Abstract
The aim of this study was to evaluate the efficacy and safety of prophylactic intraoperative bilateral uterine or internal iliac artery embolization in planned cesarean for pernicious placenta previa in the third trimester of pregnancy.
The patients with pernicious placenta previa were retrospectively included from January 2011 to May 2018, being divided into embolization group and control group. Intraoperative uterine artery embolization (UAE) or internal iliac artery embolization (IIAE) was undertaken to stop intrapartum and postpartum hemorrhage in embolization group.
There were no significant differences on age, pregnancy times, gestational age, neonatal weight, neonatal asphyxia, prenatal bleeding, placental implantation, and mortality between embolization group and control group (P > .05). The amount of intraoperative and postoperative bleeding in embolization group was significantly greater than that in control group (P < .05). However, the hysterectomy rate in the embolization group was significantly lower than that in the control group (P < .05). Two (6.25%, 2/32) cases had undergone the second time embolotherapy after 8 hours of cesarean surgery because of severe vaginal bleeding. One case (3.13%, 1/32) died of diffuse intravascular coagulation because of hemorrhagic shock in embolization group. Transient and self-remitted lumbosacral pain was present in 28 (95%, 28/32) patients and no other severe interventional complications were reported in embolization group. All babies in 2 groups were healthy at half to 5 years’ follow-up.
The prophylactic intraoperative embolization of bilateral UAE or IIAE may be an effective strategy to treat intractable peripartum hemorrhage and preserve the fertility in patients with pernicious placenta previa.
Keywords: embolization, internal iliac artery, pernicious placenta previa, uterine artery
1. Introduction
Placenta previa refers to the placenta adjacent or overlying the internal cervical os, frequently complicated with placental accrete, increta or percreta.[1,2] If placenta implants on the previous cesarean scar, it predicts severe intrapartum hemorrhage.[3] Placenta previa is often associated with previous uterine surgery, grand multiparity, recurrent abortions, previous curettage, advanced maternal age etc.[4] Pernicious placenta previa imposes a high risk of hemorrhage and hysterectomy on mothers, and increases the rate of preterm delivery, low birth weight, and neonatal admission.[1,5–7]
Cesarean hysterectomy is the current standard of management of invasive placenta,[8] but in cases of pernicious placenta previa, even hysterectomy might be difficult to control intractable hemorrhage.[9,10] The newly conservative methods of managing blood loss for pernicious placenta previa during cesarean have been introduced, including uterine or iliac arteries ligation, bilateral uterine artery embolization (UAE), or balloon occlusion of the internal iliac arteries or aortic artery.[9,11–15] Among the interventional procedures, selective UAE may be the first choice.[13,14,16,17] However, because of the uterus possibly supplied by one of the ovarian or aberrant arteries, selective UAE might fail to control the intractable bleeding.[18] Additionally, if being too urgent to access uterine arteries, internal iliac artery embolization (IIAE) may be alternative. Four cases of bilateral IIAE were mentioned in 2 studies of UAE for abnormal placenta, but no detailed information is available.[13,17]
We aimed to evaluate the effectiveness and safety of prophylactic intraoperative UAE or alternative IIAE (when uterine arteries unavailable) in planned cesarean for pernicious placenta previa in the third trimester of pregnancy.
2. Methods
2.1. Setting
The First Affiliated Hospital of Soochow University is a tertiary care referral hospital, with multidisciplinary care for the treatments of pernicious placenta previa.
2.2. Patients
From January 2011 to May 2018, the database of our institution was retrospectively reviewed to identify all cases with pernicious placenta previa. Inclusion criteria were placenta previa cases had complicated placental accrete, or increta with the placenta implanted on the site of the previous cesarean scar in the third trimester of pregnancy. The patients of pernicious placenta previa had the clinical and imaging manifestations as followed: the history of at least 1 uterine low segment cesarean delivery; in sonographic or magnetic resonance imaging (MRI) findings the placenta locating at the site of previous cesarean scar and suggestive of placenta accrete with or without thinner myometrium interface, lacunar spaces in the placental tissue, or invasion into the myometrium; the gestational age ≥28 weeks; little or no antepartum hemorrhage. Cases were treated by percutaneous transcatheter bilateral UAE and/or IIAE embolization during cesarean surgery to control intrapartum hemorrhage, and the diagnosis of pernicious placenta previa was confirmed intraoperatively. The exclusion criteria were posterior placenta previa and placental implantation away from the scar of previous cesarean. According to whether pelvic embolization was divided into embolization group, with percutaneous pelvic embolization during planed cesarean section, and control group, without embolization.
