Abstract
Background
Primary dysmenorrhea is defined as a crampy pain in the lower abdomen before or during the menstrual period in the absence of any pelvic pathology. It is the leading motherhood problem worldwide but there is limited evidence on the prevalence of primary dysmenorrhea in the study area as well in Ethiopia. Researching primary dysmenorrhea helps to focus on the treatment plan. The study aimed to assess the prevalence, intensity, impact, and associated factors of primary dysmenorrhea among female students at Gondar town preparatory school.
Methods
A cross-sectional study design conducted among female students at Gondar town Preparatory School from May 1–10/2017. A total of 459 study participants were used. A simple random sampling technique was used to select study participants. A self-administered structured questionnaire was employed. Epi Info version 7 and SPSS version 20 were used for data entry and analysis respectively. A binary logistic regression model was computed. Variables having a p-value < 0.05 in the multivariate logistic regression model were considered as statistically significant.
Results
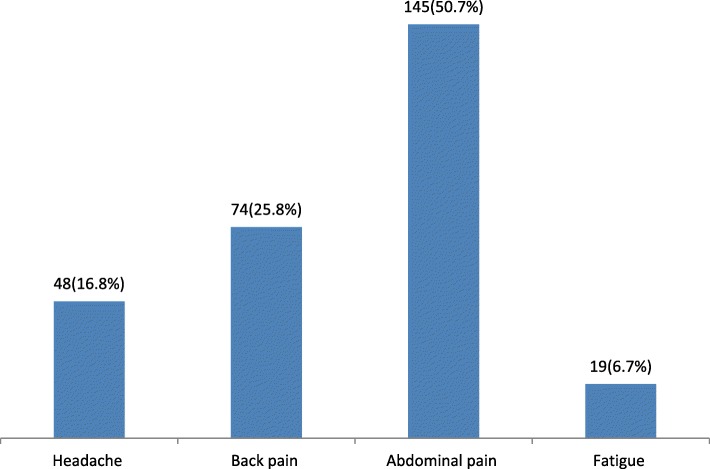
A total of 459 female students participated in the study with a response rate of 96.29%. The prevalence of primary dysmenorrhea among female students was found to be 64.7% (95% CI; 60.2–69.2%). Around 61% reported moderate intensity of menstrual pain and 50.7% complain about lower abdominal pain. Sixty-five percent of study participants reported that absenteeism from school was the impact of menstrual pain. Having irregular monthly menstrual cycle (AOR = 1.70, 95% CI; 1.02, 2.84) and positive family history of dysmenorrhea (AOR = 5.19, 95% CI: 3.21, 8.37) were significantly associated with primary dysmenorrhea.
Conclusions
The prevalence of primary dysmenorrhea was found to be high. Having an irregular monthly menstrual cycle and a positive family history of dysmenorrhea were determinants of primary dysmenorrhea.
Keywords: Female, Impact, Intensity, Primary dysmenorrhea, Prevalence, Preparatory school students
Background
Dysmenorrhea is pain associated with menstruation. It is the most commonly reported menstrual disorder in women. More than half of women who menstruate have pain for 1–2 days each month [1, 2]. It is an extremely common and sometimes debilitating condition for women of reproductive age [3]. Its prevalence varies from between16 to 91% in reproductive age women [4]. Dysmenorrhea is classified as primary and secondary dysmenorrhea. Secondary dysmenorrhea is caused by a disease or condition such as infection, ovarian cyst, and endometriosis [5].
Primary dysmenorrhea is defined as cramping pain in the lower abdomen before or during the menstruation period in the absence of any pelvic pathology [6]. It is the leading women hood problem that affects 90% of adolescent girls and more than 50% menstruating women [7]. The pathophysiology of primary dysmenorrhea is due to increased and/or abnormal uterine activity as a result of increased production and release of prostaglandins [8, 9]. The clinical feature of Primary Dysmenorrhea is frequent and crampy pain which mainly affects the lower abdomen and radiates to the back or thigh [6].
Fatigue emotional disturbance, abdominal distension, nausea, vomiting, and sleep disturbances are associated with symptoms of dysmenorrhea [4]. The causes of primary dysmenorhea were not well studied, but the common risk factors are a positive family history of dysmenorrhea, not use of oral contraceptive, smoking, higher severity of bleedings, shorter/longer menstrual period interval, stress, and menstrual cycle irregularity [1, 2, 4, 10].
