Abstract
Background:
This study aimed to compare the quadratus lumborum block (QLB) method with transversus abdominis plane block (TAPB) for postoperative pain management in patients undergoing laparoscopic colorectal surgery.
Methods:
Seventy-four patients scheduled for laparoscopic colorectal surgery were randomly assigned into 2 groups. After surgery, patients received bilateral ultrasound-guided single-dose of QLB or TAPB. Each side was administered with 20 ml of 0.375% ropivacaine. All patients received sufentanil as patient-controlled intravenous analgesia (PCIA). Resting and moving numeric rating scale (NRS) were assessed at 2, 4, 6, 24, 48 hours postoperatively. The primary outcome measure was sufentanil consumption at predetermined time intervals after surgery.
Results:
Patients in the QLB group used significantly less sufentanil than TAPB group at 24 and 48 hours (P < .05), but not at 6 hours (P = .33) after laparoscopic colorectal surgery. No significant differences in NRS results were found between the two groups at rest or during movement (P > .05). Incidence of dizziness in the QLB group was lower than in TAPB group (P < .05).
Conclusions:
The QLB is a more effective postoperative analgesia as it reduces sufentanil consumption compared to TAPB in patients undergoing laparoscopic colorectal surgery.
Keywords: laparoscopic colorectal surgery, postoperative analgesia, quadratus lumborum block, transversus abdominis plane block, ultrasound
1. Introduction
Recent advancements in gastrointestinal endoscopy techniques have increased the rate of early diagnosis for colorectal cancer. Currently, laparoscopic radical resection of colorectal cancer is the mainstay treatment for this type of cancer. Although this surgery is minimally invasive, many patients still experience pain after surgery, which is unbearable in severe cases.[1,2]
Effective and dynamic analgesia after laparoscopic colorectal surgery enhances early recovery and ambulation. The transversus abdominis plane block (TAPB) exerts analgesic effects on the skin, muscle and parietal peritoneum of the anterior abdominal wall.[3] There are three TAPB techniques performed under ultrasound guidance: subcostal approach, lateral approach, and posterior approach. The application of ultrasound-guided TAPB is simple and has fewer complications, however, it fails to provide visceral and long-lasting analgesia.[4] In a recent study, Faiz et al[5] compared posterior TAPB with lateral TAPB for pain relief and opioids consumption after cesarean section. They concluded that posterior TAPB provided a longer duration of analgesic effect and reduced the consumption of morphine.
The quadratus lumborum block (QLB) is a new posterior abdominal trunk block which produces analgesic effects through local anesthetic that covers thoracolumbar fascia and thoracic paravertebral space. Based on the injection position and approach, there are 3 QLB techniques: anterolateral approach, posterior approach and anterior approach. Oksuz et al[6] compared the posterior QLB with the lateral TAPB for pain relief in pediatric patients undergoing low abdominal surgery, and found that the QLB provided longer and more effective postoperative analgesia than TAPB.
A recent meta-analysis[7] examined the duration of analgesia after posterior and lateral TAPB for lower abdominal surgery. The study included 12 trials comprising 641 patients. Four trials examined the posterior technique and 8 trials examined the lateral technique. The researchers found that the posterior TAPB produced sustained analgesia than the lateral TAPB. A major disadvantage of TAPB is the dermatomal limitation. In a study the examined the dermatome level, T7 to T12 dermatomes were obtained by the QLB, whereas TAPB affected T10 to T12 dermatomes. The duration of the QLB analgesia ranged from 24 to 48 hours after cesarean delivery operations,[8] whereas the TAPB analgesia provided a shorter analgesia (12–24 h) after laparoscopic ovarian surgery.[9] To the best of our knowledge, no study has compared the analgesic effects of posterior QLB and posterior TAPB. In this double-blind, randomized, controlled study, we compared the QLB with TAPB for postoperative pain relief in patients undergoing laparoscopic colorectal surgery.
