Abstract
Environmental health (EH) professionals provide critical services and respond to complex and multifaceted public health threats. The role of these professionals is continually re-emphasized by emergencies requiring rapid and effective responses to address environmental issues and ensure protection of the public’s health. Given the prominence of the EH profession within the public health framework, assessing the governmental health department workforce, practice, and current and future challenges is crucial to ensure EH professionals are fully equipped and prepared to protect the nation’s health. Such an understanding of the EH profession is lacking; therefore, we initiated Understanding the Needs, Challenges, Opportunities, Vision, and Emerging Roles in Environmental Health (UNCOVER EH). Through a web-based survey, we identified EH professional demographics, characteristics, education, practice areas, and aspects of leadership and satisfaction. We distributed the survey to a convenience sample of EH professionals working in health departments, limiting the generalizability of results to the entire EH workforce. The results were strengthened, however, by purposive sampling strategies to represent varied professional and workforce characteristics in the respondent universe. The UNCOVER EH initiative provides a primary source of data to inform EH workforce development initiatives, improve the practice, and establish uniform benchmarks and professional competencies.
Introduction
News stories often cover threats to public health, such as hurricanes and their devastating effects, vectorborne diseases spreading increasingly widely by mosquitoes and ticks, and drinking water contaminated by leached chemicals and aging infrastructure. Responses to these threats and approaches to addressing associated detriments to public health are generally complex and multifaceted. In the Environmental Health Playbook: Investing in a Robust Environmental Health System (2017), the National Environmental Health Partnership Council in the U.S. recognized the serious environmental implications resulting from emergency events such as the Zika virus outbreak and the Flint water crisis. Among the needs identified for effective responses to an emergency event, the playbook called for strengthened governmental environmental health (EH) services and an increasingly skilled, well-trained workforce (National Environmental Health Partnership Council, 2017).
EH, as a profession and practice, is one of the most significant contributors to state, tribal, local, and territorial (STLT) public health. As a major segment of the public health workforce, EH professionals have the important responsibility of identifying, investigating, and controlling harmful environmental exposures to prevent related illness and injury (National Environmental Health Association [NEHA], 2013; Resnick, Zablotsky, & Burke, 2009). EH professionals must maintain a high level of competency, skills, and preparedness to fulfill their responsibilities in protecting the public health. The public health landscape is continuously changing and as emerging EH issues and concerns arise, EH professionals and their practice must evolve and adapt to meet the challenge.
The Public Health Workforce: An Agenda for the 21st Century, a report from the U.S. Department of Health and Human Services (1997), listed necessary actions for strengthening the public health workforce. Leadership and workforce development were among these actions. Various studies and assessments of public health departments examined related concepts and shed some light on the EH profession. For example, workforce estimates reported in local health department profiles revealed a decline of more than 2,000 EH full-time equivalents from 2008–2016 (National Association of County and City Health Officials [NACCHO], 2017). Additionally, the total number of different EH activities performed by state health departments reportedly decreased by 5% from 2010–2016 (Association of State and Territorial Health Officials [ASTHO], 2017).
EH professionals were included in the Public Health Workforce Interests and Needs Survey (PH WINS), the first national survey of the state health agency workforce (Sellers et al., 2015). Additionally, statewide surveys have collected information about EH program capacity and professional characteristics, competencies, and responsibilities (Dyjack, Case, Marlow, Soret, & Montgomery, 2007; Resnick et al., 2009). More than 50 years ago, the U.S. Department of Health, Education, and Welfare (1963) conducted an assessment of sanitarians working in government, the private sector, and academia. What has been missing is a comprehensive effort designed specifically to gather information directly from EH professionals practicing at health departments across the U.S.
Several groups have identified the need for information on EH workforce composition and critical functions (Centers for Disease Control and Prevention [CDC], 2003; NEHA Committee on the Future of Environmental Health, 1993; Resnick et al., 2009). Developing a robust understanding and characterization of the EH workforce is especially needed now to begin to address the challenging and complex problems faced by EH professionals, particularly when reductions in capacity and resources are consistently reported. Given the prominence of the EH profession within the public health framework, ensuring EH professionals maintain a high level of preparedness and skills is crucial to protect the nation’s health.
To meet the need, the Centers for Disease Control and Prevention (CDC), National Environmental Health Association (NEHA), and Baylor University partnered on a groundbreaking initiative: Understanding the Needs, Challenges, Opportunities, Vision, and Emerging Roles in Environmental Health (UNCOVER EH) (Gerding, Landeen, & Brooks, 2017). UNCOVER EH presented a unique and unprecedented opportunity to collect information directly from EH professionals working at STLT health departments. The overall purpose of this effort was to identify and describe key governmental EH workforce and practice elements such as professional demographics, areas of practice, and current and future challenges and opportunities. Information generated through this initiative can inform EH workforce development activities and support enhancement of the practice.
For the present study, we performed a web-based survey aimed at describing EH professional demographics, characteristics, practice areas, and aspects of leadership and satisfaction. The survey was distributed to a convenience sample of EH professionals in health departments, which presents limitations for the generalizability of study results to the entire profession. Here we present an initial attempt to describe and understand the EH workforce in the U.S.
