Abstract
OBJECTIVE:
Few studies have examined ankylosing spondylitis (AS) patients’ concerns and perceptions of biologic therapies outside of traditional surveys. In this study, we used social media data to examine AS patients’ knowledge, attitudes, and beliefs regarding biologic therapies.
METHODS:
We collected posts from 601 social media sites made between 1/1/06–4/26/17. Each post mentioned both an AS keyword and a biologic. To explore themes within the collection in an unsupervised manner, a latent Dirichlet allocation topic model was fit to the dataset. Each discovered topic was represented as a discrete distribution over the words in the collection, similar to a word cloud. The topics were manually reviewed to identify themes, which were confirmed with thematic data analysis.
RESULTS:
We examined 27,416 social media posts and found 112 themes. The majority of themes (60%, 67/112) focused on discussions surrounding AS treatment. Other themes including psychological impact of AS, reporting of medical literature, and AS disease consequences accounted for the remaining 40% (45/112). Within AS treatment discussions, most topics (54%) involved biologics, and most subthemes (78%) centered on side-effects (e.g., fatigue, allergic reactions), biologic attributes (e.g., dosing, frequency), and concerns with biologic use (e.g., increased cancer risk). Additional implicit patient needs (e.g., support) were identified using qualitative analyses.
CONCLUSION:
Social media reveals a dynamic range of themes governing AS patients’ experience and choice with biologics. The complexity of selecting among biologics and navigating their risk-benefit profiles suggests merit in creating online tailored decision-tools to support patients’ decision-making with AS biologic therapies.
INTRODUCTION
Conventional therapies used to treat ankylosing spondylitis (AS), such as non-steroidal anti-inflammatory drugs (NSAIDs), commonly fail to bring results in patients with moderate to severe AS. This, along with the non-response and dependence on corticosteroids, has spawned increased development of biological therapies, which neutralize pro-inflammatory cytokines, and thus attempt to go beyond simply managing symptoms by preventing the long-term sequelae of AS.(1) Over the past few decades many new medications have come on the market for AS, and several promising “pipeline” therapies are being evaluated in various phases of clinical investigation. For example, tumor necrosis factor (TNF)-inhibitors have been shown to effectively reduce symptoms of AS and improve spinal mobility.(2, 3) More recently, a biologic targeting interleukin (IL) 17A has also been found to be effective and approved for use in AS.(4)
Yet, despite their benefits, some biologics are associated with important side effects, including potentially increasing the risk for serious infections, cancer, and immunologic reactions, among others. With the complex risk-benefit profiles of the different biologics along with the increasing number of clinically-available therapies in AS, it is becoming more difficult for patients to make informed decisions when choosing among the various options. As a result, approximately 40–60% of AS patients have never used biologics in their lifetime (5, 6).
Thus far, few attempts have been made to examine patients’ concerns and perceptions of these therapies outside of traditional surveys and cognitive interviews.(7, 8) To address this gap, we used a novel research method known as social netnography – a type of ethnography that analyzes the free behavior of individuals on the Internet.(9) Specifically, in this study, we used social media data to examine AS patients’ concerns and perceptions regarding biologic therapies through a mixed-method approach. In contrast to traditional qualitative methods such as focus groups and interviews, social netnography allows for a wide sampling pattern and provides a contextually-based study of unfiltered, free-flowing conversations which may more reliably generalize to the AS population at large.(10)
MATERIALS AND METHODS
Data Collection
We collaborated with researchers from Treato (www.treato.com), a social media data mining service, to extract relevant social media and e-forum data. Treato automatically collects, indexes, and analyzes patient and caregiver content from over 10,000 U.S.- and international-based websites, forums, blogs, and communities such as Spondylitis.org, KickAS.org, Facebook.com, and Twitter.com, among many others. Posts are indexed using a lexicon of over 100,000 medical terms (based on the Unified Medical Language System), and a built-for-purpose “patient language” dictionary manually created by Treato researchers.(11) They then use proprietary natural language processing (NLP) classification algorithms to index posts with this lexicon; this results in an easily searched dataset that can be analyzed in aggregate.(11)
Treato extracted relevant posts from their database using a set of keywords validated by domain experts on the research team. All posts were written in English and published online between January 1, 2006 and April 26, 2017. The keyword search list included two categories: AS keywords and biologics. The AS keywords category included names, abbreviations, and common misspellings for AS. We also identified posts with “AS” containing phrases (e.g., “diagnosed with AS”, “treats my AS”) as well as those made on AS-dedicated sites (e.g., Spondylitis.org, KickAS.org) or Facebook groups. The biologics category included brand and generic names for biologics and biosimilars used to treat AS. Table 1 contains a complete list of the keywords used along with the data extraction strategy. Posts were selected for analysis if they met criteria for AS and included a keyword from the biologics category (Boolean search: AS keyword AND biologic).