2. Methods
2.1. Patients
This randomized double-blind clinical trial study was registered in the Chinese registry of clinical trials (ChiCTR1800014436). The principle of the study protocol was approved by the Research Ethics Committee of the Second Affiliated Hospital of Nanchang University. The study was carried out between January 2018 and December 2018. Informed written consent was obtained from all participants. The sample size calculation was performed before the study. The power analysis applied was based on the cumulative sufentanil consumption at 48 hours after surgery. Based on a pilot study and assuming group means ± standard deviation of 58.9 ± 15.4 μg (QLB group) and 71.3 ± 19.6 μg (TAPB group), 62 patients were required to achieve a power of 80% and the α value of 0.05 to detect differences between the 2 groups. Taking into consideration of possible dropouts of 20%, 74 patients were enrolled in the study. Inclusion criteria were according to the American Society of Anesthesiologists (ASA) physical status I or II and age of 18 to 70 years. Exclusion criteria were: body mass index (BMI) ≥30 kg/m2 or ≤15 kg/m2, colorectal tumor TNM stage III or IV, allergic to ropivacaine, localized infection, anatomic anomalies, a history of alcohol or analgesics dependence, language communication impairment, and coagulation abnormalities.
2.2. Anesthesia and surgical methods
General anesthesia was induced and maintained by the same procedure in both groups, using IV propofol (1.5 to 2.0 mg/kg) and sufentanil (0.3 μg/kg). Endotracheal intubation was facilitated by IV administration of cisatracurium (0.2 mg/kg). Anesthesia was maintained with a combined IV–inhaled anesthesia (propofol, remifentanil, and sevoflurane in oxygen), cisatracurium (0.1 mg/kg/hour) was applied to maintain muscle relaxation. Intravenous rehydration was achieved with a lactated Ringer's solution, while the infusion of IV atropine and ephedrine were used to maintain blood pressure and heart rate at the preoperative baseline range (the increase and decrease width did not exceed 20% of the baseline value). The bispectral index (BIS) value was maintained at 40 to 60.
The initial step of the surgical procedure was the establishment of the pneumoperitoneum in the abdomen. Intra-abdominal pressure was maintained at 11 to 13 mmHg. All procedures were performed by the same surgical team with standardized laparoscopic techniques. Four to five laparoscopic ports were used in all cases. A 1-cm incision was made above the umbilicus for camera insertion. Port placement was determined by the surgeons, but usually included two 5-mm ports for the surgeons and one to two 5-mm ports for the assistants. After completion of the surgical procedure, there was no port incisions infiltration of local anesthetic.
2.3. Intervention
Using Excel software (Version 2016, Microsoft Office, USA), we randomly assigned patients into 2 groups: QLB and TAPB. Before surgery, patients were informed of the pain evaluation process and trained to relieve pain using a PCIA pump. Electrocardiography, noninvasive blood pressure, peripheral oxygen saturation and BIS were monitored. In the operation room, peripheral IV access was obtained, midazolam (0.02 mg/kg) was administered intravenously 5 minutes before measurement of baseline values. Perioperative anesthesia management was performed in line with the ASA guidelines. After surgery, patients were transferred to the PACU.
An experienced anesthesiologist (XFL) performed all block techniques and administered the medication, but the patients and the resident anesthesiology (WD) were blinded to the intervention. All blocks were performed in the PACU. In both groups, the patients were placed in the supine position and the abdomen was cleaned with a surgical solution. A low frequency (4–8 MHz) convex transducer (Sonosite S-Nerve Ultrasound System, USA) covered with a sterile sheath was used. For the posterior QLB, the transducer was placed at the level of the anterosuperior iliac spine, and moved cranially until the 3 abdominal wall muscles were clearly visible. According to the characteristics of quadratus lumborum with tendon attached to the transverse process, the muscle pointed by the transverse process was the quadratus lumborum. The probe was tilted down to identify the posterior side of the quadratus lumborum. A short oblique needle (20 gauge, 100 mm, Braun, Germany) was inserted in plane from the ventral side to the dorsal side followed by a negative aspiration test with 2 ml normal saline to confirm the position. An injection of 20 ml 0.375% ropivacaine on each side was applied between the quadratus lumborum and the thoracolumbar fascia. For the posterior TAPB, the probe was positioned across the posterior axillary area, and 3 typical abdominal wall muscles were identified. The same needle was directed in plane from anterolateral side to posteromedial side followed by a negative aspiration test with 2 ml normal saline to confirm the position. Next, 20 ml 0.375% ropivacaine was injected on each side between the posterior junction of transversus abdominous muscle and the anterolateral border of quadratus lumborum. The blocks were considered successful when dissection of the fascia plane appeared smooth under the sonographic image with a good spread of the local anesthesia. The contralateral block was performed using the same procedures.