2.3. Pelvic embolization in cesarean surgery
The decision to perform the intraoperative embolization at our institution was made by consensus after multidisciplinary discussion of the Obstetrics, Intervention Radiology, and Anesthesiology. Written informed consent for the intraoperative embolization procedure was obtained. The patients were noticed the possibilities of severe hemorrhage and hysterectomy in the surgery. It was necessary to prepare adequate blood products and establish the smooth deep venous access before surgery. A panel of 3 obstetricians, 1 pediatrician, 2 interventional radiologists, 2 anesthesiologists, and nursing staff performed the combined procedures.
Two interventional radiologists worked simultaneously, on each side, to minimize procedure time and radiation dose to the fetus. Real-time ultrasound guidance was used to minimize puncture-related complications and fluoroscopy. Pelvic angiography was performed under local anesthesia with a common bilateral femoral artery approach, and provided a vascular road map for the uterine arteries or internal iliac arteries if the former is unavailable or too urgent to access. The long reverse catheter (Cook, Bloomington) was used to catheterize the uterine or internal iliac arteries. Then the cesarean section was done under general anesthesia. The abdominal wall was incised in the midline, and the vertical or transverse incision was tried to avoid blood vessels in the lower uterine segment. After fetal delivery, Alis forceps were used to stop bleeding of uterine incision temporarily. Before placenta was delivered, the interventional radiologists confirmed that the long reverse catheter was catheterized the bilateral uterine or internal iliac arteries. This helped to control intractable peripartum hemorrhage. Absorbable gelatin sponge particles (350–560 μm, Alicon Pharm SCI & TEC, Hangzhou, China) were used as embolic material in all patients. After the targeted arteries were surely embolized with blood flow markedly decreased, the placenta was removed by manual and piecemeal technique for the cases of adherent placenta. All of sutures finished; the interventional radiologists reconfirmed the embolization of the main uterine or internal iliac artery had already achieved (Fig. 1). The 5-F introducer was left in place for the following 24 hours. In the aftermath, all patients were closely monitored for vital signs, vaginal bleeding, full blood count in intensive care unit, and received prophylactic antibiotics and dexamethasone (5 mg daily) for 2 to 3 days after embolization. The cesarean section was performed in control group, without artery embolization. All the procedures were carried out in a hybrid operating room.
Figure 1.