Daily activity limitation, absenteeism from school/work, social withdrawal, decrease academic performance, and increased health care medical costs are the negative effect of primary dysmenorrhea [4, 10–14]. Use of oral contraceptives [3], non-steroidal anti-inflammatory medications [15, 16], herbal medicines [17], massage [18], and lifestyle modification [19] are treatment strategies to reduce dysmenorrheic pain.
In Ethiopia, there is limited evidence on the prevalence, intensity, impact, and associated factors of primary dysmenorrhea among preparatory school female students in the study area.
Methods
Study design and settings
A cross-sectional survey was conducted among female preparatory school students in Gondar town from May 1–10/2017. Gondar town is one of the historical towns in Ethiopia. It is found in Amhara regional state, Northwest part of Ethiopia. It is about 750 km away from Addis Ababa the capital city of Ethiopia. In Gondar town, there are five preparatory schools of which three preparatory schools were selected.
Source and study population
Female students who undergo their education in Gondar town preparatory school were considered as source population whereas female students who were present in the selected preparatory school during the data collection period were taken as the study population.
Inclusion / exclusion criteria
Female students who undergo their education in the selected preparatory school at Gondar town were included in the study whereas female students who had a known diagnosed medical history of pelvic pathology were excluded in the study.
Sample size and sampling procedures
The sample size was determined by using a single population proportion formula using the assumption of; 95% level of confidence, 4% marginal error and by taking the prevalence of dysmenorrhea from a previous study (77.6%) [12]. With these assumptions, the sample size became 417. Anticipating a10% nonresponsive rate, the required sample size was 459.The study participants were taken from the selected (Azezo, Fasiledes, and Angereb) preparatory schools using stratified random sampling with proportional allocation. The study participants were selected using a simple random sampling technique.
Data collection tools and procedures
A pretested structured questionnaire was used. The questionnaire adopted from previous literature [12, 20]. The questionnaire had three parts namely socio-demographic characteristics, obstetric /gynecological related characteristics and presence of primary dysmenorrhea, intensity and their impacts. Pain associated with menstruation without any pelvic pathology was considered as primary dysmenorrhea.
The irregular monthly menstrual cycle is taken as longer/heavy bleeding than a usual menstrual cycle [21]. Using a verbal report from the Numeric Rating Scale (NRS); the intensity of primary dysmenorrhea related pain was considered as no pain (NRS = 0), mild pain (NRS = 1–3), moderate pain (NRS = 4–6), and severe pain (NRS = 7–10) [22]. The data were collected by five nurses (three data collectors and two supervisors) from May 1–10/2017 using a self-administered technique.
Data processing and analysis
Data were checked, coded, and entered into Epi Info version 7 and exported to SPSS version 20 for analysis. Descriptive statistics such as frequency and percentage were used. Tables and bar graphs were used to display the findings. A binary logistic regression model was used to identify factors associated with primary dysmenorrhea. Variables whose p-value≤0.2 in the bivariable logistic regression analysis were taken into multivariable logistic regression analysis. For the bivariable logistic regression; Crude Odds Ratio (COR) and 95% CI, and for the multivariable logistic regression; Adjusted Odds Ratio (AOR) and 95% CI were calculated. Variables having a p-value < 0.05 in the multivariate logistic regression model were considered as statistically significant. The backward stepwise logistic regression analysis method was used. Hosmers and Lemishow goodness of fit test were done.
Results
Socio-demographic characteristics of respondents
A total of 459 female students were enrolled in the study with a response rate of 96.29%. Among study participants, 232(52.5%) were aged less than 18 years, 286(64.7%) were grade eleven, 398(90%) were single, and 403(91.2%) were Orthodox Christian followers. More than threefold (94.3%) of study participants were Amhara by ethnicity. The majority (86.7%) of the respondents were urban dwellers and 370(83.7%) were lived with their family home. Regarding family education, more than half of respondent mothers’ were illiterate and 294(66.5%) were housewives by their occupational status. Above one–third (40%) study participants carry out sports activity (Table 1).
