Abstract
Background
Malaria is one of the top-five contributors to under-5 deaths in Myanmar. Use of insecticide-treated nets (ITN) and receiving early appropriate care in case of fever are the core interventions to prevent malaria and its complications and thereby deaths. This study aimed to assess among the under-five children, (a) utilization of ITNs and its associated factors, (b) care-seeking behaviour among their caregivers and its associated factors and uptake of malaria testing among those with fever in the last 2 weeks.
Methods
This was a cross sectional study using secondary analysis of Myanmar Demographic and Health Survey (MDHS) conducted in 2015–2016. Multivariable logistic regression was used to explore the factors associated with non-utilization of ITNs and not seeking care for fever. Effect sizes have been presented using odds ratios with 95% confidence intervals. Data analysis was done using svyset command in STATA to account for the multi-stage sampling design of the survey.
Results
Of 4597 alive under-five children, 80.5% did not sleep under an ITN last night. The factors significantly associated with non-utilization of ITNs were residing in malaria elimination regions (aOR = 2.0, 1.3–3.2), urban residence (aOR = 1.8, 1.2–2.9), staying in delta region (aOR = 8.7, 4.7–12.2), hilly region (aOR = 3.0, 2.0–4.6, and having highest wealth quintile (aOR = 1.8, 1.1–3.0). Around 16% had fever in the last 2 weeks, of whom 66.7% sought care for fever and 3% got tested for malaria. Nearly half (50.9%) of the caregivers sought care from a government health facility, followed by private hospital/doctor (27.8%), shop (8.0%), village health worker (4.4%) and pharmacy (3.1%). The factors associated with not seeking care for fever were residing in specific geographical locations (hilly, delta and central plains compared to coastal region) and having lowest wealth quintile (aOR = 2.3, 1.1–5.7).
Conclusions
This study highlighted that ownership and utilization of ITNs was very poor among under-5children. Care-seeking behaviour of the caregivers of under-5 children in case of fever was dismal with two-thirds not seeking care. The programme should seriously consider addressing these barriers if Myanmar is to achieve zero malaria deaths by 2030.
Keywords: Insecticide treated net, Under-five children, Health care seeking, Demographic and Health Survey, SORT IT, Myanmar
Background
Globally, malaria is still an important public health problem with 219 million cases and 435,000 malaria-related deaths worldwide in 2017 [1]. Malaria remains a major killer of under-fives, claiming the life of one child every 2 min. It is the one of the ten leading causes of under-five mortality globally [2].
Under-5 malaria deaths have to be tackled through already known effective preventive and curative interventions. One of the core interventions recommended by the World Health Organization (WHO) to reduce under-5 deaths is sleeping under a bed net. Bed nets are broadly of two types: untreated and treated, which are referred to as insecticide-treated net (ITN)/long-lasting insecticidal net (LLIN), hereafter referred to as ITN [3]. Bed nets treated with an insecticide are much more protective than untreated nets. These insecticides kill mosquitoes as well as other insects. They also repel mosquitoes reducing the number that enter the house. National malaria control programmes across the globe distribute ITNs free of cost to improve ownership and utilization of ITNs. Bed nets have been shown to reduce under-five mortality by 18.8% in Ghana [4] and by 55% in combination with indoor residual spraying [5]. However, poor utilization of ITNs is a major concern, as reported in several studies from Africa [6, 7].
Myanmar has a high burden of malaria with more than two-third of its population at risk of malaria [8]. Malaria is endemic in 291 out of 330 townships in the country. It is also one of the countries in the Greater Mekong Sub-region (GMS) with evidence of artemisinin resistance [9]. However, the National Malaria Control Programme (NMCP) is committed to eliminate malaria from the entire country by 2030 [10].
Under-five children are the most vulnerable group affected by malaria. Malaria is one of the major causes of under-5 death in the country, after prematurity, low birth weight and acute respiratory tract infections [11]. In order to tackle malaria deaths, utilization of ITNs/LLINs in areas of high malaria transmission is one of the key preventive interventions for malaria elimination in Myanmar in all age groups including under-5 children.
Myanmar aims at achieving and maintaining 100% access and utilization of ITNs at the household level. Previous studies from Myanmar have assessed ownership and utilization of ITNs in the general population [12], in specific regions/settings [13, 14] and key migrant occupations such as plantation workers [15, 16]. However, information on ITN usage among under-five children and the associated factors is scarce.
Besides ITN use, the WHO has also emphasized early diagnosis and prompt treatment within 24 h of onset of symptoms to decrease risk of severe complications and death due to malaria [17]. Malaria testing and treatment facilities are available at all public health facilities and at the community level with the village health volunteers in Myanmar and are offered free of cost. Despite this, timely testing and early diagnosis of malaria remains a concern in Myanmar and globally. This requires an understanding of the health-seeking behaviour in case of fever. Previous studies in Myanmar have explored treatment-seeking behaviour of persons with fever in the general population [18] and amongst migrant workers [19, 20]. There is little information regarding care-seeking for fever and uptake of malaria testing services among caregivers of under-five children in Myanmar and its associated factors. A study regarding the treatment-seeking behaviour of caregivers of under-five children in Myanmar was done in a single township, which cannot be generalized to represent the whole country [21].
The first Myanmar Demographic and Health Survey (MDHS) was implemented by the Ministry of Health and Sports (MOHS) in 2015–2016. This nation-wide survey collected useful information on utilization of ITNs and health-seeking behaviour in case of fever [22]. The survey also collected socio-demographic and geographical information about the respondents. These factors could be associated with ITN use and care-seeking behaviour, though the survey did not report these associations. To fill the gaps in literature in Myanmar as mentioned earlier, the present study analyzed the DHS dataset to assess among the under-five children: i. utilization of ITNs and its associated socio-demographic and geographical factors, ii. care-seeking behaviour (number and proportion who sought care for fever and type of first provider sought) and its associated socio-demographic and demographic factors, and iii. uptake of malaria testing among those with fever in the last 2 weeks.
