ABSTRACT
Gastrointestinal bleeding is an uncommon but potentially life-threatening complication of laparoscopic adjustable gastric banding (LAGB) erosion. We present the use of a Sengstaken-Blakemore tube as a treatment device for severe gastrointestinal bleeding secondary to persistent LAGB erosion. A 72-year-old woman post-LAGB placement presented with hemorrhagic shock from gastric band erosion that was not responsive to endoscopic and angiographic interventions. A salvage attempt to tamponade with a Sengstaken-Blakemore tube resulted in successful resuscitation of the patient. When used judiciously, balloon tamponade serves as a replicable technique to control severe gastric band erosion refractory to standard management.
INTRODUCTION
Laparoscopic adjustable gastric banding (LAGB) was one of the most commonly performed bariatric procedure worldwide during the decade after its FDA approval in 2002.1 Erosion of LAGB into the lumen of the stomach affects approximately 2%–3% of patients, according to a large case series.2–4 We present the novel use of a Sengstaken-Blakemore tube in the endoscopic management of refractory gastrointestinal bleeding secondary to LAGB erosion.
CASE REPORT
A 72-year-old woman with LAGB placement 11 years ago presented with complaints of nausea, dark stools, and shortness of breath. The patient was found to have melena on examination and a hemoglobin level of 5.5 g/dL. Initial esophagogastroduodenoscopy detected LAGB erosion into the stomach lumen with active bleeding from beneath the band. Hemostatic clips were placed, but the patient's hemoglobin continued to downtrend despite transfusion. She progressed to hemorrhagic shock, necessitating vasopressor infusion, and was transferred to our center. On repeat endoscopy, it was noted that at least 50% of the band had eroded into the gastric lumen; copious blood was seen in the stomach and active oozing from mucosa deep to the band (Figure 1). A hybrid surgical and endoscopic procedure was performed to remove the eroded band and identify the bleeding site.
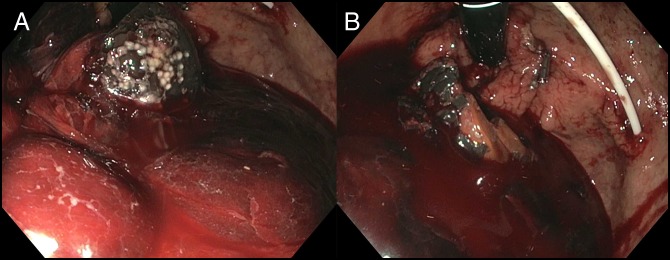
Figure 1.
Initial upper endoscopy revealed (A) at least 50% of the LAGB had eroded into the gastric lumen and (B) copious blood in the stomach with active oozing from mucosa deep to the gastric band. LAGB, laparoscopic adjustable gastric banding.
After removal of the skin port, the band was fractured with the aid of a lithotripter and removed in a manner previously described.4 At this point, diffuse oozing was noted from within the LABG tract. Attempts at hemostasis with clips and hemostatic powder were unsuccessful, and interventional radiology was consulted. Computed tomography (CT) illustrated active bleeding within the proximal stomach, and the patient was referred for emergent angiography. The angiogram did not reveal active bleeding in the celiac trunk distribution; given the CT findings, the left gastric artery was empirically embolized. Despite this, the bleeding continued. Because the patient was believed to be at high risk for a surgical intervention, a third endoscopy was performed 4 hours after embolization. On endoscopy, there remained active bleeding from the LAGB tract in the cardia, but the exact source could not be visualized (Figure 2). To tamponade the bleeding, a Sengstaken-Blakemore tube was placed, and the gastric balloon was inflated with the tube placed on traction (Figure 3). After Sengstaken-Blakemore tube placement, the patient's hemodynamics improved, and her hemoglobin stabilized. The Sengstaken-Blakemore tube was removed 12 hours later, at which point the bleeding had clinically resolved. The patient was transferred to the surgical ward and experienced no further bleeding, being discharged 4 days later. The patient has been stable, without recurrent bleeding, 4 months after discharge.
Figure 2.