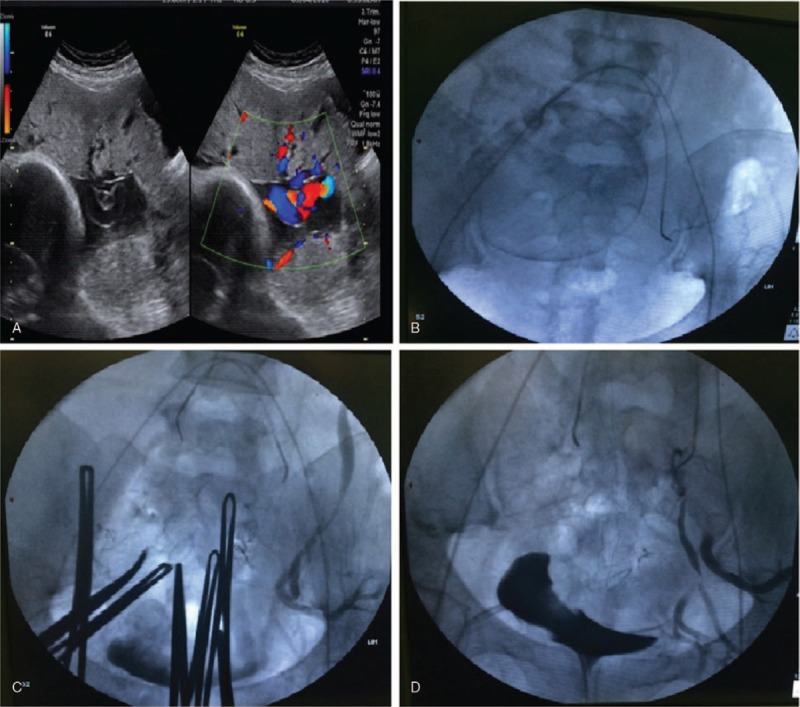
Ultrasound and radiological findings from Case No.16. (A) On sonographic ultrasound the placenta was located at the site of previous cesarean scar and overlied the internal cervical os. (B) Before cesarean section, the long reverse catheters were placed to catheterize the uterine artery. (C) After fetal delivery, Alis forceps stopped bleeding of uterine incision temporarily. (D) Finishing all of sutures, the interventional radiologist reconfirmed that the embolization of bilateral uterine or internal iliac arteries had already achieved.
A retrospective review was conducted for patients’ demographics, obstetric history, intervention radiological procedure and operative details, peripartum course. Maternal serum β-human chorionic gonadotropin (hCG), menstruation resume, and babies’ health were followed after discharge. Main outcomes were intraoperative blood loss, transfusion requirement, hysterectomy rate, endovascular or surgical complications, and significant postoperative morbidity. This study was performed with institutional review board approval. No consent was obtained from the patients, as it was a retrospective study. All the data were reviewed separately by 2 researchers. Any discrepancy would be sent to a senior researcher for the final agreement.
Descriptive statistics were used to describe the basic features of the data gathered from our study. Data were presented as percentages or mean ± SD. Statistical analysis was performed using Pearson χ2 and Fisher exact tests. Value of P < .05 (2-sided) was considered as statistical significance. SPSS software version 22.0 (IBM, Armonk, NY) was used for all the data analysis.
3. Results
A total of 47 patients with pernicious placenta previa were enrolled in this study: the embolization group (n = 32) and the control group (n = 15). The mean maternal age was 33.25 years (26–41 years). There were no significant differences in age, pregnancy times, gestational age, neonatal weight, neonatal asphyxia, prenatal bleeding, placental implantation, and mortality between the embolized group and the control group (P > .05). The amount of intraoperative and postoperative bleeding in the embolization group was significantly greater than that in the control group (P < .05). The hysterectomy rate in the embolization group was significantly lower than that in the control group (P < .05, Table 1).
Table 1.
Correlation of embolization in elective cesarean section with clinical parameters in patients with pernicious placenta previa.
