Abstract
Background:
The effectiveness of the Patient Empowerment Program (PEP) has been demonstrated in people with diabetes mellitus (DM); however, the underlying reasons for its effectiveness remain unclear. To improve effectiveness, we need to study the psychological mechanism(s) of PEP to understand why it is effective. This study hypothesized that the Theory of Planned Behavior (TPB), modified specifically for people with DM, could describe the mechanism explaining PEP effects.
Methods:
A longitudinal design was used. Patients with type 2 DM (n = 365; 151 males; mean age = 62.9 ± 9.6 years) received two education sessions (i.e. seminars delivered by registered nurses to provide disease-specific knowledge), and some (n = 210) further enrolled afterwards in five empowerment sessions (i.e. small-group interactive workshops conducted by social workers to practice action planning, problem solving, and experience sharing). Validated questionnaires were used to measure risk perception, health literacy, attitude, subjective norm, perceived behavioral control and behavioral intention on diabetes self-care behaviors, and four diabetes self-care behaviors (diet control, exercise, blood glucose monitoring, and foot care) at baseline. Three months later (i.e. at the end of PEP), all participants completed the behavioral intention and diabetes self-care behaviors measures again. Attitude, subjective norm, perceived behavioral control, behavioral intention, and diabetes self-care behaviors were assessed to represent the TPB constructs. Risk perception and health literacy elements relevant to people with DM were assessed and added to modify the TPB.
Results:
The behavioral intention was associated with three diabetes self-care behaviors: exercise, blood glucose monitoring, and foot care. The behavioral intention was found to be a significant mediator in the following relationships: empowerment session participation and exercise (β = 0.045, p = 0.04), and empowerment session participation and foot care (β = 0.099, p < 0.001).
Conclusions:
The effects of enrollment of empowerment sessions in PEP on exercise and foot care were likely to be mediated through behavioral intention.
Keywords: primary care, self-management, theory of planned behavior, type 2 diabetes
Introduction
Diabetes mellitus (DM), a demanding and progressive disease usually resulting in serious short- and long-term consequences, is a burden to public health.1 In 2013, the number of people aged between 20 and 79 years living with DM worldwide was 382 million, the global number increased to 424.9 million in 2017.2,3 Moreover, the projected global number by 2045 is 592 million, about 10% of world population.3 Additionally, people with DM have nearly twice the mortality rate of their healthy counterparts.4 DM-related complications, such as cardiovascular diseases (CVD), are likely to jeopardize the quality of life of people with DM.5 Therefore, establishing diabetes self-care behaviors to help people with DM to manage their illness is deemed to be an appropriate method to improve their health.6
Four diabetes self-care behaviors have been identified as important management strategies to help people with DM maintain or improve their health: diet control, exercise, blood glucose monitoring through hemoglobin A1c (HbA1c), and foot care.1,7,8 The Patient Empowerment Program (PEP) was developed in 2010 by the Hong Kong Hospital Authority to improve the diabetes self-care behaviors of people with DM through improving their knowledge, skills, and sense of empowerment.9 The PEP was found to reduce general outpatient clinic utilization rates,10 decrease all-cause mortality and CVD rates,11 and improve quality of life.12 All these promising results may be due to changes in diabetes self-care behaviors in DM management.9
The PEP adopts the fundamental concept that ‘patient empowerment is a process where people gain greater control over decisions affecting their health’13; however, to the best of our knowledge, no studies have applied any theoretical model to explain such health-related behaviors by testing the relationships of various underlying psychological processes (i.e. the routes and paths of underlying factors in the mind of an individual that contribute to complex human behaviors) of the PEP. Therefore, a theoretical model is warranted to help healthcare providers understand the effectiveness of the PEP. Specifically, a theoretical model can help us understand why the PEP works, and, thus, provide a conceptual framework that allows replicated effective interventions in other contexts.14 In this paper, we propose to construct a modified Theory of Planned Behavior (TPB) to explain the effects of empowerment enrollment in PEP on the behaviors of people with DM through behavioral intention.
In the original TPB, the followings are triggers for an individual to have a behavioral intention to engage in a healthy behavior: attitude (a person’s cognitive and affective evaluation of a healthy behavior such as exercise as being good for them to manage their DM); subjective norms (the important people in a person’s life who encourage the person to perform healthy behaviors, such as ‘my spouse would like me to exercise to manage my DM)’; and perceived behavioral control (the confidence or capability to perform a healthy behavior, such as ‘I am confident to do exercises for DM management’).15 In addition, perceived behavioral control contributes to the engagement of the final behavior (e.g. the diabetes self-care behaviors in this study). However, the parsimony of the TPB has been criticized as insufficient in explaining a complicated psychological mechanism.16 For these reasons, studies have suggested modifying the TPB to include important factors to explain specific behaviors in respective contexts (e.g. risk perception for behaviors that may contribute to health problems).17–23 Although all the original TPB factors are relevant to people with DM (e.g.24,25), adding other relevant underlying factors, such as the risk perception mentioned above, may increase the capability of TPB to explain behaviors for people with DM.
