Abstract
Cognitive-behavioral therapy (CBT), consisting of exposure and response prevention (EX/RP), is both efficacious and preferred by patients with obsessive–compulsive disorder (OCD), yet few receive this treatment in practice. This study describes the implementation of an Internet-based CBT program (ICBT) developed in Sweden in individuals seeking OCD treatment in New York. After translating and adapting the Swedish ICBT for OCD, we conducted an open trial with 40 adults with OCD. Using the RE-AIM implementation science framework, we assessed the acceptability, feasibility, and effectiveness of ICBT. The Yale–Brown Obsessive Compulsive Scale (Y-BOCS) was the primary outcome measure. Of 40 enrolled, 28 participants completed the 10-week ICBT. In the intent-to-treat sample (N = 40), Y-BOCS scores decreased significantly over time (F = 28.12, df = 2, 49, p < . 001). Depressive severity (F = 5.87, df = 2, 48, p < . 001), and quality of life (F = 12.34, df = 2, 48, p < . 001) also improved. Sensitivity analyses among treatment completers (N = 28) confirmed the intent-to-treat results, with a large effect size for Y-BOCS change (Cohen’s d = 1.38). ICBT took less time to implement than face-to face EX/RP and participants were very to mostly satisfied with ICBT. On a par with results in Sweden, the adapted ICBT program reduced OCD and depressive symptoms and improved quality of life among individuals with moderate to severe OCD. Given its acceptability and feasibility, ICBT deserves further study as a way to increase access to CBT for OCD in the United States.
Keywords: Internet, cognitive-behavioral therapy, treatment, OCD
Obsessive–Compulsive Disorder (OCD) is a disabling mental illness, with a lifetime prevalence of about 2%, a relatively early onset, and a typically chronic course (Eisen et al., 2013; Ruscio, Stein, Chiu, & Kessler, 2010). Cognitive-behavioral therapy (CBT), consisting of exposure and response prevention (EX/RP), is one of the most efficacious OCD treatments (Simpson, Huppert, Petkova, Foa, & Liebowitz, 2006; Skapinakis et al., 2016). Individuals with OCD prefer EX/RP to serotonin reuptake inhibitor (SRI) medications alone (Patel, Galfavy, Kimeldorf, Dixon, & Simpson, 2016; Patel & Simpson, 2010), yet few receive this treatment in clinical practice (Eisen et al., 1999; Marques et al., 2010; Patel et al., 2014). Uncertainty about where to seek treatment, lack of trained therapists, shame, stigma, and costs associated with seeking mental health care are documented barriers to care (Blanco, Olfson, Stein, Simpson, & Narrow, 2006; Marques et al., 2010).
Efforts to improve access to CBT for OCD include self-help (Bachofen et al., 1999; Clark, Kirkby, Daniels, & Marks, 1998; Greist et al., 1998, 2002; Kenwright, Marks, Graham, Franses, & Mataix-Cols, 2005; Marks et al., 1998; Mataix-Cols & Marks, 2006; Pearcy, Anderson, Egan, & Rees, 2016; Tolin et al., 2007) with some of the most promising results demonstrated for Internet-based treatment delivery formats used largely outside of the United States (Andersson et al., 2011, 2012, 2015; Moritz, Wittlekind, Hauschildt, & Timpano, 2011; Seol, Kwon, Kim, Kim, & Shin, 2016; Wootton et al., 2011). Compared to face-to-face EX/RP treatment, Internet-based treatments provide convenient access to treatment at any time, can be self-paced, and the treatment content can be customized to the individual’s experience in some programs. Internet-based treatments that include therapist support have seen superior results (Andersson et al., 2012; Moritz et al., 2011; Seol et al., 2016) compared with those without therapist support. Among these, an Internet-based CBT (ICBT) for OCD, developed at the Karolinska Institutet in Sweden (Andersson et al., 2011, 2012, 2015), has been shown to be highly effective. In this ICBT program, individuals use an Internet-based treatment to learn about their illness and practice EX/RP under the confidential e-mail guidance of a therapist. When compared with an active control condition in a randomized controlled trial in Sweden, ICBT led to reduction in OCD severity with large effect sizes on the Yale–Brown Obsessive Compulsive Scale (Y-BOCS; Cohen’s d = 1.12; Goodman et al., 1989)—also, a significantly higher percentage of people receiving ICBT responded to treatment (60% vs. 6%, respectively). This response rate is similar to that seen in standard face-to-face CBT protocols, but ICBT requires only about one fourth the therapist time (Andersson et al., 2012). Moreover, ICBT enables individuals who face barriers to care to access CBT for the first time (Andersson et al., 2011, 2012).
While ICBT is a clear advance for self-help programs for OCD, there are no data available on the acceptability, feasibility, and effectiveness of this ICBT program in the United States. Research has shown that individuals with OCD in the United States often do not receive evidence-based care, with lower rates of treatment with EX/RP (range = 7.5–18%) than SRI medications (range = 39–77%), even though EX/RP is often a preferred treatment (Eisen et al., 1999; Marques et al., 2010; Patel et al., 2014, 2016). To begin exploring the utility of an ICBT program for OCD as a method to increase access to EX/RP for OCD in the United States, we collaborated with Karolinska Institutet in Sweden to adapt their ICBT program and evaluate its effect in a diverse sample of OCD participants seeking treatment in New York. We used the RE-AIM implementation research framework to evaluate the transfer of this e-health program from research to the real world (Glasgow, McKay, Piette, & Reynolds, 2001). We first adapted the ICBT program by translating the Swedish language-based ICBT program to English, culturally adapting the program content prior to implementation (e.g., case vignettes, language used to explain therapeutic concepts), and vetting it using local experts in EX/RP and four test OCD patients. We then tested this adapted ICBT program in 40 adults with OCD. With these adaptations, we hypothesized that ICBT would be an acceptable and feasible approach for individuals with OCD and would lead to improvements in OCD symptoms, depression, and quality of life, comparable to results with ICBT in Sweden.
Methods
Setting and Recruitment
The study was conducted at the Center for Obsessive-Compulsive and Related Disorders, an outpatient research clinic in New York City, New York, known for its expertise in the diagnosis and multimodal treatment of OCD. Participants were recruited from March 2014 to March 2016 via a study-specific website (http://columbiaocd.wixsite.com/icbt) on the clinic’s website, clinician referrals, and study-specific advertisements posted in online forums and the community. The Institutional Review Board approved the research protocol and all participants provided written informed consent.
Participants
Eligible participants were adults (ages 18–75 years) with a principal diagnosis of OCD according to DSM-5 criteria (American Psychiatric Association, 2013). Participants on psychotropic medications were eligible if they had been on a stable dose for at least 2 months and agreed to maintain a constant dosage during the trial. Participants with comorbid depression or anxiety disorders were eligible only if OCD was the most severe and impairing condition. Participants were also required to have regular access to a computer in order to access the Internet.
Individuals were excluded if they had (a) a diagnosis of bipolar or psychotic disorder; (b) current substance abuse or dependence; (c) clinically significant suicidal ideation or lifetime history of suicide attempt or hospitalization; (d) hoarding as the primary OCD symptom; (e) severe to extreme OCD (as measured by the Y-BOCS > 30; Goodman et al., 1989); or (f) a current serious physical illness that could interfere with ICBT, consistent with previous trials of ICBT in Sweden. After completing an initial eligibility telephone screen, participants were invited for an in-person evaluation in the clinic. Doctoral-level clinicians administered the Structured Clinical Interview for DSM-IV (First, Williams, Karg, & Spitzer, 2015) to verify OCD diagnostic criteria and determine eligibility.
Procedures
After providing written informed consent, participants were oriented to the ICBT platform, instructed that they had 12 weeks to complete the ICBT treatment, and assigned to an individual therapist to monitor their progress and provide support via e-mail and telephone. Independent evaluators (IEs) assessed participants at baseline, posttreatment, and at 4 months after the treatment.
ICBT Treatment
The ICBT platform used in the present study was adapted from the version found to be effective in Sweden (Andersson et al., 2011, 2012). ICBT incorporates the established CBT techniques of psychoeducation, self-monitoring, cognitive restructuring, EX/RP, and relapse prevention. The treatment information is provided in text and divided into 10 modules. Worksheets accompany modules to reinforce concepts, to monitor EX/RP exercises, and to gather patient information related to symptoms. Modules 1–4 involve psychoeducation, cognitive restructuring, and individual EX/RP hierarchy formation. Modules 5–10 consist of daily in vivo EX/RP exercises and monitoring of subjective units of distress (SUDS) levels. The treatment platform included tailored examples of obsessions and compulsions for particular OCD symptom subtypes (washing, checking, symmetry, and forbidden thoughts).
A therapist was assigned to each participant for the duration of the treatment. Therapists did not have face-to-face contact with participants during treatment and instead provided support via e-mail messages within the platform and regularly scheduled weekly phone calls (each lasting up to 30 minutes) during the EX/RP phase of treatment and as needed during the first four modules of the treatment. Therapists gave feedback on homework assignments, granted access to modules based on clinical judgment, monitored progress, and answered questions in a timely fashion (i.e., within 24 hours). Therapists were some junior clinicians with minimal CBT/EX/RP experience (treating on average 3 cases, range = 2–4), one senior clinician with CBT experience but minimal EX/RP experience, and one expert EX/RP supervisor who provided group supervision and monitored therapist communication in the ICBT platform on a weekly basis.
Adaptations to ICBT
In collaboration with the developers of ICBT at the Karolinska Institutet in Sweden (E.A. and C.R.), we adapted the ICBT program to the U.S. context. First, we translated the ICBT program from Swedish into English using best practices: forward translation with consensus bilingual committee review (Bravo, Canino, Rubio-Stipec, &Woodbury- Fariña, 1991). Then we made the materials culturally appropriate. For example, in the case of a vignette to illustrate contamination fears, the example of Jörgen who has fears of contamination when he sees a dirty rag changed to John who has fears of contamination when he touches a doorknob. To provide participants with the option to listen to the text-based information in the treatment platform, we also added mp3 audio recordings to each module. To confirm that the program met standard practices for U.S. manuals of EX/RP, we asked two expert EX/RP therapists to review the program. Finally, once translated and vetted, we tested the program with four patients with OCD. This led us to add weekly phone calls (up to seven calls of up to 30 minutes) when the participants began the EX/RP phase (Modules 5–10) to provide additional support and discussion of exposures. We also developed an orientation guide for participants to learn how to navigate through the treatment platform including a guide to the most frequently asked questions. Finally, to standardize therapist delivery of ICBT we also developed a therapist manual, which provided guidelines for implementing ICBT. This included recommendations to enhance patient adherence to ICBT modules and worksheets, as well as guidelines for patient contacts, including charting and maintaining Health Insurance Portability and Accountability Act (HIPAA) compliance. We also developed a therapist orientation video, in which new therapists learned how to navigate the treatment platform and participant dashboard (e-mail system, homework completion, and weekly participant self-rating scales) to manage their ICBT participant caseload.
Implementation Framework
We used the RE-AIM implementation science framework to evaluate the acceptability, feasibility and effectiveness when transferring an e-health program from research to real world (Glasgow et al., 2001; see Table 1). To assess acceptability (RE-AIM: adoption), we used adherence to ICBT (i.e., the number of modules completed). We also asked participants at posttreatment to rate their satisfaction with the ICBT program using three questions from the Client Satisfaction Questionnaire (CSQ; Larsen, Attkisson, Hargreaves, & Nguyen, 1979), a commonly utilized measure of treatment satisfaction. We also included three open-ended questions that asked about their reason for seeking an Internet-based treatment, their ICBT experience, and their recommendations to improve ICBT.
Table 1.