Table 1.
Socio-demographic characteristics of female students at Gondar town preparatory school Northwest Ethiopia, 2017, (n = 442)
| Variables | Category | Frequency (n) | Percent (%) |
|---|---|---|---|
| Age in year | ≥18 | 210 | 47.5 |
| < 18 | 232 | 52.5 | |
| Student grade | 11th | 286 | 64.7 |
| 12th | 156 | 35.3 | |
| Religion | Orthodox Christian | 403 | 91.2 |
| Muslim | 28 | 6.3 | |
| Protestant | 11 | 2.5 | |
| Marital status | Single | 398 | 90 |
| Married | 39 | 8.8 | |
| Divorced | 4 | 0.9 | |
| Widowed | 1 | 0.2 | |
| Ethnicity | Amhara | 417 | 94.3 |
| Qimant | 13 | 3 | |
| Tigray | 12 | 2.7 | |
| Origins of residence | Urban | 383 | 86.7 |
| Rural | 59 | 13.3 | |
| Place of residence | At family home | 370 | 83.7 |
| With other relatives | 37 | 8.4 | |
| At dormitory | 35 | 7.9 | |
| Mother’s education | Illiterate | 228 | 51.6 |
| Primary school | 61 | 13.8 | |
| Secondary school | 95 | 21.5 | |
| College and above | 58 | 13.1 | |
| Mother’s Occupation | Government employed | 88 | 19.9 |
| Housewife | 294 | 66.5 | |
| Merchant | 50 | 13.6 | |
| Sport activity | Yes | 177 | 40 |
| No | 265 | 60 |
Obstetrics and gynecology related characteristics
Among study participants, 250(56.6%) experienced 1st menstruation at the age group of 12–14 years. Nearly three-fourths (73.5%) of study participants had regular monthly menstrual cycle pattern and the vast majority (91.9%) of study participants reported menstrual bleeding duration ≤7 days. One hundred eighty- three (41.4%) of study participants reported that they had a positive family history of dysmenorrhea (Table 2).
Table 2.
Obstetric and gynecological related characteristics of female students at Gondar town preparatory school Northwest Ethiopia, 2017, (n = 442)
| Variables | Category | Frequency (n) | Percent (%) |
|---|---|---|---|
| Age at menarche | 12–14 | 250 | 56.6 |
| ≥15 | 192 | 43.4 | |
| Monthly menstrual cycle | Regular | 325 | 73.5 |
| Irregular | 117 | 26.5 | |
| Menstrual bleeding duration (in days) | ≤7 | 406 | 91.9 |
| > 7 | 36 | 36.1 | |
| Estimated amount of menstrual flow /by no. of pads | ≤2 | 288 | 65.2 |
| 3–4 | 141 | 31.9 | |
| > 4 | 13 | 2.9 | |
| Any family planning method? | Yes | 30 | 6.8 |
| No | 412 | 93.2 | |
| Type of family planning used | Depo provera | 10 | 33.3 |
| Pills | 8 | 26.7 | |
| Implanol | 7 | 23.3 | |
| IUCD | 5 | 16.7 | |
| Family history of dysmenorhea | Yes | 183 | 41.4 |
| No | 259 | 58.6 | |
| Circumcision history | Yes | 38 | 8.6 |
| No | 404 | 91.4 | |
| Abortion history | Yes | 10 | 2.3 |
| No | 432 | 97.7 |
IUCD; Intrauterine Contraceptive Device
Prevalence, intensity, and impact of primary dysmenorrhea
The prevalence of primary dysmenorrhea was found to be 64.7%(95% CI; 60.2, 69.2%) of which nearly half (50.7%) of them complain about lower abdominal pain (Fig. 1). The intensity of pain during menstruation was 83(29%), 174(60.8%), and 29(10.2%) reported having mild, moderate, and severe menstrual pain respectively. Seventy-three (25.5%) used analgesic medications. Paracetamol 44(60.3%), diclofenac 15(20.5%), and Ibuprofen 14(19.2%) were used to relieve the pain. Absenteeism from school 186(65%), limited activity daily living 57(20%) and anxiety 43(15%) were the impact of menstrual pain reported by study participants.
Fig. 1.
