Abstract
Background
Trauma registries are essential to trauma systems, to enable collection of the data needed to enhance clinical knowledge and monitor system performance. The King Saud Medical City (KSMC) in Riyadh, Kingdom of Saudi Arabia (KSA) is aiming to become a Level 1 Trauma Centre, and required a trauma registry in order to do so. Our objective was to establish the Saudi TraumA Registry (STAR) at the (KSMC) and ready it for national deployment. The challenge was that no formal trauma data collection had occurred previously and clinicians had no prior experience of trauma registries.
Methods
To develop the registry, a novel 12 step implementation plan was created and followed at the KSMC. Registry criteria and a Minimum Dataset were selected; training was delivered; database specifications were written; operating procedures were developed and regular reporting was initiated.
Results
Data collection commenced on August 1st 2017. The registry was fully operational by April 2018, eight months ahead of schedule. During the first year of data collection an average of 216 records per month were entered into the database. An inaugural report was presented at the Saudi Trauma Conference in February 2019.
Conclusions
The strategy deployed at the KSMC has successfully established the STAR. In the short term, process indicators will track the development of the hospital into a Level 1 Trauma Centre. In the medium to long term the STAR will be rolled out nationally to capture the impact of public health initiatives aimed at reducing injury in the KSA. The effect of the STAR will be that the country is better equipped to deliver continuous improvements in trauma systems and quality of care.
Keywords: Registries, Epidemiological Monitoring, Trauma Severity Indices, Benchmarking, Data Collection
Background
Injuries are a significant cause of death and disability worldwide, regardless of the development status of the country [1]. The World Health Organization (WHO) reported on the magnitude of the entire problem at the Global Forum on Trauma Care in 2009 [2], and also declared the targeted Decade of Action for Road Safety 2011–2020 [3]. Trauma systems have been developed to address this growing threat to public health, of which the Victorian State Trauma System (VSTS) is a world-class example. A key component system wide monitoring and governance, based on accurate data from the state trauma registry. Following implementation in 2000, risk adjusted mortality decreased by 50% [4].
The Kingdom of Saudi Arabia (KSA) is the largest Arab country in the Middle East and is highly developed. It has a rapidly growing population estimated at 32.4 million people in 2017 [5] but is suffering a well-documented rise in the incidence of serious injuries that occur on the roads, in the workplace and elsewhere [6, 7]. Health care is provided largely by the Saudi Arabian Ministry of Health (MOH) with 407 primary health care centres. Other health care sectors include university, military and private groups [8]. MOH hospitals provide emergency care at Emergency Departments and it is to these that most trauma patients are transported by a combination of Saudi Red Crescent Society ambulances, private ambulances, police or military vehicles and private transport.
In response to the increasing burden of traumatic injuries on the community, the MOH requested the King Saud Medical City (KSMC) to engage the Alfred Hospital and Monash University to assist with trauma service development, including a trauma registry program based on the Victorian model which could be scaled to the country as a whole. This study aimed to examine the process of establishing the registry at the hospital with a view to rolling the prototype out nationally. This was a challenge as the hospital had no previous involvement with a trauma registry and it required establishment without any prior experience from clinical staff.
KSMC is located in the capital city, Riyadh, which is home to approximately six million people. It is the MOH centre that receives the most emergency patients in the Kingdom [9] and is therefore the logical initial site for a trauma registry that ultimately will be rolled out nationally. Recent reports reveal that approximately 350 people a day present to the Emergency Department (ED) at the KSMC, a significant proportion of whom will be admitted to one of the facility’s 1400 beds. Over 300 people per month presented with the level of trauma that potentially fell within the population of interest for a registry. To capture these data accurately required considerable effort and a robust methodology.
Methods
Work plan
A plan was created by the project team, based on the operating principles in the 2008 Australian Commission on Safety and Quality in Healthcare (ACSQH) [10], that stipulated 12 steps (Table 1).
Table 1.
Trauma registry implementation 12 step plan
| Step | Rationale |
|---|---|
| Step 1. Select inclusion criteria. | Trauma registries must consider the population of interest and determine the characteristics of eligible cases. It is not practical for a registry to collect all cases, as the burden and the cost of data collection would very quickly outweigh the benefit of the information gained from trivial or minor injuries. |
| Step 2. Select exclusion criteria. | It is equally important to select appropriate exclusion criteria, as this will assist in identifying cases of interest and increase the likelihood that only cases that meet criteria are registered on the database. Similar to the inclusion criteria, they must be clearly documented and applied rigorously. |
| Step 3. Select Minimum Dataset (MDS). | Once the population of interest has been considered and the inclusion and exclusion criteria have been identified, the Registry must select data items that will best capture the required information. Data items are otherwise known as variables, data elements or data points. The items must then be documented in a data dictionary that unequivocally defines each element and provides the rules for use. |
| Step 4. Identify data sources. | Selected data items must be readily available from the medical record or existing hospital systems. To ensure consistent data collection practices and reproducible data, the source of each item must be identified so that the same piece of information can be obtained from the same place for every case. The source should be documented in operational documents for ongoing reference by Registry staff. |
| Step 5. Determine method of collection. | Data collection methods depend on the existing systems at the facility; the processes that are already in place and whether it is undertaken in real time during the patient admission or retrospectively after discharge. The use of a paper form is the simplest method of data collection and arguably the most practical for a newly established registry. The hard copy form is usually completed by the data collector according to an agreed process, and then subsequently entered into a database at a later time. The advantage of this method is that paper is portable; data entry can be undertaken at any place and any time and does not need sophisticated technical input. Disadvantages include that it is difficult to store appropriately and the information is more vulnerable to human error due to the longer journey from source to database. |
| Step 6. Determine data collection personnel. | The personnel who collect data must understand the importance of the task, and prioritise it accordingly. Clinical staff will already have some training and understanding of the information they are required to collect, but may not prioritise the task when they have a competing priority to deliver clinical care to the patient. Non-clinical staff may be able to dedicate themselves to the task more completely, but they will require a greater degree of training to enable them to understand the data properly and perform effectively. The decision on who should collect the data is multifactorial and may depend on the outcome of Steps 4 and 5. |
| Step 7. Decide on reporting requirements. | The Registry will require a suite of reports that will meet its operational and research needs. These reports will enable monitoring of all aspects of trauma service activity at the facility, as well as provide information that drives research. The reporting functionality of a database should be flexible and be able to be generated routinely as well as on an as needs basis. |
| Step 8. Determine database functionality. | Registries require a system that will accept, store and report the data securely. They have a choice whether to acquire a product externally or build a product internally. If the system is built internally it requires a Systems Requirement Specification (SRS) that documents the business needs of the registry and the functionality required to meet those needs. |
| Step 9. Construct the database. | If the facility chooses to build a system internally, the primary reference for the software developers will be the data dictionary, previously referred to in Step 3. The system will be configured to the functionality previously determined in Step 8. |
| Step 10. Create a training program. | When the components of the registry are in place, the pre-determined data collection personnel must understand the purpose of the registry; be committed to the task of data collection and be trained to enter the data accurately and efficiently. A training program should be adjusted to suit the skill level of the participants. |
| Step 11. Create training materials. | Appropriate training materials should be available to data collectors, not only for use during the training program, but to be retained as a ready reference at all times. Training and reference materials include but are not limited to a data collection manual that provides clear instructions as to when, where and how the information is to be entered onto either the paper form or into the database; medical dictionaries, anatomical charts and other information appropriate to the skill level of the trainees. |
| Step 12. Deliver the training to data collectors. | The primary aim of a training program is to ensure that consistent data collection practices are in place and all personnel are cognisant of the agreed process. The format of the training should be appropriate to the environment at the facility and the learning style of the participants. Options for delivery of the training may be in a classroom format to a large group; a focus group format to a small group, or one on one. Once the training has been completed satisfactorily, and management is confident that data collection can commence, the implementation of the registry can be considered to be complete and ongoing operations can begin. |
The initial steps were taken in sequence, with the latter steps taken either contemporaneously or out of sequence, depending on the progress at that time. Each step included a rationale and examples taken from other registries administered by the Alfred and Monash University, particularly the Australian Trauma Registry (ATR), the Victorian State Trauma Registry (VSTR) and the Alfred Health Trauma Registry (AHTR).
Selection of the inclusion and exclusion criteria and Minimum Dataset (MDS)
Initial steps required the selection of inclusion and exclusion criteria and the selection of a Minimum Dataset (MDS). These are critical as the former identifies the target population of interest [11] and the latter specifies the required information, arguably forming the framework of the entire registry.
Our criteria were based on those of the VSTR and designed to include cases that added the most value to the knowledge gained from the registry, and exclude cases that the experience of the VSTR showed added minimal value (Table 2).
Table 2.
STAR inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
|
1. Traumatic injury as reason for acute care and one or more of the following: • Death in the Emergency Department as a consequence of injury. • Inpatient death following injury. • Admission to the Intensive Care Unit. |
1. Traumatic injury NOT the reason for acute care. 2. Any injuries distal to the wrist or ankle, except for amputation of the hand or foot at or proximal to the level of the metacarpals/metatarsals. 3. Length of stay < 3 calendar days apart from death and/or ICU admission. 4. Date of injury > 1 week prior to admission to the first hospital. |
The literature reveals that other trauma registries have selected their MDS using a Delphi technique [12, 13], however our project chose to work with the trauma MDS collated by the Global Alliance for Care of the Injured (GACI). This option was available via the Monash University Accident Research Centre (MUARC), which is a World Health Organisation (WHO) collaborating centre. The MDS was in draft form at that time and has been referenced as such in the resultant KSMC data dictionary.
The final dataset necessarily included some variables that were specific to the KSA, evolving from an initial selection of 67 elements to the final listing of 83 elements. A significant number of these are drawn from those proposed by the WHO GACI working group. Additional File 1 lists each variable, the dictionary reference and dictionary definition.
Site visits
Five site visits by the Alfred/Monash project team were necessary to implement the registry. Both visits included activities that were targeted at taking steps on the plan. The first visit in April 2017 achieved steps one to six. The second visit in August 2017 delivered a two-day training course to the on-site team as per step 12. A training program and materials had been created during the intervening months to complete steps 10 and 11. The course curriculum included presentations on data, registries and injury coding that were considered sufficient for the basic knowledge needed to implement the registry.
At the time of the second visit, all the steps of the 12-point plan had been taken except for step nine, construction of the database. However, this did not preclude the commencement of data collection on paper forms, which began on Wednesday 16th August.
The third, fourth and fifth visits incrementally progressed the implementation of the registry, culminating with User Acceptance Testing (UAT) of the database in March 2018 and the official Saudi TraumA Registry (STAR) launch in April 2018.
Construction of the database
There are guides available to organisations that provide details on technical expectations and standards of clinical registries [14]. However, the decision on which data collection system to adopt is subjective, and depends on the organisation’s needs and resources. The KSMC project team found that the primary differential in the choice of database was whether it was acquired externally, or was a bespoke system that was built internally.
Specifications for the database were prepared by the project team and provided to the KSMC IT Department. No programming code was provided, as this is particular to development of the software and would be unique to the construction.
Once the project team considered the arguments for and against building the database internally, and the IT Department assessed whether they had the technical expertise to do so, the decision was made to proceed. Construction commenced in August 2017.
Timeline
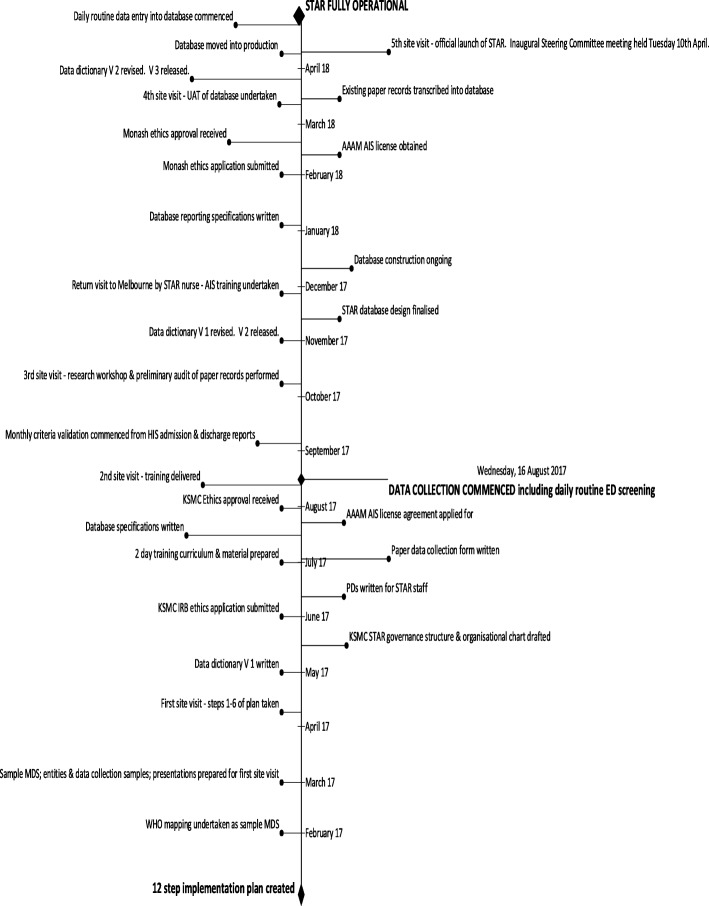
The time taken to implement the KSMC STAR was 16 months, from the commencement of project activities in January 2017 to the move into production of the database in April 2018 (Fig. 1).
Fig. 1.
STAR implementation timeline
STAR operations
The day to day operations of registries differs between organisations according to the registry’s need and purpose. There are valuable recommendations in the literature [15] on the various strategies and methodologies, but as with the choice of data collection system there is no ‘one size fits all’. In the absence of any generic Standard Operating Procedures (SOPs) that would suffice, the STAR has written those necessary at this first site, that will also be applicable at ensuing sites.
An SOP was created for the methodology based on the experience of AHTR and the VSTR, which is that of retrospective data collection of cases that present to hospital and are found to meet inclusion criteria. The daily routine commenced on the 16th August. Cases were backdated to those with dates of injury beginning on the 1st August 2017 and the dataset was documented on paper forms initially. The database was ready for direct data entry in April 2018, after which time the registry was considered to be fully operational.
Results
During the first year of data collection an average of 216 records per month were entered into the STAR database, screened from the approximately 300 cases of potential interest that presented to the KSMC ED. From this monthly average, 175 were confirmed to meet inclusion criteria and progressed to completion of the case. A data quality and cleaning regime was initiated within one month of reporting being available from the database, to immediately ensure prompt monitoring of data integrity. Inbuilt database edits disallowed blank fields, therefore no null values were found. The cleaning regime assessed completeness and quality as the proportion of ‘unknown’ values; and anomalous, or mismatched, values. Each report interrogated the injury event and definitive care variables, and has consistently revealed the variables of concern to be those relevant to the injury event; injury coding and operations coding (Table 3).
Table 3.
Error rates of concerning STAR variables at one month post go live of the database
| n | % unknown | % anomalous/mismatched | % total errors | |
|---|---|---|---|---|
| MRN | 1803 | 0.00 | 0.00 | 0.00 |
| Full name | 1803 | 4.83 | 0.00 | 4.83 |
| DOB | 1803 | 0.00 | 0.50 | 0.50 |
| Age at event | 1803 | 0.00 | 0.22 | 0.22 |
| Gender | 1803 | 0.00 | 0.00 | 0.00 |
| Injury date & time | 1803 | 0.00 | 1.39 | 1.39 |
| Event description | 1803 | 0.00 | 10.43 | 10.43 |
| Cause of injury | 1803 | 0.67 | 14.03 | 14.70 |
| Description if Cause is Other | 9 | 0.00 | 77.78 | 77.78 |
| Injury type | 1803 | 0.06 | 1.55 | 1.61 |
| Description if type is Other | 2 | 0.00 | 0.00 | 0.00 |
| Injury intent | 1803 | 0.44 | 1.11 | 1.55 |
| Place of injury | 1803 | 25.51 | 0.22 | 25.73 |
| Description if Place is Other | 9 | 55.56 | 11.11 | 66.67 |
| Activity at time of injury | 1803 | 49.14 | 0.00 | 49.14 |
| Activity description if Other | 7 | 71.43 | 14.29 | 85.72 |
| ? Traffic event (activates counterpart fiels) | 1803 | 0.00 | 10.65 | 10.65 |
| Traffic counterpart | 726 | 7.71 | 0.14 | 7.85 |
| Geographical location of injury | 1803 | 5.05 | 8.93 | 13.98 |
| AIS codes | 3479 | N/A | 7.70 | 7.70 |
| Operation codes | 891 | N/A | 66.78 | 66.78 |
There was a marked difference between the demographics variables, and the variables of concern, which had higher error rates. The sample size of ‘Descriptions if Cause/Place/Activity is other’ variables was small, however the rate reflects the consistent error of coding the value as ‘Other’, when in fact the value could have been captured in the codeset of the primary variable.
It is not possible to determine at which point newly implemented registries should be achieving a particular standard of data quality and completeness. What is agreed is that data quality should be optimised and that missing data is a known problem [16, 17]. These quality reports have provided insight into the work still needing to be done at any given time.
In addition to ongoing quality reports, a comprehensive audit in October 2018 interrogated approximately 10% of records from the first 12 months of operations. The resulting recommendations addressed the data quality issues and will ensure continuous improvement as the STAR matures.
An inaugural epidemiological report of the first 12 months of data collection has been prepared and was presented at the Saudi Trauma Conference held in Riyadh in February 2019. Ongoing annual reports of calendar years are planned.
Discussion
The challenge facing the project team tasked with implementing a trauma registry at the KSMC was that trauma data had not formally been collected at the site previously, and there was no existing local example of how to do so. Despite this, the STAR has been successfully established at the KSMC and was fully operational eight months ahead of the project deliverable date of December 31st 2018. The 12 step implementation plan that was especially created for the project provided the framework for the process. Each step gave the project team confidence to proceed to the next step or schedule the required tasks accordingly. This process may be useful for other jurisdictions.
Through its partnership with the Monash University Collaborating Centre, the STAR was able to refer to the WHO draft trauma MDS for assistance in selecting its variables. KSMC has made a contribution to the WHO goal of promoting “wider and more standardised collection of data for injury surveillance and trauma care quality improvement.” [18] The education curriculum that was developed to meet the initial training needs of the STAR personnel; the specifications for the construction of the database and the myriad of other tasks that were required have showcased our plan as a project that the WHO can consider to be an example of a case study of good implementation practice. Collaboration will be ongoing as the project continues.
The timeline of the implementation showed the constant tasks required to implement the registry. Some were done by the Alfred-Monash team; some were done by the KSMC; some were done on site in Riyadh and some of them were done off site in Melbourne. The successful completion of each task contributed to the completion of the next and no single task could be achieved in isolation from another.
The project team were required to make a difficult decision on which data collection system would meet the KSMC’s needs. Choosing the option to construct the database on site has proven to be the correct one, as the system is purpose built and amenable to an upgrade that will enable it to accept data from multiple sites, thus meeting the needs of a national registry.
Of local significance is that for the first time the hospital has access to data that will inform process indicators such as time spent in the Emergency Department; rate of trauma team activation; time to operation and length of stay in the Intensive Care Unit. This information alone will assist the KSMC with its goal of achieving verification as a Level 1 Trauma Centre.
Of national significance to the KSA is that the STAR will mature to the point where it can be rolled out across the country, offering robust operating procedures and a functional database. The multi-site experience of the VSTR and the ATR will support the KSMC to be the locus for registry activity elsewhere in the greater Riyadh region and across the Kingdom. Last but not least, neighbouring countries will benefit from the knowledge gained of the implementation process from KSMC.
