ROBO2 restricts the nephrogenic field and regulates Wolffian duct-nephrogenic cord separation. Dev Biol. 2015;404(2):88–102. 10.1016/j.ydbio.2015.05.023 [DOI] [PubMed] [Google Scholar]
- 64. Grieshammer U, Le Ma, Plump AS, et al. : SLIT2-mediated ROBO2 signaling restricts kidney induction to a single site. Dev Cell. 2004;6(5):709–17. 10.1016/s1534-5807(04)00108-x [DOI] [PubMed] [Google Scholar]
- 65. Kume T, Deng K, Hogan BL: Murine forkhead/winged helix genes Foxc1 (Mf1) and Foxc2 (Mfh1) are required for the early organogenesis of the kidney and urinary tract. Development. 2000;127(7):1387–95. [DOI] [PubMed] [Google Scholar]
- 66. Neirijnck Y, Reginensi A, Renkema KY, et al. : Sox11 gene disruption causes congenital anomalies of the kidney and urinary tract (CAKUT). Kidney Int. 2018;93(5):1142–53. 10.1016/j.kint.2017.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lu W, van Eerde AM, Fan X, et al. : Disruption of ROBO2 is associated with urinary tract anomalies and confers risk of vesicoureteral reflux. Am J Hum Genet. 2007;80(4):616–32. 10.1086/512735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hwang DY, Kohl S, Fan X, et al. : Mutations of the SLIT2-ROBO2 pathway genes SLIT2 and SRGAP1 confer risk for congenital anomalies of the kidney and urinary tract. Hum Genet. 2015;134(8):905–16. 10.1007/s00439-015-1570-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Cheng Q, Wu J, Zhang Y, et al. : SOX4 promotes melanoma cell migration and invasion though the activation of the NF-κB signaling pathway. Int J Mol Med. 2017;40(2):447–53. 10.3892/ijmm.2017.3030 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 70. Grote D, Boualia SK, Souabni A, et al. : Gata3 acts downstream of beta-catenin signaling to prevent ectopic metanephric kidney induction. PLoS Genet. 2008;4(12):e1000316. 10.1371/journal.pgen.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bridgewater D, Cox B, Cain J, et al. : Canonical WNT/beta-catenin signaling is required for ureteric branching. Dev Biol. 2008;317(1):83–94. 10.1016/j.ydbio.2008.02.010 [DOI] [PubMed] [Google Scholar]
- 72. Miyamoto N, Yoshida M, Kuratani S, et al. : Defects of urogenital development in mice lacking Emx2. Development. 1997;124(9):1653–64. [DOI] [PubMed] [Google Scholar]
- 73. Reginensi A, Clarkson M, Neirijnck Y, et al. : SOX9 controls epithelial branching by activating RET effector genes during kidney development. Hum Mol Genet. 2011;20(6):1143–53. 10.1093/hmg/ddq558 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 74. Marose TD, Merkel CE, McMahon AP, et al. : Beta-catenin is necessary to keep cells of ureteric bud/Wolffian duct epithelium in a precursor state. Dev Biol. 2008;314(1):112–26. 10.1016/j.ydbio.2007.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Wilkinson LJ, Neal CS, Singh RR, et al. : Renal developmental defects resulting from in utero hypoxia are associated with suppression of ureteric β-catenin signaling. Kidney Int. 2015;87(5):975–83. 10.1038/ki.2014.394 [DOI] [PubMed] [Google Scholar]
- 76. Gimelli S, Caridi G, Beri S, et al. : Mutations in SOX17 are associated with congenital anomalies of the kidney and the urinary tract. Hum Mutat. 2010;31(12):1352–9. 10.1002/humu.21378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kobayashi A, Kwan KM, Carroll TJ, et al. : Distinct and sequential tissue-specific activities of the LIM-class homeobox gene Lim1 for tubular morphogenesis during kidney development. Development. 2005;132(12):2809–23. 10.1242/dev.01858 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 78. Miyazaki Y, Oshima K, Fogo A, et al. : Bone morphogenetic protein 4 regulates the budding site and elongation of the mouse ureter. J Clin Invest. 2000;105(7):863–73. 10.1172/JCI8256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Weaver M, Dunn NR, Hogan BL: Bmp4 and Fgf10 play opposing roles during lung bud morphogenesis. Development. 2000;127(12):2695–704. [DOI] [PubMed] [Google Scholar]
- 80. Motamedi FJ, Badro DA, Clarkson M, et al. : WT1 controls antagonistic FGF and BMP-pSMAD pathways in early renal progenitors. Nat Commun. 2014;5:4444. 10.1038/ncomms5444 [DOI] [PubMed] [Google Scholar]
- 81. Michos O, Gonçalves A, Lopez-Rios J, et al. : Reduction of BMP4 activity by gremlin 1 enables ureteric bud outgrowth and GDNF/WNT11 feedback signalling during kidney branching morphogenesis. Development. 2007;134(13):2397–405. 10.1242/dev.02861 [DOI] [PubMed] [Google Scholar]
- 82. Weber S, Taylor JC, Winyard P, et al. : SIX2 and BMP4 Mutations Associate With Anomalous Kidney Development. J Am Soc Nephrol. 2008;19(5):891–903. 10.1681/ASN.2006111282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. van Eerde AM, Duran K, van Riel E, et al. : Genes in the Ureteric Budding Pathway: Association Study on Vesico-Ureteral Reflux Patients. PLoS One. 2012;7(4):e31327. 10.1371/journal.pone.0031327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Desai PB, San Agustin JT, Stuck MW, et al. : Ift25 is not a cystic kidney disease gene but is required for early steps of kidney development. Mech Dev. 2018;151:10–7. 10.1016/j.mod.2018.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 85. Blake J, Di Hu, Cain JE, et al. : Urogenital development in Pallister-Hall syndrome is disrupted in a cell-lineage-specific manner by constitutive expression of GLI3 repressor. Hum Mol Genet. 