Health literacy and risk perception were added because both factors help an individual judge the importance of a healthy behavior.26–28 For example, a person with DM who has good health literacy in DM management knows that exercise is important, and may have higher intention to exercise than a person with DM who does not have such knowledge. Also, if a person with DM acknowledges that excessive sugar intake may worsen the symptoms (a kind of risk perception), he or she may not want to consume sugar. Moreover, enrollment in empowerment sessions in PEP was included in the modified TPB because the empowerment concept indicates the need to provide the capability for patients to engage in health decision-making. Thus, attending PEP sessions may enhance the behavioral intention of a person with DM to perform appropriate diabetes self-care behaviors.
Thus, we proposed a modified TPB for people with DM attending PEP, by adding the concepts of health literacy and risk perception. Additionally, we treated enrollment of empowerment sessions in the PEP as an exploratory variable in the modified TPB to assess whether enrollment of empowerment sessions in the PEP works on behavioral intention, and finally change the diabetes self-care behaviors of people with DM. In the modified TPB, the six factors were hypothesized to predict behavioral intention: attitude, subjective norm, perceived behavioral control, health literacy, risk perception, and enrollment in empowerment sessions. Perceived behavioral control and behavioral intention were hypothesized to explain four types of diabetes self-care behaviors: diet control, exercise, blood glucose monitoring, and foot care. Moreover, behavioral intention was hypothesized to be a mediator in the modified TPB.
Methods
Before commencement, the study was examined and approved by the Departmental Research Committee, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University.
Study design and procedures
A longitudinal design was used.
Participant recruitment
Participants were recruited from patients with DM who were referred to the PEP by medical doctors at general outpatient clinics. Specifically, participants were recruited from one community-based organization, which served four areas in Hong Kong during the study period. The inclusion criteria included: 18 years of age or above, diagnosed with type 2 DM by medical officers, and volunteering to participate in the study. Several research assistants first explained the objectives and procedures of the study to eligible participants before the commencement of the PEP. Those who were interested in the study were then requested to provide written informed consent. After signing consent, the participants completed the set of questionnaires with support from the research assistants. The participants were approached again by the research assistants 3 months after the first assessment to complete part of the same set of questionnaires.
Patient empowerment program
PEP, a primary care initiative collaborated by the Hospital Authority and nongovernment organizations in Hong Kong SAR under Family Medicine, consists of two components: two education sessions conducted by nurses and five empowerment sessions on DM self-management conducted by trained health professionals such as social workers. In brief, the entire PEP comprises seminars and empowerment sessions, where all participants attended all seminars, and over 90% of participants who enrolled in the empowerment sessions completed all sessions. The education sessions were conducted using seminars. Specifically, all participants were first given a seminar delivering health knowledge on diabetes care, and some attended the empowerment sessions based on their autonomy. The empowerment sessions were conducted using small-group interactive workshops. Specifically, social workers and healthcare providers used different methods to enlarge the patient’s perception on his or her contribution to decisions making. Moreover, self-efficacy and self-management behaviors were taught in these sessions using the design of the Stanford Chronic Disease Self-management Program.9 In brief, education sessions focused more on information delivery, and the empowerment sessions emphasized a more hands-on practice (such as practicing action planning, problem solving, and experience sharing). Other detailed information on PEP is described elsewhere.9–12
Instruments
All the following measures were administered to DM patients at baseline. Behavioral intention and diabetes self-care behaviors were assessed again at the end of the PEP (i.e. the post-test conducted 3 months after the baseline).
Health literacy was measured using 15 multiple-choice questions described in the Chinese Health Literacy Scale for Diabetes,29 which measures the capability of a respondent regarding their understanding and processing of basic health information that assists in health decisions. A higher score represents better knowledge in health literacy. The basic psychometric properties of the Chinese Health Literacy Scale for Diabetes were acceptable in the current sample: Cronbach’s α = 0.88.
Risk perception was measured by the Risk Perception Survey for Developing Diabetes,30 which was recently translated into Chinese with established linguistic validity and acceptable psychometric properties.9 A higher score indicates a higher level of risk perception in diabetes. The basic psychometric properties of the Chinese Risk Perception Survey for Developing Diabetes were acceptable in the current sample: Cronbach’s α = 0.78.
Diabetes self-efficacy was used to capture the perceived behavioral control in the TPB, and was measured using eight items rated on a 1–10 scale, where 1 indicates no confidence at all and 10 indicates full confidence.31 The Diabetes Self-Efficacy Scale was recently translated into Chinese with established linguistic validity and acceptable psychometric properties.9 A higher score indicates a higher level of behavioral control in diabetes. The basic psychometric properties of the Diabetes Self-Efficacy Scale were acceptable in the current sample: Cronbach’s α = 0.81.
Attitude was measured using four items rated on a five-point Likert-type scale (1 = strongly disagree; 5 = strongly agree) designed by the authors. These four items were designed according to the major components of PEP including regular exercises, emotional management, problem solving, and health information seeking. A sample item is ‘Doing exercise such as jogging, swimming, and bicycling can improve your health.’ A higher score indicates better attitude toward engaging diabetes self-care behaviors. The basic psychometric properties of the four items were acceptable in the current sample: Cronbach’s α = 0.77.