Methods
Setting
Myanmar is a south-east Asian country inhabited by 51 million people, 70% residing in rural areas. It is divided into seven states, seven regions and one capital territory (Nay Pyi Taw Council territory) which are further subdivided into 74 districts with 330 townships [8]. The terrain, sub-tropical climate, precipitation and vegetation favours mosquito breeding and malaria transmission.
Study design
This study analysed secondary data from the MDHS 2015–2016, which is a cross-sectional survey. The details about the survey and its methodology are described below in brief.
Myanmar 2015–2016 Demographic and Health Survey (DHS)
The Myanmar DHS is a nationally representative survey of women and men aged 15–49 years to assess the population and health status of adults of reproductive age and their children under 5 years. This is part of the worldwide DHS Program which is funded by the United States as well as many other donors. The 2015–2016 survey is the first DHS ever conducted in Myanmar, and was supported by United States Agency for International Development and the Three Millennium Development Goal (3MDG) Fund.
Sample and sampling technique
The DHS sample has characteristics similar to that of the general population as it covered all states/regions in the country. A master sampling frame was created based on the 2014 census which consisted of 4000 Primary Sampling Units (PSUs) drawn from the entire census frame. Each PSU is either a census enumeration area (EA) or ward in urban areas or village tract in rural areas. The survey followed a stratified two-stage sample design and was intended to allow estimates of key indicators at the national level, in urban and rural areas, and for each of the seven states and eight regions of Myanmar. Stratification was achieved by separating each state or region (n = 15) into urban and rural areas, each of which formed a separate sampling stratum. In total, 30 sampling strata (15*2) were created. The first stage involved selecting clusters/PSUs from these strata. A total of 442 clusters (123 urban and 319 rural) were selected from the master sample (Fig. 1). At the second stage, a fixed number of 30 households was selected from each of the selected clusters (a total of 13,260 households), using equal probability systematic sampling. The response rate was 98%.
Fig. 1.

Map showing the clusters covered under the Myanmar Demographic and Health Survey, 2015–2016
All women aged 15–49 years who were either permanent residents of the selected households or visitors who stayed in the households the night before the survey were eligible for interview. In the survey, questions related to under-5 children in the household about the ownership and utilization of ITNs and health-seeking behaviour (in case of fever) were asked to the female respondent in the family.
Data variables
The key outcome variables included in this study were not sleeping under ITN the last night prior to the survey, not seeking care for fever, first place where care was sought for fever and whether tested for malaria. Other socio-demographic characteristics included the caregiver’s (women aged 15–49 years) age, education and occupation, father’s education and occupation, household characteristics, place of residence and region (See Table 1).
Table 1.
List of variables, variable labels, field type and their categories extracted from the Demographic and Health Survey Myanmar, 2015–2016
| Variable name | Variable label | Field type | Value labels |
|---|---|---|---|
| Respsex | Respondent’s sex | Integer |
Female Male Not recorded |
| Respage | Respondent’s age | Integer | |
| Childsex | Sex of under-five children | Integer |
Female Male |
| Childage | Children’s age in completed months | Integer | |
| Wealthindex | Wealth index of household | Integer |
Poorest Poor Middle Richer Richest |
| Occumom | Occupation of mother | I |
Dependent Casual Staff Migrant Own |
| Occudata | Occupation of father | I |
Dependent Casual Staff Migrant Own Unknown |
| Edumom | Education of mother | Integer |
Literacy Primary Middle Higher Graduated Not recorded |
| Edudad | Education of father | Integer |
Literacy Primary Middle Higher Graduated |
| Region | Region where for interviewed HH | Interger |
Kachin Kayah Kayin Chin Mon Delta Rakhine Shan Yangon Mandalay Sagaing Magway Bago Thanitarry NayPyiTaw territory |
| Resid | Place residence of HH | I |
Rural Urban |
| Hhmember | Number of HH member | I | |
| Numu5 | Number of Under 5 children | I | |
| Sleepu5 | Number of U5 children slept under INT | I |
Yes No |
| Hhitn | HH possess ITN | I |
Yes No |
| Feveru5 | Number of U5 Child had fever within 2 weeks | I | |
| U5seek | Number of U5 children with fever taken to health facility or health care provider | I |
Operational definitions
The care-seeking for fever among under-5 children means seeking advice or treatment from a health provider, a health facility or a pharmacy. This definition is according to the survey guidelines.
An ITN is defined as 1. A factory-treated net that does not require any further treatment (long-lasting insecticidal net, or LLIN) or 2. A pretreated net obtained within the past 12 months or 3. A net that has been soaked with insecticide within the past 12 months.
Data analysis
Myanmar DHS Data set (Stata file) was analysed using STATA version 15.0. The children (KR) data set from DHS data set was used and a subset of the data related to alive under-5 children was extracted for this study. Key indicators such as ITN utilization and treatment-seeking behaviour for fever within last 2 weeks among under-five children have been presented in the form of proportions (95% confidence intervals). To describe the factors associated with non-utilization of ITN and not seeking care for fever, logistic regression was run and effect sizes have been presented using odds ratios with 95% confidence intervals and p-values. A p value less than < 0.05 was considered as significant. The analysis was weighted for the multi-stage sampling design and hence, weighted estimates have been provided. “Svyset” command was used in STATA to account for sampling weights, clustering and stratification in the KR dataset.