2016;25(3):437–47. 10.1093/hmg/ddv483 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 86. San Agustin JT, Klena N, Granath K, et al. : Genetic link between renal birth defects and congenital heart disease. Nat Commun. 2016;7:11103. 10.1038/ncomms11103 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 87. Elliott KH, Brugmann SA: Sending mixed signals: Cilia-dependent signaling during development and disease. Dev Biol. 2019;447(1):28–41. 10.1016/j.ydbio.2018.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Weber S, Landwehr C, Renkert M, et al. : Mapping candidate regions and genes for congenital anomalies of the kidneys and urinary tract (CAKUT) by array-based comparative genomic hybridization. Nephrol Dial Transplant. 2011;26(1):136–43. 10.1093/ndt/gfq400 [DOI] [PubMed] [Google Scholar]
- 89. Basson MA, Akbulut S, Watson-Johnson J, et al. : Sprouty1 Is a Critical Regulator of GDNF/RET-Mediated Kidney Induction. Dev Cell. 2005;8(2):229–39. 10.1016/j.devcel.2004.12.004 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 90. Yosypiv IV, Boh MK, Spera MA, et al. : Downregulation of Spry-1, an inhibitor of GDNF/Ret, causes angiotensin II-induced ureteric bud branching. Kidney Int. 2008;74(10):1287–93. 10.1038/ki.2008.378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Nishimura H, Yerkes E, Hohenfellner K, et al. : Role of the Angiotensin Type 2 Receptor Gene in Congenital Anomalies of the Kidney and Urinary Tract, CAKUT, of Mice and Men. Mol Cell. 1999;3(1):1–10. 10.1016/s1097-2765(00)80169-0 [DOI] [PubMed] [Google Scholar]
- 92. Michos O, Cebrian C, Hyink D, et al. : Kidney development in the absence of Gdnf and Spry1 requires Fgf10. PLoS Genet. 2010;6(1):e1000809. 10.1371/journal.pgen.1000809 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 93. Morrisey EE, Hogan BLM: Preparing for the First Breath: Genetic and Cellular Mechanisms in Lung Development. Dev Cell. 2010;18(1):8–23. 10.1016/j.devcel.2009.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Saburi S, Hester I, Fischer E, et al. : Loss of Fat4 disrupts PCP signaling and oriented cell division and leads to cystic kidney disease. Nat Genet. 2008;40(8):1010–5. 10.1038/ng.179 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 95. Zhang H, Bagherie-Lachidan M, Badouel C, et al. : FAT4 Fine-Tunes Kidney Development by Regulating RET Signaling. Dev Cell. 2019;48(6):780–792.e4. 10.1016/j.devcel.2019.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 96. Komaki F, Miyazaki Y, Niimura F, et al. : Foxc1 gene null mutation causes ectopic budding and kidney hypoplasia but not dysplasia. Cells Tissues Organs. 2013;198(1):22–7. 10.1159/000351291 [DOI] [PubMed] [Google Scholar]
- 97. Saifudeen Z, Dipp S, Stefkova J, et al. : p53 regulates metanephric development. J Am Soc Nephrol. 2009;20(11):2328–37. 10.1681/ASN.2008121224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. El-Dahr S, Hilliard S, Aboudehen K, et al. : The MDM2-p53 pathway: Multiple roles in kidney development. Pediatr Nephrol. 2014;29(4):621–7. 10.1007/s00467-013-2629-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Yun K, Ajima R, Sharma N, et al. : Non-canonical Wnt5a/Ror2 signaling regulates kidney morphogenesis by controlling intermediate mesoderm extension. Hum Mol Genet. 2014;23(25):6807–14. 10.1093/hmg/ddu397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Debiec H, Kutsche M, Schachner M, et al. : Abnormal renal phenotype in L1 knockout mice: A novel cause of CAKUT. Nephrol Dial Transplant. 2002;17 Suppl 9:42–4. 10.1093/ndt/17.suppl_9.42 [DOI] [PubMed] [Google Scholar]
- 101. Brophy PD, Ostrom L, Lang KM, et al. : Regulation of ureteric bud outgrowth by Pax2-dependent activation of the glial derived neurotrophic factor gene. Development. 2001;128(23):4747–56. [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 102. Lu W, Quintero-Rivera F, Fan Y, et al. : NFIA haploinsufficiency is associated with a CNS malformation syndrome and urinary tract defects. PLoS Genet. 2007;3(5):e80. 10.1371/journal.pgen.0030080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Rutledge EA, Parvez RK, Short KM, et al. : Morphogenesis of the kidney and lung requires branch-tip directed activity of the Adamts18 metalloprotease. Dev Biol. 2019;454(2):156–69. 10.1016/j.ydbio.2019.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 104. Lindström NO, Guo J, Kim AD, et al. : Conserved and Divergent Features of Mesenchymal Progenitor Cell Types within the Cortical Nephrogenic Niche of the Human and Mouse Kidney. J Am Soc Nephrol. 2018;29(3):806–824. 10.1681/ASN.2017080890 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 105. Lindström NO, McMahon JA, Guo J, et al. : Conserved and Divergent Features of Human and Mouse Kidney Organogenesis. J Am Soc Nephrol. 2018;29(3):785–805. 10.1681/ASN.2017080887 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 106. Lindström NO, Tran T, Guo J, et al. : Conserved and Divergent Molecular and Anatomic Features of Human and Mouse Nephron Patterning. J Am Soc Nephrol. 2018;29(3):825–840. 10.1681/ASN.2017091036 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation