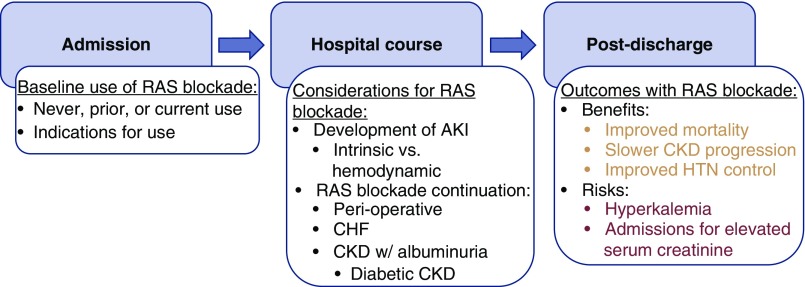
Renin-angiotensin system (RAS) blockade has been associated with improved outcomes in numerous disease states, including reduced mortality in congestive heart failure (CHF), hypertension, and diabetes (1,2). RAS blockade remains central to the management of both cardiovascular disease and CKD, particularly diabetic CKD. For patients with hypertension and CKD complicated by albuminuria, RAS blockade is recommended as first-line therapy to control BP and slow disease progression (3). The management of RAS blockade in patients who are hospitalized remains a topic of ongoing research. Topics of continued controversy include continuation of RAS blockade in the perioperative setting, timely discontinuation of RAS blockade before cardiac surgery or cardiac catheterization, and the timing of either initiation or resumption of previously prescribed RAS blockade after AKI, a common dilemma in the hospitalized setting (Figure 1) (4,5).
Figure 1.
RAS blockade in patients before, during, and after hospitalization. CHF, congestive heart failure; HTN, hypertension; RAS, renin-angiotensin system.
Patients who develop AKI are at high risk for subsequent CKD, cardiovascular disease, and mortality. Further, the risks of mortality and CKD progression may increase with recurrent AKI episodes (6). The use of angiotensin-converting enzyme inhibitors (ACE-I) or angiotensin receptor blockers (ARB) to prevent or slow the progression of CKD after AKI often competes with the concern for recurrent AKI. Given these concerns, therefore, Hsu et al. (7) investigate the critically important question of recurrent AKI risk with RAS blockade. They used data from the Kaiser Permanente healthcare delivery system to explore these associations in patients who notably did not have prior heart failure and who were not exposed to either ACE-I or ARB therapy up to 5 years before their index hospitalization. Despite these exclusions, the authors observed 47% of patients either had a documented eGFR <60 ml/min per 1.73 m2 or proteinuria before index hospitalization. In total, 18% of the 10,242 patients in their final analytic population were initiated on RAS blockade. They observed a recurrent AKI rate of 5.7 per 100 person-years in patients while receiving RAS blockade compared with 6.1 per 100 person-years in patients while not receiving RAS blockade. This difference was non-significant after adjustment for time-dependent confounders and time-varying ACE-I/ARB use (adjusted odds ratio, 0.71; 95% CI, 0.45 to 1.12).
Although initiation of RAS blockade can lead to an acute decrease in GFR, recent studies suggest that the reduction in GFR seen with RAS blockade does not reflect true tubular injury (8). From a mechanistic standpoint, the relatively greater vasodilation of efferent arterioles over afferent arterioles due to RAS blockade leads to reduced intraglomerular pressure, subsequent decreased glomerular filtration, and impaired capacity for autoregulation of GFR (9). This impaired autoregulation makes the kidney prone to GFR decrements associated with minor physiologic and hemodynamic insults such as reduction in BP or volume depletion. However, the accompanying improvement in tubular blood flow and oxygenation increases the proximal tubule’s ability to combat ischemic and nephrotoxic insults and reduces progression of tubulointerstitial fibrosis. Indeed, participants in the Systolic Blood Pressure Intervention Trial who were randomized to the intensive BP arm had reductions in GFR due to lower achieved BP, but these participants did not have elevated levels of tubular-injury biomarkers compared with those in the standard arm (8). Therefore, we argue that providers should distinguish true AKI with intrinsic tubular injury from hemodynamic “AKI” attributed to RAS blockade, in which a rise in serum creatinine does not reflect true kidney damage.
This study offers significant contributions to the literature of RAS blockade in the setting of AKI and benefits from rigorous study design. Based on the results of this study, a significant proportion of patients admitted to the hospital can initiate RAS blockade after AKI without a significantly increased risk of recurrent AKI. Another strength of the study is the use of an integrated healthcare delivery system for more complete covariate measurement and outcome ascertainment in follow-up, with robustness in the measurement of medical comorbidities, for example, using both hospitalization codes, outpatient diagnosis codes, and prescription information. Further, the authors’ use of time-updated marginal structural modeling allows for a less biased estimate of the effect of ACE-I/ARB use on recurrent AKI risk.
The exclusion of patients with prevalent CHF from entry into this study requires further discussion. The authors describe the reasoning for their choice to exclude patients with a diagnosis of CHF from their study population, stating that removal of these patients may reduce confounding by indication, because a prior study by Brar et al. (10) demonstrate an increased risk of CHF at 6 months. Further, Hsu et al. highlight that the results of this study are not generalizable to the heart-failure population, although this may not be clinically significant because the reinitiation of ACE-I/ARB in patients with heart failure is less difficult of a decision than the use of ACE-I/ARB for kidney diseases. However, a large subset of patients with AKI in the hospital have a diagnosis of CHF, and providers continue to struggle with optimal timing of initiation of RAS blockade in these patients. Additionally, heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF) represent very different disease phenotypes. Although the use of ACE-I or ARB therapy is a class-1 recommendation in HFrEF to reduce morbidity and mortality, the use of ACE-I or ARB in HFpEF remains a class-2a recommendation in HFpEF for the control of hypertension predominantly (11). We agree that the use of RAS blockade in patients with CHF, especially in HFrEF, should not be limited simply due to a rise in serum creatinine in the absence of other reasons for AKI.