Evaluating ICBT for OCD Using RE-AIM
| RE-AIM element | Definition | Metric |
|---|---|---|
| Reach | The number and percentage of those invited and eligible who participate and their representativeness | Percentage eligible/excluded (characteristics and reasons why)/participate (reasons for refusal) characteristics of participants versus nonparticipants |
| Effectiveness | The amount of change in outcomes and impact on quality of life | Yale-Brown Obsessive Compulsive Scale (Y-BOCS) severity, Hamilton Depression Rating Scale (HAM-D), Quality of Life Enjoyment and Satisfaction Questionnaire—Short Form (Q-LES-Q-SF) (postassessment) Obsessive Compulsive Inventory—Revised (OCI-R) and Quick Inventory of Depressive Symptoms—Self-Report (QIDS-SR) (postassessment) Short-term attrition (Weeks 0–10): percentage who initiate treatment and discontinue treatment (and reasons why) |
| Adoption (individual) | The number, percentage, and representativeness of participants invited to participate | Adherence: number of modules completed, Client Satisfaction Questionnaire (CSQ) |
| Implementation | The extent to which a program is delivered consistently, and the time and costs | Treatment administration and intensity (therapist level): average time spent per patient, number of messages, reminder telephone calls |
| Maintenance | The long-term effects on key outcomes and quality-of-life impact | Y-BOCS severity, HAM-D, Q-LES-Q-SF (4-month naturalistic follow-up) |
To assess feasibility (RE-AIM: reach, implementation), we collected data on sample participation and representativeness through a clinical trial tracking log (screening to study completion) used by the study coordinator as well as a demographic form. Using metrics recorded in the treatment platform, we also assessed therapist burden by measuring the number of phone calls/e-mails, and the time spent making phone calls, reviewing platform materials, and writing e-mails.
To assess effectiveness (RE-AIM: effectiveness, maintenance) we used validated clinical scales completed in person or via telephone by IEs at baseline, posttreatment, and 4 months after treatment completion. The IEs assessed OCD severity using the Y-BOCS (Goodman et al., 1989) and depressive severity using the Hamilton Depression Rating Scale (HAM-D; Hamilton, 1960). The IEs were doctoral-level clinical psychologists with substantial experience assessing OCD as part of clinical trials conducted in our clinic. IEs were trained to administer the Y-BOCS and HAM-D with a standardized IE manual and participated in quarterly interrater reliability exercises in which they were asked to rate an IE recorded in our clinic. The Y-BOCS is the “gold standard” measure of OCD severity. It is a semi-structured interview consisting of 10 items used to assess the severity of obsessions and compulsions in the past week. Each item is rated on a 5-point Likert scale from 0 (no symptoms) to 4 (extreme.) Total scores range from 0 to 40 with higher scores indicating more severe symptoms. The Y-BOCS has good internal consistency, excellent interrater reliability, and good test–retest reliability (American Psychiatric Association, 2013). Cronbach’s alpha indicated that the Y-BOCS had excellent reliability in the present sample (α = .93). The HAM-D is a 17-item clinician-administered interview that is a commonly used measure of depression severity. Total scores range from 0 to 50 (with higher scores indicating more severe depression). The HAM-D has good psychometric properties, including good interrater reliability, internal consistency, and test–retest reliability. In the present sample the HAM-D evidenced good reliability (α = .83). At baseline, posttreatment, and 4-month follow-up, participants also completed the Quality of Life Enjoyment and Satisfaction Questionnaire—Short Form (Q-LES-QSF; Endicott, Nee, Harrison, & Blumenthal, 1993). The Q-LES-Q is a 15-item self-reported measure of quality of life frequently used in research. Higher scores indicate higher quality of life. This measure has good reliability, validity, and sensitivity to change. In the present sample the Q-LES-Q-SF had good reliability (α = .90).
To monitor weekly clinical progress from baseline to posttreatment (Week 10), participants also completed two self-report questionnaires in the ICBT treatment platform prior to accessing each module: the Obsessive Compulsive Inventory—Revised (OCI-R; Foa et al., 2002) and the Quick Inventory of Depressive Symptoms—Self-Report (QIDS-SR; Rush et al., 2003). The OCI-R is a commonly utilized measure of self-reported OCD symptom severity. The measure consists of 18 items measuring distress associated with obsessions and compulsions, with higher scores indicating more severe symptoms. In the present sample, the OCI-R had good reliability (α = .88). The QIDS-SR is a 16-item measure of depressive symptom severity. In the present sample, the QIDS-SR had good reliability (α = .85).
Statistical Analyses
SPSS version 24.0 and the statistical language R (R version 3.1.2 [2014-10-31] Copyright 2014 The R Foundation for Statistical Computing) were used for the statistical analysis.
Descriptive statistics were calculated to describe sample characteristics, scores on the CSQ, patient adherence, and therapist time. Open-ended questions about the ICBT program were abstracted using an inductive process suggested by Hill, Thompson, and Williams (1997). Two coders (S. R.P. and O.P.) each developed a preliminary list of themes by independently reviewing the open-ended question data. The coders met and iteratively modified themes comparing and discussing the data until they reached consensus on themes reported by at least 10% of the sample.
To assess clinical outcomes, primary analyses were carried out in the intent-to-treat (ITT; N = 40) sample. The primary outcome was the Y-BOCS; secondary outcomes included the HAM-D and QLES-Q-SF. For all three scales, repeated measures were analyzed as dependent variables using mixed-effect regression models (Pinheiro & Bates, 2000), with the three-level time variable as the categorical independent variable, subject-specific random intercepts, and an AR correlation structure for the subject-level residuals. For the weekly platform self-ratings, OCI-R and QIDS-SR weekly average item scores were analyzed using linear mixed-effect regression models with number of weeks as a (linear) predictor, subject-specific random intercepts, and an AR correlation structure for the subject-level residuals.
Sensitivity analyses were conducted on those who completed the 10-week treatment (N = 28), using paired samples t tests (baseline to posttreatment) for the Y-BOCS, HAM-D, and Q-LES-Q-SF, and two self-report measures—the OCI-R and the QIDS-SR. Cohen’s d was calculated to estimate effect sizes for the sensitivity analyses. Alpha was set at p < .05. Finally, for the Y-BOCS, we used a ≥ 25% reduction in OCD symptoms as the definition for treatment response (Simpson et al., 2006).