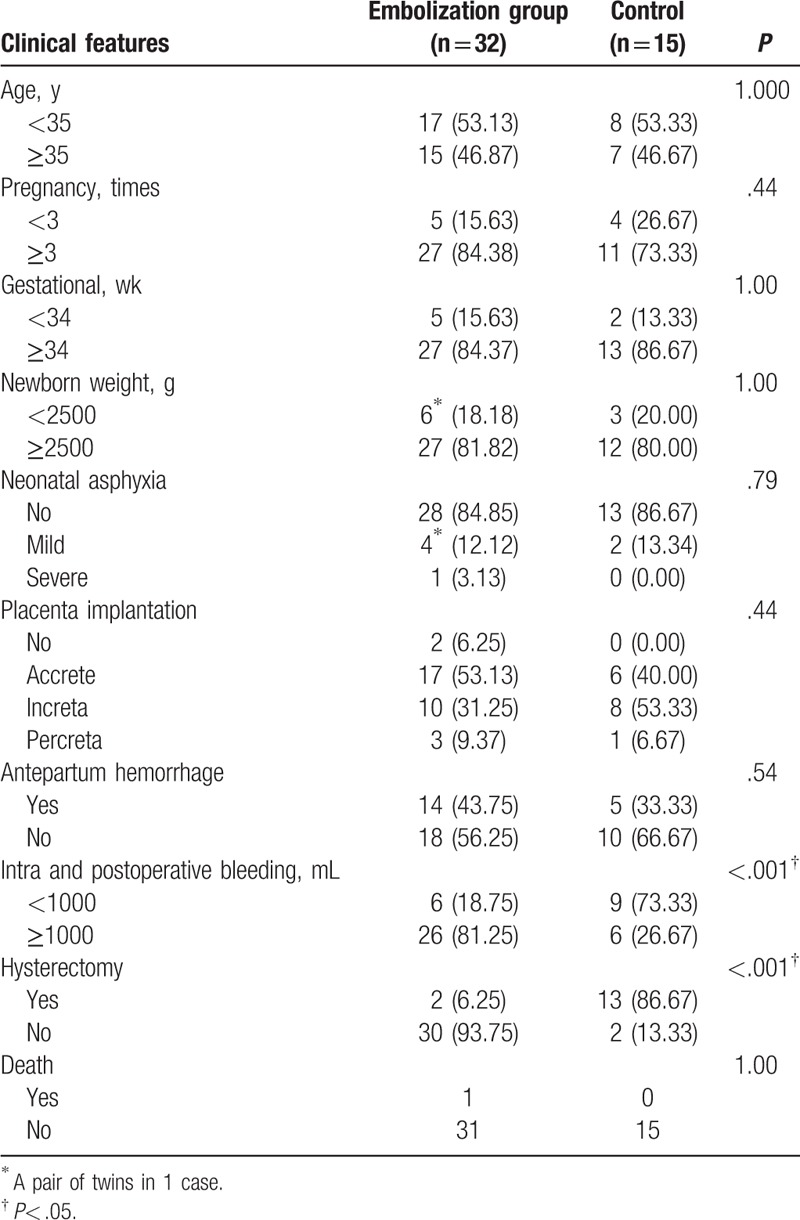
Thirty-two patients with pernicious placenta previa were treated by percutaneous transcatheter embolotherapy (UAE, n = 14; IIAE, n = 18) in planned cesarean. The mean maternal age was 32.75 ± 3.45 years. Average gravidity was 3.78 ± 1.21, and average parity was 2.20 ± 0.41. The mean gestational age was 253.65 ± 13.41 days. Thirty-one women had single-fetus pregnancies. Only 1 woman had twins pregnancy. Two (6.25%, 2/32) cases had underwent the second-time embolotherapy after 8 hours of cesarean surgery because of severe vaginal bleeding. The emergency postpartum hysterectomy was performed for 1 (3.13%, 1/32) case after failed embolotherapy because of uncontrolled massive hemorrhage and hypovolemic shock. However, 9 (9/15, 60.0%) cases had hysterectomy after cesarean delivery in the control group. One case (3.13%, 1/32) died of diffuse intravascular coagulation because of hemorrhagic shock. Transient and self-remitted lumbosacral pain was present in 28 (95%, 28/32) patients and no other severe interventional complications were reported. The serum β-hCG decreased to normal in all patients after 1 month of delivery. The left 30 (93.75%, 30/32) patients with retained uterine had regular monthly cycles. All babies in 2 groups were healthy and no patient had further pregnancy at half to 5 years’ follow-up.
4. Discussion
In this study, previous cesarean was present in all 47 cases, whose placenta just located on the cesarean scars. Prophylactic intraoperative UAE or IIAE (if uterine arteries unavailable or too urgent to access) in scheduled cesarean delivery was performed for these patients with pernicious placenta previa in the third trimester of pregnancy. Hysterectomy and reembolization rate were only 3.13% respectively. In 30 patients with uterine retained, their normal menstruations resumed at follow-up. No newborn mortality and severe interventional complications were reported. This strategy of UAE and alternative IIAE was considered as effective and safe. To our knowledge, this is the first study that assesses alternative prophylactic IIAE for UAE in a series of abnormal placenta patients undergoing interventional and conservative managements.