The literature [19] identifies several features of successful registries including but not limited to organisational support; existence of a steering committee; viable funding options; surety of purpose; committed registry management; training of registry staff; attention to data quality; organised data collection; secure data storage system and flexible reporting options. However, to the best of our knowledge the literature has not described any other step-by-step guide used in the establishment of other trauma registries and indeed O’Reilly et al [20] cited a perception among their study participants that no such guide was available. Our process may therefore be a first, and useful for other jurisdictions.
The STAR registry will enable robust assessment of outcomes and international benchmarking as it accrues increasingly high quality, accurate and accessible data that are available for interrogation and research.
Conclusion
By taking a systematic approach to registry development, the KSMC- The Alfred International trauma Program has implemented a scalable regional trauma registry with robust and rigorous data collection, collation and potential to drive trauma system improvements. The STAR experience demonstrates essential development steps for implementation which will be effective in other regions.
Supplementary information
Additional file 1. STAR Minimum Dataset. Full listing of dictionary data domain; dictionary reference; variable name and dictionary definition
Acknowledgements
The authors wish to acknowledge the members of the STAR Steering Committee for their support, oversight and guidance of the implementation and ongoing operations of the STAR. Further acknowledgement is made of the STAR team for the collection and curation of the data reported in this study.
Abbreviations
- ACSQH
Australian commission on safety and quality in healthcare
- AHTR
Alfred health trauma registry
- ATR
Australian trauma registry
- ED
Emergency department
- GACI
Global alliance for care of the injured
- IT
Information technology
- KSA
Kingdom of Saudi Arabia
- KSMC
King saud medical city
- MDS
Minimum dataset
- MOH
Ministry of health
- MUARC
Monash university accident research centre
- SOP
Standard operating procedure
- STAR
Saudi trauma registry
- UAT
User acceptance testing
- VSTR
Victorian state trauma registry
- VSTS
Victorian state trauma system
- WHO
World Health Organisation
Author’s contributions
JF wrote the majority of the manuscript and described all the operational detail. ASA and SAAA facilitated the development, funding and operations of the STAR onsite thus enabling the study to proceed. PC and MF contributed to the manuscript with comments, edits and additional references. In his position of Chief Executive Officer of the King Saud Medical City (KSMC) and Chair of the Steering Committee, ASA authorised organisational detail contained in the manuscript and referenced as such; enabled ongoing acquisition of data at the site and had final approval of the manuscript. DF contributed to the manuscript with contextual knowledge of the Middle East, comments on population statistics and suggestions for relevant references. All authors are project team members and/or members of the STAR Steering Committee. They all read and approved the final manuscript.
Funding
This study is the Registry component of the King Saud Medical City (KSMC)-The Alfred International Trauma Program, and funded as such by the Ministry of Health, Kingdom of Saudi Arabia. The project funds enabled working groups that implemented the STAR at the site, the convening of the project team and their ongoing operations that include data collection. Under the auspices of the project the authors have collaborated on the analysis and interpretation of the data; and the writing of the manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this article and its supplementary information file.
Ethics approval and consent to participate
This study was approved by the King Saud Medical City Institutional Review Board on July 9th 2017 and registered with the number H-01-R-053. Ethics approval to waive informed consent was requested and granted due to the impracticality of obtaining same from seriously injured patients; the level of their distress at the time; the explanations necessary of the type of information collected and the volume of the patients involved.
Consent for publication
No data relevant to any particular individual is included in this manuscript thus consent for publication was is not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12913-019-4881-8.