Results
Using the RE-AIM framework, results of the study are summarized below.
Reach
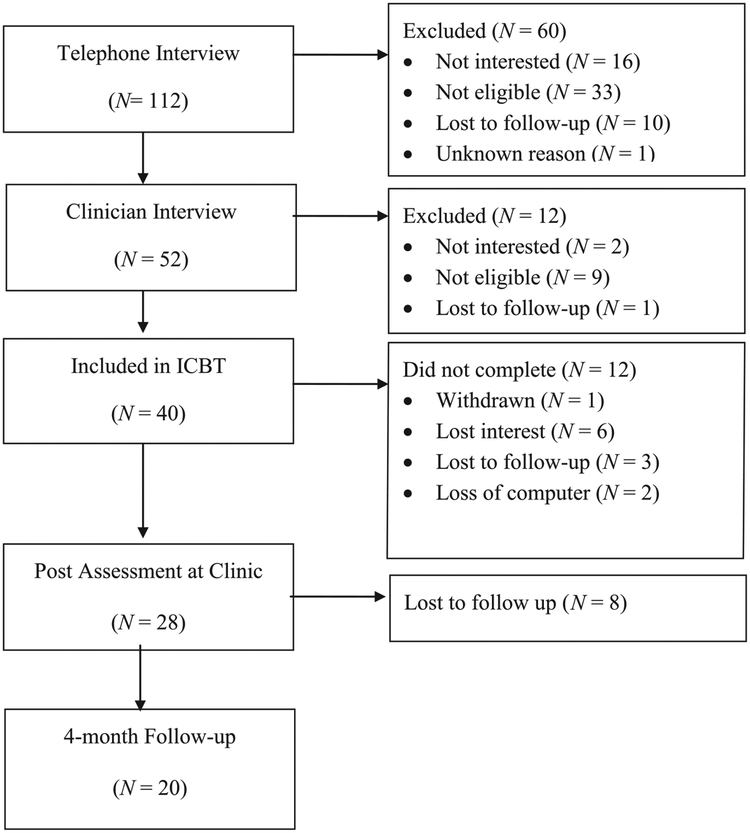
Figure 1 presents participant flow through the trial. Forty-two of 112 individuals screened were not eligible for the study; for most, this was because OCD was not their primary diagnosis, they had had recent medication changes, or they had a history of a suicide attempt or psychiatric hospitalization. Another 18 reported they were not interested; reasons included their being unwilling to travel to the clinic for an initial evaluation and preference for face-to-face contact with therapist (i.e., via Skype or videoconference).
FIGURE 1.
Flow of participants through the ICBT program.
Forty individuals signed consent and were enrolled in the study. Demographic and clinical data are shown in Table 2. Our sample was majority non-Hispanic White (82%) as well as Asian and Pacific Islander (7.5%), Black (7.5%), and Native American (2.5%) individuals with moderate to severe OCD (Y-BOCS = 25.8 ± 4.6) and mild depressive symptoms (HAM-D = 9.1 ± 6.3). Participants self-reported an average of 23 years since receiving a diagnosis of OCD (SD = 12.1), and approximately one third were on medications for OCD (37.5%) and one quarter or less had a history of CBT (27%) or EX/RP (15%).
Table 2.
Demographic and Clinical Characteristics
| Variable | N | % | |
|---|---|---|---|
| Gender | Women | 23 | 57.5 |
| Men | 17 | 42.5 | |
| Age | Mean age (SD) | 36.61 (11.1) | |
| Ethnicity | Hispanic | 1 | 2.5 |
| Non-Hispanic | 39 | 97.5 | |
| Race | White | 32 | 80 |
| Asian or Pacific Islander | 3 | 7.5 | |
| Black | 2 | 5.0 | |
| Other | 3 | 7.5 | |
| Employment | Employed | 25 | 62.5 |
| Homemaker | 1 | 2.5 | |
| Student | 5 | 12.5 | |
| Unemployed | 5 | 12.5 | |
| Retired | 1 | 2.5 | |
| Disabled | 1 | 2.5 | |
| Other | 2 | 5.0 | |
| Education | High school | 2 | 5.0 |
| Some college | 9 | 22.5 | |
| College graduate | 14 | 35.0 | |
| Graduate or professional | 15 | 37.5 | |
| Income | Less than $19,999 | 6 | 15.0 |
| $20,000–$59,999 | 18 | 67.5 | |
| $60,000–$70,000 | 13 | 32.5 | |
| $60,000–$99,000 | 13 | 32.5 | |
| More than $100,000 | 10 | 25.0 | |
| OCD duration | Mean length in years (SD) | 23.04 (12.1) | |
| Comorbid diagnoses | Mean (SD) | 1.92 (1.18) | |
| Current comorbid diagnoses | Social phobia | 5 | |
| Other anxiety | 3 | ||
| Other (e.g., major depressive disorder) | 4 | ||
| Current medication | 15 | 37.5 | |
| History of CBT | 12 | 26.7 | |
| History of prior EX/RP | 6 | 15 |
Note. SD = standard deviation; OCD = obsessive–compulsive disorder; CBT = cognitive-behavioral therapy; EX/RP = exposure and response prevention.
Of the 40 individuals who enrolled in the study, 28 (70%) completed (defined as completion of all 10 modules) ICBT and the posttreatment assessment. One participant was withdrawn due to worsening OCD and depressive symptoms; the others dropped out of their own accord (loss of interest in treatment, N = 6; loss of computer access, N = 2; unknown, N = 3). Individuals who dropped out of treatment and were lost to follow-up did not differ from those completing the treatment on baseline values of the Y-BOCS, HAM-D, or the Q-LES-QSF, all p > .05. Of the 28 who completed treatment, 20 completed the 4-month assessment.