Previous cesarean has been best known as one of the major risk factors of placenta previa.[4,19] All patients had the history of cesarean in our study. The incidence of pernicious placenta previa is rising, primarily because of the high cesarean section rate in China. In a large sample study, placenta previa is significantly associated with the high risk of postpartum hemorrhage, blood transfusion, and hysterectomy.[6] For patients with pernicious placenta previa, early diagnosis and identification are essential.[20] The diagnostic choice for placenta previa is transabdominal and transvaginal ultrasonography and confirmed by magnetic resonance images, which may better verify the extent of placental invasion.[1] In our cases, pernicious placenta previa were strictly diagnosed by concurrent positive transabdominal and transvaginal ultrasonography imaging and intraoperative findings, in which the diagnostic pattern was supported by D'Souza et al.[8]
In our study, the success rate of the pelvic embolization was 93.75% and the procedure was unsuccessful for controlling intractable hemorrhage in only 1 woman (3.13% compared to 60.0% in control group), requiring emergency hysterectomy, and 1 case died of diffuse intravascular coagulation because of hemorrhagic shock. The hysterectomy rate was very similar to that of a previous study covering total 308 cases of placenta previa during a 8-year period.[21] Other small sample studies reported higher hysterectomy rate, varying from 9% to 31%.[8,12,13,17,18] Estimated blood loss in the embolization group during the surgery was numerically not much different from or even less compared with those of other studies.[13,17,20,22]
Major complications of obstetrics interventional radiology included maternal thromboembolic event,[18] pelvic hematoma and arteriovenous malformations,[23] peritonitis, and endometritis.[13] UAE may complicate vesicovaginal fistula.[18] Buttock necrosis and paraplegia were present in a case after bilateral internal iliac artery embolization,[24] which was an exceedingly rare adverse event.[25] As for main IIAE, some studies reported catheter-related complications. Nevertheless, there was no maternal or fetal mortality related to IIAE.[23,26,27] In our study, even >50% of patients undertook bilateral internal iliac arteries embolization but the above-mentioned major events were not reported. Well-equipped hospitals with skilled radiologists could prevent from severe adverse events. It is confirmed by our experiences that the procedure of UAE or alternative IIAE is safe for conservative managements of abnormal placentation. Moreover, further pregnancies and fetal growth were not affected in 8 women with a history of bilateral IIAE for postpartum hemorrhage.[28]
We preferred to selectively embolize bilateral uterine arteries because UAE has proven to be very effective and is considered the first choice of treatment for patients with postpartum hemorrhage.[16] But in some cases, if uterine arteries being not available or too urgent to access, IIAE was alternative. The alternative procedure was also applied by other authors[13,17,23] because it may be difficult to access uterine arteries in the urgent situation of intrapartum bleeding,[8] or because of arterial spasm.[23] And that other pelvic branches (apart from uterine arteries) may supply blood flow of the uterine. To embolize the anterior iliac arteries bilaterally would be better than only the uterine arteries.[8] The anterior division of IIA was often embolized.[25] However, bilateral internal iliac artery embolization is also effective, without major complications.[23,26] Although bilateral main IIA were temporarily embolized by gelatin sponge, pelvic vessels should reanalyze after dozens of days.
The use of balloon catheters to prevent post-partum hemorrhage in women with placenta accreta is controversial. Combining balloon occlusion with UAE appears to be beneficial.[20,27] Uterus resection rate (20%) was higher in balloon occlusion of the lower abdominal aorta in cesarean section surgery for the patients with pernicious placenta previa, compared to ours (3.13%).[12] Prophylactic internal iliac artery balloon occlusion followed by classical caesarean and UAE was carried out in 10 patients, with hysterectomy rate 30%.[8] Thus our strategy of UAE or alternative IIAE was even not inferior to combined prophylactic balloon occlusion with immediate embolization.