Ethics
Ethical approval for this study was obtained from Ethics Review Committee of the Department of Medical Research, Ministry of Health and Sports, Myanmar (Ethic/DMR/2018/164) and The Union Ethics Advisory Group, Paris, France (EAG number: 40/18). Permission to use the DHS data was obtained from the DHS program and the Department of Public Health, Ministry of Health and Sports, Myanmar. This being a secondary data analysis of DHS database, a waiver of informed consent was granted by the ethics committees.
Results
Socio-demographic and household characteristics
Of 4815 underweight children who were part of the MDHS, 4597 (95.5%) eligible (alive) children were included in this study. There were no missing data in these children who were part of this study. Of 4597 under-five children, half were males (52%, 2402), predominantly rural residents (77.4%, N = 3617), nearly 40.4% (n = 1842) belonged to 3–5 years age group with almost an equal number in the 1–2 years age group. Around half of the caregivers (45.8%, n = 2034) were educated up to primary level and 55.7% (n = 2425) were working (Table 2).
Table 2.
Socio-demographic, geographic and household characteristics of under-five children included in Myanmar Demographic and Health Survey, 2015–2016 (N = 4597)
| Characteristics | Unweighted count | Weighted % | |
|---|---|---|---|
| Total | N = 4597 | (%) | (95% CI) |
| Age of the child (in months) | |||
| < 12 | 940 | (19.6) | (18.3–21.0) |
| 12–35 | 1815 | (39.8) | (38.3–41.4) |
| 36–59 | 1842 | (40.4) | (38.8–42.0) |
| Sex of the child | |||
| Male | 2402 | (52.0) | (50.0–53.8) |
| Female | 2195 | (48.0) | (46.1–49.9) |
| Age of the caregiver (in years) | |||
| 15–24 | 865 | (19.0) | (17.4–20.8) |
| 25–34 | 2368 | (52.1) | (50.0–54.1) |
| ≥ 35 | 1364 | (28.7) | (27.0–30.5) |
| Education of the caregiver | |||
| No formal education | 802 | (17.8) | (15.1–20.7) |
| Primary | 2034 | (45.8) | (43.2–48.4) |
| Secondary | 1440 | (28.6) | (26.4–31.0) |
| More than secondary | 321 | (7.6) | (6.5–8.9) |
| Father’s education | |||
| No education | 792 | (17.7) | (15.2–20.5) |
| Primary | 1797 | (40.4) | (38.0–42.9) |
| Secondary | 1664 | (34.3) | (31.9–36.9) |
| More than secondary | 253 | (5.5) | (4.7–6.9) |
| Don’t know | 89 | (1.7) | (1.2–2.2) |
| Occupation of the caregiver | |||
| Working | 2425 | (55.7) | (53.1–58.3) |
| Not-working | 2170 | (44.2) | (41.6–46.8) |
| Father’s occupation | |||
| Manual worker | 2599 | (57.5) | (54.2–60.7) |
| Agricultural | 1280 | (26.3) | (23.0–29.9) |
| Others | 718 | (16.1) | (14.1–18.4) |
| No of household members | |||
| 1–3 | 450 | (11.0) | (9.7–12.5) |
| 4–6 | 2606 | (58.7) | (56.4–60.9) |
| 7–10 | 1335 | (26.4) | (24.4–28.4) |
| More than 10 | 206 | (3.8) | (2.9–4.9) |
| Wealth index | |||
| Lowest | 1383 | (29.5) | (26.7–32.5) |
| Second | 1043 | (22.1) | (20.3–24.0) |
| Middle | 826 | (16.8) | (15.2–18.6) |
| Fourth | 775 | (17.0) | (15.2–19.0) |
| Highest | 570 | (14.4) | (12.5–16.5) |
| Region | |||
| Malaria elimination regions | 1497 | (42.0) | (39.5–44.6) |
| Other regions | 3100 | (57.9) | (55.3–60.4) |
| Geographical location | |||
| Hilly | 1810 | (23.3) | (21.2–25.6) |
| Coastal | 895 | (13.6) | (11.9–15.4) |
| Delta | 810 | (32.3) | (29.8–34.8) |
| Central plains | 1082 | (30.6) | (28.3–33.1) |
| Place of residence | |||
| Urban | 980 | (22.5) | (20.5–24.7) |
| Rural | 3617 | (77.4) | (75.3–79.4) |
Figures given in parentheses are weighted percentages
CI Confidence intervals
Factors associated with non-utilization of ITN
In 2015–2016, almost all households (97%) in Myanmar had at least one mosquito net (treated or untreated), but only 27% had at least one ITN (data not tabulated). Overall, 80.5% under-fives did not sleep under an ITN last night. In the adjusted analysis, malaria elimination regions (aOR = 2.0, 1.3–3.2, p-value = 0.003), urban residence (aOR = 1.8, 1.2–2.9, p-value = 0.006), residing in delta region (aOR = 8.7, 4.7–12.2, p-value < 0.001), hilly region (aOR = 3.0, 2.0–4.6, p-value < 0.001),and highest wealth quintile (aOR = 1.8, 1.1–3.0, p-value = 0.01) were significantly associated with non-utilization of ITNs (Table 3).
Table 3.