Effectiveness
Effectiveness results in the ITT sample (N = 40) are presented in Table 3. In the ITT sample, OCD severity as measured by the Y-BOCS declined significantly over time, F = 28.12, df = 2, 49, p < .001; from baseline to posttreatment: mean decrease = −7.48, SE = 1.11, t(49) = −6.71, p < .001; and from baseline to 4-month follow-up: mean decrease = −9.50, SE = 1.49, t(49) = −6.36, p < .001. Depressive severity as measured by the HAM-D also declined significantly, F = 5.87, df = 2, 48, p < .001; from baseline to posttreatment: mean decrease = −2.45, SE = 1.06, t(48) = −2.31, p = .025; and from baseline to 4-month follow-up: mean decrease = −4.80, SE = 1.43, t(48) = −3.35, p = .001,. Quality of life as measured by the Q-LES-Q-SF significantly increased, F = 12.34, df = 2, 48, p < .001; from baseline to posttreatment: mean increase = 6.50, SE = 2.94, t(48) = 2.21, p = .032; and from baseline to 4-month follow-up: mean increase = 16.94, SE = 3.42, t(48) = 4.96, p < .001. OCI-R weekly scores declined significantly over the course of the study (itemwise mean decline estimate: b = −0.06/week, SE = 0.01, df = 315, t = − 6.78, p < .0001), as did QIDS-SR scores (itemwise mean b = − 0.02 points/week, SE = 0.01, df = 364, t = −4.78, p < .0001).
Table 3.
Effectiveness of ICBT: Observed Data
| Variable | Mean ± SD | Mean ± SD | Mean ± SD | F | df | p |
|---|---|---|---|---|---|---|
| Baselinea | Posttreatmentb | Follow-upc | ||||
| ITT Sample | ||||||
| Y-BOCS | 25.8 ± 4.6 | 18.6 ±7.9 | 16.3 ± 8.2d | 28.12 | 2, 49 | < .001 |
| HAM-D | 9.1 ±6.3 | 6.97 ± 6.3 | 4.2 ± 4.3 | 5.87 | 2, 48 | .005 |
| Q-LES-Q-SF | 55.1 ± 15.8 | 61.5 ± 19.9 | 73.3 ± 16.4 | 12.34 | 2, 48 | < .001 |
| OCI-Re | 30.8 ± 12.5 | 18.8 ± 13.2 | ||||
| QIDS-SRe | 12.0 ± 5.4 | 8.7 ±8.1 |
Note. ITT = intent to treat (YBOCS, HAM-D, and Q-LES-Q-SF using longitudinal mixed-effects models); Y-BOCS = Yale–Brown Obsessive Compulsive Scale; HAM-D = Hamilton Depression Rating Scale; Q-LES-Q-SF = Quality of Life Enjoyment and Satisfaction Questionnaire—Short Form; OCI-R = Obsessive Compulsive Inventory—Revised; QIDS-SR = Quick Inventory of Depressive Symptoms—Self-Report.
Number of subjects (N = 40).
Number of subjects (N = 30).
Number of subjects (N =.20).
Number of subjects (N = 21).
Number of subjects (N =.37).
There were no differences between treatment completers (N = 28) and those not available for follow up (N = 20) in posttreatment Y-BOCS severity (completers M = 18.3 vs. those not available for follow-up, M = 19.1, t = −0.24, df = 28, p = .81) or pre–post treatment Y-BOCS change (completers M = −7.5 vs. those not available for follow-up, M = −8, t = −0.20, df = 28, p = .84).
Sensitivity analyses on treatment completers (N = 28) examined baseline to posttreatment scores on both IE and self-report measures among individuals who completed the 10-week treatment. Paired samples t tests showed significant reductions in OCD severity, Y-BOCS baseline: M = 26.1, SD = 4.5 posttreatment: 18.2, SD = 7.9, t(27) = 6.44, p < .001; depressive severity, HAM-D baseline: M = 9.3, SD = 6.5 posttreatment: 6.2, SD = 5.8, t(27) = 3.85, p = .001; and improved quality of life, Q-LES-Q-SF baseline: M = 54.9, SD = 13.8 posttreatment: 63.4, SD =19.1, t(27) = −3.78, p = .001. Effect size was large (Y-BOCS Cohen’s d = 1.38) for reduction in OCD symptoms, and medium for change in depression (Cohen’s d = .74) and quality of life (Cohen’s d = .79). For OCD and depression self-report platform measures, the results corroborated the IE ratings, OCI-R baseline M = 32.6, SD = 12.6 posttreatment: 18.7, SD = 14.2, t(27) = 4.87, p < .001, Cohen’s d = .92 and QIDS-SR baseline M = 11.9, SD = 5.6 posttreatment: 7.8, SD = 8.2, t(27), p = .001, Cohen’s d = .75.
At posttreatment, 16 (40%) of the 40 who started and 16 (57%) of the 28 who completed met response criteria for OCD (≥ 25% Y-BOCS reduction; Simpson et al., 2006). In addition, 7 of these (ITT sample: 17.5%; treatment completer sample: 25%) attained mild or minimal OCD symptoms (Y-BOCS ≤ 12), a marker of posttreatment wellness (Farris, McLean, Van Meter, Simpson, & Foa, 2013).
Adoption (Individual)
Among the ITT sample, participants completed 8 modules on average including the weekly exercises (range = 1–10, SD = 3.0) of the 10-week treatment; 70% completed all 10 modules. None of the participants reported any changes in medication or initiation of concurrent psychological treatment during their participation in the 10-week treatment.
On the CSQ, a majority of the treatment completer sample (79%) reported they were mostly to very satisfied with ICBT. Out of the treatment completer sample, (78%) reported that they would come back to the ICBT program if they were to seek help again.
Review of the open-ended question data revealed that competing demands of work, a desire to avoid treatment with medication, shame/embarrassment, convenience and access to treatment, and therapist recommendation were top reasons why participants chose to participate in this ICBT program. Out of those who completed the program, most (73%) reported a positive experience with ICBT. Treatment completers’ top three recommendations made for improving ICBT included increasing communication with therapists (31%), enhancing resources or learning tools for EX/RP (e.g., more examples of individuals with OCD, simpler worksheets, adding videos [27%], and offering longer treatment duration [15%]).