TABLE 1.
Full list of keywords and data extraction strategy used by Treato.
| Ankylosing spondylitis keywords |
|
| Biologic medications | “biologic” “biologics” “biologicals” “biological drugs” “biological drug” “tnf inhibitor” “tnf inhibitors” “TNFs” “TNF's” “Tumor Necrosis Factor Inhibiting Agents” “TNF blocker” “TNF drugs” “TNF drug” “DMARD TNF” “TNF alpha blocker” “TNF blockers” “TNF alpha blockers” “TNF antagonist” “TNF antagonists” “TNF antibody” “TNF antibodies” “tnfinihibitor”) “Humira” “humra” “Humaria” “Humera” “humria” “hmira” “adalimumab” “adlimumab” “adalimuamb” “Enbrel” “Enbel” “Enbrels” “Embrel” “embril” “Enbral” “Enbrell” “enbril” “Enebrel” “ennbrel” “enbrl” “etanercept” “etenercept” “etancercept” “Simponi” “smponi” “simpony” “symponi” “symponi aria” “golimumab” “galimumab” “glimumab” “Cimzia” “cmzia” “simzia” “cimza” “certolizumab” “certolizumabpegol” “Remicade” “Remicad” “remicaide” “remcaide” “Remicaid” “infliximab” “inflixmab” “Inflectra” “adalimumabatto” “attoadalimumab” “erelzi” “Amjevita” basic_concepts:F0020905 “Cosentyx” “cosentix” “cosintyx” “Secukinumab” “AIN 457” “AIN457” “il-17a” “il17a” “il17” (“biosimilar” “biosimilars” “bio similar” “bio similars” “biogeneric” “biogenerics” “bio generic” “generic versions of a biological” “generic version of biological” “GENERIC BIOLOGICal” “adalimumabatto” “attoadalimumab” |
Quantitative Methods
To explore themes within the collection in an unsupervised manner, a latent Dirichlet allocation (LDA) topic model was fit to the dataset. Under LDA, each discovered topic is represented as a discrete distribution over the words in the collection, which may be thought of as a word cloud (i.e., words with more probability are larger in the cloud). Topics were manually examined by an expert panel of medical professionals and researchers and grouped into categories and subcategories based on keyword content. The grouping was confirmed with a sample of a posts most representative of each topic. Each primary category consisted of at least one subcategory identified as a specific theme within the topic.
LDA alpha hyperparameters were estimated, representing the relative sparsity of data such that lower values indicate topics occurring less often throughout the data. Topics sharing common primary categories were aggregated and the sums of the alpha hyperparameters were used as an approximate measure of the importance of a topic relative to the number of times they were identified (i.e., sparsity). Topics with a cumulative sparsity greater than 1.0 were separated into the next lowest subcategory; the process was repeated until all categories had sparsity parameters less than 1.0.
Qualitative Methods
In addition to our quantitative analysis, we adopted a qualitative approach to understand, in-depth, patients’ perceptions regarding biologic therapies in AS. The thematic data analysis helps us understand meanings and interpretations given to AS treatment – a prevalent category that was identified in the first round of our quantitative analysis.