Socio-demographic, geographic and household characteristics associated with non-utilization of ITNs among under-five children in Myanmar Demographic and Health Survey, 2015–16 (N = 4597)
| Characteristics | Total | ITN non-utilization N (%) | Unadjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value |
|---|---|---|---|---|---|---|
| Total | 4597 | 3328 (80) | ||||
| Age of the child (in months) | 0.07 | |||||
| 36–59 | 1842 | 1355 (81) | 1 | 1 | ||
| 12–35 | 1815 | 1320 (81) | 1.0 (0.8–1.2) | 1.0 (0.8–1.2) | 0.9 | |
| <12 | 940 | 653 (79) | 0.9 (0.8–1.12) | 0.9 (0.8–1.2) | 0.5 | |
| Sex of the child | 0.6 | |||||
| Male | 2402 | 1731 (80) | 1 | |||
| Female | 2195 | 1597 (81) | 1.0 (0.9–1.2) | |||
| Age of caregiver (in years) | 0.8 | |||||
| 15–24 | 865 | 632 (81) | 1 | |||
| 25–34 | 2368 | 1715 (81) | 1.0 (0.7–1.3) | |||
| ≥35 | 1364 | 981 (80) | 0.9 (0.7–1.2) | |||
| Education of the caregiver | < 0.001 | |||||
| No formal education | 802 | 539 (72) | 1 | 1 | ||
| Primary | 2034 | 1454 (80) | 1.6 (1.1–2.3) | 1.0 (0.7–1.4) | 0.8 | |
| Secondary | 1440 | 1058 (84) | 2.0 (1.4–3.0) | 1.0 (0.7–1.5) | 0.9 | |
| More than secondary | 321 | 277 (91) | 3.9 (2.2–7.2) | 1.3 (0.6–2.6) | 0.5 | |
| Father’s education | < 0.001 | |||||
| No education | 792 | 532 (72) | 1 | 1 | ||
| Primary | 1797 | 1310 (82) | 1.7 (1.2–2.5) | 1.2 (0.8–1.7) | 0.3 | |
| Secondary | 1664 | 1208 (82) | 1.8 (1.2–2.6) | 0.9 (0.6–1.3) | 0.5 | |
| More than secondary | 253 | 212 (88) | 2.9 (1.6–5.2) | 0.8 (0.4–1.7) | 0.6 | |
| Occupation of the caregiver | 0.03 | |||||
| Not-working | 2170 | 1538 (80) | 1 | 1 | ||
| Working | 2425 | 1788 (81) | 1.1 (0.9–1.4) | 0.9 (0.7–1.2) | 0.7 | |
| Father’s occupation | 0.001 | |||||
| Manual worker | 2599 | 1892 (81) | 1 | 1 | ||
| Agricultural | 1280 | 886 (77) | 0.8 (0.6–1.0) | 0.8 (0.6–1.1) | 0.1 | |
| Others | 718 | 550 (83) | 1.2 (0.8–1.6) | 0.7 (0.5–1.1) | 0.09 | |
| Number of household members | 0.07 | |||||
| 1–3 | 450 | 344 (84) | 1 | 1 | ||
| 4–6 | 2606 | 1897 (81) | 0.8 (0.6–1.2) | 1.0 (0.7–1.5) | 0.8 | |
| 7–10 | 1335 | 938 (78) | 0.7 (0.5–1.0) | 1.1 (0.7–1.6) | 0.7 | |
| More than 10 | 206 | 149 (78) | 0.7 (0.4–1.3) | 1.0 (0.5–2.2) | 0.9 | |
| Wealth index | 4,597 | < 0.001 | ||||
| Lowest | 1383 | 928 (74) | 1 | 1 | ||
| Second | 1043 | 722 (77) | 1.2 (0.9–1.6) | 1.1 (0.8–1.4) | 0.7 | |
| Middle | 826 | 573 (81) | 1.5 (1.1–2.2) | 1.3 (0.9–1.8) | 0.2 | |
| Fourth | 775 | 616 (87) | 2.4 (1.6–3.5) | 1.8 (1.1–2.7) | 0.01 | |
| Highest | 570 | 489 (91) | 3.4 (2.2–5.3) | 1.8 (1.0–3.3) | 0.06 | |
| Region | < 0.001 | |||||
| Other regions | 3100 | 2025 (73) | 1 | 1 | ||
| Malaria elimination regions | 1497 | 1303 (90) | 3.4 (2.4–4.8) | 2.0 (1.3–3.2) | 0.003 | |
| Geographical location | < 0.001 | |||||
| Coastal | 895 | 459 (51) | 1 | 1 | ||
| Hilly | 1810 | 1174 (73) | 2.6 (1.7–4.0) | 3.0 (2.0–4.6) | < 0.001 | |
| Delta | 810 | 764 (94) | 14.9 (8.6–25.8) | 12.7 (7.7–21.2) | < 0.001 | |
| Central plains | 1082 | 931 (85) | 5.3 (3.1–9.2) | 4.0 (2.3–7.3) | < 0.001 | |
| Place of residence | < 0.001 | |||||
| Rural | 3617 | 2489 (77) | 1 | 1 | ||
| Urban | 980 | 839 (91) | 3.1 (2.2– 4.6) | 1.8 (1.2–2.9) | 0.006 |
Figures presented here are weighted estimates
ITN insecticide treated net, CI Confidence Interval
Care-seeking for under-five children with a fever and factors associated with not seeking care
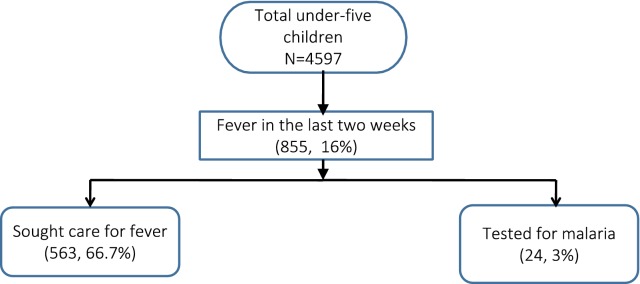
Of 4597 under-five children, 16% (n = 855) had fever in the last 2 weeks, of whom 66.7% (n = 563) sought care for fever and 3% (n = 24) got tested for malaria (Fig. 2).