Subjective norm was measured using four items on how the family members of the participants encourage and support them to perform diabetes self-care behaviors using a five-point Likert-type scale (1 = strongly disagree; 5 = strongly agree). A higher score indicates a higher level of subjective norm. These four items were designed according to various roles of family members highlighted in the intervention. The basic psychometric properties of the four items were acceptable in the current sample: Cronbach’s α = 0.71.
Behavioral intention was measured using eight items retrieved from the Chinese version of the University of Rhode Island Change Assessment and rated on a five-point Likert-type scale (1 = strongly disagree; 5 = strongly agree).32 A higher score indicates more intention to engage in diabetes self-care behaviors. The basic psychometric properties of the four items were acceptable in the current sample: Cronbach’s α = 0.70 (baseline measure) and 0.75 (post-test).
Diabetes self-care behaviors were measured using eight items retrieved from the Summary of Diabetes Self-Care Activities, which measures the self-perceived performance of a respondent on four behaviors (diet control, exercise, blood glucose monitoring, and foot care) in the past 7 days.8 The original diet control subscale in the Summary of Diabetes Self-Care Activities contains four items (two on general eating plan and another two on frequency of servings of fruits and vegetables), and we used only two frequency items in the current study. The main reason is because the general eating plan reflects less on the actual diabetes self-care behaviors, and more on the cognitive aspect of the behaviors; that is, planning for diabetic diet. For example, a person plans to eat vegetables does not mean that the person actually eats vegetables. The person may plan to eat vegetables and finally does not eat them because of other barriers. Therefore, we considered that a general eating plan cannot indicate whether a patient with DM really engaged in self-care behaviors. A higher score in the Summary of Diabetes Self-Care Activities indicates better diabetes self-care behaviors. Given that the four behaviors were different, we separated these behaviors in our analyses.
Data analysis
In addition to the descriptive statistics, we used paired t tests to examine the changes in diabetes self-care behaviors for the entire sample, for the subsample who enrolled in the empowerment sessions (n = 209), and for the subsample who did not enroll in the empowerment sessions (n = 156).
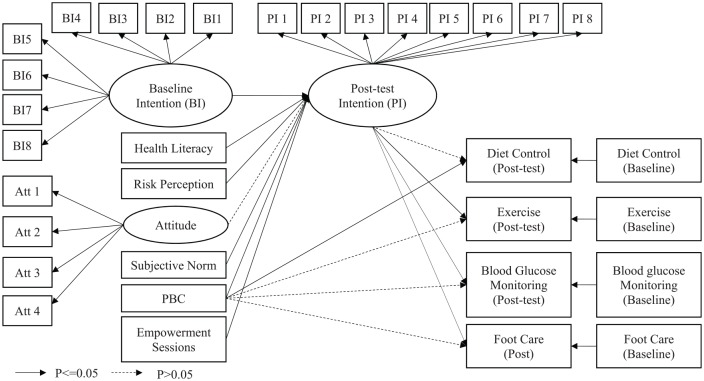
A modified TPB on the whole sample was examined using structural equation modeling (SEM) (n = 365). In the SEM, we examined whether health literacy, risk perception, attitude, perceived behavioral control, and enrollment of empowerment sessions (yes versus no) predicted post-test behavioral intention, and whether perceived behavioral control and post-test behavioral intention explained each diabetes self-care behavior: diet control, exercise, blood glucose monitoring, and foot care. In addition, baseline behavioral intention and diabetes self-care behaviors were controlled in the SEM (Figure 1). The fitness of the proposed model was estimated using the diagonally weighted least-square method, and examined using the following criteria in the fit indices: a nonsignificant Chi-square test, comparative fit index (CFI), Tucker-Lewis index (TLI) >0.9, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR) <0.08, and weighted root mean square residual (WRMR) <1.0.22,33,34 Moreover, given that behavioral intention could be a mediator in the modified TPB, we further used a bootstrapping method to examine whether the mediated effect was significant using a bootstrap-based p-value < 0.05.
Figure 1.
The examined modified TPB model and the result.
BI, baseline intention; PBC, perceived behavioral control; PI, post-test intention; TPB theory of planned behavior.
In both regression and SEM analyses, missing values were tackled using multiple imputation methods. Additionally, the missing values occurred in the post-test self-management behaviors (29.0% in diet control and foot care; 29.6% in exercise; 30.1% in blood glucose monitoring).
All the descriptive statistics and paired t tests were performed using SPSS 23.0 (IBM, Armonk, NY, USA); the SEM and the bootstrapping method were conducted using the lavaan package in R software (http://lavaan.ugent.be/).