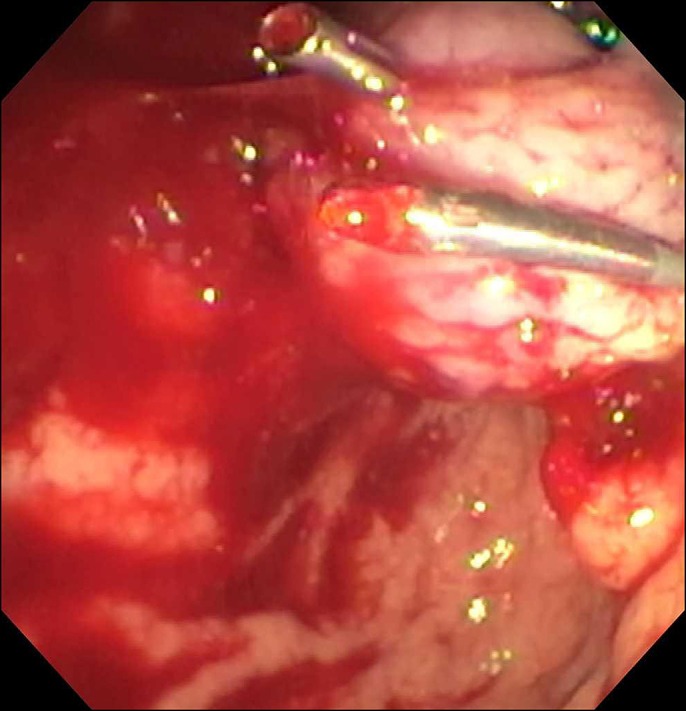
After removal of the LAGB, repeat upper endoscopy demonstrated active bleeding from the LAGB tract in the cardia, but the exact source could not be visualized. LAGB, laparoscopic adjustable gastric banding.
Figure 3.
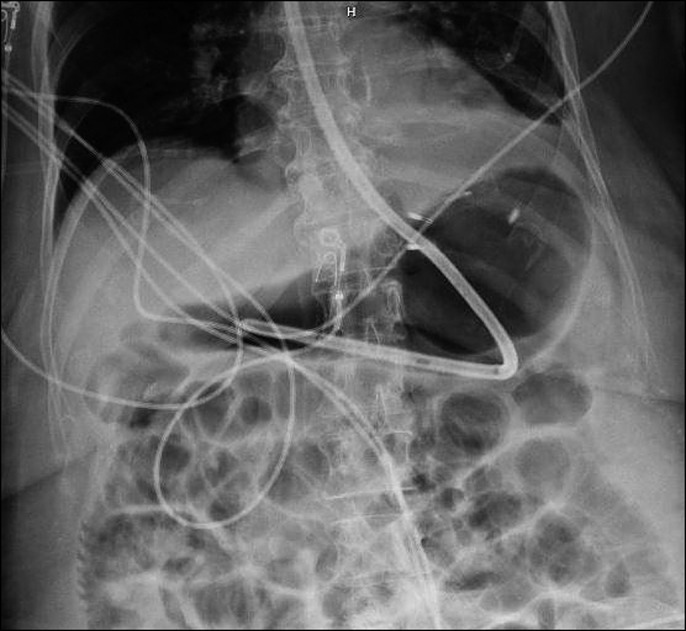
Radiography demonstrates placement of the Sengstaken-Blakemore tube with a gastric balloon inflated to tamponade bleeding. LAGB, laparoscopic adjustable gastric banding.
DISCUSSION
To our knowledge, this is the first report of the use of a Sengstaken-Blakemore tube to control gastric bleeding from LAGB erosion not responsive to endoscopic and angiographic interventions, thereby allowing the patient to avoid gastrectomy. As this case illustrates, bleeding related to LABG erosion is uncommon but difficult to manage during an adverse event.5–8
The pathogenesis of band erosion is likely to pressure necrosis of the stomach wall from band restriction.3,4,9 The most common presenting symptoms include loss of early satiety resulting in weight regain, infection or pain at the port site, and abdominal discomfort.4 Risk factors for erosion include oversewing the buckle mechanism, smaller band size, and a perigastric approach rather than the pars flaccida technique.4 Although often seen on CT scan, upper gastrointestinal endoscopy is the most common diagnostic modality to diagnose and potentially treat LAGB erosion. Removal of an eroded band is typically accomplished with a hybrid endoscopic-surgical approach, where the skin port is removed and the connector tube is cut from the skin side. Next, the band is fractured under endoscopic guidance with the aid of a lithotripter and removed preorally using a snare or forceps.10,11
Developed in 1950, the Sengstaken-Blakemore tube is an established device to control hemorrhage from esophageal varices through balloon tamponade.12 Because endoscopic techniques in hemorrhage management have since evolved, balloon tamponade is now considered a temporizing measure or alternative rescue therapy because of its risk of adverse events.13,14 Beyond hemostasis of variceal hemorrhage, its novel use has been successful in the salvage management of severe ulcerative esophagitis, aortoesophageal fistula, and postpartum hemorrhage.13,15,16 This is the first case to demonstrate that the Sengstaken-Blakemore tube effectively tamponades suspected short gastric artery bleeding from LAGB erosion refractory to therapeutic endoscopy and angiographic embolization. Balloon tamponade carries a considerable risk of esophageal injury and pressure necrosis of the stomach and esophagus if not used cautiously; thus, it should only be used when all other means of hemostasis are ineffective.