Implementation
The ICBT platform logged the amount of time that therapists spent interacting with participant materials (e.g., reviewing homework and writing e-mails). In the ITT sample, therapists sent on average 24 e-mails (range = 4–75, SD = 13.5), which translated into on average 164 minutes (range = 11.5–815, SD = 209.1) over the 10-week treatment (i.e., 16 minutes per patient per week on e-mails). On average therapists conducted eight telephone calls per participant over the 10 weeks (range = 2–25, SD = 8.5); each telephone call lasted an average of 23 minutes per call (range = 8–33, SD = 6.6). In total, therapists spent on average 393 minutes per participant including platform correspondence and telephone calls.
We did not find a therapist effect on Y-BOCS values (p = .21) and there were no significant associations found between number of e-mails sent or phone calls and posttreatment Y-BOCS score and pre–post treatment Y-BOCS change (all p > .05).
Discussion
In this study, we adapted ICBT for an OCD program found to be effective in Sweden for a U. S. population and tested it with 40 adults with moderately severe OCD living in the New York metropolitan area. This adapted version of ICBT showed promise as an acceptable, feasible, and effective treatment for OCD.
In terms of acceptability, although some at screening were not interested in ICBT and others were not eligible, 70% of participants who enrolled in ICBT completed the entire 10-module program within the 12-week treatment window. Reasons for not completing included loss of interest in treatment, loss of computer access, and worsening OCD symptoms. Importantly, the dropout rate in the present trial (30%) appeared higher than that reported in Swedish trials (12.0–12.5%; Andersson et al., 2011, 2012), suggesting that ICBT may be less acceptable for some individuals in the United States. On the other hand, qualitative data from our study indicated that some of our participants (15 out of 40) preferred ICBT to face-to-face treatment because it was more convenient in their busy lives. Together, these data suggest that ICBT may not be acceptable to all, but may be an attractive option for many. Importantly, among those who completed treatment, a majority reported being satisfied with the treatment program (based on the CSQ). Notably, although our sample was primarily non-Hispanic White, our sample included a much higher proportion of non-White participants (20%) as compared to prior OCD treatment trials, where a recent review included on average only 8.5% non-White participants (range = 0–13%; Williams, Powers, Yun, & Foa, 2010). The possibility that ICBT may be a more acceptable option for minority participants who have been greatly underrepresented in OCD treatment trials deserves future study.
Our trial also suggests that ICBT is a feasible and resource-efficient treatment option. Specifically, ICBT used less therapist time than traditional face-to-face treatments. Thus, ICBT could enable therapists to expand their caseloads, allowing more patients access to their care. Moreover, ICBT can also increase access to care given that it may be conducted remotely. Importantly, lack of access to clinicians experienced in treating OCD is frequently cited as a barrier to receiving care (Marques et al., 2010), particularly in rural areas with few providers.
We also found it is feasible to deliver ICBT using a treatment team of therapists, most of whom had a range of experience with EX/RP and were provided a therapist manual and received weekly supervision by an EX/RP expert. This model may provide one way to maximize therapist resources and expertise in the treatment of OCD and provide an efficient way to ensure that patients receive EX/RP with high treatment integrity. In this respect, ICBT may be similar to face-to-face CBT for OCD, in which more junior clinicians (with little specific OCD experience) appear to perform as well as more experienced colleagues when using a treatment manual and expert supervision (Franklin, Abramowitz, Furr, Kalsy, & Riggs, 2003)
In terms of treatment effectiveness, we found that ICBT was associated with significant improvement in OCD symptoms, as well as depression severity and quality of life. Similar to trials conducted in Sweden (Andersson et al., 2012), ICBT was associated with large within-group effect sizes for reducing OCD symptoms, and medium effect sizes for improving depression and quality of life. Moreover, the effect size for reducing OCD symptoms was within the range reported in trials of face-to-face CBT for OCD (Skapinakis et al., 2016) and larger than most trials with computer-based treatments that did not provide therapist support (Bachofen et al., 1999; Greist et al., 1998, 2002; Kenwright et al., 2005; Moritz et al., 2011; Seol et al., 2016; Tolin et al., 2007; Wootton et al., 2011). Although we did not control for outside treatment during the follow-up period, we found preliminary evidence that the benefit of ICBT was maintained in this sample 4 months after the treatment was completed. In addition, more than half of those who completed the ICBT treatment experienced reliably significant change, and approximately one quarter of completers achieved posttreatment OCD severity scores previously used as a marker of wellness (low symptoms and restored functioning). These data suggest that for some individuals, a brief course of ICBT may prove to be a sufficiently intense intervention to achieve remission from OCD. For others, ICBT may lead to smaller improvements, but could be helpful as a preliminary step before a more intensive treatment (i.e., face-to-face). Thus, ICBT can be considered as a low-intensity option offered as a first-line intervention in a stepped-care model.
Our results should be understood within the context of study limitations. First, as this was a pilot study, there was no randomization to a control condition, which rendered it difficult to claim that any improvements were caused by the treatment alone. However, OCD is regarded as a stable and often chronic disease (Kessler et al., 2005; Murray & Lopez, 1996) and with a low response rate to placebo (Huppert et al., 2004)—thus, we believe it is unlikely the overall treatment results were due to time alone. Second, as did the ICBT pilot trial in Sweden, we excluded severe OCD (Y-BOCS > 30) and excluded serious mental illness and substance use disorders. In subsequent randomized trials of ICBT, the effects of ICBT have been tested without an upper limit on the Y-BOCS (Andersson et al., 2015)—however, the effects of ICBT in individuals with extreme OCD remains untested in the United States. Future work should test the effectiveness of ICBT in the broader OCD patient population to determine whether it works equally well for all OCD patients. If ICBT is most effective in those patients with relatively mild to moderate OCD who prefer ICBT as a treatment modality, then ICBT may be offered as a first step in a stepped-care system, in which more resource-intensive options are offered to more severely ill patients.