Results
After approaching 744 patients with DM, 365 agreed to participate in the study. The mean age (SD) of the 365 participants was 62.94 (9.56) years, mean duration of having DM was 5.00 (6.47) years, and slightly less than half were males (41.4%). Nearly three-quarters of the participants had been married (74.2%). Table 1 presents the participants’ scores for risk perception, perceived behavioral control, health literacy, attitude, and behavioral intention.
Table 1.
Participant characteristics (n = 365).
| Age (year); M ± SD | 62.9 ± 9.6 |
| Gender (male); n (%) | 151 (41.4) |
| Marital status (married); n (%) | 271 (74.2) |
| Educational level (primary or below); n (%) | 163 (44.7) |
| Occupation (full or part time employed); n (%) | 116 (31.8) |
| Duration of having diabetes mellitus (years); M ± SD | 5.00 ± 6.47 |
| Enrollment of empowerment sessions; n (%) | 210 (57.5) |
| Risk perception (0–5 MCQ); M ± SD | 2.71 ± 0.30 |
| Perceived behavioral control (1–10 scale); M ± SD | 7.12 ± 1.69 |
| Health literacy (0–15 MCQ); M ± SD | 9.92 ± 4.15 |
| Attitude (1–5 Likert scale); M ± SD | 4.03 ± 0.41 |
| Subjective norm (1–5 Likert scale); M ± SD | 3.42 ± 0.63 |
| Baseline intention (1–5 Likert scale); M ± SD | 3.99 ± 0.33 |
| Follow-up intention (1–5 Likert scale); M ± SD | 3.93 ± 0.32 |
M, mean; MCQ, multiple-choice question; N, frequency; SD, standard deviation.
Diabetes self-care behaviors were significantly improved at post-test compared with baseline scores (p = 0.028 for diet control; <0.001 for exercise, blood glucose monitoring, and foot care) using the whole sample. After stratifying the sample into two subsamples (with and without the empowerment sessions), the improvement was stronger in the subsample with empowerment sessions (p < 0.001 for all behaviors) than for the subsample without empowerment sessions (p = 0.13 for diet control, 0.008 for exercise, 0.023 for blood glucose monitoring, and 0.042 for foot care; Table 2).
Table 2.
Changes in self-management behavior.
| Behavior | Baseline score | Post score | Difference (p value) |
|---|---|---|---|
| All participants | |||
| Diet control (n = 259) | 4.97 | 5.28 | 0.31 (0.028) |
| Exercise (n = 257) | 3.91 | 4.78 | 0.87 (<0.001) |
| Blood glucose monitoring (n = 255) | 0.83 | 1.81 | 0.98 (<0.001) |
| Foot care (n = 259) | 2.11 | 3.20 | 1.09 (<0.001) |
| Enrolled in the empowerment sessions | |||
| Diet control (n = 160) | 4.66 | 5.34 | 0.68 (<0.001) |
| Exercise (n = 159) | 3.95 | 5.01 | 1.06 (<0.001) |
| Blood glucose monitoring (n = 156) | 0.70 | 2.06 | 1.36 (<0.001) |
| Foot care (n = 159) | 2.11 | 3.54 | 1.43 (<0.001) |
| Not enrolled in the empowerment sessions | |||
| Diet control (n = 99) | 5.48 | 5.19 | −0.29 (0.13) |
| Exercise (n = 98) | 3.84 | 4.40 | 0.57 (0.008) |
| Blood glucose monitoring (n = 99) | 1.04 | 1.42 | 0.38 (0.023) |
| Foot care (n = 100) | 2.12 | 2.67 | 0.55 (0.042) |
The modified TPB showed satisfactory fit, except for the significant Chi-square test (χ2 = 674.748; df = 530; p < 0.001), CFI = 0.927, TLI = 0.917, RMSEA (90% CI) = 0.027 (0.021, 0.033), SRMR = 0.056, and WRMR = 1.007. Moreover, baseline intention [standardized coefficient (β) = 0.258; p < 0.001], health literacy (β = 0.117, p = 0.028), risk perception (β = 0.098, p = 0.029), subjective norm (β = 0.180, p = 0.001), perceived behavioral control (β = 0.115, p = 0.003), and, with the empowerment sessions (β = 0.288, p < 0.001), significantly predicted post-test behavioral intention. The post-test behavioral intention was significantly associated with three behaviors: exercise (β = 0.287, p < 0.001), blood glucose monitoring (β = 0.229, p = 0.001), and foot care (β = 0.441, p < 0.001) (Table 3). Bootstrapping further examined the mediated effects of behavioral intention; the results showed that the effects of empowerment sessions on exercise and foot care behaviors were all mediated by behavioral intention (Table 4).
Table 3.