Common complaining symptoms associated with primary dysmenorrhea among female students at Gondar town preparatory school, Northwest Ethiopia, 2017
Factors associated with primary dysmenorrhea
All variables with p-value ≤0.2 in the bivariable logistic regression analysis were taken into multivariable analysis. Having an irregular monthly menstrual cycle and a positive family history of dysmenorrhea were significantly associated with primary dysmenorrhea in multivariable logistic regression analysis (Table 3).
Table 3.
Factors associated with primary dysmenorrhea among female students at Gondar town preparatory school Northwest Ethiopia, 2017, (n = 442)
| Variables | Primary dysmenorrhea | COR, 95% CI | AOR, 95% CI | |
|---|---|---|---|---|
| Yes | No | |||
| Place of residence | ||||
| At family home | 239 | 131 | 1.216 (0.599,2.471) | 1.442 (0.650,2.471) |
| With other relatives | 26 | 11 | 1.576 (0.593,4.185) | 2.105 (0.725,6.106) |
| At dormitory | 21 | 14 | 1 | 1 |
| Age at menarche | ||||
| 12–14 | 164 | 86 | 1.094 (0.739,1.621) | 1.046 (0.672,1.629) |
| ≥ 15 | 122 | 70 | 1 | 1 |
| Monthly menstrual cycle | ||||
| Regular | 200 | 125 | 1 | 1 |
| Irregular | 86 | 31 | 1.734 (1.086,2.767) | 1.701 (1.019, 2.839)a |
| Menstrual bleeding duration | ||||
| ≤ 7 days | 262 | 144 | 1 | 1 |
| > 7 days | 24 | 12 | 1.099 (0.534,2.263) | 1.081 (0.467,2.502) |
| Family history of menstrual pain | ||||
| Yes | 153 | 30 | 4.832 (3.047,7.661) | 5.188 (3.214,8.373)a |
| No | 133 | 126 | 1 | 1 |
| Circumcision history | ||||
| Yes | 28 | 10 | 1.584 (0.748,3.354) | 1.531 (0.681,3.443) |
| No | 258 | 146 | 1 | 1 |
astatistically significant at p-value < 0.001
Discussion
The prevalence of primary dysmenorrhea was found to be 64.7% (95% CI; 60.2, 69.2%). Lower abdominal pain (50.7%), back pain (25.5%), headache (16.8%), and fatigue (6.7%) were the commonly reported symptoms among study participants. Nearly 61% reported moderate intensity of menstrual pain. Sixty-five percent of study participants reported that absenteeism from school is the main impact of menstrual pain. The finding of this study is in line with a study conducted at Debre Tabor, Ethiopia 62.3% [23] and Chandigarh, India 61.33% [24]. The finding of the current study was higher than a study in Canada (60%), Japan (46,5%) and (54.4%), Tbilisi, Georgia (52.07%), and Southern India (45%) [25–29]. The variation is due to the assessment tool, method of data collection such as interviewing using a cell phone, use of clinical assessment like ultrasound and laboratory test, and sample size used.
To the contrary, the finding of the current study was lower than a study conducted in Iran (89.1%), Turkey (72.7%), Debre Birhan University (85.4%) and University of Gondar Ethiopia (77.6%), Mansoura, Egypt (75%), Pakistan (78%), Iran (73.2%), and Saveetha University (70.4%) [26, 30–35]. This is due to the study setting, age of study participants, and most of the studies did not differentiate whether the dysmenorrhea is primary or secondary.
In this particular study, a positive family history of dysmenorrhea and irregular menstrual cycle are the determinant factors of primary dysmenorrhea. The study revealed that females who had a positive family history of dysmenorrhea were five times more likely to develop primary dysmenorrhea [AOR = 5.19, 95% CI: 3.21, 8.37] compared to those who had no family history of dysmenorrhea. This is supported by a study in Turkey [31], Iran [30], Eastern, Benin [36], Serbia [37], and Australia [38]. This is related to genetic linkage between the mother and the child that makes to develop menstrual pain. Studies suggest that genetic background influences the severity of dysmenorrhea [39].