All the procedures of UAE or IIAE were carried out in a hybrid operating room at our hospital, to avoid extra transferring between angiography room and operation room. We think this is one of the key points to decrease procedure duration, prevent massive bleeding, and reduce fetal radiation exposure, as Konishi et al suggested.[29] Intraoperative transporting may be unsafe because of nonstable hemodynamics,[14] subsequently increased maternal mortality, and morbidity.[8,29]
In the management of placenta, we preferred to remove it as possible. This supports the idea that the success of conservative management depends on the amount of placental tissue left behind.[30] Placenta left in situ at the time of delivery may potentially increase the risk of postpartum hemorrhage and hysterectomy.[8,13,29,31] After the targeted arteries were surely embolized with blood flow markedly decreased, the placenta was removed by manual and piecemeal technique for the cases of adherent placenta in our study. Placenta removal and prophylactic antibiotics reduced hysterectomy rate and prevented complications of endometritis.
Fetal radiation exposure was present in our study group. Owing to the radiological machine, fetal radiation doses could not be calculated. The section of catheter placement was optimized to reduce fetal exposure before delivery. Most related studies faced fetal radiation exposure.[7,14] Kai et al[32] found that the fetal radiation doses ranged from 12.88 to 31.6 mGy in prophylactic internal iliac artery balloon occlusion. At doses of <50 mGy, the risk of harmful effects to the fetus is considered negligible.[33] Yu et al tried to conduct catheter insertion and UAE after fetal delivery, so there was no fetal radiation in 11 cases. However, 2 patients undertook emergency hysterectomy because of massive bleeding.[13] Thus, fetal radiation exposure is a challenge of interventional radiology in the Obstetrics. A hybrid operation room, high-quality fluoroscopy equipment, and optimized preoperative catheter placement are helpful to reduce the time of angiographic catheterization and fetal exposure.[14]
Limitations of this study included the relatively small sample, retrospective design, and potential harm of fetal radiation exposure. Fetal radiation doses could not be measured, which failed to evaluate the risk of long-term harmful effects on babies. Antepartum MRI and later pathologic diagnosis were not performed to clarify placenta accreta/increta. The effectiveness was not compareed between UAE and IIAE in this study because the later was the alternative to the former during the management.
In conclusion, UAE or alternative IIAE may be an effective strategy to control intraoperative bleeding and preserve the uterus in patients with pernicious placenta previa during scheduled caesarean delivery in the third trimester of pregnancy. In the future, prospective and controlled studies would further compare the efficacy and success of this strategy with other managements, such as UAE alone, or combined internal iliac artery balloon occlusion and UAE.
Acknowledgment
The authors acknowledge all patients included in the study.
Author contributions
Conceptualization: Juan Wang, Youguo Chen, Jinhua Zhou.
Data curation: Juan Wang, Xiu Shi, Yan Li, Zhi Li, Youguo Chen, Jinhua Zhou.
Formal analysis: Juan Wang, Xiu Shi, Yan Li, Zhi Li, Jinhua Zhou.
Investigation: Juan Wang, Yan Li, Zhi Li, Youguo Chen, Jinhua Zhou.
Methodology: Juan Wang, Xiu Shi, Yan Li, Zhi Li, Jinhua Zhou.
Project administration: Juan Wang, Zhi Li, Youguo Chen, Jinhua Zhou.
Resources: Juan Wang, Xiu Shi, Yan Li, Zhi Li, Jinhua Zhou.
Software: Juan Wang, Xiu Shi, Jinhua Zhou.
Supervision: Juan Wang, Zhi Li, Youguo Chen, Jinhua Zhou.
Validation: Juan Wang, Zhi Li, Jinhua Zhou.
Visualization: Juan Wang, Yan Li, Youguo Chen, Jinhua Zhou.
Writing – original draft: Juan Wang, Yan Li, Jinhua Zhou.
Writing – review & editing: Juan Wang, Jinhua Zhou.
Footnotes
Abbreviations: IIAE = internal iliac artery embolization, UAE = uterine artery embolization.