Results of proposed model.
| Dependent variable | Coefficient | SE | p-value | Standardized coefficient |
|---|---|---|---|---|
| Independent variable | ||||
| Post-test intention a | ||||
| Baseline intentionb | 0.323 | 0.080 | <0.001 | 0.258 |
| Health literacy | 0.009 | 0.003 | 0.028 | 0.117 |
| Risk perception | 0.106 | 0.049 | 0.029 | 0.098 |
| Attitudec | −0.022 | 0.020 | 0.271 | −0.041 |
| Subjective normd | 0.099 | 0.030 | 0.001 | 0.180 |
| Perceived behavioral control | 0.023 | 0.008 | 0.003 | 0.115 |
| Empowerment sessions (Yes) | 0.189 | 0.033 | <0.001 | 0.288 |
| Post-test diet control | ||||
| Baseline diet control | 0.165 | 0.052 | 0.001 | 0.195 |
| Post-measured intention | 0.116 | 0.177 | 0.53 | 0.022 |
| Perceived behavioral control | 0.171 | 0.060 | 0.005 | 0.165 |
| Post-test exercise | ||||
| Baseline exercise | 0.412 | 0.063 | <0.001 | 0.456 |
| Post-measured intention | 1.050 | 0.287 | <0.001 | 0.158 |
| Perceived behavioral control | 0.022 | 0.093 | 0.82 | 0.017 |
| Post-test blood glucose monitoring | ||||
| Baseline blood glucose monitoring | 0.658 | 0.132 | <0.001 | 0.505 |
| Post-measured intention | 0.730 | 0.229 | 0.001 | 0.122 |
| Perceived behavioral control | −0.017 | 0.064 | 0.79 | −0.014 |
| Post-test foot care | ||||
| Baseline foot care | 0.396 | 0.067 | <0.001 | 0.370 |
| Post-measured intention | 2.808 | 0.441 | <0.001 | 0.343 |
| Perceived behavioral control | −0.046 | 0.092 | 0.62 | −0.029 |
The standardized factor loadings for items on baseline intention were all significant and ranged from 0.31 to 0.51.
The standardized factor loadings for items on post-measured intention were all significant and ranged from 0.34 to 0.73.
The standardized factor loadings for items on attitude were all significant and ranged from 0.66 to 0.88.
The standardized factor loadings for items on subjective norm were all significant and ranged from 0.53 to 0.70.
Table 4.
Mediated effects of intention using bootstrapping method.
| Behavior | Independent variable | Coefficient (bootstrap SE)/p value | Standardized coefficient |
|---|---|---|---|
| Diet control | Health literacy | 0.001 (0.004)/0.79 | 0.003 |
| Exercise | Health literacy | 0.009 (0.013)/0.47 | 0.018 |
| Blood glucose monitoring | Health literacy | 0.007 (0.010)/0.49 | 0.014 |
| Foot care | Health literacy | 0.025 (0.034)/0.45 | 0.040 |
| Diet control | Risk perception | 0.012 (0.044)/0.78 | 0.002 |
| Exercise | Risk perception | 0.111 (0.096)/0.25 | 0.015 |
| Blood glucose monitoring | Risk perception | 0.077 (0.073)/0.29 | 0.012 |
| Foot care | Risk perception | 0.297 (0.219)/0.18 | 0.034 |
| Diet control | Subjective norm | 0.011 (0.045)/0.80 | 0.004 |
| Exercise | Subjective norm | 0.104 (0.102)/0.31 | 0.028 |
| Blood glucose monitoring | Subjective norm | 0.072 (0.069)/0.29 | 0.022 |
| Foot care | Subjective norm | 0.277 (0.220)/0.21 | 0.062 |
| Diet control | PBC | 0.003 (0.009)/0.78 | 0.003 |
| Exercise | PBC | 0.024 (0.026)/0.35 | 0.018 |
| Blood glucose monitoring | PBC | 0.016 (0.018)/0.37 | 0.014 |
| Foot care | PBC | 0.063 (0.055)/0.25 | 0.039 |
| Diet control | Empowerment | 0.022 (0.061)/0.72 | 0.006 |
| Exercise | Empowerment | 0.198 (0.095)/0.04 | 0.045 |
| Blood glucose monitoring | Empowerment | 0.138 (0.080)/0.09 | 0.035 |
| Foot care | Empowerment | 0.530 (0.141)/<0.001 | 0.099 |
PBC, perceived behavioral control; SE, standard error.
Discussion
Similar to the findings of Cheung and his colleagues,9 our results indicated that PEP is an effective program in improving diabetes self-care behaviors. Although we found that participants who did not enroll in the empowerment sessions also had improved diabetes self-care behaviors, our analyses showed that those who had attended the empowerment sessions gained more improvement than those who did not attend the empowerment sessions of PEP. Because all participants had attended a seminar introducing the importance of diabetes self-care behaviors, those who did not attend empowerment sessions might have gained the benefits in the seminar and subsequently improved their diabetes self-care behaviors. Nevertheless, the effects of attending the empowerment sessions of PEP were promising, and were partly explained by the modified TPB. The modified TPB revealed that the empowerment sessions of PEP had significant effects on the behavioral intention of participants with DM, and that behavioral intention was associated with increases in the participants’ performance on the three diabetes self-care behaviors: exercise, blood glucose monitoring, and foot care.