Having an irregular monthly menstrual cycle is the determinant factor of primary dysmenorrhea. Female students who had irregular monthly menstrual cycle is nearly two times more likely to develop primary dysmenorrhea compared to those having regular monthly menstrual cycle [AOR = 1.701, 95% CI: 1.02,2.84]. No studies showed the relationship between the irregular monthly menstrual cycle and menstrual pain but it is associated with prostaglandin secretion. The author only used reports obtained from the respondents, no clinical examination was done. Since most studies conducted dysmenorrhea as a combined manner (primary and secondary dysmenorrhea) the author forced to discuss the current study with those studies. Further research is needed to find out the real cause of primary dysmenorrhea.
Conclusions
The prevalence of primary dysmenorrhea among female students found to be high. Irregular monthly menstrual cycle and positive family history of dysmenorrhea are determinant factors of primary dysmenorrhea. Absenteeism from school was the main impact of primary dysmenorrhea. Hence, researching primary dysmenorrhea significantly improves its impact by educating females about the management of primary dysmenorrhea.
Acknowledgments
The authors would like to thank the ethical review committee of the school of nursing at the University of Gondar, study participants, and data collectors for their collaboration during the data collection.
Abbreviations
- AOR
Adjusted Odds Ratio
- CI
Confidence Interval
- COR
Crude Odds Ratio
- IUCD
Intrauterine Contraceptive Device
- NRS
Numeric Rating Scale
Authors’ contributions
AWA conceived the idea and wrote the proposal, participated in the data collection process, analyze data, and draft the paper. DGK and TAW approved the proposal with some revisions, participated in data analysis, and reviewed the manuscript. All the authors approved the final draft of the manuscript.
Funding
No funding was received for this study.
Availability of data and materials
The raw data would not be provided for the reason of protecting patients’ confidentiality but, the summary data are available in the main document.
Ethics approval and consent to participate
The study was approved by the school of the nursing ethical review committee of the University of Gondar with reference number S/N/178/2017. Verbal informed consent was obtained from each study participant. No personal identifiers such as name, ID number, and phone number were used. The information obtained from each study participants was kept secured, locked, and stored as an electronic dataset.
Consent for publication
Not applicable.
Competing interests
The authors have declared that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Abere Woretaw Azagew, Email: wabere@ymail.com, Email: Abere.Woretaw@uog.edu.et.
Destaye Guadie Kassie, Email: dstgd32@gmail.com, Email: destaye.guadie@uog.edu.et.
Tarkie Abebe Walle, Email: robaname@gmail.com, Email: Tarkie.Abebe@uog.edu.et.
References
- 1.Dawood M. Dysmenorrhea. J Reprod Med. 1985;30(3):154–167. [PubMed] [Google Scholar]
- 2.Friederich MA. Dysmenorrhea. Women Health. 1983;8(2–3):91–106. doi: 10.1300/J013v08n02_05. [DOI] [PubMed] [Google Scholar]
- 3.Lefebvre G, Pinsonneault O, Antao V, Black A, Burnett M, Feldman K, et al. Primary dysmenorrhea consensus guideline. J Obstet Gynaecol Can. 2005;27(12):1117–1146. doi: 10.1016/S1701-2163(16)30395-4. [DOI] [PubMed] [Google Scholar]
- 4.Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2013;36(1):104–113. doi: 10.1093/epirev/mxt009. [DOI] [PubMed] [Google Scholar]
- 5.Johnston L. Menstrual pain (dysmenorrhoea) Prof Nurs Today. 2014;18(1):13–14. [Google Scholar]
- 6.Smith R, Kaunitz A. Primary dysmenorrhea in adult women: clinical features and diagnosis. Alphen aan den Rijn: Wolters Kluwer; 2015. [Google Scholar]
- 7.Berkley KJ. Primary dysmenorrhea: an urgent mandate. Pain. 2013;1(1):8.