Social media posts that focused on AS treatment and biologics were analyzed based on an inductive open-coding approach. We assigned a reader to examine social media posts multiple times before the coding process. Throughout reading, data texts were divided into distinctive meaning units or codes. Each unit or code communicates sufficient information for the reader even without the context. Hence, numerous codes were defined and illustrated by text fragments. As different inductive codes emerge, they were regrouped into defined categories with more specific meanings. Additionally, these categories were iteratively revised and refined throughout the analysis process. While some categories were combined, others were linked under a superordinate category when the meanings were similar. This reduced redundancy among the categories, similar to the quantitative data analysis approach. Therefore, categories were conceptualized onto broader themes and links between them were created. The thematic data analysis was presented with verbatim quotes and therefore spelling or grammatical issues were in context.
Institutional Review Board Approval and Ethical Considerations
This study was reviewed by the Cedars-Sinai Medical Center Institutional Review Board (Pro46580) and it was deemed exempt from review, as it did not meet the definition of “human subject research” under Department of Health and Human Services or U.S. Food and Drug Administration regulations.
RESULTS
Quantitative Analysis: Main Themes Identified by Topic Modeling
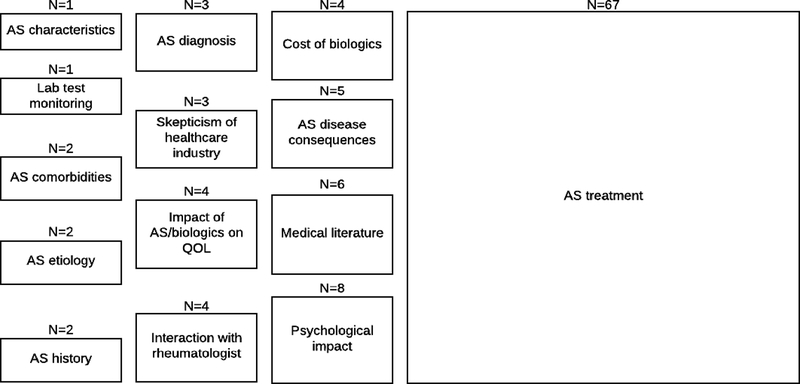
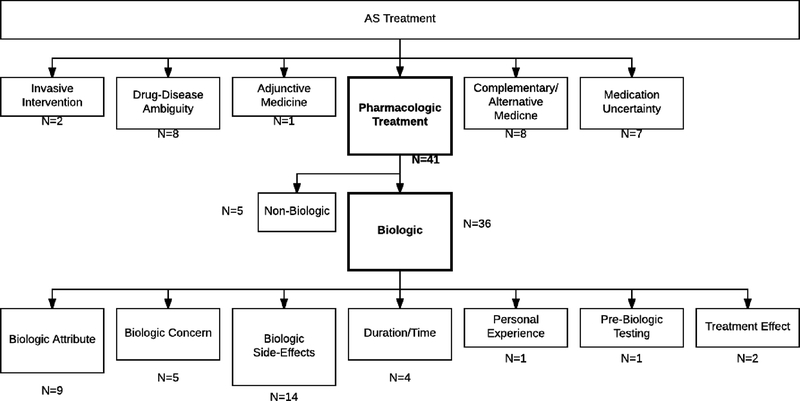
We examined 27,416 social media posts made between January 1, 2006 and April 26, 2017 that focused on AS and biologics and found 112 main themes (Figure 1). The posts were made by 13,262 users resulting in a median of one post per user, with 1,210 users having more than one post, and 27 of those users having more than 100 posts. Of those posters, only one had more than 1,000 posts. The majority of themes (60%, 67/112) focused on discussions surrounding AS treatment. Other main themes including psychological impact of AS, reporting of medical literature, and AS disease consequences, among others, accounted for the remaining 40% (45/112) of topics. Figure 2 depicts the main themes within the AS treatment category, and most topics (61%, 41/67) involved discussions about pharmacologic treatment (biologic [n=36] and non-biologic options [n=5]). Within biologics, 78% (28/36) of the identified subthemes centered on side-effects related to its use (e.g., fatigue, allergic reactions), biologic attributes (e.g., dosing, frequency), and concerns with its use (e.g., increased cancer risk, reproductive concerns).
FIGURE 1.