Methods
In November 2017, a link to a web-based survey consisting of multiple choice, scaled, rank ordered, and open-ended questions was e-mailed to 8,996 EH professionals working at STLT health departments. The survey required roughly 30 minutes to complete. It was designed to align with content and elements of different public health workforce and profile surveys, along with recommended workforce study criteria and horizonscanning methods (ASTHO, 2017; Boulton et al., 2014; Boxall et al., 2012; Furley et al., 2018; NACCHO, 2017; Sellers et al., 2015; Van den Brink et al., 2018).
We followed recommendations to contact potential respondents at five points to maximize the response rate (Dillman, 2007). The five points included e-mailing 1) an introductory message, 2) an invitation with the survey link, 3) a reminder to complete the survey, 4) a second reminder, and 5) a final message encouraging respondents to complete the survey. The Office of Management and Budget approved the survey and collection of information (Control #0920–1187) in accordance with the Paperwork Reduction Act.
The majority of EH professionals were identified in EH staff directories obtained directly from health departments. Additional sources included online staff directories or lists, state credentialing records for registered sanitarians and registered environmental health specialists, and NEHA state affiliate association membership rosters. Information from all data sources was compiled to generate a comprehensive list of respondent e-mail addresses.
We filtered this list to contain only e-mail addresses for EH professionals employed by STLT health departments. We also tried to ensure this sample included and represented EH professionals from different geographic areas and levels of government. At the end of the survey period, we downloaded results to an Excel spreadsheet and prepared the dataset for analysis. Descriptive statistics were used to examine workforce data, which we categorized as demographics, professional characteristics, education and training, practice, leadership, and satisfaction.
Results
Of the 8,996 EH professionals invited to complete the survey, 56 actively declined participation, 474 partially completed the survey, and 6,730 provided no response. Overall, 1,736 EH professionals fully completed the survey, resulting in a 19% response rate. We included only fully completed surveys in our analysis. The 1,736 respondents represented a relatively balanced representation among states across the nation. By U.S. Census regions, 31% of respondents were from the South, 30% from the Midwest, 27% from the West, and 12% from the Northeast. Respondents from the West included seven EH professionals from Pacific Island territorial health departments. Two state-level health departments from the South declined participation in the survey. These two states have a centralized governance structure and the decision to decline participation resulted in the exclusion of all local-level health departments within those states. We received no responses from territories that had recently been impacted by Hurricanes Irma and Maria.
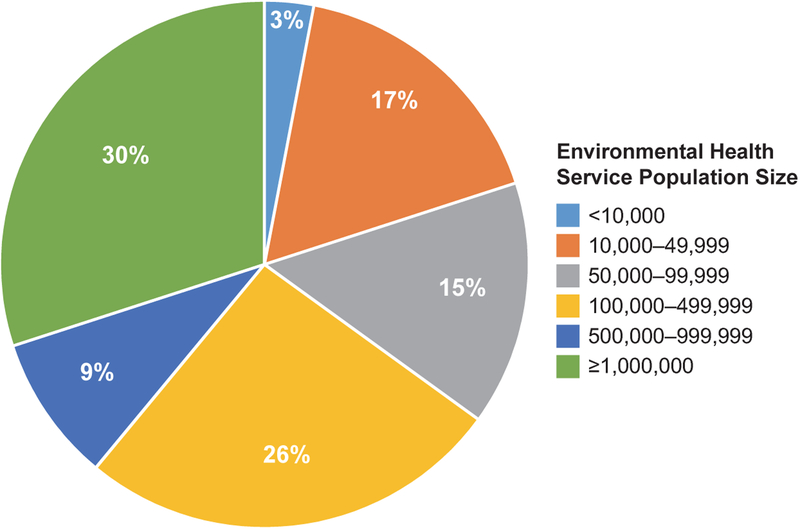
The majority of EH professional respondents were employed by local health departments (72%, n = 1,242), followed by those at state (23%, n = 406), territorial (0.5%, n = 8), and tribal (0.4%, n = 7) levels. A small percentage of EH professionals responded from the federal level (2%, n = 27), and likely worked for federal agencies that provide STLT-level services. Figure 1 shows the percentages of population sizes served by respondent health departments. Among respondents, 65% reported that their respective health departments provided services to populations of ≥100,000, with the largest percentage of departments (30%) found in the category of ≥1,000,000.
FIGURE 1.