In all patients, pain management was achieved using multimodal analgesia regimen. Patients in both groups regularly received IV parecoxib (40 mg every 12 hour) for postoperative analgesia. They also received sufentanil followed by PCIA pump (microcomputer electronic analgesia pump, China), which was programmed to deliver 3 μg sufentanil on demand with a lockout interval of 15 minutes and no background infusion. When the NRS score exceeded 3, the patients employed the PCIA pump. The maximum sufentanil dose of bolus per hour was 12 ug. Any complications occurring during the perioperative period were recorded.
The primary outcome measure was the cumulative consumption of PCIA sufentanil at stationary time intervals (6, 24, and 48 hours) postoperatively. Secondary outcomes included resting or moving (dynamic) NRS scores at 2, 4, 6, 24, and 48 hours postoperatively and postoperative side effects. All patients were followed up for 48 hours by the same resident anesthesiology who was blinded to the group allocation.
2.4. Statistical analyses
Statistical analyses were performed using SPSS v.19.0 software (IBM, Armonk, NY). The quantitative variables are expressed as mean ± standard deviation for normally continuous variables. Two-sample Student t test was used to compare 2 groups. The qualitative data are expressed as the number of cases for nominal variables, and comparison was performed using Chi-square test and Fisher exact test. A 2-tailed P < .05 was considered as statistically significant.
3. Results
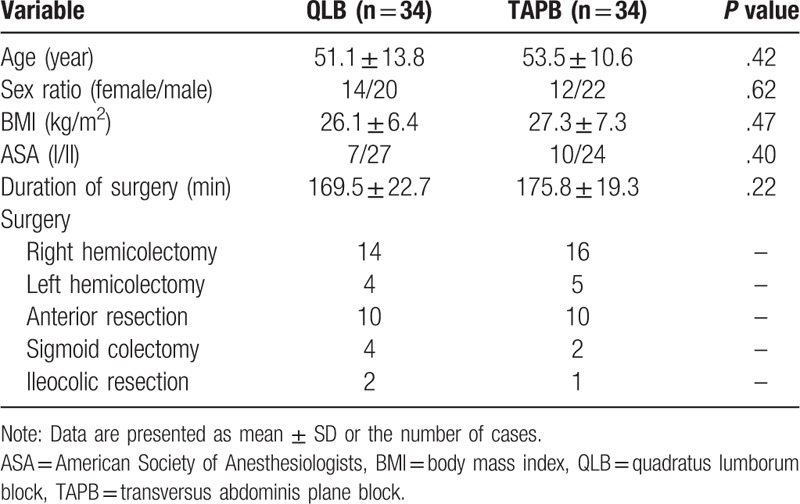
A total of 74 patients were randomly enrolled in the study (Fig. 1). Six patients withdrew from the study before completion. Each group had 34 patients (Fig. 1). Patients’ demographic characteristics such as age, sex, BMI, and ASA grades were not significantly different between the 2 groups (Table 1).
Figure 1.

Flow of the participants through the study. QLB = quadratus lumborum block, TAPB = transversus abdominis plane block.
Table 1.
Demographic and intraoperative characteristics.
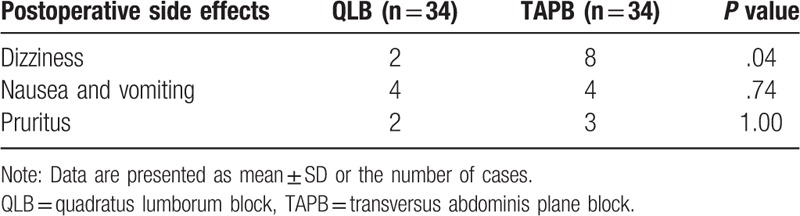
Compared to the TAPB group, the patients in the QLB group used significantly less sufentanil at 24 and 48 hours (P < .05), but no significant difference was observed between the 2 groups at 6 hours (P = .33) after surgery (Table 2). There were no significant differences in NRS results between the 2 groups at rest or during movement (P > .05, Tables 3 and 4). Incidence of dizziness in the QLB group was lower than in the TAP group (P < .05), and the occurrence of pruritus, nausea and vomiting were not significantly different between the 2 groups (P > .05, Table 5).
Table 2.
Sufentanil consumption (ug).