How to cite this article: Wang J, Shi X, Li Y, Li Z, Chen Y, Zhou J. Prophylactic intraoperative uterine or internal iliac artery embolization in planned cesarean for pernicious placenta previa in the third trimester of pregnancy. Medicine. 2019;98:44(e17767).
XS is the co-first author.
The authors report no conflicts of interest.
References
- [1].Bauer ST, Bonanno C. Abnormal placentation. Semin Perinatol 2009;33:88–96. [DOI] [PubMed] [Google Scholar]
- [2].Downes KL, Hinkle SN, Sjaarda LA, et al. Previous prelabor or intrapartum cesarean delivery and risk of placenta previa. Am J Obstet Gynecol 2015;212:669 e661–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hasegawa J, Matsuoka R, Ichizuka K, et al. Predisposing factors for massive hemorrhage during Cesarean section in patients with placenta previa. Ultrasound Obstet Gynecol 2009;34:80–4. [DOI] [PubMed] [Google Scholar]
- [4].Usta IM, Hobeika EM, Musa AA, et al. Placenta previa-accreta: risk factors and complications. Am J Obstet Gynecol 2005;193(3 pt 2):1045–9. [DOI] [PubMed] [Google Scholar]
- [5].Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of cesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol 1997;177:1071–8. [DOI] [PubMed] [Google Scholar]
- [6].Onwere C, Gurol-Urganci I, Cromwell DA, et al. Maternal morbidity associated with placenta praevia among women who had elective caesarean section. Eur J Obstet Gynecol Reprod Biol 2011;159:62–6. [DOI] [PubMed] [Google Scholar]
- [7].Bodner LJ, Nosher JL, Gribbin C, et al. Balloon-assisted occlusion of the internal iliac arteries in patients with placenta accreta/percreta. Cardiovasc Intervent Radiol 2006;29:354–61. [DOI] [PubMed] [Google Scholar]
- [8].D'Souza DL, Kingdom JC, Amsalem H, et al. Conservative management of invasive placenta using combined prophylactic internal iliac artery balloon occlusion and immediate postoperative uterine artery embolization. Can Assoc Radiol J 2015;66:179–84. [DOI] [PubMed] [Google Scholar]
- [9].Khan M, Sachdeva P, Arora R, et al. Conservative management of morbidly adherant placenta - a case report and review of literature. Placenta 2013;34:963–6. [DOI] [PubMed] [Google Scholar]
- [10].Peng ZH, Xiong Z, Zhao BS, et al. Prophylactic abdominal aortic balloon occlusion: an effective method of controlling hemorrhage in patients with placenta previa or accreta. Exp Ther Med 2019;17:1492–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shahin AY, Farghaly TA, Mohamed SA, et al. Bilateral uterine artery ligation plus B-Lynch procedure for atonic postpartum hemorrhage with placenta accreta. Int J Gynaecol Obstet 2010;108:187–90. [DOI] [PubMed] [Google Scholar]
- [12].Chen M, Xie L. Clinical evaluation of balloon occlusion of the lower abdominal aorta in patients with placenta previa and previous cesarean section: a retrospective study on 43 cases. Int J Surg 2016;34:6–9. [DOI] [PubMed] [Google Scholar]
- [13].Yu PC, Ou HY, Tsang LL, et al. Prophylactic intraoperative uterine artery embolization to control hemorrhage in abnormal placentation during late gestation. Fertil Steril 2009;91:1951–5. [DOI] [PubMed] [Google Scholar]
- [14].Lim HJ, Kim JY, Kim YD, et al. Intraoperative uterine artery embolization without fetal radiation exposure in patients with placenta previa totalis: two case reports. Obstet Gynecol Scisnce 2013;56:45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Li N, Yang T, Liu C, et al. Feasibility of infrarenal abdominal aorta balloon occlusion in pernicious placenta previa coexisting with placenta accrete. BioMed Res Int 2018;2018:4596189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Chauleur C, Fanget C, Tourne G, et al. Serious primary post-partum hemorrhage, arterial embolization and future fertility: a retrospective study of 46 cases. Hum Reprod 2008;23:1553–9. [DOI] [PubMed] [Google Scholar]