References
- 1.Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC, et al. The global burden of injury; incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22(1):3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. Global forum on trauma care. Meeting report. Rio de Janeiro; 2009. 30 p. [accessed 2019 October 31] Available from: https://www.who.int/emergencycare/trauma/global_forum_meeting_report.pdf?ua=1
- 3.World Health Organization. Decade of Action for Road Safety 2011-2020. [accessed 2018 July 10] Available from: http://www.who.int/roadsafety/decade_of_action/en/
- 4.Cameron PA, Gabbe BJ, Cooper DH, Walker T, Judson R, McNeil J. A statewide system of trauma care in Victoria: effect on patient survival. Med J Aust. 2008;189:546–550. doi: 10.5694/j.1326-5377.2008.tb02176.x. [DOI] [PubMed] [Google Scholar]
- 5.Australian Government Department of Foreign Affairs and Trade (DFAT). Saudi Arabia Country/Economic Fact Sheet. [Accessed 2018 July 12]. Available from: http://dfat.gov.au/geo/saudi-arabia/Pages/saudi-arabia.aspx
- 6.Al-Naami MY, Arafah MA, Al-Ibrahim FS. Trauma care systems in Saudi Arabia: an agenda for action. Ann Saudi Med. 2010;30(1):50–58. doi: 10.5144/0256-4947.59374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alghnam S, Alkelya M, Al-Bedah K, Al-Enazi S. Burden of traumatic injuries in Saudi Arabia: lessons from a major trauma registry in Riyadh, Saudi Arabia. Ann Saudi Med. 2014;34(4):291–296. doi: 10.5144/0256-4947.2014.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oxford Business Group. The report. Saudi Arabia 2018. Dubai(UAE): 2017. p. 350 ISBN 978-1-902339-00-9
- 9.King Saud Medical City. About City [Internet]. Riyadh (KSA): 2018. [accessed 2018 June 27]. Available from: https://www.ksmc.med.sa/en/about/pages/default.aspx
- 10.Australian Commission on Safety and Quality in Health Care. Operating principles and technical standards for Australian clinical quality registries. Sydney. 2008. p. 14.
- 11.Hurley SB, Cummings SR, Browner WS, Grady DG, Newman TB. Designing clinical research. 3rd ed. Philadelphia. PA: Lippincott Williams & Wilkins. 2007:29.
- 12.Mohammadi A, Ahmadi M, Gharagozlu A. Developing a minimum data set for an information management system to study traffic accidents in Iran. Iran Red Crescent Med J. 2016;18(3):e23677. doi: 10.5812/ircmj.23677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meidani Z, Mahdian M, Ayan A, Mohammadzade M, Nickfarjam A, Moosavi GA. Registry data coordinator (RDC); a proper accessible strategy for improving road traffic injury (RTI) hospital based trauma registry systems in developing countries and low income countries. ACTA Inform Med. 2018;26(1):35–41. doi: 10.5455/aim.2018.26.35-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Australian Commission on Safety and Quality in Health Care. Framework for Australian clinical quality registries. Sydney. Mar: p. 2014:23.
- 15.Bommakanti K, Feldhaus I, Motwani G, Dicker RA, Juillard C. Trauma registry implementation in low- and middle-income countries: challenges and opportunities. J Surg Res 2018 Mar: 223: 72–86 https://doi.org/10.1016/jss.2017.09.039 [DOI] [PubMed]
- 16.O’Reilly GM, Jolley DJ, Cameron PA, Gabbe B. Missing in action: a case study of the application of methods for dealing with missing data to trauma system benchmarking. Acad Emerg Med. 2010;17(10):1122–1129. doi: 10.1111/j/1553-2712.2010.00887.x. [DOI] [PubMed] [Google Scholar]
- 17.Shivasabesan G, Mitra B, O’Reilly GM. Missing data in trauma registries: a systematic review. Injury [Internet] Mar. 2018;S0020-1383(18):20164–20165. doi: 10.1016/j.injury.2018.03.035. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organisation [internet]. Geneva (CHE): © 2018 WHO: Emergency and trauma care; Global Alliance for Care of the Injured; GACI working groups. [accessed 2018 June 28]. Available from: http://www.who.int/emergencycare/gaci/activities/en/
- 19.Mandavia R, Knight A, Phillips J, Mossialos E, Littlejohns P, Schilder A. What are the essential features of a successful surgical registry? A Syst Rev BMJ Open. 2017;7:e017373. doi: 10.1136/bmjopen-2017-017373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Reilly GM, Gabbe B, Braaf S, Cameron PA. An interview of trauma registry custodians to determine lessons learnt. Injury, Int. J. Care Injured. 2016;47:116–124. doi: 10.1016/j.injury.2015.06.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. STAR Minimum Dataset. Full listing of dictionary data domain; dictionary reference; variable name and dictionary definition
Data Availability Statement
All data generated or analysed during this study are included in this article and its supplementary information file.