With improvement in diabetes self-care behaviors, people with DM are likely to gain health benefits, as shown by Wong and colleagues.10–12 The modified TPB we proposed, however, explained only part of the effects of the empowerment sessions on diabetes self-care behaviors. That is, the modified TPB showed that behavioral intention was significantly associated with engagements in exercise, blood glucose monitoring, and foot care. Therefore, the modified TPB demonstrates that people with DM who attended more empowerment sessions in the PEP had more health-protective behaviors (i.e. more frequent diabetes self-care behaviors) through elevated behavioral intention. However, given that we did not assess the level of empowerment for participants, one cannot conclude whether the improved diabetes self-care behaviors are caused by patient empowerment. Specifically, there are two possibilities to explain the positive relationships we found in the modified TPB: first, when the participants were empowered (i.e. making decisions on their owns), they exhibited health-protective behaviors; second, when the participants were influenced by healthcare providers (i.e. not making decisions on their owns), they had health-damaging behaviors. These two possible conditions can both result in a positive relationship between enrollment of empowerment sessions and diabetes self-care behaviors. Therefore, future studies are needed to further clarify the degree to which condition more reflects reality.
Dietary control was not significantly correlated with behavioral intention in the modified TPB. A possible explanation is that the benefits of dietary control are well known in the general population.26,35 In other words, our participants might have had good diet control before they entered the PEP. Our findings in diabetes self-care behaviors showed that the participants had higher scores and lower improvements in diet control (4.97 at baseline and 5.28 at post-test) as compared with exercise (3.91 at baseline and 4.78 at post-test), blood glucose monitoring (0.83 at baseline and 1.81 at post-test), and foot care (2.11 at baseline and 3.20 at post-test). As having good diet control was already shaped before behavioral intention, our participants might not have gained further benefits from elevated behavioral intention.
The strength of this study includes applying a psychological model to explain the PEP effects on a relatively large sample (n = 365) with DM. Also, a longitudinal study with a 3-month post-test provides stronger evidence of causal relationships to determine PEP effects.
There are several limitations to this study. First, participants were recruited from one operating organization. Patients with DM who received healthcare services from other operating organizations were not included in this study. Given that the PEP might be conducted differently in different operating organizations, this may limit the external validity of our findings. Second, the diabetes self-care behaviors were based on patient subjective self-report, and we were unable to exclude the effects of recall bias and social desirability, particularly in older patients. Future studies using objective measures are thus encouraged. Alongside this limitation, some of our questionnaire items were designed to specify ‘diabetes’ and may sound artificial and illogical to respondents. Future research should consider whether it is necessary to use the term ‘diabetes’ specifically when designing questionnaire items. Moreover, the items on attitude and subjective norm were designed by the authors according to their past PEP experience. Therefore, the validity of attitude and subjective norm may not be perfect. However, we believe that this will not be a serious problem given the high internal consistency of our findings (α = 0.77 for attitude and 0.71 for subjective norm).
Third, all the participants were diagnosed as type 2 DM; our results cannot be generalized to those with type 1 DM. Although the prevalence of type 1 DM is much less than that of type 2 DM,36 people with type 1 DM are also likely to benefit from PEP. Future studies including patients with type 1 DM are thus recommended. Fourth, although we measured four important diabetes self-care behaviors for our patients with type 2 DM, we did not assess their adherence to medication. Given that medication adherence is another important diabetes self-care behavior for people with type 2 DM, future studies are warranted to see whether our modified TPB model with enrollment of empowerment sessions can explain medication adherence. Fifth, our study is not a randomized controlled trial. With the lack of a control group, caution should be taken when making conclusions on the effectiveness of the PEP. Nevertheless, our results provide somewhat strong evidence of the causal relationship between other baseline measures (i.e. risk perception, attitude, and empowerment sessions) and behavioral intention. Last, we did not actually measure the level of psychological empowerment of participants. Rather, we simply postulated that, if a participant attended empowerment sessions, the participant was empowered. However, attending empowerment sessions is not equivalent to having a high level of empowerment. Therefore, future studies are warranted, and these should use a validated instrument to assess empowerment and additionally investigate whether our postulation is supported.37
Conclusion
In conclusion, the modified TPB describes why the PEP is an effective program to improve the diabetes self-care behaviors of people with type 2 DM. Healthcare providers may consider incorporating other techniques in the PEP (e.g. cognitive behavioral and motivational interviewing techniques) to enhance the behavioral intention for people with DM; thus, their behaviors in exercise, blood glucose monitoring, and foot care can be improved. However, behavioral intention showed no effect on changes in diet control and exercise. Thus, future studies are encouraged to examine other possible mechanisms to explain the effectiveness of PEP on diet control and exercise behaviors.