- 8.Zahradnik H, Breckwoldt M. Contribution to the pathogenesis of dysmenorrhea. Arch Gynecol. 1984;236(2):99–108. doi: 10.1007/BF02134006. [DOI] [PubMed] [Google Scholar]
- 9.Åkerlund M. Pathophysiology of dysmenorrhea. Acta Obstet Gynecol Scand. 1979;58(sup87):27–32. doi: 10.3109/00016347909157786. [DOI] [PubMed] [Google Scholar]
- 10.Abdel-Salam DM, Alnuman RW, Alrwuaili RM, Alrwuaili GA, Alrwuaili EM. Epidemiological aspects of dysmenorrhea among female students at Jouf University, Saudi Arabia. Middle East Fertil Soc J. 2018;23(4):435–439. doi: 10.1016/j.mefs.2018.08.001. [DOI] [Google Scholar]
- 11.Gagua T, Tkeshelashvili B, Gagua D. Primary dysmenorrhea: prevalence in adolescent population of Tbilisi, Georgia and risk factors. J Turk Ger Gynecol Assoc. 2012;13(3):162. doi: 10.5152/jtgga.2012.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gebeyehu Minaleshewa Biruk, Mekuria Abebe Basazn, Tefera Yonas Getaye, Andarge Dagmawi Abate, Debay Yabsira Belayneh, Bejiga Geremew Sokile, Gebresillassie Begashaw Melaku. Prevalence, Impact, and Management Practice of Dysmenorrhea among University of Gondar Students, Northwestern Ethiopia: A Cross-Sectional Study. International Journal of Reproductive Medicine. 2017;2017:1–8. doi: 10.1155/2017/3208276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burnett MA, Antao V, Black A, Feldman K, Grenville A, Lea R, et al. Prevalence of primary dysmenorrhea in Canada. J Obstet Gynaecol Can. 2005;27(8):765–770. doi: 10.1016/S1701-2163(16)30728-9. [DOI] [PubMed] [Google Scholar]
- 14.Akiyama S, Tanaka E, Cristeau O, Onishi Y, Osuga Y. Evaluation of the treatment patterns and economic burden of dysmenorrhea in Japanese women, using a claims database. Clinicoecon Outcomes Res. 2017;9:295. doi: 10.2147/CEOR.S127760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawood MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstet Gynecol. 2006;108(2):428–441. doi: 10.1097/01.AOG.0000230214.26638.0c. [DOI] [PubMed] [Google Scholar]
- 16.De Sanctis V, Soliman A, Bernasconi S, Bianchin L, Bona G, Bozzola M, et al. Primary dysmenorrhea in adolescents: prevalence, impact and recent knowledge. Pediatr Endocrinol Rev. 2015;13(2):512–20. [PubMed]
- 17.Nahid K, Fariborz M, Ataolah G, Solokian S. The effect of an Iranian herbal drug on primary dysmenorrhea: a clinical controlled trial. J Midwifery Womens Health. 2009;54(5):401–404. doi: 10.1016/j.jmwh.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Karampour E, Khoshnam E, Khoshnam MS, Mohammadi HR, Jahromi FZ, Nikseresht AA. The effect of massage training on primary dysmenorrhea. Adv Environ Biol. 2012. p. 3040–3.
- 19.Durain D. Primary dysmenorrhea: assessment and management update. J Midwifery Womens Health. 2004;49(6):520–528. doi: 10.1016/j.jmwh.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Hailemeskel S, Demissie A, Assefa N. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: evidence from female university students in Ethiopia. Int J Women's Health. 2016;8:489. doi: 10.2147/IJWH.S112768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamamoto K, Okazaki A, Sakamoto Y, Funatsu M. The relationship between premenstrual symptoms, menstrual pain, irregular menstrual cycles, and psychosocial stress among Japanese college students. J Physiol Anthropol. 2009;28(3):129–136. doi: 10.2114/jpa2.28.129. [DOI] [PubMed] [Google Scholar]
- 22.Breivik H, Borchgrevink P, Allen S, Rosseland L, Romundstad L, Breivik Hals E, et al. Assessment of pain. BJA. 2008;101(1):17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]
- 23.Awoke Giletew WB. Prevalence and associated factors of primary dysmenorrhea among Debre Tabor University students, north Central Ethiopia. Int J Biomed Eng Clin Sci. 2019;4(4):70–74. [Google Scholar]
- 24.Ahuja A, Sharma MK, Singh A. Impact of dysmenorrhea on quality of life of adolescent girls of Chandigarh. J Child Adolesc Behav. 2016;4(295):2.