Primary patient discussion themes identified by topic modeling. Note: Size of individual boxes represents relative prevalence of theme.
FIGURE 2.
Main themes within AS treatment identified by topic modeling. Note: Size of individual boxes represents relative prevalence of theme. Boxes in bolded font emerged as predominant subthemes.
Quantitative Analysis: Topic Sparsity Assessment
As each post can contain multiple themes, we conducted a topic sparsity assessment. After adjusting for topic sparsity, 49% of text consisted of content concerning the following six topics: (i) medication uncertainty, (ii) psychosocial impact, (iii) duration/time of biologic treatment, (iv) interactions with rheumatologists, (v) attributes of biologics, and (vi) personal experience with pharmacological treatment of AS. The remaining 51% of the text consisted of content related to the remaining 106 themes.
Qualitative Analysis
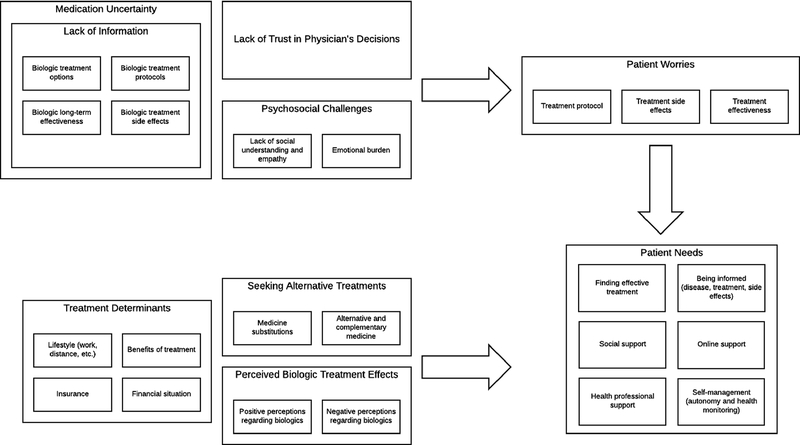
In our qualitative analysis, eight inductive categorical groups were identified related to AS treatments and biologics (Figure 3): (i) medication uncertainty and lack of information, (ii) lack of trust in physician decisions, (iii) psychosocial challenges, (iv) patient worries, (v) perceived biologic effects, (vi) biologic substitutions, (vii) perceived treatment determinants, and (viii) seeking alternative treatments.
FIGURE 3.
Thematic data analysis based on predominant themes from topic models.
While most of the identified topics were similar to those found with topic modeling, an additional important category group emerged in our open-coding analysis – patient needs – that was not identified in the quantitative analysis. Needs of patients were often expressed explicitly as advice from the community across domains such as information seeking, support seeking, and self-management (e.g., “I was just searching for support chats”; “you should discuss biologics with your rheumy”; “If you are still able to control your symptoms at this point, do not rush to start a strong medicine like [Biologic X]”). More often, however, such information could be derived from discussions in the AS community about medication uncertainty and determining treatment.
The thematic data analysis found three primary challenges patients with AS face in their everyday lives in the domains of understanding a complex treatment regimen, communicating with their provider, and coping with intrapersonal and interpersonal struggles. First, a broad theme of uncertainty with the use of medication was expressed primarily as lack of information about a variety of topics related to biologics. Patients often lacked information regarding biologic treatment options (e.g., “I don’t know much about all the options available”). Others reported not being familiar with medication protocols such as the dosage and length of treatment (e.g., “should I take [Biologic X] once a week instead of every other week?”). A lack of familiarity with medication side effects was reported, especially among individuals not yet starting treatment (e.g., “I am just scared about injecting my body with something I am unsure about…I am unsure what to do”). Among individuals who had started biologics, apprehension regarding their long-term effectiveness were prevalent (e.g., “have any of you found that all of the biologics just don’t last long enough”).
Second, patients expressed distrust in their physicians’ decisions (e.g., “How would my rheumy know what biologic would work on me?”). Such concerns often escalated to eliciting medical advice from online communities (e.g., “do you think I should try switching my medicine?”). Third, psychological and social challenges were expressed as the inability of friends and family to empathize with the symptoms of AS, even in the presence of support (e.g., “I have amazing support from my family but really no one understands unless they can spend a day in [my] body”).