DISCLOSURES
Author contributions: All authors contributed equally to this manuscript. V. Kushnir is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Chung AY, Strassle PD, Schlottmann F, Patti MG, Duke MC, Farrell TM. Trends in utilization and relative complication rates of bariatric procedures. J Gastrointest Surg. 2019;23(7):1362–72. [DOI] [PubMed] [Google Scholar]
- 2.Furbetta N, Gragnani F, Flauti G, Guidi F, Furbetta F. Laparoscopic adjustable gastric banding on 3566 patients up to 20-year follow-up: Long-term results of a standardized technique. Surg Obes Relat Dis. 2019;15(3):409–16. [DOI] [PubMed] [Google Scholar]
- 3.Cappell MS, Mogrovejo E, Desai T. Case report of patient presenting in shock from band penetration into stomach after LAGB surgery: Diagnosis by emergency EGD after misdiagnosis by abdominal CT. Dig Dis Sci. 2016;61(11):3366–8. [DOI] [PubMed] [Google Scholar]
- 4.Brown WA, Egberts KJ, Franke-Richard D, Thodiyil P, Anderson ML, O'Brien PE. Erosions after laparoscopic adjustable gastric banding: Diagnosis and management. Ann Surg. 2013;257(6):1047–52. [DOI] [PubMed] [Google Scholar]
- 5.Campos J, Ramos A, Neto MG, et al. Hypovolemic shock due to intragastric migration of an adjustable gastric band. Obes Surg. 2007;17(4):562. [DOI] [PubMed] [Google Scholar]
- 6.Rao AD, Ramalingam G. Exsanguinating hemorrhage following gastric erosion after laparoscopic adjustable gastric banding. Obes Surg. 2006;16(12):1675–8. [DOI] [PubMed] [Google Scholar]
- 7.Iqbal M, Manjunath S, Seenath M, Khan A. Massive upper gastrointestinal hemorrhage: An unusual presentation after laparoscopic adjustable gastric banding due to erosion into the celiac axis. Obes Surg. 2008;18(6):759–60. [DOI] [PubMed] [Google Scholar]
- 8.Jouvin I, Barral M, Pocard M, Najah H. A late life-threatening complication of laparoscopic adjustable gastric banding. Surgery. 2018;163(5):1186–7. [DOI] [PubMed] [Google Scholar]
- 9.Kurian M, Sultan S, Garg K, Youn H, Fielding G, Ren-Fielding C. Evaluating gastric erosion in band management: An algorithm for stratification of risk. Surg Obes Relat Dis. 2010;6(4):386–9. [DOI] [PubMed] [Google Scholar]
- 10.Dellaportas D, Nastos C, Theodosopoulos T, Fragulidis G, Polydorou A, Vezakis A. Novel endoscopic management of eroding laparoscopic adjustable gastric band: A case series. Case Rep Gastrointest Med. 2018;2018:2747852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Lorenzo N, Lorenzo M, Furbetta F, et al. Intragastric gastric band migration: Erosion: An analysis of multicenter experience on 177 patients. Surg Endosc. 2013;27(4):1151–7. [DOI] [PubMed] [Google Scholar]
- 12.Sengstaken RW. Balloon tamponage for the control of hemorrhage from esophageal varices. Ann Surg. 1950;131(5):781–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seet E, Beevee SS, Cheng AA, Lim EE. The Sengstaken-Blakemore tube: Uses and abuses. Singapore Med J. 2008;49:e195–7. [PubMed] [Google Scholar]
- 14.Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Practice Guidelines Committee of the American Association for the Study of Liver Diseases tPPCotACoG. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922–38. [DOI] [PubMed] [Google Scholar]
- 15.Chen YI, Dorreen AP, Warshawsky PJ, Wyse JM. Sengstaken-blakemore tube for non-variceal distal esophageal bleeding refractory to endoscopic treatment: A case report & review of the literature. Gastroenterol Rep. 2014;2(4):313–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Majumdar A, Saleh S, Davis M, Hassan I, Thompson PJ. Use of balloon catheter tamponade for massive postpartum haemorrhage. J Obstetrics Gynaecol. 2010;30(6):586–93. [DOI] [PubMed] [Google Scholar]