Using our results, two implications can be applied in clinical settings. First, we found that better health literacy, higher risk perception, higher level of subjective norm, and greater perceived behavioral control toward diabetes self-care behaviors had positive effects on behavioral intention, and, consequently, improved exercise, blood glucose monitoring, and foot care for our participants. Therefore, healthcare providers may want to enhance health literacy, risk perception, subjective norm, and perceived behavioral control for people with DM. That is, our results echo the suggestion made by Cheung and his colleagues (p. 1895) that ‘modification of the current content of PEP could thus include the addition of an element to enhance patients’ risk perception by operating organizations.’9 Moreover, the addition may also include increasing perceived behavioral control since other studies have shown the effects of perceived behavioral control on self-management skills among people with chronic illness.38,39 Second, behavioral intention was a significant mediator between PEP and two behaviors (exercise and foot care) in our modified model. Additionally, the association between behavioral intention and the two behaviors was strongly significant. Thus, healthcare providers may consider incorporating other techniques in the PEP to improve the behavioral intention for people with DM.
Footnotes
Authors’ note: All authors contributed to the study concept and design. CYL and MKC contributed to data analysis, interpretation of data, and drafting the paper. MKC, ATH, and SCC contributed to the acquisition of data. All authors were responsible for revising the manuscript critically for important intellectual content, and approved the version to be published.
Funding: The authors received no financial support for the research, authorship, and publication of this article.
Conflict of interest statement: The authors declare that there is no conflict of interest.
ORCID iD: Mike K.T. Cheung  https://orcid.org/0000-0002-7238-6788
https://orcid.org/0000-0002-7238-6788
Contributor Information
Chung-Ying Lin, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China.
Mike K. T. Cheung, The Hong Kong Society for Rehabilitation, Room 9B, 1/F, HKSR Lam Tin Complex, 7 Rehab Path, Lam Tin, Kowloon, Hong Kong SAR, China.
Anchor T. F. Hung, The Hong Kong Society for Rehabilitation, Hong Kong SAR, China
Peter K. K. Poon, The Hong Kong Society for Rehabilitation, Hong Kong SAR, China
Sam C. C. Chan, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China
Chetwyn C. H. Chan, Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China
References
- 1. Lin CY, Lee TY, Sun ZJ, et al. Development of diabetes-specific quality of life module to be in conjunction with the World Health Organization quality of life scale brief version (WHOQOL-BREF). Health Qual Life Outcomes 2017; 15: 167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014; 103: 137–149. [DOI] [PubMed] [Google Scholar]
- 3. International Diabetes Federation. IDF diabetes atlas 2017. 8th ed. Brussels: International Diabetes Federation. [PubMed] [Google Scholar]
- 4. Hunt BR, Whitman S, Henry CA. Age-adjusted diabetes mortality rates vary in local communities in a metropolitan area: racial and spatial disparities and correlates. Diabetes Care 2014; 37: 1279–1286. [DOI] [PubMed] [Google Scholar]
- 5. Solli O, Stavem K, Kristiansen IS. Health-related quality of life in diabetes: the associations of complications with EQ-5D scores. Health Qual Life Outcomes 2010; 8: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Babazadeh T, Dianatinasab M, Daemi A, et al. Association of self-care behaviors and quality of life among patients with type 2 diabetes mellitus: Chaldoran County, Iran. Diabetes Metab J 2017; 41: 449–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Saffari M, Lin CY, O’Garo K, et al. Psychometric properties of Persian diabetes-mellitus specific quality of life (DMQoL) questionnaire in a population-based sample of Iranians. Int J Diabetes Dev Ctries 2018; 39: 218–227. [Google Scholar]
- 8. Wu SFV, Courtney M, Edwards H, et al. Self-efficacy, outcome expectations and self-care behaviour in people with type 2 diabetes in Taiwan. J Clin Nurs 2007; 16: 250–257. [DOI] [PubMed] [Google Scholar]
- 9. Cheung MK, Chan SC, Hung AT, et al. A latent profile analysis on patient empowerment programme in a Hong Kong primary care setting. Patient Educ Couns 2017; 100: 1890–1897. [DOI] [PubMed] [Google Scholar]
- 10. Wong CK, Wong WC, Lam CL, et al. Effects of patient empowerment programme (PEP) on clinical outcomes and health service utilization in type 2 diabetes mellitus in primary care: an observational matched cohort study. PLoS One 2014; 9: e95328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wong CK, Wong WC, Wan YF, et al. Patient empowerment programme in primary care reduced all-cause mortality and cardiovascular diseases in patients with type 2 diabetes mellitus: a population-based propensity-matched cohort study. Diabetes Obes Metab 2015; 17: 128–135. [DOI] [PubMed] [Google Scholar]
- 12. Wong CK, Wong WC, Wan EY, et al. Increased number of structured diabetes education attendance was not associated with the improvement in patient-reported health-related quality of life: results from patient empowerment programme (PEP). Health Qual Life Outcomes 2015; 13: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nutbeam D. Health promotion glossary. Health Promot Int 1998; 13: 349–364. [Google Scholar]