Conclusions
In summary, this study provides preliminary evidence that ICBT is effective and feasible to implement in the United States. ICBT provides a potentially cost-effective, flexible, and patient-centered treatment program for individuals with OCD to access and receive care in their own community. Yet substantial future research on this treatment modality is needed. Specifically, to ensure that the treatment benefits of ICBT are specific to this intervention a randomized trial could compare ICBT with another potential intervention (i.e., online anxiety management training). At the same time, effectiveness trials could be done to test the acceptability of ICBT in community practice. Finally, ICBT should be tested with a broader range of patients and in comparison to face-to-face CBT. This direct comparison might allow for analysis of treatment moderators and predictors, in order to determine who is likely to benefit from ICBT and who may instead require face-to-face treatment. In this way, future implementation could explore ways to integrate ICBT with other recommended treatment options (e.g., medications) in a stepped-care model.
Funding:
A New York State Office of Mental Health Policy Scholar Award (SRP), K24 MH091555 (HBS), and the New York State Office of Mental Hygiene supported this work.
Footnotes
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Contributor Information
Sapana R. Patel, New York State Psychiatric Institute, Research Foundation for Mental Hygiene, Columbia University, College of Physicians and Surgeons
Michael G. Wheaton, Barnard College
Hanga Galfavy, Columbia University, College of Physicians and Surgeons, Mailman School of Public Health.
Olivia Pascucci, New York State Psychiatric Institute, Research Foundation for Mental Hygiene.
Robert W. Myers, New York State Office of Mental Health
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed, text rev.). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Andersson E, Enander J, Andrén P, Hedman E, Ljótsson B, Hursti T, … Rück C (2012). Internet-based cognitive behaviour therapy for obsessive–compulsive disorder: A randomized controlled trial. Psychological Medicine, 42(10), 2193–2203. 10.1017/S0033291712000244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson E, Hedman E, Enander J, Radu Djurfeldt D, Ljótsson B, Cervenka S, … Rück C (2015). D-cycloserine vs placebo as adjunct to cognitive behavioral therapy for obsessive-compulsive disorder and interaction with antidepressants: A randomized clinical trial. JAMA Psychiatry, 72(7), 659–667. 10.1001/jamapsychiatry.2015.0546 [DOI] [PubMed] [Google Scholar]
- Andersson E, Ljótsson B, Hedman E, Kaldo V, Paxling B, Andersson G, … Rück C (2011). Internet-based cognitive behavior therapy for obsessive compulsive disorder: A pilot study. BMC Psychiatry, 11(1), 125 10.1186/1471-244X-11-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachofen M, Nakagawa A, Marks IM, Park JM, Greist JH, Baer L, … Dottl SL (1999). Home self-assessment and self-treatment of obsessive-compulsive disorder using a manual and a computer-conducted telephone interview: Replication of a UK-US study. Journal of Clinical Psychiatry, 60(8), 545–549. [DOI] [PubMed] [Google Scholar]
- Blanco C, Olfson M, Stein DJ, Simpson HB, & Narrow WH (2006). Treatment of obsessive-compulsive disorder by US psychiatrists. Journal of Clinical Psychiatry, 67(6), 946–951. [DOI] [PubMed] [Google Scholar]
- Bravo M, Canino GJ, Rubio-Stipec M, & Woodbury-Fariña M (1991). A cross-cultural adaptation of a psychiatric epidemiologic instrument: The diagnostic interview schedule’s adaptation in Puerto Rico. Culture, Medicine and Psychiatry, 15(1), 1–18. [DOI] [PubMed] [Google Scholar]
- Clark A, Kirkby KC, Daniels BA, & Marks IM (1998). A pilot study of computer-aided vicarious exposure for obsessive-compulsive disorder. Australian and New Zealand Journal of Psychiatry, 32(2), 268–275. 10.3109/00048679809062738 [DOI] [PubMed] [Google Scholar]
- Eisen JL, Goodman WK, Keller MB, Warshaw MG, DeMarco LM, Luce DD, & Rasmussen SA (1999). Patterns of remission and relapse in obsessive-compulsive disorder: A 2-year prospective study. Journal of Clinical Psychiatry, 60(5), 346–351. 10.4088/jcp.v60n0514 [DOI] [PubMed] [Google Scholar]
- Eisen JL, Sibrava NJ, Boisseau CL, Mancebo MC, Stout RL, Pinto A, & Rasmussen SA (2013). Five-year course of obsessive-compulsive disorder: Predictors of remission and relapse. Journal of Clinical Psychiatry, 74 (3), 233 10.4088/JCP.12m07657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, & Blumenthal R (1993). Quality of Life Enjoyment and Satisfaction Questionnaire: A new measure. Psychopharmacology Bulletin, 29(2), 321–326. [PubMed] [Google Scholar]
- Farris SG, McLean CP, Van Meter PE, Simpson HB, & Foa EB (2013). Treatment response, symptom remission, and wellness in obsessive-compulsive disorder. Journal of Clinical Psychiatry, 74(7), 685–690. 10.4088/JCP.12m07789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured Clinical Interview for DSM-5—Research Version. Arlington, VA: American Psychiatric Association. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, & Salkovskis PM (2002). The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment, 14(4), 485. [PubMed] [Google Scholar]
- Franklin ME, Abramowitz JS, Furr JM, Kalsy S, & Riggs DS (2003). A naturalistic examination of therapist experience and outcome of exposure and ritual prevention for OCD. Psychotherapy Research, 13(2), 153–167. 10.1080/713869637 [DOI] [Google Scholar]
- Glasgow RE, McKay HG, Piette JD, & Reynolds KD (2001). The RE-AIM framework for evaluating interventions: What can it tell us about approaches to chronic illness management? Patient Education and Counseling, 44(2), 119–127. 10.1016/S0738-3991(00)00186-5 [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, … Charney DS (1989). The Yale-Brown Obsessive Compulsive Scale: I. Development, use, and reliability. Archives of General Psychiatry, 46 (11), 1006–1011. 10.1001/archpsyc.1989.01810110048007 [DOI] [PubMed] [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ, … Clary CM (2002). Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. Journal of Clinical Psychiatry, 63(2), 138–145. [DOI] [PubMed] [Google Scholar]