Population Size Served by Environmental Health Professionals in Health Departments in the United States (n = 1,734)
Demographics
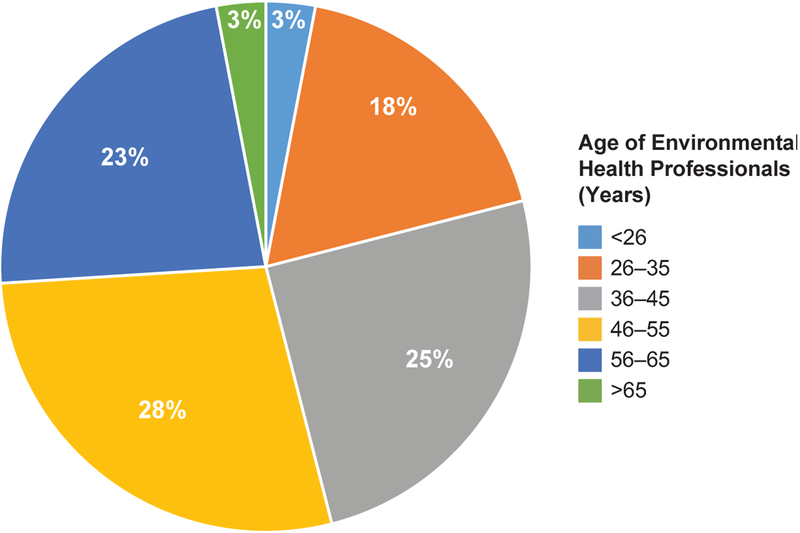
EH professionals of all races responded to the survey (Table 1). The category with the highest proportion of respondents was White (86%, n = 1,494), while the lowest was Native Hawaiian or other Pacific Islander (1%, n = 13). Approximately 6% (n = 105) of the respondents were Hispanic. Relatively even numbers of males (51%) and females (49%) responded. Figure 2 shows the percentages of EH professionals in six age ranges. The highest percentage of EH professionals was 46–55 years of age (28%) and more than half of all respondents were ≥46 years (54%).
TABLE 1.
Race, Ethnicity, and Professional Characteristics of Environmental Health Professionals in Health Departments in the United States
| Characteristic | # | % |
|---|---|---|
| Race | ||
| American Indian or Alaska Native | 53 | 3 |
| Asian | 73 | 4 |
| Black or African American | 126 | 7 |
| Native Hawaiian or other Pacific Islander | 13 | 1 |
| White | 1,494 | 86 |
| Ethnicity | ||
| Hispanic | 105 | 6 |
| Position level | ||
| Director/chief | 237 | 14 |
| Supervisor/manager | 419 | 24 |
| Field staff | 922 | 53 |
| Other | 157 | 9 |
| Position title | ||
| Environmental health specialist | 813 | 47 |
| Environmental health technician | 17 | 1 |
| Environmental scientist | 50 | 3 |
| Environmentalist | 45 | 3 |
| Inspector | 77 | 4 |
| Laboratory technician or analyst | 6 | 0.3 |
| Sanitarian | 350 | 20 |
| Other | 377 | 22 |
| Employment status | ||
| Full-time | 1,680 | 97 |
| Part-time | 39 | 2 |
| Seasonal | 1 | 0.1 |
| Temporary | 0 | 0 |
| Prefer not to say | 5 | 0.3 |
| Other | 10 | 0.6 |
Note. Respondents sometimes selected more than one race; percentages for each category were based on the number of respondents (n = 1,735).
FIGURE 2.
Age of Environmental Health Professionals in Health Departments in the United States (n = 1,735)
Professional Characteristics
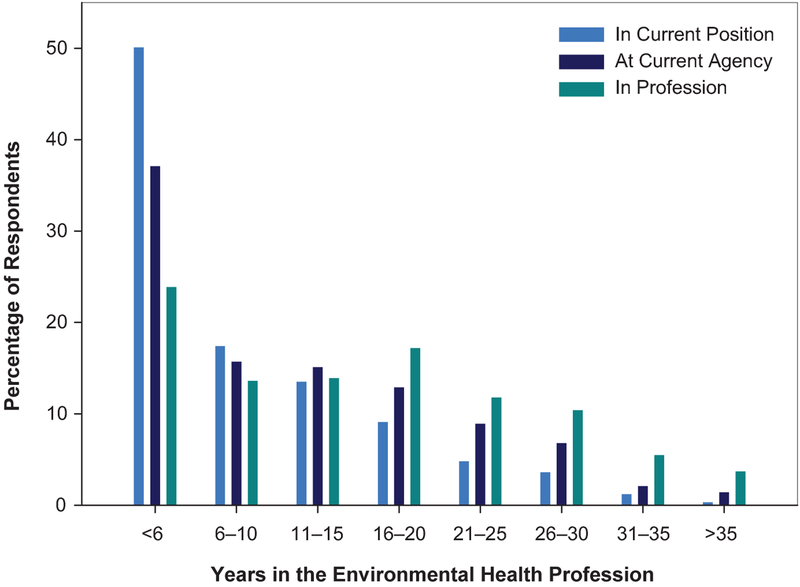
Table 1 shows professional characteristics of the respondents. Most respondents identified themselves as field staff (53%, n = 922), followed by supervisors or managers (24%, n = 419), and then program directors or chiefs (14%, n = 237). The most common job titles were environmental health specialist (47%, n = 813) and sanitarian (20%, n = 350). Nearly two thirds (64%) of the EH professionals were registered environmental health specialists or registered sanitarians and almost all respondents were fulltime employees (97%, n = 1,680). Figure 3 shows the number of year respondents had spent in their current position, at their current agency, and in the EH profession. The highest percentages of EH professionals had ≤5 years in these three categories. The percentages declined monotonically as age categories increased, except for time in the EH profession, which slightly increased in the 6–20year range.