- 14. Lin CY, Strong C, Scott AJ, et al. A cluster randomized controlled trial of a theory-based sleep hygiene intervention for adolescents. Sleep 2018; 41: 170. [DOI] [PubMed] [Google Scholar]
- 15. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991; 50: 179–211. [Google Scholar]
- 16. Sniehotta FF, Presseau J, Araújo-Soares V. Time to retire the theory of planned behaviour. Health Psychol Rev 2014; 8: 1–7. [DOI] [PubMed] [Google Scholar]
- 17. Ajzen I. The theory of planned behaviour is alive and well, and not ready to retire: a commentary on Sniehotta, Presseau, and Araújo-Soares. Health Psychol Rev 2015; 9: 131–137. [DOI] [PubMed] [Google Scholar]
- 18. Conner M. Extending not retiring the theory of planned behaviour: a commentary on Sniehotta, Presseau and Araújo-Soares. Health Psychol Rev 2015; 9: 141–145. [DOI] [PubMed] [Google Scholar]
- 19. Gollwitzer PM, Oettingen G. From studying the determinants of action to analysing its regulation: a commentary on Sniehotta, Presseau and Araújo-Soares. Health Psychol Rev 2015; 9: 146–150. [DOI] [PubMed] [Google Scholar]
- 20. Schwarzer R. Some retirees remain active: a commentary on Sniehotta, Presseau and Araújo-Soares. Health Psychol Rev 2015; 9: 138–140. [DOI] [PubMed] [Google Scholar]
- 21. Trafimow D. On retiring the TRA/TPB without retiring the lessons learned: a commentary on Sniehotta, Presseau and Araújo-Soares. Health Psychol Rev 2015; 9: 168–171. [DOI] [PubMed] [Google Scholar]
- 22. Lin CY, Oveisi S, Burri A, et al. Theory of planned behavior including self-stigma and perceived barriers explain help-seeking behavior for sexual problems in Iranian women suffering from epilepsy. Epilepsy Behav 2017; 68: 123–128. [DOI] [PubMed] [Google Scholar]
- 23. Lin CY, Updegraff JA, Pakpour AH. The relationship between the theory of planned behavior and medication adherence in patients with epilepsy. Epilepsy Behav 2016; 61: 231–236. [DOI] [PubMed] [Google Scholar]
- 24. Baig AA, Benitez A, Quinn MT, et al. Family interventions to improve diabetes outcomes for adults. Ann N Y Acad Sci 2015; 1353: 89–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rosa S, Sunvisson H, Ahlström G. Lived experience of significant others of persons with diabetes. J Clin Nurs 2007; 16: 215–222. [DOI] [PubMed] [Google Scholar]
- 26. Lin CY, Scheerman JF, Yaseri M, et al. A cluster randomised controlled trial of an intervention based on the health action process approach for increasing fruit and vegetable consumption in Iranian adolescents. Psychol Health 2017; 32: 1449–1468. [DOI] [PubMed] [Google Scholar]
- 27. Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull 2014; 140: 511–543. [DOI] [PubMed] [Google Scholar]
- 28. Wynia MK, Osborn CY. Health literacy and communication quality in health care organizations. J Health Commun 2010; 15: 102–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Leung AY, Lau HF, Chau PH, et al. Chinese health literacy scale for diabetes–multiple-choice version (CHLSD-MC): a validation study. J Clin Nurs. 2015; 24: 2679–2682. [DOI] [PubMed] [Google Scholar]
- 30. Walker EA, Mertz CK, Kalten MR, et al. Risk perception for developing diabetes: comparative risk judgments of physicians. Diabetes Care 2003; 26: 2543–2548. [DOI] [PubMed] [Google Scholar]
- 31. Lorig K, Ritter PL, Laurent DD, et al. Online diabetes self-management program: a randomized study. Diabetes Care 2010; 33: 1275–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chan SC, Chan CC, Siu AM, et al. Stage of change in self-management of chronic diseases: psychometric properties of the Chinese version of the University of Rhode Island change assessment (C-URICA) scale. Rehabil Psychol 2007; 52: 103. [Google Scholar]
- 33. Cook KF, Kallen MA, Amtmann D. Having a fit: impact of number of items and distribution of data on traditional criteria for assessing IRT’s unidimensionality assumption. Qual Life Res 2009; 18: 447–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lin YC, Strong C, Tsai MC, et al. Validating sizing them up: a parent-proxy weight-related quality-of-life measure, with community-based children. Int J Clin Health Psychol 2018; 18: 81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ou HT, Su CT, Luh WM, et al. Knowing is half the battle: the association between leisure-time physical activity and quality of life among four groups with different self-perceived health status in Taiwan. Appl Res Qual Life 2017; 12: 799–812. [Google Scholar]
- 36. Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: a review of current trends. Oman Med J 2012; 27: 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Spreitzer GM. Psychological empowerment in the workplace: dimensions, measurement, and validation. Acad Manage J 1995; 38: 1442–1465. [Google Scholar]
- 38. Chan SC, Chan CC. Attitude, social influence, and self-efficacy among Chinese participants of chronic disease self-management program: a latent growth curve modeling study. Rehabil Psychol 2011; 56: 191–199. [DOI] [PubMed] [Google Scholar]
- 39. Chan SC, Chan CC, Siu AM, et al. A conceptual model of patient-professional communication as a self-management skill: a latent growth change modeling. Disabil Health J 2015; 8: 602–610. [DOI] [PubMed] [Google Scholar]