Patients reported internal struggles, often recognizing depressive symptoms, and in some cases, suicidality (e.g., “I am losing the will to live with AS”). Given lack of information about biologics, trust in physicians, and empathy from others, patients with AS find themselves online seeking information, advice and support from their peers in similar situations to assuage their concerns. Patients expressed worries about protocols (e.g., “I understand from previous discussions that [Biologic X] has more room for dosage customization”), side effects (e.g., “I worry that I may trade two bad days for a week or two”), and the effectiveness of treatments (e.g., “I notice a lot of folks switch biologics due to losing effectiveness”).
Additional thematic data analysis also revealed discussions regarding determining a course of treatment that balances patient lifestyle with their desires to be pain free. Some patients expressed efficacy of biologics (e.g., “I am on [Biologic X]…so far it has helped out lots able to work again”), however numerous posts featured dissatisfaction due to poor efficacy and other factors (e.g., “Biologics never helped and made me sick”). Other treatment determinants included impact on patient lifestyle (e.g., “One reason I choose [Biologic X] for the once a month dosing is travel”) and financial and insurance issues (e.g., “there is a process to go through first to make sure that the cheaper drugs are not effective”). As alternatives to biologics, patients discussed pharmacological treatments such as corticosteroids, narcotics, and neuromuscular medicine in relieving pain. The discussions concerning alternatives also highlighted the role of complementary and alternative medicine such as chiropractor visits and acupuncture in helping patients with AS. In addition, the analysis revealed that alternative practices and physical activities such as ultrasound, exercising, as well as using ice and heat, were perceived as beneficial for patients with AS.
DISCUSSION
Social netnography analysis reveals a wide range of themes governing AS patients’ knowledge, attitudes, and beliefs regarding biologics. Using over 27,000 posts made by patients with AS on social media and health-related websites, we identified and grouped common themes among related posts, quantitatively examined the prevalence of each theme, and qualitatively generated themes with sample posts using thematic data analysis. Our approach leveraged data science and human insights to explore a large repository of social media posts both thoroughly and efficiently.
This is the first study, of which we are aware, that employed a mixed-methods approach using large-scale, social media data to examine AS patients’ concerns and perceptions of biologic therapies. The study provides novel insight on patient experiences with biologics and identifies actionable needs that may improve their quality of life. The findings also highlight the distinct, yet related contributions of topic modeling and thematic data analysis to examining health-related social media posts. While quantitative approaches identified a greater variety of topics and more subcategories, they did not provide relational information between posts. In contrast, qualitative approaches were limited in the number of identified categories, but integrated each topic as part of a larger relational model. Moreover, qualitative approaches identified patient needs, an implicit category with high utility due to its actionable subtopics.
As expected, topic modeling found that patients predominantly discussed biologics as treatment for their AS, often posting about and seeking information concerning side effects and other personal experiences with biologics. Topics derived from discussions about biologics indicate that these discussions may refer to attributes of biologics that vary patient to patient based on preferences. For instance, some patients may be able to tolerate certain side effects given better treatment effects and more convenient dosage schedules. Conversely, other patients may want to avoid side effects at all costs, even at the expense of reduced efficacy and less convenient dosing regimens. These findings suggest that conjoint analysis, a survey methodology often used in market research to determine consumer preferences for products, may be adapted as a decision-support tool for patients. In our prior research, we employed conjoint analysis to examine how those with inflammatory bowel disease (IBD) approached biologic decision-making and how they balanced efficacy, side effect profiles, and mode of administration, among other characteristics.(12) Here, we found that the biologic decision-making process was highly personalized and that demographic and disease characteristics poorly predicted individual patient preferences. Because of this finding, we used the conjoint analysis developed and tested in the study to support an online decision aid called “IBD&me” (www.ibdandme.org). The website uses conjoint analysis to quantify and rank the biologic attributes that drive an individual patient’s decision-making preferences, which may help improve shared decision-making between the patient and clinician, and optimize biologic selection in a more personalized and structured manner. The same highly-individualized approach to selecting a biologic therapy seen in IBD may also be seen in AS, but that must be formally tested and is the subject of our future research.