- [17].Pan Y, Zhou X, Yang Z, et al. Retrospective cohort study of prophylactic intraoperative uterine artery embolization for abnormally invasive placenta. Int J Gynaecol Obstet 2017;137:45–50. [DOI] [PubMed] [Google Scholar]
- [18].Maassen MS, Lambers MD, Tutein Nolthenius RP, et al. Complications and failure of uterine artery embolisation for intractable postpartum haemorrhage. BJOG 2009;116:55–61. [DOI] [PubMed] [Google Scholar]
- [19].Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol 2006;107:927–41. [DOI] [PubMed] [Google Scholar]
- [20].Chaudhari HK, Shah PK, D'Souza N. Morbidly adherent placenta: its management and maternal and perinatal outcome. J Obstet Gynaecol India 2017;67:42–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Crane JM, Van den Hof MC, Dodds L, et al. Maternal complications with placenta previa. Am J Perinatol 2000;17:101–5. [DOI] [PubMed] [Google Scholar]
- [22].Chou MM, Hwang JI, Tseng JJ, et al. Internal iliac artery embolization before hysterectomy for placenta accreta. J Vasc Interv Radiol 2003;14(9 pt 1):1195–9. [DOI] [PubMed] [Google Scholar]
- [23].Sidhu HK, Prasad G, Jain V, et al. Pelvic artery embolization in the management of obstetric hemorrhage. Acta Obstet Gynecol Scand 2010;89:1096–9. [DOI] [PubMed] [Google Scholar]
- [24].Al-Thunyan A, Al-Meshal O, Al-Hussainan H, et al. Buttock necrosis and paraplegia after bilateral internal iliac artery embolization for postpartum hemorrhage. Obstet Gynecol 2012;120(2 pt 2):468–70. [DOI] [PubMed] [Google Scholar]
- [25].Lo TK, So CH, Yeung SW, et al. Comparison of selective and non-selective internal iliac artery embolization for abnormal placentation with major postpartum hemorrhage. Int J Gynaecol Obstet 2017;136:103–4. [DOI] [PubMed] [Google Scholar]
- [26].Kume K, Y. MT, Soga T, et al. A case of placenta percreta with massive hemorrhage during cesarean section. J Med Invest 2014;61:208–12. [DOI] [PubMed] [Google Scholar]
- [27].Dilauro MD, Dason S, Athreya S. Prophylactic balloon occlusion of internal iliac arteries in women with placenta accreta: literature review and analysis. Clin Radiol 2012;67:515–20. [DOI] [PubMed] [Google Scholar]
- [28].Picone O, Salomon LJ, Ville Y, et al. Fetal growth and Doppler assessment in patients with a history of bilateral internal iliac artery embolization. J Matern Fetal Neonatal Med 2003;13:305–8. [DOI] [PubMed] [Google Scholar]
- [29].Konishi Y, Yamamoto S, Sugiki K, et al. A novel and multidisciplinary strategy for cesarean delivery with placenta percreta: intraoperative embolization in a hybrid suite. A & A case reports 2016;7:135–8. [DOI] [PubMed] [Google Scholar]
- [30].Timmermans S, van Hof AC, Duvekot JJ. Conservative management of abnormally invasive placentation. Obstetrical & gynecological survey 2007;62:529–39. [DOI] [PubMed] [Google Scholar]
- [31].Chung MY, Cheng YK, Yu SC, et al. Nonremoval of an abnormally invasive placenta at cesarean section with postoperative uterine artery embolization. Acta Obstet Gynecol Scand 2013;92:1250–5. [DOI] [PubMed] [Google Scholar]
- [32].Kai K, Hamada T, Yuge A, et al. Estimating the radiation dose to the fetus in prophylactic internal iliac artery balloon occlusion: three cases. Case Rep Obstet Gynecol 2015;2015:170343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Patel SJ, Reede DL, Katz DS, et al. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics 2007;27:1705–22. [DOI] [PubMed] [Google Scholar]