FIGURE 3.
Years in Current Position, at Current Agency, and in the Profession for Environmental Health Professionals in Health Departments in the United States (n = 1,734)
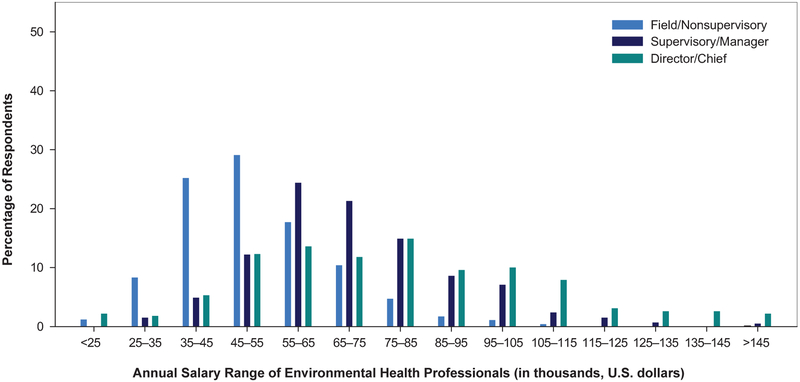
Responses pertaining to retirement and career plans revealed that approximately one quarter of EH professionals planned to retire within the next 5 years (26%, n = 451). Almost three quarters of respondents, however, had no plans to leave their agency within the next year (71%, n = 1,231). Annual salary by position level (field/nonsupervisory, supervisory/manager, and director/chief) showed that most EH professionals in field and nonsupervisory-level positions had salaries ranging from $35,000 to $54,999. Salaries for managers or supervisors mostly ranged from $55,000 to $74,999, whereas salaries for directors or chiefs were distributed across the salary ranges, from <$25,000 to >$145,000 (Figure 4).
FIGURE 4.
Annual Salaries of Environmental Health Professionals by Position Level in Health Departments in the United States (n = 1,735)
Education and Training
Respondent EH professionals held bachelor’s (72%, n = 1,241), master’s (31%, n = 538), and doctoral (2%, n = 43) degrees in a wide range of fields or concentrations. A few respondents did not complete a college degree (3%, n = 53). The survey allowed selection of two fields of study for each degree type (Table 2). The highest number of EH professionals received bachelor’s degrees in the biological and biomedical sciences (n = 464). Among all the EH professionals with bachelor’s degrees, only 213 indicated their field of study was EH and 76 identified it as public health. Of these 289 professionals, 66 indicated their degree was received from an academic program accredited by the National Environmental Health Science and Protection Accreditation Council (EHAC), 10 from a program accredited by the Council on Education for Public Health, and 25 reported their degree was from a program accredited by both organizations. Public health (n = 179) and specifically EH (n = 90) were the most common fields of study among those holding master’s degrees. Overall, most EH professionals continued their education by completing training courses within the last year (90%, n = 1,554) and with support from their agencies to travel to attend training (89%, n = 1,538).
TABLE 2.
Degrees and Fields of Study of Environmental Health Professionals in Health Departments in the United States
| Field of Study | Bachelor’s | Master’s | Doctoral |
|---|---|---|---|
| Agriculture and natural resources | 89 | 25 | 3 |
| Architecture and related services | 3 | 1 | 0 |
| Area, ethnic, cultural, gender, and group studies | 4 | 0 | 0 |
| Biological and biomedical sciences | 464 | 51 | 7 |
| Business | 33 | 26 | 0 |
| Communication, journalism, and related programs | 13 | 3 | 0 |
| Communications technologies | 2 | 0 | 0 |
| Computer and information sciences | 5 | 2 | 0 |
| Education | 52 | 21 | 4 |
| Engineering | 38 | 10 | 0 |
| Engineering technologies | 6 | 5 | 0 |
| English language and literature/letters | 5 | 0 | 0 |
| Environmental health | 213 | 90 | 9 |
| Environmental science | 218 | 66 | 1 |
| Family and consumer sciences/human sciences | 8 | 1 | 0 |
| Foreign languages, literature, and linguistics | 4 | 1 | 0 |
| Health professions and related programs | 45 | 25 | 4 |
| Homeland security, law enforcement, or firefighting | 2 | 1 | 0 |
| Legal professions and studies | 4 | 3 | 4 |
| Liberal arts and sciences, general studies, and humanities | 15 | 0 | 0 |
| Library science | 0 | 0 | 0 |
| Mathematics and statistics | 12 | 2 | 0 |
| Military technologies and applied sciences | 5 | 1 | 0 |
| Multi/interdisciplinary studies | 2 | 2 | 0 |
| Parks, recreation, leisure, and fitness studies | 6 | 0 | 0 |
| Philosophy and religious studies | 5 | 2 | 1 |
| Physical sciences and science technologies | 52 | 5 | 0 |
| Precision production | 0 | 0 | 0 |
| Psychology | 29 | 3 | 0 |
| Public administration and social services | 6 | 57 | 1 |
| Public health | 76 | 179 | 5 |
| Social sciences and history | 25 | 1 | 1 |
| Theology and religious vocations | 1 | 3 | 0 |
| Transportation and materials moving | 2 | 0 | 0 |
| Visual and performing arts | 4 | 0 | 0 |
| Other | 191 | 77 | 12 |
| Total | 1,241 | 663 | 52 |
Note. The survey allowed selection of two fields of study for each degree type. Of the respondents, 53 did not complete a college degree.