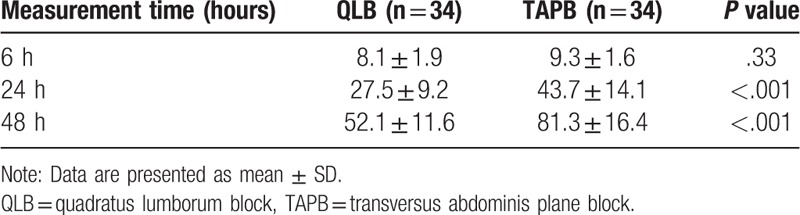
Table 3.
Numeric rating scale scores at rest.
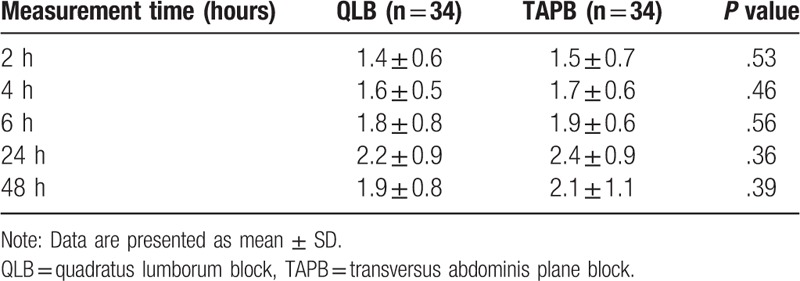
Table 4.
Numeric rating scale scores with movement.
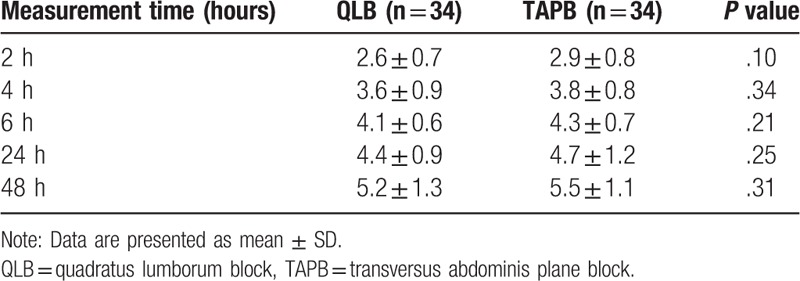
Table 5.
Postoperative side effects.
No other complications were observed, such as arrhythmia or hypotension.
4. Discussion
To our knowledge, this is the first prospective, randomized, double-blind, controlled study comparing the QLB with TAPB for pain relief in patients undergoing laparoscopic colorectal surgery. Our results show that QLB is an effective, reliable, and safe analgesic procedure and does not produce any adverse reaction.
Opioids such as sufentanil are the most commonly used analgesics in China. However, the adverse reactions associated with opioids such as nausea, vomiting, constipation and respiratory depression cannot be ignored. These effects compromise the postoperative recovery process.[10] In this study, application of QLB produced a significant reduction in sufentanil consumption at 24 and 48 hours compared to the TAPB. We note, however, that the use of multimodal analgesia scheme (parecoxib) in this study may have masked some of the benefits of the QLB. Nonetheless, the results of this study show that QLB is superior to TAPB in postoperative pain management. Our results are consistent with those of Oksuz et al.[6]
The TAPB has been established as an important component of multimodal analgesia techniques as it provides effective analgesia for abdominal surgical procedures. Subcostal TAPB technique provides analgesia for upper abdominal surgery,[11] whereas lateral and posterior TAPB provide analgesia for lower abdominal transverse incisions.[12] The QLB is a novel type of trunk block technique widely applied in lower and upper abdominal surgery, hip and lower extremity surgery.[13,14,15] Later modifications to this technique created three QLB approaches: anterolateral approach (in the anterolateral edge of the quadratus lumborum), posterior approach (in between quadratus lumborum and thoracolumbar fascia) and anterior approach (in between quadratus lumborum and psoas major muscle). In the anterior approach, local anesthesia is injected into the anterior border of the quadratus lumborum.[16] Compared with other methods, posterior QLB is safer and more superficial block. The needle tip is separated from the peritoneum by quadratus lumborum, hence the risk of intraperitoneal injection and intestinal injury in the posterior QLB is avoided.