- Greist JH, Marks IM, Baer L, Parkin JR, Manzo PA, Mantle JM, … Forman L (1998). Self-treatment for obsessive compulsive disorder using a manual and a computerized telephone interview: A US-UK study. MD Computing, 15(3), 149–157. [PubMed] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 23(1), 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill CE, Thompson BJ, & Williams EN (1997). A guide to conducting consensual qualitative research. The Counseling Psychologist, 25(4), 517–572. 10.1177/0011000097254001 [DOI] [Google Scholar]
- Huppert JD, Schultz LT, Foa EB, Barlow DH, Davidson JR, Gorman JM, … Woods SW (2004). Differential response to placebo among patients with social phobia, panic disorder, and obsessive-compulsive disorder. American Journal of Psychiatry, 161(8), 1485–1487. 10.1176/appi.ajp.161.8.1485 [DOI] [PubMed] [Google Scholar]
- Kenwright M, Marks I, Graham C, Franses A, & Mataix-Cols D (2005). Brief scheduled phone support from a clinician to enhance computer-aided self-help for obsessive-compulsive disorder: Randomized controlled trial. Journal of Clinical Psychology, 61(12), 1499–1508. 10.1002/jclp.20204 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, et al. (2005). Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry, 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, & Nguyen TD (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2(3), 197–207. 10.1016/0149-7189(79)90094-6 [DOI] [PubMed] [Google Scholar]
- Marks IM, Baer L, Greist JH, Park JM, Bachofen M, Nakagawa A, … Mantle JM (1998). Home self-assessment of obsessive-compulsive disorder. Use of a manual and a computer-conducted telephone interview: Two UK-US studies. British Journal of Psychiatry, 172(5), 406–412. [DOI] [PubMed] [Google Scholar]
- Marques L, LeBlanc NJ, Weingarden HM, Timpano KR, Jenike M, & Wilhelm S (2010). Barriers to treatment and service utilization in an internet sample of individuals with obsessive–compulsive symptoms. Depression and Anxiety, 27 (5), 470–475. 10.1002/da.20694 [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, & Marks I (2006). Self-help with minimal therapist contact for obsessive–compulsive disorder: A review. European Psychiatry, 21(2), 75–80. 10.1016/j.eurpsy.2005.07.003 [DOI] [PubMed] [Google Scholar]
- Moritz S, Wittekind CE, Hauschildt M, & Timpano KR (2011). Do it yourself? Self-help and online therapy for people with obsessive-compulsive disorder. Current Opinion in Psychiatry, 24(6), 541–548. 10.1097/YCO.0b013e32834abb7f [DOI] [PubMed] [Google Scholar]
- Murray CJL, & Lopez AD (1996). The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard School of Public Health, Harvard University Press. [Google Scholar]
- Patel SR, Galfavy H, Kimeldorf MB, Dixon LB, & Simpson HB (2016). Patient preferences and acceptability of evidence-based and novel treatments for obsessive-compulsive disorder. Psychiatric Services, 68(3), 250–257. 10.1176/appi.ps.201600092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Humensky JL, Olfson M, Simpson HB, Myers R, & Dixon LB (2014). Treatment of obsessive-compulsive disorder in a nationwide survey of office-based physician practice. Psychiatric Services, 65(5), 681–684. 10.1176/appi.ps.201300192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, & Simpson HB (2010). Patient preferences for OCD treatment. Journal of Clinical Psychiatry, 71(11), 1434 10.4088/JCP.09m05537blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearcy CP, Anderson RA, Egan SJ, & Rees CS (2016). A systematic review and meta-analysis of self-help therapeutic interventions for obsessive–compulsive disorder: Is therapeutic contact key to overall improvement? Journal of Behavior Therapy and Experimental Psychiatry, 51, 74–83. 10.1016/j.jbtep.2015.12.007 [DOI] [PubMed] [Google Scholar]
- Pinheiro JC, & Bates DM (2000). Linear mixed-effects models: Basic concepts and examples Mixed-effects models in S and S-PLUS (pp. 3–56). New York, NY: Springer. [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, & Kessler RC (2010). The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry, 15(1), 53–63. 10.1038/mp.2008.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, … Thase ME (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. 10.1016/S0006-3223(02)01866-8 [DOI] [PubMed] [Google Scholar]
- Seol S, Kwon J, Kim Y, Kim S, & Shin M (2016). Internet-based cognitive behavioral therapy for obsessive-compulsive disorder in Korea. Psychiatry Investigation, 13(4), 373 10.4306/pi.2016.13.4.373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Huppert JD, Petkova E, Foa EB, & Liebowitz MR (2006). Response versus remission in obsessive-compulsive disorder. Journal of Clinical Psychiatry, 67(2), 269–276. [DOI] [PubMed] [Google Scholar]
- Skapinakis P, Caldwell DM, Hollingworth W, Bryden P, Fineberg NA, Salkovskis P, … Lewis G (2016). Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 3(8), 730–739. 10.1016/S2215-0366(16)30069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Hannan S, Maltby N, Diefenbach GJ, Worhunsky P, & Brady RE (2007). A randomized controlled trial of self-directed versus therapist-directed cognitive-behavioral therapy for obsessive-compulsive disorder patients with prior medication trials. Behavior Therapy, 38(2), 179–191. 10.1016/j.beth.2006.07.001 [DOI] [PubMed] [Google Scholar]
- Williams M, Powers M, Yun YG, & Foa E (2010). Minority participation in randomized controlled trials for obsessive–compulsive disorder. Journal of Anxiety Disorders, 24(2), 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wootton BM, Titov N, Dear BF, Spence J, Andrews G, Johnston L, & Solley K (2011). An internet administered treatment program for obsessive–compulsive disorder: A feasibility study. Journal of Anxiety Disorders, 25(8), 1102–1107. 10.1371/journal.pone.0020548 [DOI] [PubMed] [Google Scholar]