Fig. 2.
Fever among under-five children and uptake of care and testing services for fever among their caregivers in Myanmar Demographic and Health Survey, 2015–2016
Overall, 33.3% did not seek care for fever at all in the last 2 weeks. In the adjusted analysis, geographical location (hilly, delta and central plains compared to coastal region) and lowest wealth quintile (aOR = 2.3, 1.1–5.7, p-value = 0.03), were significantly associated with not seeking care for fever (Table 4).
Table 4.
Socio-demographic, geographic and household characteristics associated with non-seeking of care among caregivers of under-five children who had fever last 2 weeks in Myanmar Demographic and Health Survey, 2015–2016 (N = 855)
| Characteristics | Total | Non-seeking of care N (%) | Unadjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value |
|---|---|---|---|---|---|---|
| Total | 855 | 292 (33) | ||||
| Age of the child (in months) | 0.1 | |||||
| 36–59 | 268 | 127 (35) | 1 | 1 | ||
| 12-35 | 411 | 64 (32) | 0.9 (0.6–1.4) | 0.9 (0.6–1.4) | 0.6 | |
| <12 | 176 | 101 (35) | 1.0 (0.6–1.7) | 1.1 (0.6–1.9) | 0.8 | |
| Sex of the child | 0.8 | |||||
| Male | 440 | 152 (34) | 1 | |||
| Female | 415 | 140 (32) | 0.9 (0.7–1.3) | |||
| Age of caregiver (in years) | 0.9 | |||||
| 15–24 | 178 | 58 (40 ) | 1 | |||
| 25–34 | 428 | 148 (31) | 0.7 (0.4–1.2) | |||
| ≥35 | 249 | 86 (31) | 0.6 (0.4–1.2) | |||
| Education of caregiver | 0.1 | |||||
| No education | 149 | 54 (32) | 1 | 1 | ||
| Primary | 385 | 141 (36) | 1.2 (0.6–2.3) | 1.1 (0.6–2.0) | 0.8 | |
| Secondary | 275 | 88 (33) | 1.1 (0.5–2.1) | 1.2 (0.6–2.6) | 0.6 | |
| More than secondary | 46 | 9 (18) | 0.5 (0.1–1.3) | 0.7 (0.2–2.1) | 0.5 | |
| Father’s education | 0.61 | |||||
| No education | 134 | 45 (29) | 1 | |||
| Primary | 357 | 127 (37) | 1.5 (0.8–2.7) | |||
| Secondary | 309 | 100 (30) | 1.0 (0.5–2.0) | |||
| More than secondary | 35 | 9 (25) | 0.8 (0.3–2.5) | |||
| Occupation of caregiver | 0.07 | |||||
| Not Working | 372 | 115 (30) | 1 | 1 | ||
| Working | 481 | 177 (36) | 1.3 (0.9–1.9) | 1.2 (0.8–1.7) | 0.8 | |
| Father’s occupation | < 0.001 | |||||
| Manual worker | 477 | 131 (32) | 1 | 1 | ||
| Agricultural | 266 | 125 (39) | 1.4 (0.9–2.2) | 1.2 (0.8–1.9) | 0.4 | |
| Others | 112 | 36 (29) | 0.9 (0.5–1.6) | 1.1 (0.5–2.2) | 0.8 | |
| No of household members | 0.7 | |||||
| 1–3 | 67 | 19 (30) | 1 | |||
| 4–6 | 466 | 159 (32) | 1.1 (0.6–2.2) | |||
| 7–10 | 271 | 96 (35) | 1.3 (0.6–2.5) | |||
| More than 10 | 51 | 18 (41) | 1.7 (0.6–4.7) | |||
| Wealth index | < 0.001 | |||||
| Highest | 86 | 19 (23) | 1 | 1 | ||
| Fourth | 137 | 29 (23) | 1.0 (0.5–1.9) | 0.9 (0.4–1.8) | 0.7 | |
| Middle | 128 | 50 (42) | 2.3 (1.1–5.1) | 2.3 (1.0–5.1) | 0.04 | |
| Second | 226 | 87 (34) | 1.7 (0.8–3.6) | 1.7 (0.7–3.9) | 0.2 | |
| Lowest | 278 | 107 (38) | 2.0 (0.9–4.1) | 2.3 (0.9–5.7) | 0.08 | |
| Region | 0.6 | |||||
| Other regions | 654 | 220 (32) | 1 | |||
| Malaria elimination region | 201 | 72 (37) | 1.2 (0.8–2.0) | |||
| Geographical location | < 0.001 | |||||
| Coastal | 169 | 31 (18) | 1 | 1 | ||
| Hilly | 403 | 158 (37) | 2.7 (1.4–4.9) | 2.8 (1.5–5.3) | 0.002 | |
| Delta | 144 | 50 (34) | 2.3 (1.2-4.4) | 2.3 (1.–4.6) | 0.01 | |
| Central plains | 139 | 53 (38) | 2.8 (1.4–5.3) | 3.1 (1.5–6.2) | 0.002 | |
| Place of residence | 0.3 | |||||
| Rural | 683 | 239 (33) | 1 | |||
| Urban | 172 | 53 (34) | 1.1 (0.6–1.8) |
Figures presented here are weighted estimates
CI = Confidence Interval
First treatment-seeking source for fever
Around half (50.9%) of the caregivers sought care from a government health facility, followed by private hospital/doctor (27.8%), shop (8.0%), village health worker (4.4%) and pharmacy (3.1%) (Fig. 3).