A notable complication of QLB is the weakening of the lower limbs. Ueshima et al[17] reviewed 2382 patients who underwent the QLB technique, including 771 cases of lateral approach, 1485 cases of posterior approach, and 81 cases of anterior approach. They found that the incidence of quadriceps muscle weakness in the 3 methods was 1%, 19%, and 65%, respectively, and the incidence was highest in anterior approach. To reduce the occurrence of lower limb muscle weakness, we chose the posterior approach. We did not observe significant muscle weakness in our study. However, our small sample size may mask some rare complications of QLB. Murouchi et al[9] compared QLB with TAPB in laparoscopic ovarian surgery. After injection of 150 mg of ropivacaine, the peak concentration of ropivacaine was significantly lower in patients that received QLB compared to those that received TAPB. Moreover, the QLB provided a more extensive and long-lasting analgesia. Interestingly, the mechanism of QLB is currently unknown. Dam et al[18] reported that the local anesthetic of QLB spreads to thoracic paravertebral space through the thoracolumbar fascia, reaching transversalis fascia and arcuate ligament to achieve the analgesic effect of paravertebral block. Therefore, they suggested that the spread of local anesthetic into the paravertebral space was the main mechanism of the blockade. However, in a magnetic resonance imaging study, it was reported[19] that the calculated volume reaching paravertebral space was too small, and instead suggested that the local anesthetic effect on the thoracolumbar fascia formed the main component of QLB.
The thoracolumbar fascia is composed of three layers: anterior, middle and posterior fascia, and is wrapped around the erector spinae and the quadratus lumborum. The anterior layer is located behind the erector spinae and is also the initial aponeurosis of the latissimus dorsi. The middle layer separates the erector spinae and the quadratus lumborum. Whereas the middle and anterior layers meet at the lateral edge of the erector spinae, the posterior layer covers the anterior boundary of the quadratus lumborum. The three layers of fascia meet at the lateral border of the quadratus lumborum to form the initial aponeurosis of the internal abdominal oblique and transversus abdominis muscles. The thoracolumbar fascia not only acts as a pathway for the local anesthetic spreading to the paravertebral space, but also distributes the spinal nerve branches (the lateral branches of posterior branch of L1-L3 spinal nerve) and multiple sympathetic fibers. There are high-density mechanoreceptors and pain receptors within the thoracolumbar fascia.[20] Under the induction and action of external factors, the above receptors are directly involved in the production of chronic waist and back pain. In addition, sympathetic fibers are involved in the pathophysiological mechanism of fascia dysfunction. Therefore, Blanco et al postulated that the direct action of local anesthetics on the thoracolumbar fascia was the main mechanism of QLB.
Additional studies are required to explore the mechanism of QLB as well as compare QLB and the subcostal TAPB in upper abdominal surgeries. Furthermore, investigations are needed to provide general recommendations for the use of QLB.
5. Conclusion
Our results show that QLB is a more effective postoperative analgesia as it reduces sufentanil consumption compared to the TAPB in patients undergoing laparoscopic colorectal surgery.
Author contributions
Conceptualization: Shuchun Yu.
Data curation: Wei Deng.
Formal analysis: Wei Deng.
Investigation: Wei Deng, Xiaofei Long, Liwei Guo.
Methodology: Wei Deng, Shuchun Yu.
Project administration: Xiaofei Long.
Resources: Guohai Xu.
Software: Manjun Li, Chang Li, Liwei Guo.
Supervision: Guohai Xu.
Writing – original draft: Manjun Li, Chang Li.
Writing – review & editing: Chang Li.
Shuchun Yu orcid: 0000-0003-0041-9103.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, BIS = bispectral index, BMI = body mass index, NRS = numeric rating scale, PCIA = patient-controlled intravenous analgesia, QLB = quadratus lumborum block, TAPB = transversus abdominis plane block.
How to cite this article: Deng W, Long X, Li M, Li C, Guo L, Xu G, Yu S. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain management after laparoscopic colorectal surgery: a randomized controlled trial. Medicine. 2019;98:52(e18448).
WD and XL contributed equally to this work and are co-first authors.
This work was supported by National Natural Science Foundation of China (Grant No. 81760338) and Natural Science Foundation of Jiangxi Province, China (Grant No. 20171BAB205029).
The authors have no conflicts of interests to disclose.