One important question that this study does not address is the reinitiation of RAS blockade after AKI. Notably, patients who have been receiving ACE-I/ARB therapy within 5 years of index hospitalization were excluded from this study. These individuals likely represent a large proportion of the patients who are regularly seen in the hospital, and about whom providers often struggle with the reinitiation of ACE-I/ARB therapy after AKI. In the study by Brar et al., new use of ACE-I/ARB therapy after AKI was associated with an increased risk of hospitalization for kidney diseases (adjusted hazard ratio, 1.32; 95% CI, 1.03 to 1.69), as was resumption of prior ACE-I/ARB therapy (adjusted hazard ratio, 1.34; 95% CI, 1.16 to 1.55) compared with nonusers. Notably, however, both of these groups were found to have a lower risk of mortality compared with nonusers. Future studies are needed to continue to move this research forward, investigating the optimal timing of RAS blockade initiation, the potential differences in outcomes based on prior RAS blockade use, and the potential differences in outcomes based on diagnosis of CHF.
In recent years, studies evaluating the association of RAS blockade with kidney outcomes after AKI have been limited by generalizability concerns (only evaluating patients in the setting of the intensive care unit) and by AKI diagnosis (using discharge codes and not laboratory measures of serum creatinine). Additionally, the current literature investigating kidney outcomes after RAS blockade consists primarily of observational studies and post hoc analyses of prospective studies and clinical trials. To answer the question of RAS blockade and subsequent kidney outcomes after AKI, potential future studies can include clinical trials with random assignment to RAS blockade versus alternative therapies and more precise, biomarker-driven assessments of tubular health to confirm the lack of intrinsic injury to proximal tubular cells.
Disclosures
Dr. Menez has nothing to disclose. Dr. Parikh reports consulting fees from Akebia Therapeutics and Genfit Biopharmaceutical Company, and a position on the advisory board at and owning equity in RenalytixAI.
Funding
Dr. Menez is supported by National Heart, Lung, and Blood Institute (NHLBI) T32 training grant HL007024. Dr. Parikh is supported by NHLBI grant RO1-HL085757 and National Institute of Diabetes and Digestive and Kidney Diseases grant UO1-DK082185.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related article, “Renin-Angiotensin System Blockade after Acute Kidney Injury (AKI) and Risk of Recurrent AKI,” on pages 26–34.
References
- 1.van Vark LC, Bertrand M, Akkerhuis KM, Brugts JJ, Fox K, Mourad JJ, Boersma E: Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: A meta-analysis of randomized clinical trials of renin-angiotensin-aldosterone system inhibitors involving 158,998 patients. Eur Heart J 33: 2088–2097, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eurich DT, Majumdar SR, Tsuyuki RT, Johnson JA: Reduced mortality associated with the use of ACE inhibitors in patients with type 2 diabetes. Diabetes Care 27: 1330–1334, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, de Zeeuw D, Shahinfar S, Toto R, Levey AS; AIPRD Study Group : Progression of chronic kidney disease: The role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: A patient-level meta-analysis. Ann Intern Med 139: 244–252, 2003 [DOI] [PubMed] [Google Scholar]
- 4.van Diepen S, Norris CM, Zheng Y, Nagendran J, Graham MM, Gaete Ortega D, Townsend DR, Ezekowitz JA, Bagshaw SM: Comparison of angiotensin-converting enzyme inhibitor and angiotensin receptor blocker management strategies before cardiac surgery: A pilot randomized controlled registry trial. J Am Heart Assoc 7: e009917, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bainey KR, Rahim S, Etherington K, Rokoss ML, Natarajan MK, Velianou JL, Brons S, Mehta SR; CAPTAIN Investigators : Effects of withdrawing vs continuing renin-angiotensin blockers on incidence of acute kidney injury in patients with renal insufficiency undergoing cardiac catheterization: Results from the Angiotensin Converting Enzyme Inhibitor/Angiotensin Receptor Blocker and Contrast Induced Nephropathy in Patients Receiving Cardiac Catheterization (CAPTAIN) trial. Am Heart J 170: 110–116, 2015 [DOI] [PubMed] [Google Scholar]
- 6.Thakar CV, Christianson A, Himmelfarb J, Leonard AC: Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clin J Am Soc Nephrol 6: 2567–2572, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu CY, Liu KD, Yang J, Glidden DV, Tan TC, Pravoverov L, Zheng S, Go AS: Renin-angiotensin system blockade after acute kidney injury (AKI) and risk of recurrent AKI. Clin J Am Soc Nephrol 15: 26–34, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malhotra R, Craven T, Ambrosius WT, Killeen AA, Haley WE, Cheung AK, Chonchol M, Sarnak M, Parikh CR, Shlipak MG, Ix JH; SPRINT Research Group : Effects of intensive blood pressure lowering on kidney tubule injury in CKD: A longitudinal subgroup analysis in SPRINT. Am J Kidney Dis 73: 21–30, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kobori H, Nangaku M, Navar LG, Nishiyama A: The intrarenal renin-angiotensin system: From physiology to the pathobiology of hypertension and kidney disease. Pharmacol Rev 59: 251–287, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Brar S, Ye F, James MT, Hemmelgarn B, Klarenbach S, Pannu N; Interdisciplinary Chronic Disease Collaboration : Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with outcomes after acute kidney injury. JAMA Intern Med 178: 1681–1690, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr., Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C: 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart failure society of America. J Card Fail 23: 628–651, 2017 [DOI] [PubMed] [Google Scholar]