In our analyses, we also found that discussions regarding medication uncertainty were highly prevalent in the examined posts. Moreover, we discovered that many individuals expressed a lack of trust in their physicians’ treatment recommendations and even turned to their online peers with questions and to seek validation. Yet, the quality and accuracy of AS information obtained through social media and other online forums is largely unknown. In IBD, investigators noted that the quality of IBD websites varied widely, with many that are too difficult to comprehend or contained out of date information.(13–17) The same is likely to be found for AS-focused social media sites and e-forums. As the number of individuals going online seeking AS-specific information will only continue to grow,(18) informed stakeholders (e.g., healthcare providers, patient advocacy societies, professional societies) should increase their presence in social media to improve the quality and accuracy of online AS- and biologics-related information.
Prior studies examining patients’ experiences with biologics were consistent with results from our study. For instance, lack of information, especially about biologic treatment, has been identified in a similar study among Italian rheumatoid arthritis patients. Even though nearly all patients reported satisfaction about disease-specific information, only approximately a third of patients reported satisfaction with treatment information, indicating they would turn to other sources such as the Internet to meet their needs (19). More importantly, a study using Internet-based surveys among patients suffering from chronic inflammatory rheumatic diseases demonstrated that treatment history, negative beliefs about treatment, and lack of perceived medical and social support were three determinants of self-discontinuation that were also identified in our analyses. Additionally, the same study found that pain and self-administration of injections predicted discontinuation, which were specific examples of treatment side effects and treatment protocol, respectively(20). Further, a study of patients with inflammatory arthritis found that individuals were significantly influenced by their social support network with respect to treatment decision-making related to biologics, reflecting our findings regarding the needs of patients to establish social support and an online support(8).
Our study has important limitations. First, the study may be limited in generalizability due to the nature of social media posts as a platform where some posters may yield a relatively large share of the discussions. Still, the posts obtained for this study were made by over 13,000 users, included a highly diverse number of posters, and was not overly dominated by a few individuals. Second, the study can only be generalized to individuals with AS who also use social media. Although we do not have a true estimate of this distribution, approximately 88% percent of individuals under the age of 30 and 80% under the age of 49 use social media.(21) Hence, the use of social media as a source of data could be especially relevant for newly diagnosed patients, as onset is usually before the age of 30 and rarely after the age of 40.(22) Third, given that the inclusion criteria for posts required some mention of a biologic, discussions related to biologics were overrepresented and may not generalize to patients who choose to treat AS using non-biologic options. Finally, there also may have been patient misclassification, as we did not confirm AS diagnoses or have access to linked ICD-10 codes. However, many prior studies evaluating the reliability of self-reported diagnoses of chronic diseases have found high validity of such self-reports.(23–28) Furthermore, AS is a specific diagnosis made by healthcare providers, and our study specifically focused on biologic therapies used in AS.
In summary, social media reveals a dynamic range of themes governing AS patients’ experience and choice with biologics. The findings in this study can help researchers and clinicians anticipate the needs of patients with AS, as well as provide insight into thoughts and concerns some patients may have throughout the course of their treatment. Moreover, these findings highlight the complexity that AS patients face when selecting among the biologic options. With the increasing number of biologic therapies available to those with AS, further research and development of online decision tools that support them in selecting a therapy that fits their treatment needs and lifestyle are warranted.
SIGNIFICANCE AND INNOVATION:
The study used innovative social netnography techniques to reveal ankylosing spondylitis patients’ concerns and perceptions regarding biologic therapies.
Patients had a continuum of preference for side effects and treatment effects throughout the online discussions, suggesting that clinical decision-making tools may be useful to help patients identify biologic therapies that meet their treatment and lifestyle needs.
Medication uncertainty and information seeking identified by the mixed methods approach suggests the need for greater presence of informed stakeholders (i.e., clinicians, patient advocacy societies, professional societies) on social media.