Fig. 3.
Type of first care provider sought by caregivers of under-five children with fever in the Myanmar Demographic and Health Survey, 2015–2016 (n = 563)
Discussion
This is the first nationally representative study from Myanmar reporting care-seeking behaviour for fever and ITN utilization among the vulnerable under-five population. The study had some interesting findings.
This study finding highlighted that only less than one-fifth of under-five children slept under an ITN the night prior to the survey. This is probably due to poor ownership of ITNs which is also reported in previous studies from Myanmar [12, 15]. This calls for mass distribution of ITNs with emphasis on households with under five children to improve ownership of ITNs. Household mapping which is done before distribution of ITNs should be meticulously planned especially while doing a head count in households with under five children.
Previous studies in African countries have reported higher utilization of ITNs among children ranging from 42 to 51% [7, 23]. Studies from Myanmar have also reported higher ITN utilization of 45–50% among the migrant population and the Regional Artemisinin Resistance Initiative areas of Myanmar, probably due to the increased focus of the programme through heightened routine activities and increased external funding in these high risk areas [24, 25]. Reasons for poor ITN utilization among caregivers of under-five children in this study need to be explored through qualitative research.
This study demonstrated higher utilization rates for ITN among rural children than their urban counterparts similar to previous studies [26]. This was contrary to what was found in a meta-analysis of 13 surveys, which included five Demographic Health Surveys for African countries, where children in urban households were found to be more likely to use nets than children in rural households [27]. One possible reason for this could be the low incidence of malaria in urban areas such as Yangon and Mandalay which are moving towards malaria elimination. This leads to low perceived threat of mosquito bite and probably also explains the poor ITN utilization in malaria elimination regions. However, the exact reasons require an in-depth qualitative exploration.
Low ITN use has been reported in the delta and hilly regions. This is concerning for the programme as these are high malaria transmission regions. The reasons are beyond the scope of this study, warranting further qualitative studies.
Among the caregivers of under-five children with a fever, only two-third sought care. This figure is much lower than the 100% defined by the Myanmar National Malaria Control Programme [28]. This finding is alarming, given that malaria is a major cause of fever in children in Myanmar and prompt care-seeking is necessary to reduce morbidity and mortality. It suggests the need for intensified social and behaviour change communication strategies to improve care-seeking efforts. The results are similar to what was reported in previous studies from Senegal and Mozambique, in which around one-third of children with fever did not receive any treatment or medical advice [29, 30].
However, previous studies from Myanmar have reported higher proportion (~ 80%) of children with fever receiving care, possibly because these studies were conducted in specific groups of populations such as the migrants, ethnic minority groups and malaria endemic rural areas which are high priority areas for the national malaria programme and receives maximum attention and resource allocation. Also, the definition used to define care-seeking varied across studies [21, 31, 32].
Respondents residing in the hilly areas have reported poor care-seeking probably due to the difficult terrain, thus creating access barriers to seeking care. The role of village level volunteers is crucial in these areas to provide doorstep decentralized services.
This study showed poor care-seeking among caregivers of under-five children belonging to the lowest socio-economic status. This has been reported by several studies from low-middle income countries [33–35]. These findings are also consistent with studies focusing on other childhood illnesses, such as diarrhoea and ARI in similar settings [36, 37]. Concerns about payment for consultation remain a barrier to seeking health care and achieving better health outcomes for the poor.
The proportion of children with fever getting tested for malaria was dismally low with only 3%. Similar concerns were also raised in previous studies among migrants and the general population in Myanmar which reported lower uptake of malaria testing (12–24%) [18, 32]. Several patient (self-medication, not giving due importance to fever, transportation difficulty, uninformed about malaria testing by VHV) and provider (lack of test kits, testing only seriously ill patients) related factors were identified in a qualitative study done previously to explain poor uptake of malaria testing [32]. These factors need to be tackled as part of a comprehensive strategy to improve the knowledge and practice of caregivers related to malaria, especially the need for testing within 24 h of fever. Malaria being a major killer among under-fives, appropriate management of fever among children should be a national programme priority to achieve zero malaria deaths.
The major strengths of the study were that the data were obtained from a large nationally representative survey covering all the states/regions of Myanmar; the survey followed a standard DHS methodology; the response rate was high; missing values were minimum; and the subject is an identified national and global research priority. The study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for the reporting of observational studies.
The study had few limitations. The study did not explore reasons for poor health-seeking behaviour in case of fever and poor utilization of ITNs which require qualitative studies in future. Also, the study did not explore other personal and behavioural factors such as knowledge, attitude, beliefs and perception regarding the role of ITN and health care-seeking which are known to influence behaviours. The responses were self-reported which could be influenced by social desirability bias, although, wherever possible, observation of self-reported ITNs and ITNs mounted over the sleeping area was done during the interview.
Conclusion
This study highlighted poor ownership and utilization of ITNs among the under five children. Nearly one-third of the caregivers of under-five children did not seek care for fever which has implications on childhood morbidity and mortality. The programme should seriously consider addressing these barriers if Myanmar is to achieve zero malaria deaths by 2030. Continuous and strengthened community awareness campaigns in various forums such as immunization/antenatal sessions, under five clinics, and other community gatherings is needed to bring about appropriate change in behaviour.