References
- [1]. Hubner M, Blanc C, Roulin D, et al. Randomized clinical trial on epidural versus patient-controlled analgesia for laparoscopic colorectal surgery within an enhanced recovery pathway. Ann Surg 2015;261:648–53. [DOI] [PubMed] [Google Scholar]
- [2]. Niraj G, Kelkar A, Hart E, et al. Comparison of analgesic efficacy of four-quadrant transversus abdominis plane (TAP) block and continuous posterior TAP analgesia with epidural analgesia in patients undergoing laparoscopic colorectal surgery: an open-label, randomised, non-inferiority trial. Anaesthesia 2014;69:348–55. [DOI] [PubMed] [Google Scholar]
- [3]. Karaman T, Ozsoy AZ, Karaman S, et al. The effects of transversus abdominis plane block on analgesic and anesthetic consumption during total abdominal hysterectomy: a randomized controlled study. Rev Bras Anestesiol 2018;68:285–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Baeriswyl M, Kirkham KR, Kern C, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg 2015;121:1640–54. [DOI] [PubMed] [Google Scholar]
- [5]. Faiz S, Alebouyeh MR, Derakhshan P, et al. Comparison of ultrasound-guided posterior transversus abdominis plane block and lateral transversus abdominis plane block for postoperative pain management in patients undergoing cesarean section: a randomized double-blind clinical trial study. J Pain Res 2018;11:5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Oksuz G, Bilal B, Gurkan Y, et al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med 2017;42:674–9. [DOI] [PubMed] [Google Scholar]
- [7]. Abdallah FW, Laffey JG, Halpern SH, et al. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth 2013;111:721–35. [DOI] [PubMed] [Google Scholar]
- [8]. Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med 2016;41:757–62. [DOI] [PubMed] [Google Scholar]
- [9]. Murouchi T, Iwasaki S, Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med 2016;41:146–50. [DOI] [PubMed] [Google Scholar]
- [10]. Jin LJ, Wen LY, Zhang YL, et al. Thoracic paravertebral regional anesthesia for pain relief in patients with breast cancer surgery. Medicine (Baltimore) 2017;96:e8107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Carrie C, Biais M. Subcostal TAP block and postoperative respiratory function after abdominal surgery. Anaesthesia 2014;69:1056–7. [DOI] [PubMed] [Google Scholar]
- [12]. Walter CJ, Maxwell-Armstrong C, Pinkney TD, et al. A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc 2013;27:2366–72. [DOI] [PubMed] [Google Scholar]
- [13]. Okmen K, Metin OB, Topal S. Ultrasound-guided posterior quadratus lumborum block for postoperative pain after laparoscopic cholecystectomy: a randomized controlled double-blind study. J Clin Anesth 2018;49:112–7. [DOI] [PubMed] [Google Scholar]
- [14]. Johnston DF, Sondekoppam RV. Continuous quadratus lumborum block analgesia for total hip arthroplasty revision. J Clin Anesth 2016;35:235–7. [DOI] [PubMed] [Google Scholar]
- [15]. Parras T, Blanco R. Randomised trial comparing the transversus abdominis plane block posterior approach or quadratus lumborum block type I with femoral block for postoperative analgesia in femoral neck fracture, both ultrasound-guided. Rev Esp Anestesiol Reanim 2016;63:141–8. [DOI] [PubMed] [Google Scholar]
- [16]. Dam M, Hansen CK, Borglum J, et al. A transverse oblique approach to the transmuscular Quadratus Lumborum block. Anaesthesia 2016;71:603–4. [DOI] [PubMed] [Google Scholar]
- [17]. Ueshima H, Hiroshi O. Incidence of lower-extremity muscle weakness after quadratus lumborum block. J Clin Anesth 2018;44:104. [DOI] [PubMed] [Google Scholar]
- [18]. Dam M, Moriggl B, Hansen CK, et al. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg 2017;125:303–12. [DOI] [PubMed] [Google Scholar]
- [19]. Adhikary SD, El-Boghdadly K, Nasralah Z, et al. A radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. Anaesthesia 2017;72:73–9. [DOI] [PubMed] [Google Scholar]
- [20]. Vleeming A, Schuenke MD, Danneels L, et al. The functional coupling of the deep abdominal and paraspinal muscles: the effects of simulated paraspinal muscle contraction on force transfer to the middle and posterior layer of the thoracolumbar fascia. J Anat 2014;225:447–62. [DOI] [PMC free article] [PubMed] [Google Scholar]