Practice
EH professionals had responsibilities in multiple programs (Table 3). The largest percentages of professionals worked in food safety and protection, public swimming pools, and emergency preparedness and response programs. Few EH professionals indicated that they spend 91–100% in one particular program. We also examined time spent in each program area, where the highest number of responses for spending essentially all of their time focused in one program were for food safety and protection (n = 50), public drinking water (n = 10), and onsite wastewater (n = 5). Approximately 17% of the respondents reported that in addition to EH-related work responsibilities, they also work with other health department programs. Of those EH professionals, 37% spent more than half of their time working in a non-EH program such as health education or immunization programs.
TABLE 3.
Percentage of Environmental Health Professionals Working in Various Programs in Health Departments in the United States (n = 1,735)
| Environmental Health Program | % |
|---|---|
| Food safety and protection | 76 |
| Public swimming pools | 57 |
| Emergency preparedness and response | 47 |
| Schools | 46 |
| Onsite wastewater (e.g., septic systems) | 44 |
| Private or onsite drinking water | 43 |
| Hotels/motels | 39 |
| Vector control | 38 |
| Body art (tattoo) | 36 |
| Day care/early child development facilities | 34 |
| Special events/mass gatherings | 31 |
| Campgrounds and recreational vehicles | 30 |
| Public drinking water systems | 28 |
| Lead prevention | 25 |
| Solid waste | 25 |
| Smoke-free ordinances | 24 |
| Children’s camps | 22 |
| Indoor air quality | 22 |
| Other recreational water (e.g., beaches) | 21 |
| Healthy homes | 20 |
| Mobile homes | 18 |
| Radon control | 17 |
| Animal control | 16 |
| Hazardous waste disposal | 16 |
| Land use planning | 16 |
| Pollution prevention | 14 |
| Health-related facilities | 13 |
| Outdoor air quality | 12 |
| Hazardous materials response | 11 |
| Tobacco retailers | 8 |
| Cosmetology businesses | 6 |
| Noise pollution | 6 |
| Collection of unused Pharmaceuticals | 5 |
| Injury prevention | 5 |
| Radiation control | 5 |
| Occupational health | 4 |
| Toxicology | 4 |
| Milk processing | 3 |
| Poison control | 2 |
| Other | 28 |
Leadership and Satisfaction
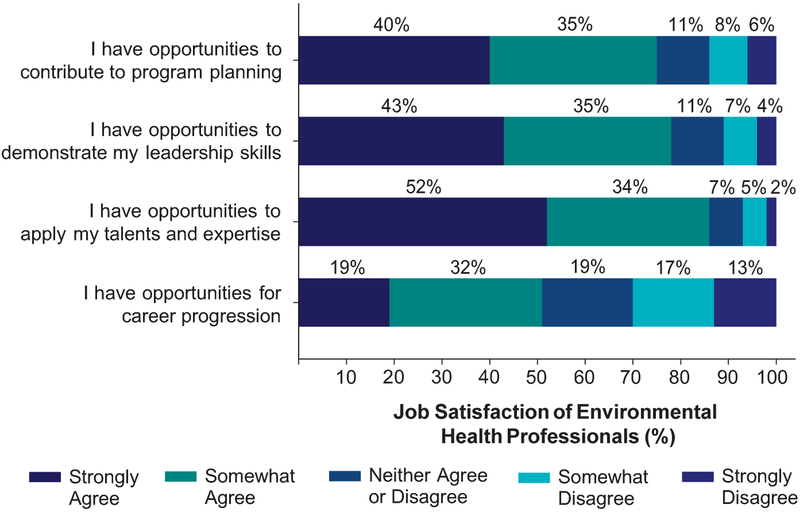
Most EH professionals occasionally or routinely engaged in leadership activities (Table 4). Problem solving and critical thinking was a routine activity for a large percentage of respondents (82%). Participating in community-based events drew the least engagement and most EH professionals strongly or somewhat agreed they have opportunities for professional development and making contributions to their programs (Figure 5). Nearly all respondents reported that leadership training is important for EH professionals (95%, n = 1,649) (data not shown).
TABLE 4.
Engagement in Leadership Activities of Environmental Health Professionals in Health Departments in the United States (n = 1,734)
| Leadership Activity | Routinely (%) | Sometimes (%) | Never (%) |
|---|---|---|---|
| Collaborating with other governmental agencies and staff | 53 | 41 | 6 |
| Collecting and analyzing data | 44 | 44 | 12 |
| Communicating risk to the public | 57 | 37 | 6 |
| Decision making that influences program planning | 47 | 39 | 14 |
| Evaluating the effectiveness of services and activities | 37 | 46 | 16 |
| Participating in community-based initiatives or events | 22 | 61 | 17 |
| Problem solving and critical thinking | 82 | 16 | 2 |
FIGURE 5.