GRANT SUPPORT:
This study was funded by Novartis Pharmaceuticals Corporation. The Cedars-Sinai Center for Outcomes Research and Education (CS-CORE) is supported by The Marc and Sheri Rapaport Fund for Digital Health Sciences & Precision Health. Dr. Almario is supported by a career development award from the American College of Gastroenterology. Drs. Almario, Ishimori, Arnold, and Spiegel were supported by a NIH/National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881.
Footnotes
DISCLOSURES: Dr. Park is an employee of Novartis Pharmaceuticals Corporation. The remaining authors do not have any relevant disclosures.
REFERENCES
- 1.Bruner V, Atteno M, Spano A, Scarpa R, Peluso R. Biological therapies for spondyloarthritis. Therapeutic advances in musculoskeletal disease 2014;6(3):92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marzo-Ortega H, McGonagle D, O’Connor P, Emery P. Efficacy of etanercept in the treatment of the entheseal pathology in resistant spondylarthropathy: a clinical and magnetic resonance imaging study. Arthritis and rheumatism 2001;44(9):2112–7. [DOI] [PubMed] [Google Scholar]
- 3.Poddubnyy D, Rudwaleit M, Haibel H, Listing J, Marker-Hermann E, Zeidler H, et al. Rates and predictors of radiographic sacroiliitis progression over 2 years in patients with axial spondyloarthritis. Annals of the rheumatic diseases 2011;70(8):1369–74. [DOI] [PubMed] [Google Scholar]
- 4.Braun J, Baraliakos X, Deodhar A, Baeten D, Sieper J, Emery P, et al. Effect of secukinumab on clinical and radiographic outcomes in ankylosing spondylitis: 2-year results from the randomised phase III MEASURE 1 study. Annals of the rheumatic diseases 2017;76(6):1070–7. [DOI] [PubMed] [Google Scholar]
- 5.Jones GT, Dean LE, Basu N, Kay L, Pathan E, Sturrock RD, et al. 224. The British Society for Rheumatology Biologics Register for Ankylosing Spondylitis: Characteristics of Study Participants. Rheumatology 2015;54(suppl_1):i136–i. [Google Scholar]
- 6.Wallis D, Haroon N, Ayearst R, Carty A, Inman RD. Ankylosing spondylitis and nonradiographic axial spondyloarthritis: part of a common spectrum or distinct diseases? The Journal of rheumatology 2013:jrheum. 130588. [DOI] [PubMed] [Google Scholar]
- 7.Bolge SC, Eldridge HM, Lofland JH, Ravin C, Hart PJ, Ingham MP. Patient experience with intravenous biologic therapies for ankylosing spondylitis, Crohn’s disease, psoriatic arthritis, psoriasis, rheumatoid arthritis, and ulcerative colitis. Patient preference and adherence 2017;11:661–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hart RI, Foster HE, McDonagh JE, Thompson B, Kay L, Myers A, et al. Young people’s decisions about biologic therapies: who influences them and how? Rheumatology (Oxford, England). 2015;54(7):1294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bowler GM. Netnography: A Method Specifically Designed to Study Cultures and Communities Online. The Qualitative Report 2010;15(5):1270–5. [Google Scholar]
- 10.Martinez B, Dailey F, Almario CV, Keller MS, Desai M, Dupuy T, et al. Patient Understanding of the Risks and Benefits of Biologic Therapies in Inflammatory Bowel Disease: Insights from a Large-scale Analysis of Social Media Platforms. Inflammatory bowel diseases 2017;23(7):1057–64. [DOI] [PubMed] [Google Scholar]
- 11.Whitman CB, Reid MW, Arnold C, Patel H, Ursos L, Sa’adon R, et al. Balancing opioid-induced gastrointestinal side effects with pain management: Insights from the online community. Journal of opioid management 2015;11(5):383–91. [DOI] [PubMed] [Google Scholar]
- 12.Almario C, Keller M, Mosadeghi S, Martinez B, Whitman C, Lasch K, et al. Examining Patient Decision-Making Surrounding Biologic Therapies in Inflammatory Bowel Disease: Insights from a Conjoint Analysis Survey. American College of Gastroenterology Annual Meeting. Las Vegas, NV; 2016. [Google Scholar]