Acknowledgements
We would like to thank the DHS Program Demographic and Health Surveys for sharing and the Department of Public Health giving permission to use the dataset used in this study. This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR). The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union) and Medécins sans Frontières (MSF/Doctors Without Borders). The specific SORT IT program which resulted in this publication was jointly organized and implemented by The Centre for Operational Research, The Union, Paris, France; The Department of Medical Research, Ministry of Health and Sports, Myanmar; The Department of Public Health, Ministry of Health and Sports, Myanmar; The Union Country Office, Mandalay, Myanmar; The Union South-East Asia Office, New Delhi, India; and London School of Hygiene and Tropical Medicine, London, UK.
Abbreviations
- 3MDG
three millennium development goals fund
- DMR
Department of Medical Research
- DHS
Demographic and Health Survey
- RHC
rural health centre
- UHC
urban health centre
- MOHS
Ministry of Health and Sports
- FGD
focus group discussion
- BHS
basic health staff
- GMS
greater Mekong subregion
- ITN
insecticide-treated bed net
- LLIN
long-lasting insecticidal net
- RDT
rapid diagnostic test
- NMCP
National malaria control programme
- RAI
regional artemisinin initiative
- WHO
World Health Organization
Authors’ contributions
KTM, TMM, JPT and MMO were involved in conception and design of the study, data cleaning and analysis, interpretation of findings and drafting of the manuscript. TO, ZL and AT were involved in interpretation of results and critical review of the manuscript. All the authors approved the final version of the manuscript. All authors read and approved the final manuscript.
Funding
The training programme, within which this paper was developed, was funded by the Department for International Development (DFID), UK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The open access publications costs were funded by the Department for International Development (DFID), UK and La Fondation Veuve Emile Metz-Tesch (Luxembourg).
Availability of data and materials
Data are not available in public domain because they are currently being analyzed in related papers. However, data are available with the corresponding author (KTM) and will be made accessible on reasonable request at the following e-mail: drktmin@gmial.com.
Ethics approval and consent to participate
Ethical approval for this study was obtained from Ethics Review Committee of the Department of Medical Research, Ministry of Health and Sports, Myanmar and The Union Ethics Advisory Group, Paris, France. This being a secondary data analysis of DHS database, a waiver of informed consent was granted by the ethics committees. De-identified data related to study objectives were extracted from the survey dataset to ensure data confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. World Malaria Report 2017. Geneva: World Health Organization; 2017.
- 2.WHO. Causes of death among children. Geneva: World Health Organization; 2018. http://www.who.int/maternal_child_adolescent/data/causes-death-children/en/.
- 3.WHO. Aframework for malaria elimination. Geneva: World Health Organization: 2017.
- 4.Afoakwah C, Nunoo J, Andoh FK. Effect of insecticide-treated bed net usage on under-five mortality in northern Ghana. Malar J. 2015;14:309. doi: 10.1186/s12936-015-0827-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eisele TP, Larsen D, Steketee RW. Protective efficacy of interventions for preventing malaria mortality in children in Plasmodium falciparum endemic areas. Int J Epidemiol. 2010;39(Suppl 1):i88–i101. doi: 10.1093/ije/dyq026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diabaté S, Druetz T, Bonnet E, Kouanda S, Ridde V, Haddad S. Insecticide-treated nets ownership and utilization among under-five children following the 2010 mass distribution in Burkina Faso. Malar J. 2014;13:353. doi: 10.1186/1475-2875-13-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wanzira H, Yeka A, Kigozi R, Rubahika D, Nasr S, Sserwanga A, et al. Long-lasting insecticide-treated bed net ownership and use among children under five years of age following a targeted distribution in central Uganda. Malar J. 2014;13:185. doi: 10.1186/1475-2875-13-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ministry of Health and Sports . Health in Myanmar 2014. Nay Pyi Taw: Republic of Union of Myanmar; 2015. [Google Scholar]
- 9.WHO. Emergency response to artemisinin resistance in the Greater Mekong subregion: regional framework for action 2013–2015. Geneva: World Health Organization, 2015.
- 10.NMCP. National Plan For Malaria Elimination 2016–2030. Nay Pyi Taw: Republic of Union of Myanmar: National Malaria Control Programme; 2017.
- 11.Department of Public Health . Study on cause of under-five mortality. Nay Pyi Taw: Republic of Union of Myanmar; 2014. [Google Scholar]
- 12.Maung TM, Oo T, Wai KT, Hlaing T, Owiti P, Kumar B, et al. Assessment of household ownership of bed nets in areas with and without artemisinin resistance containment measures in Myanmar. Infect Dis Poverty. 2018;7:19. doi: 10.1186/s40249-018-0399-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aung T, Wei C, McFarland W, Aung YK, Khin HSS. Ownership and use of insecticide-treated nets among people living in malaria endemic areas of Eastern Myanmar. PLoS ONE. 2016;11:e0162292. doi: 10.1371/journal.pone.0162292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu H, Xu J, Guo X, Havumaki J, Lin Y, Yu G, et al. Coverage, use and maintenance of bed nets and related influence factors in Kachin Special Region II, northeastern Myanmar. Malar J. 2015;14:212. doi: 10.1186/s12936-015-0727-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nyunt MH, Aye KM, Kyaw MP, Kyaw TT, Hlaing T, Oo K, et al. Challenges in universal coverage and utilization of insecticide-treated bed nets in migrant plantation workers in Myanmar. Malar J. 2014;13:211. doi: 10.1186/1475-2875-13-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Than WP, Oo T, Wai KT, Thi A, Owiti P, Kumar B, et al. Knowledge, access and utilization of bed-nets among stable and seasonal migrants in an artemisinin resistance containment area of Myanmar. Infect Dis Poverty. 2017;6:138. doi: 10.1186/s40249-017-0353-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO. Guideline for the treatment of malaria. 3rd Edn. Geneva: World Health Organization; 2015.