Job Satisfaction Level of Environmental Health Professionals in Health Departments in the United States (N = 1,736)
Discussion
UNCOVER EH, a comprehensive and tailored assessment designed specifically for EH, provided a much-needed description of the current STLT health department EH workforce in the U.S. Such information will support future efforts for ensuring EH professionals are well equipped and prepared to meet the complex needs of tomorrow. Results presented in this article fill an important gap in the current understanding of the EH profession and practice.
Survey respondents provided a seemingly broad representation of the EH workforce, with some exceptions, including the limited representation of professionals from tribal and territorial health departments. Considering demographics, a disproportionately high percentage (86%) of EH professionals indicated their race as White. This number is slightly higher than recent observations among the broader state health agency workforce (ASTHO, 2017; Sellers et al., 2015). Those surveys also showed that females represented almost three quarters of the state health agency workforce. In contrast, our survey received responses from an almost even number of male and female respondents. These results might indicate that the EH workforce is slightly less diverse yet has a more balanced male-to-female ratio than the general public workforce, particularly at the state level.
Maintaining a sufficient workforce in light of retirements, and retaining and recruiting staff, is a recognized topic of concern among public health and EH managers (Hilliard & Boulton, 2012; Resnick et al., 2009). Approximately one half of the respondents had worked in their current jobs for ≤5 years and approximately one quarter had spent ≤5 years in the EH profession. At the mid-career range (16–20 years), respondents consistently had served longer in the EH profession than in their current position and agency. More than one half (54%) of the survey respondents were ≥46 years and more than one quarter (26%) were ≥56 years. Approximately one quarter (26%) of the EH professionals planned to retire within 5 years, which tends to align with our survey results indicating an aging EH workforce. The public health workforce as a whole, and other specific discipline areas such as public health nurses, face similar percentages of upcoming retirements (Beck & Boulton, 2016; Pourshaban, Basurto-Dávila, & Shih, 2015). Considering these trends, enhancing recruitment efforts and incentives will be essential for preserving the EH workforce and ensuring a sufficient supply of talented and skilled persons to enter the profession.
A workforce’s education and training, work setting, job titles, and functions are important criteria for defining a profession. These criteria are especially relevant for describing and enumerating the public health workforce (Gebbie & Merrill, 2001). Researchers have acknowledged significant challenges in identifying and classifying public health professionals among different settings and governmental levels, which is also realized for the EH workforce (Beck, Boulton, & Coronado, 2014; Massoudi, Blake, & Marcum, 2012). Though the objectives of this present study did not include EH workforce enumeration, our results show some consistency in various criteria pertaining to the STLT EH workforce. For example, more than one half of the respondents reported their job titles as environmental health specialist or sanitarian. A similar proportion possessed the registered environmental health specialist or registered sanitarian credential.
We saw less consistency, however, in the respondents’ field of study for college degrees. Most EH professionals did not receive formal undergraduate training in EH, which might hamper their ability to effectively deliver essential environmental public health services. Among respondents holding a bachelor’s degree, a small proportion identified EH as their field of study. Less than one half of those respondents who studied EH obtained their bachelor’s degree from an EHAC-accredited academic program.
EHAC accreditation indicates that an academic program meets stringent requirements, ensuring students receive education in the full range of EH science, with intentions of producing graduates ready to enter the practice (Fletcher, Aighewi, & Murphy, 2016; Marion & Murphy, 2016). As the leading accreditation body for EH academic programs, such observations present a decided opportunity to increase EH degrees granted by EHAC-accredited programs and thus increase capacity of the EH workforce. Regardless, our observations suggest the EH workforce includes professionals who have widely varied educational backgrounds, sometimes nonscience based, and who lack formal academic preparation in the EH sciences and practice. This finding reinforces the current need for workforce development and training opportunities to ensure EH professionals receive essential education in the general EH sciences and practice.
A high number of professionals with master’s degrees reported their field of study was EH, which might result from those EH professionals who lacked undergraduate preparation in the field seeking this specialization in their graduate studies. This finding could highlight the need to increase the availability of EH academic programs and encourage recruitment of their graduates to the STLT workforce. Additionally, attention could be given to ensure that those without an EH degree have access to advanced training in the EH practice. Increasing awareness of the opportunities associated with an EH career and the existence of accredited EH academic programs could be essential for equipping a workforce that has academic credentials specific to the profession.
The EH practice is multifaceted. Most EH professionals appear to fill the role of the generalist in their job function, with responsibilities in a range of programmatic areas. Respondents reported working in traditional EH programs, including food safety, private drinking water, and onsite wastewater, along with newer priority areas such as body art and enforcing smoke-free ordinances. Many EH professionals had responsibilities in areas such as vector control and emergency preparedness/response, which could reflect increased emphasis on response to natural disasters and emerging vectorborne diseases. Most respondents had opportunities to engage in leadership activities, think critically, and solve problems. Leadership training and guidance are essential for preparing EH professionals to address new and emerging challenges and guide continual transformation of the workforce (CDC, 2003).