- 13.Bernard A, Langille M, Hughes S, Rose C, Leddin D, Veldhuyzen van Zanten S. A systematic review of patient inflammatory bowel disease information resources on the World Wide Web. The American journal of gastroenterology 2007;102(9):2070–7. [DOI] [PubMed] [Google Scholar]
- 14.Langille M, Bernard A, Rodgers C, Hughes S, Leddin D, van Zanten SV. Systematic review of the quality of patient information on the internet regarding inflammatory bowel disease treatments. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2010;8(4):322–8. [DOI] [PubMed] [Google Scholar]
- 15.Mukewar S, Mani P, Wu X, Lopez R, Shen B. YouTube and inflammatory bowel disease. Journal of Crohn’s & colitis 2013;7(5):392–402. [DOI] [PubMed] [Google Scholar]
- 16.Promislow S, Walker JR, Taheri M, Bernstein CN. How well does the Internet answer patients’ questions about inflammatory bowel disease? Canadian journal of gastroenterology = Journal canadien de gastroenterologie 2010;24(11):671–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Marel S, Duijvestein M, Hardwick JC, van den Brink GR, Veenendaal R, Hommes DW, et al. Quality of web-based information on inflammatory bowel diseases. Inflammatory bowel diseases 2009;15(12):1891–6. [DOI] [PubMed] [Google Scholar]
- 18.Cooksey R, Brophy S, Husain MJ, Irvine E, Davies H, Siebert S. The information needs of people living with ankylosing spondylitis: a questionnaire survey. BMC musculoskeletal disorders 2012;13:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giacomelli R, Gorla R, Trotta F, Tirri R, Grassi W, Bazzichi L, et al. Quality of life and unmet needs in patients with inflammatory arthropathies: results from the multicentre, observational RAPSODIA study. Rheumatology 2014;54(5):792–7. [DOI] [PubMed] [Google Scholar]
- 20.Betegnie A-L, Gauchet A, Lehmann A, Grange L, Roustit M, Baudrant M, et al. Why do patients with chronic inflammatory rheumatic diseases discontinue their biologics? An assessment of patients’ adherence using a self-report questionnaire. The Journal of rheumatology 2016;43(4):724–30. [DOI] [PubMed] [Google Scholar]
- 21.Pew Research Center. Social Media Fact Sheet 2017 2017-January-12 [cited; Available from: http://www.pewinternet.org/fact-sheet/social-media/
- 22.Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A. Ankylosing spondylitis: an overview. Annals of the rheumatic diseases. 2002;61 Suppl 3:iii8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barisic A, Glendon G, Weerasooriya N, Andrulis IL, Knight JA. Accuracy of Self-Reported Breast Cancer Information among Women from the Ontario Site of the Breast Cancer Family Registry. J Cancer Epidemiol 2012;2012:310804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta V, Gu K, Chen Z, Lu W, Shu XO, Zheng Y. Concordance of self-reported and medical chart information on cancer diagnosis and treatment. BMC Med Res Methodol. 2011;11:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Irving SA, Donahue JG, Shay DK, Ellis-Coyle TL, Belongia EA. Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine 2009;27(47):6546–9. [DOI] [PubMed] [Google Scholar]
- 26.Klein BE, Lee KE, Moss SE, Trentham-Dietz A, Klein R. Self- and registry-reported cancer in a population-based longitudinal study. WMJ 2010;109(5):261–6. [PMC free article] [PubMed] [Google Scholar]
- 27.McCarthy AM, McGuire E, Bristol M, Fredricks T, Domchek SM, Armstrong K. Agreement of self-reported hormone receptor status with cancer registry data in young breast cancer patients. Cancer Epidemiol 2013;37(5):601–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Overbeek A, van den Berg MH, Hukkelhoven CW, Kremer LC, van den Heuvel-Eibrink MM, Tissing WJ, et al. Validity of self-reported data on pregnancies for childhood cancer survivors: a comparison with data from a nationwide population-based registry. Hum Reprod 2013;28(3):819–27. [DOI] [PubMed] [Google Scholar]