- 18.Naing PA, Maung TM, Tripathy JP, Oo T, Wai KT, Thi A. Awareness of malaria and treatment-seeking behaviour among persons with acute undifferentiated fever in the endemic regions of Myanmar. Trop Med Health. 2017;45:31. doi: 10.1186/s41182-017-0070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye A, Win N, Maung TM, Wai KT, Oo T, Thi A, et al. Understanding malaria treatment-seeking preferences within the public sector amongst mobile/migrant workers in a malaria elimination scenario: a mixed-methods study. Malar J. 2017;16:462. doi: 10.1186/s12936-017-2113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hlaing T, Wai KT, Oo T, Sint N, Min T, Myar S, et al. Mobility dynamics of migrant workers and their socio-behavioral parameters related to malaria in Tier II, Artemisinin Resistance Containment Zone Myanmar. BMC Public Health. 2015;15:886. doi: 10.1186/s12889-015-2241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thandar MM, Kyaw MP, Jimba M, Yasuoka J. Caregivers’ treatment-seeking behaviour for children under age five in malaria-endemic areas of rural Myanmar: a cross-sectional study. Malar J. 2015;14:1. doi: 10.1186/1475-2875-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.MOHS. Myanmar Demographic and Health Survey (2015–16). Nay Pyi Taw:, Republic of Union of Myanmar: Ministry of Health and Sports; 2017.
- 23.Diema Konlan K, Japiong M, Dodam Konlan K, Afaya A, Salia SM, Kombat JM. Utilization of insecticide-treated bed nets (ITNs) among caregivers of children under five years in the Ho Municipality. Interdiscip Perspect Infect Dis. 2019;2019:1–7. doi: 10.1155/2019/3693450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Linn SY, Maung TM, Tripathy JP, Shewade HD, Oo SM, Linn Z, et al. Barriers in distribution, ownership and utilization of insecticide-treated mosquito nets among migrant population in Myanmar, 2016: a mixed methods study. Malar J. 2019;18:172. doi: 10.1186/s12936-019-2800-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maung Maung T, Prasad Tripathy J, Oo T, Mon Oo S, Naing Soe T, Thi A, et al. Household ownership and utilization of insecticide-treated nets under the regional artemisinin resistance initiative in Myanmar. Trop Med Health. 2018;46:27. doi: 10.1186/s41182-018-0111-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oresanya OB, Hoshen M. Sofola OT Utilization of insecticide-treated nets by under-five children in Nigeria: assessing progress towards the Abuja targets. Malar J. 2008;7:145. doi: 10.1186/1475-2875-7-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Korenromp EL, Miller J, Cibulskis RE, Kabir Cham M, Alnwick D, Dye C. Monitoring mosquito net coverage for malaria control in Africa: possession vs. use by children under 5 years. Trop Med Int Health. 2003;8:693–703. doi: 10.1046/j.1365-3156.2003.01084.x. [DOI] [PubMed] [Google Scholar]
- 28.NMCP. Guidelines for Malaria Diagnosis and Treatment in Myanmar. Nay Pyi Taw, Republic of Union of Myanmar: National Malaria Control Programme; 2015.
- 29.Smith LA, Bruce J, Gueye L, Helou A, Diallo R, Gueye B, et al. From fever to anti-malarial: the treatment-seeking process in rural Senegal. Malar J. 2010;9:333. doi: 10.1186/1475-2875-9-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cassy A, Saifodine A, Candrinho B, Do M, Martins R, Da Cunha S, et al. Care-seeking behaviour and treatment practices for malaria in children under 5 years in Mozambique: a secondary analysis of 2011 DHS and 2015 IMASIDA datasets. Malar J. 2019;18:115. doi: 10.1186/s12936-019-2751-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu J-W, Xu Q-Z, Liu H, Zeng Y-R. Malaria treatment-seeking behaviour and related factors of Wa ethnic minority in Myanmar: a cross-sectional study. Malar J. 2012;11:417. doi: 10.1186/1475-2875-11-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hein KT, Maung TM, Htet KK, Shewade HD, Tripathy JP, Oo SM, et al. Low uptake of malaria testing within 24 h of fever despite appropriate health-seeking among migrants in Myanmar: a mixed-methods study. Malar J. 2018;17:396. doi: 10.1186/s12936-018-2546-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Najnin N, Bennett CM, Luby SP. Inequalities in care-seeking for febrile illness of under-five children in urban Dhaka Bangladesh. J Health Popul Nutr. 2011;29:523–531. doi: 10.3329/jhpn.v29i5.8907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thind A. Health service use by children in rural Bihar. J Trop Pediatr. 2004;50:137–142. doi: 10.1093/tropej/50.3.137. [DOI] [PubMed] [Google Scholar]
- 35.Taffa N, Chepngeno G. Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop Med Int Health. 2005;10:240–245. doi: 10.1111/j.1365-3156.2004.01381.x. [DOI] [PubMed] [Google Scholar]
- 36.El Arifeen S, Baqui AH, Victora CG, Black RE, Bryce J, Hoque DME, et al. Sex and socioeconomic differentials in child health in rural Bangladesh: findings from a baseline survey for evaluating integrated management of childhood illness. J Health Popul Nutr. 2008;26:22–35. [PMC free article] [PubMed] [Google Scholar]
- 37.Goldman N, Pebley AR, Gragnolati M. Choices about treatment for ARI and diarrhea in rural Guatemala. Soc Sci Med. 2002;55:1693–1712. doi: 10.1016/S0277-9536(01)00260-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are not available in public domain because they are currently being analyzed in related papers. However, data are available with the corresponding author (KTM) and will be made accessible on reasonable request at the following e-mail: drktmin@gmial.com.