Our findings confirm anecdotal evidence that EH professionals play an important role in protecting and promoting community health beyond traditional EH roles and responsibilities. We report here that 17% of respondents worked on public health efforts outside of EH, and of those, 37% spent more than half of their time in a non-EH program. In other words, about 5% of survey respondents reported spending more than half of their time working in non-EH functions. For many rural health departments, the EH professional likely represents the largest and most stable governmental public health workforce constituent. This condition likely arises from the fee-for-service nature of EH programming, which inherently provides staffing stability.
Most respondents (90%) reported they had completed training in the last year and an almost equal percentage received travel support to attend training, which indicates that EH professionals have access to training opportunities for up-to-date information on current EH topics, along with scientific and technological advances. At the same time, 95% of the respondents felt additional leadership training would be beneficial. EH professionals generally possess strong science educations, are working in programs outside their core responsibilities, and are likely to represent the majority of the workforce in smaller jurisdictions. These factors, in aggregate, make a compelling case to consider a national strategy to embed or dovetail leadership training within traditional training that tends to be more focused on regulatory enforcement.
It is important to note that this study focused on EH professionals practicing at STLT health departments. The EH profession extends beyond this setting to different governmental agencies with varying EH-related responsibilities (Burke, Shalauta, Tran, & Stern, 1997; Sexton & Perlin, 1990). Future assessments would improve our understanding of other EH professionals and the practice in other government agencies and areas such as the private sector. Although the survey respondents provided a relatively broad representation of the EH workforce, the survey results likely are not generalizable to the entire EH workforce.
Respondent selection and response biases can influence the representativeness of the study findings. These biases might result from nonresponse, not identifying EH professionals working in non-EH programs, including EH professionals not currently employed by a health department, and inadvertent inclusion of non-EH professionals in the respondent universe. This study was intended to provide a general description of EH professional and workforce characteristics. Future UNCOVER EH publications will include in-depth statistical analyses of various topics with intentions of determining how different characteristics might, for example, vary among EH professionals’ educational background and position level, along with health department size and governmental level.
Conclusion
UNCOVER EH is an essential step forward for assessing and understanding the EH workforce. The next phase of the UNCOVER EH initiative, which includes in-person focus groups and workshops, as well as upcoming publications, will delve deeper into current and emerging EH challenges and opportunities. This initiative will establish a primary source of EH workforce data that could be used to inform workforce development initiatives, support improvement of the practice, establish uniform benchmarks and professional competencies, and effectively allocate funds to support improvement of the practice.
The EH profession and practice is dynamic, plays a critical role in protecting public health, and must continue to evolve to meet future needs and challenges. To meet calls to enhance the public health workforce, such as those presented by Public Health 3.0 and the National Consortium for Public Health Workforce Development, the EH profession will be required to continually advance its approaches and strategic skills (DeSalvo et al., 2017; National Consortium for Public Health Workforce Development, 2017). Vigilant observation of EH practice trends is essential for maintaining a well-prepared and well-equipped workforce ready to meet tomorrow’s challenges.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of CDC.
Contributor Information
Justin A. Gerding, National Center for Environmental Health, Centers for Disease Control and Prevention.
Elizabeth Landeen, National Environmental Health Association.
Kaitlyn R. Kelly, Environmental Health Science Program, Department of Environmental Science, Institute of Biomedical Studies, Baylor University
Sandra Whitehead, National Environmental Health Association.
David T. Dyjack, National Environmental Health Association.
John Sarisky, National Center for Environmental Health, Centers for Disease Control and Prevention.
Bryan W. Brooks, Environmental Health Science Program, Department of Environmental Science, Institute of Biomedical Studies, Baylor University.