- 25.Margaret A, Burnett VA, Black A, Feldman K, Grenville A, Lea R, Lefebvre G, Pinsonneault O, Robert M. Prevalence of Primary Dysmenorrhea in Canada. J Obstet Gynaecol Can. 2005;27(8):765–770. doi: 10.1016/S1701-2163(16)30728-9. [DOI] [PubMed] [Google Scholar]
- 26.Sayako Akiyama ET, Cristeau O, Onishi Y, Osuga Y. Evaluation of the treatment patterns and economic burden of dysmenorrhea in Japanese women, using a claims database. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tinatin Gagua BT. David Gagua. Primary dysmenorrhea: prevalence in adolescent population of Tbilisi, Georgia and risk factors. J Turkish-German Gynecol Assoc. 2012;2012(13):162–168. doi: 10.5152/jtgga.2012.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.KMaKN MK. Prevalence of Dysmenorrhea and Its Correlating Lifestyle Factors in Japanese Female Junior High School Students. Ohoku J Exp Med. 2015;2015(236):107–113. doi: 10.1620/tjem.236.107. [DOI] [PubMed] [Google Scholar]
- 29.Maitri Shah AM, Patel S, Shah M, Bakshi H. A study of prevalence of primary dysmenorrhea in young students healthline. 2013. pp. 30–34. [Google Scholar]
- 30.Habibi N, Huang MSL, Gan WY, Zulida R, Safavi SM. Prevalence of Primary Dysmenorrhea and Factors Associated with its intensity among undergraduate students. J Pain Manage Nurs. 2015;16(6):855–61. [DOI] [PubMed]
- 31.Alaettin Unsal UA. Mustafa Tozun, Gul Arslan & Elif Calik. Prevalence of dysmenorrhea and its effect on quality of life among a group of female university students. Ups J Med Sci. 2010;2010(115):138–145. doi: 10.3109/03009730903457218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gebeyehu Minaleshewa Biruk, Mekuria Abebe Basazn, Tefera Yonas Getaye, Andarge Dagmawi Abate, Debay Yabsira Belayneh, Bejiga Geremew Sokile, Gebresillassie Begashaw Melaku. Prevalence, Impact, and Management Practice of Dysmenorrhea among University of Gondar Students, Northwestern Ethiopia: A Cross-Sectional Study. International Journal of Reproductive Medicine. 2017;2017:1–8. doi: 10.1155/2017/3208276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El-Gilany AH, Badawi K, El-Fedawy S. Epidemiology of dysmenorrhoea among adolescent students in Mansoura, Egypt. East Mediterr Health J. 2005;11:155–163. [PubMed] [Google Scholar]
- 34.Solomon Hailemeskel AD. Nigussie Assefa. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: evidence from female university students in Ethiopia. Int J Women's Health. 2016;2016(8):489–496. doi: 10.2147/IJWH.S112768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saleema Gulzar SK, Abbas K, Arif S, Husain SS, Imran HI. Jacoline Sommer Prevalence, Perceptions and Effects of Dysmenorrhea in School Going Female Adolescents of Karachi, Pakistan. Int J Innovative Res Dev. 2015;4(2):236–240. [Google Scholar]
- 36.Sidi IHB, Obossou AAA, Salifou K, Vodouhe M, Denakpo J, Perrin R. Primary Dysmenorrhea in the Schools of Parakou: Prevalence, Impact and Therapeutic Approach. Gynecol Obstet. 2016;6(5).
- 37.Jankovic APiaS. Riskfactorsfordysmenorrheaamongyoungadultfemaleuniversitystudents. AnnIstSuperSanità 2016;52(1):98–103.
- 38.Hong Ju MJ. And Gita Mishra. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2016;2014(36):104–113. doi: 10.1093/epirev/mxt009. [DOI] [PubMed] [Google Scholar]
- 39.Jones AV, Hockley JR, Hyde C, Gorman D, Sredic-Rhodes A, Bilsland J, et al. Genome-wide association analysis of pain severity in dysmenorrhea identifies association at chromosome 1p13. 2, near the nerve growth factor locus. Pain. 2016;157(11):2571. doi: 10.1097/j.pain.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data would not be provided for the reason of protecting patients’ confidentiality but, the summary data are available in the main document.