References
- Association of State and Territorial Health Officials. (2017). Profile of state and territorial public health, volume 4. Arlington, VA: Author; Retrieved from http://www.astho.org/Profile/Volume-Four/2016-ASTHO-Profile-of-State-and-Territorial-Public-Health/ [Google Scholar]
- Beck AJ, & Boulton ML (2016). The public health nurse workforce in U.S. state and local health departments, 2012. Public Health Reports, 131(1), 145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AJ, Boulton ML, & Coronado F (2014). Enumeration of the governmental public health workforce. American Journal of Preventive Medicine, 47(5 Suppl. 3), S306–S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulton ML, Beck AJ, Coronado F, Merrill JA, Friedman CP, Stamas GD, … Leep CJ (2014). Public health workforce taxonomy. American Journal of Preventive Medicine, 47(5 Suppl. 3), S314.–. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boxall AB, Rudd MA, Brooks BW, Caldwell DJ, Choi K, Hickmann S, … Van Der Kraak G (2012). Pharmaceuticals and personal care products in the environment: What are the big questions? Environmental Health Perspectives, 120(9), 1221–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke TA, Shalauta NM, Tran NL, & Stern BS (1997). The environmental web: A national profile of the state infrastructure for environmental health and protection. Journal of Public Health Management and Practice, 3(2), 1–12. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2003). A national strategy to revitalize environmental public health services. Atlanta, GA: Author; Retrieved from http://www.cdc.gov/nceh/ehs/docs/nationalstrategy2003.pdf [Google Scholar]
- DeSalvo KB, Wang CY, Harris A, Auerbach J, Koo D, & O’Carroll P (2017). Public health 3.0: A call to action for the public health to meet the challenges of the 21st century. Preventing Chronic Disease, 14, 170017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman DA (2007). Mail and Internet surveys: The tailored design method (2nd ed.). Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Dyjack DT, Case P, Marlow HJ, Soret S, & Montgomery S (2007). California’s county and city environmental health services delivery system. Journal of Environmental Health, 69 (8), 35–43. [PubMed] [Google Scholar]
- Fletcher MD, Aighewi IT, & Murphy TJ (2016). The value and benefits of an environmental health bachelor’s degree accredited by the National Environmental Health Science and Protection Accreditation Council for community college transfer students. Pedagogy in Health Promotion, 2(1), 78–82. [Google Scholar]
- Furley TH, Brodeur J, Silva de Assis HC, Carriquiriborde P, Chagas KR, Corrales J, … Brooks BW (2018). Towards sustainable environmental quality: Identifying priority research questions for Latin America. Integrated Environmental Assessment and Management, 14(3), 344–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebbie KM, & Merrill J (2001). Enumeration of the public health workforce: Developing a system. Journal of Public Health Management and Practice, 7(4), 8–16. [DOI] [PubMed] [Google Scholar]
- Gerding JA, Landeen E, & Brooks BW (2017). Understanding the needs, challenges, opportunities, vision, and emerging roles in environmental health. Journal of Environmental Health, 80(1), 36–37. [Google Scholar]
- Hilliard TM, & Boulton ML (2012). Public health workforce research in review: A 25-year retrospective. American Journal of Preventive Medicine, 42(5 Suppl. 1), S17–S28. [DOI] [PubMed] [Google Scholar]
- Marion JW, & Murphy TJ (2016). A fork in the road for environmental health workforce development and U.S. public health. Journal of Environmental Health, 79(2), 40–43. [PubMed] [Google Scholar]
- Massoudi M, Blake R, & Marcum L (2012). Enumerating the environmental public health workforce—Challenges and opportunities. Journal of Environmental Health, 75(4), 34–36. [PubMed] [Google Scholar]
- National Association of County and City Health Officials. (2017). 2016 national profile of local health departments. Retrieved from http://nacchoprofilestudy.org/wp-content/uploads/2017/10/ProfileReport_Aug2017_final.pdf
- National Consortium for Public Health Workforce Development. (2017). Building skills for a more strategic health workforce: A call to action. Retrieved from https://www.debeaumont.org/building-skills-for-a-more-strategic-health-workforce-a-call-to-action/
- National Environmental Health Association. (2013). New perspectives on environmental health: The approval of new definitions. Journal of Environmental Health, 76(3), 72–73. Retrieved from http://www.neha.org/sites/default/files/publications/positionpapers/NEHA_Adopted_EH_Definition_July_2013.pdf [PubMed] [Google Scholar]
- National Environmental Health Association Committee on the Future of Environmental Health. (1993). The future of environmental health: Part 1. Journal of Environmental Health, 55(4), 28–32. [Google Scholar]
- National Environmental Health Partnership Council. (2017). Environmental health playbook: Investing in a robust environmental health system. Retrieved from https://apha.org/-/media/files/pdf/topics/environment/eh_playbook.ashx?la=en&hash=FBAE72B837D58A3C3145602B1043250DE7BD41BD
- Pourshaban D, Basurto-Dávila R, & Shih M (2015). Building and sustaining strong public health agencies: Determinants of workforce turnover. Journal of Public Health Management and Practice, 21(Suppl. 6), S80–S90. [DOI] [PubMed] [Google Scholar]
- Resnick BA, Zablotsky J, & Burke TA (2009). Protecting and promoting the nation’s health: The environmental public health workforce as a critical component. Journal of Public Health Management and Practice, 15(Suppl. 6), S40–S45. [DOI] [PubMed] [Google Scholar]
- Sellers K, Leider JP, Harper E, Castrucci BC, Bharthapudi K, Liss-Levinson R, … Hunter EL (2015). The public health workforce interests and needs survey: The first national survey of state health agency employees. Journal of Public Health Management and Practice, 21(Suppl. 6), S13.–. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton K, & Perlin SA (1990). The federal environmental health workforce in the United States. American Journal of Public Health, 80(8), 913–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Public Health Service. (1997). The public health workforce: An agenda for the 21st century: A report of the Public Health Functions Project. Washington, DC: Author. [Google Scholar]
- U.S. Department of Health, Education, and Welfare, Public Health Service. (1963). Sanitarians In Health manpower sourcebook. Washington, DC: Author. [Google Scholar]
- Van den Brink PJ, Boxall ABA, Maltby L, Brooks BW, Rudd MA, Backhaus T, … van Wensem J (2018). Towards sustainable environmental quality: Priority research questions for Europe. Environmental Toxicology and Chemistry, 37(9), 2281–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]