Abstract
Infection with influenza virus increases morbidity and mortality in patients with risk factors, including cardiovascular disease (CVD). This study aimed to evaluate factors associated with influenza vaccination coverage in Korean CVD patients.
We included 19,599 adults from the 2010 to 2012 Korea National Health and Nutrition Examination Survey. Influenza vaccination rates were compared in subjects with and without CVD. Logistic regression analysis was performed to identify factors associated with influenza vaccination in Korean adults with CVD before and after stratification for age (<65 and ≥65 years).
Significantly higher vaccination rates were observed in individuals with CVD than in those without CVD (61.4% vs 31.0%, P < .001). However, young individuals (19–49 years) had decreased influenza vaccination rates, with no difference based on CVD status (20.3% vs 21.6%, P = .859). A lack of private insurance (odds ratio [OR], 0.47; 95% confidence interval [CI], 0.23–0.98) and recent health screening (OR, 4.56; 95% CI, 1.90–10.92) were independent factors for influenza vaccination in CVD patients aged <65 years, whereas female sex (OR, 3.71; 95% CI, 1.24–11.07) and less education (OR, 4.59; 95% CI, 1.27–16.61) were independent factors in CVD patients aged ≥65 years.
Improving influenza vaccination coverage for Korean adults with CVD is important, especially in young patients. For young patients with CVD, influenza vaccination status is independently associated with the presence of private insurance and recent health screening. This finding could help establish public health policies to promote influenza vaccination in this population.
Keywords: cardiovascular disease, influenza, Korean, vaccination
1. Introduction
Influenza is an acute respiratory illness caused by influenza A or B viruses. It occurs in epidemics nearly every year, mainly during the winter season in temperate climates. Annual influenza vaccination is an important public health measure for preventing influenza infection. Prevention is key because influenza infection is associated with increased morbidity and mortality not only in infants, pregnant women, and elderly but also in people with cardiovascular disease (CVD), diabetes mellitus, asthma, obstructive pulmonary disease, and malignancy who are more vulnerable to serious complications.[7,18]
CVD continues to be a major public health problem worldwide. An estimated 17.9 million people died from CVD in 2016, accounting for 31% of all global deaths. Of these deaths, 85% were because of heart attack and stroke.[2] In Korea, CVD is now one of the leading preventable causes of death, resulting in 22% of all deaths in 2011.[1] For patients with CVD, the risk of mortality and serious complications owing to influenza infection is especially high.[3,4,11,14,19] In addition, cardiovascular-related death is the leading cause of mortality during the influenza season.[4,14,19] Numerous studies have suggested an association between influenza and increased risk of cardiovascular events. For example, meta-analyses and systematic reviews suggested that influenza serves as a trigger for acute myocardial infarction.[3,8,19] Although recent studies have focused the early detection and risk stratification of CVD with advanced imaging techniques,[10,21,22] it is important to prevent complications by preventing potential risks for public health.
Current guidelines from the Centers for Disease Control and Prevention highly recommend annual influenza vaccinations for adults and children with CVD (excluding isolated hypertension).[7] Some studies have examined the prevalence of influenza vaccination coverage and the associated factors among Korean populations.[9,12,16,17] However, influenza vaccination rates and factors associated with vaccination status have not been evaluated among Korean adults with CVD. It is important to clarify the rate of influenza vaccination among individuals with CVD and identify associated factors that affect influenza vaccination rates. These findings may help identify subgroups that benefit from preventative interventions. Therefore, this study examined factors associated with the vaccination rate in Korean adults with CVD using nationally representative data.
2. Methods
2.1. Study population
We used data collected during the fifth Korea National Health and Nutrition Examination Survey (KNHANES), which was conducted by the Korean Center for Disease Control and Prevention (KCDC) from January 2010 to December 2012.
KNHANES is a cross-sectional, nationally representative, and reliable study for determining the health and nutritional status of the civilian, noninstitutionalized, Korean population. The survey includes health and household interviews, nutrition surveys, and direct standardized physical examinations. KNHANES was approved by the institutional review board of the KCDC, and all participants signed a written consent form. The present study and the use of KNHANES data were approved by the KCDC.
For KNHANES, participants were selected by proportional allocation-systematic sampling with multistage stratification (age, sex, and region). Of the 19,599 adults (>19 years old) that participated in KNHANES (2010–2012), 17,872 adults with available information regarding CVD and influenza vaccination were included in the analysis.
2.2. Variables
2.2.1. CVD
A history of CVD was defined as a physician's diagnosis of any of the following: stroke, myocardial infarction, or angina.
2.2.2. Influenza vaccination
Information on the seasonal influenza vaccination status in the past 12 months was obtained.
2.2.3. Independent variables
Independent variables that have been associated with screening practice included socio-demographic variables (age, sex, marital status, education level, and household income, insurance status, private insurance, and body mass index [BMI]) and health-related lifestyle factors (drinking and exercise), and health status (history of chronic disease such as hypertension, diabetes, and dyslipidemia, and perceived health status) as well as recent health screening.
Socio-demographic variables were current age (19–49, 50–64, and ≥65 years), marital status (unmarried, separated, widowed, and divorced subjects were allocated a “no spouse” status), national insurance state (national health insurance, medical aid, or not involved in either), private health insurance (no, yes), and obesity (BMI <25 or ≥25 kg/m2).[6] BMI was calculated by dividing weight (kg) by the square of height (m2). Household income level was divided into national quartile groups (lowest quartile, 2nd and 3rd quartile, highest quartile). Education level was categorized as less than elementary, middle/high, or college and higher.
For health-related lifestyle factors, drinking behavior was assessed using the Alcohol Use Disorders Identification Test (in which scores ≥12 and <12 indicate heavy and nonheavy drinkers, respectively).[13] Routine exercisers were defined as people who performed at least low-intensity physical activity, which was defined as walking or commuting for >30 minutes more than 3 times per week.
Comorbidities include self-reported physician's diagnosis of hypertension, diabetes, and dyslipidemia, and perceived health status (good, normal, bad). Participants provided “yes” or “no” responses to questions regarding recent health screening, such as “have you undergone a health check-up within the last 2 years?”
2.3. Statistical analysis
Results are presented as percentages (± standard errors of percentages) for categorical variables and estimated means (± standard errors of means) for continuous variables. Categorical variables and continuous variables were compared using the Chi-square test or Student t test for comparison between respondents with and without CVD.
Influenza vaccination coverage according to variables was compared in subjects with and without CVD. Finally, logistic regression analysis was used to identify factors associated with influenza vaccination in Korean adults with CVD before and after stratification for age (age, <65 and ≥65 years).
All analyses were adjusted for the complex survey design in KNHANES using the complex sample analysis program in PASW 18.0 (SPSS Inc, Chicago, IL, USA). A P-value of <.05 (2-sided) was considered significant.
3. Results
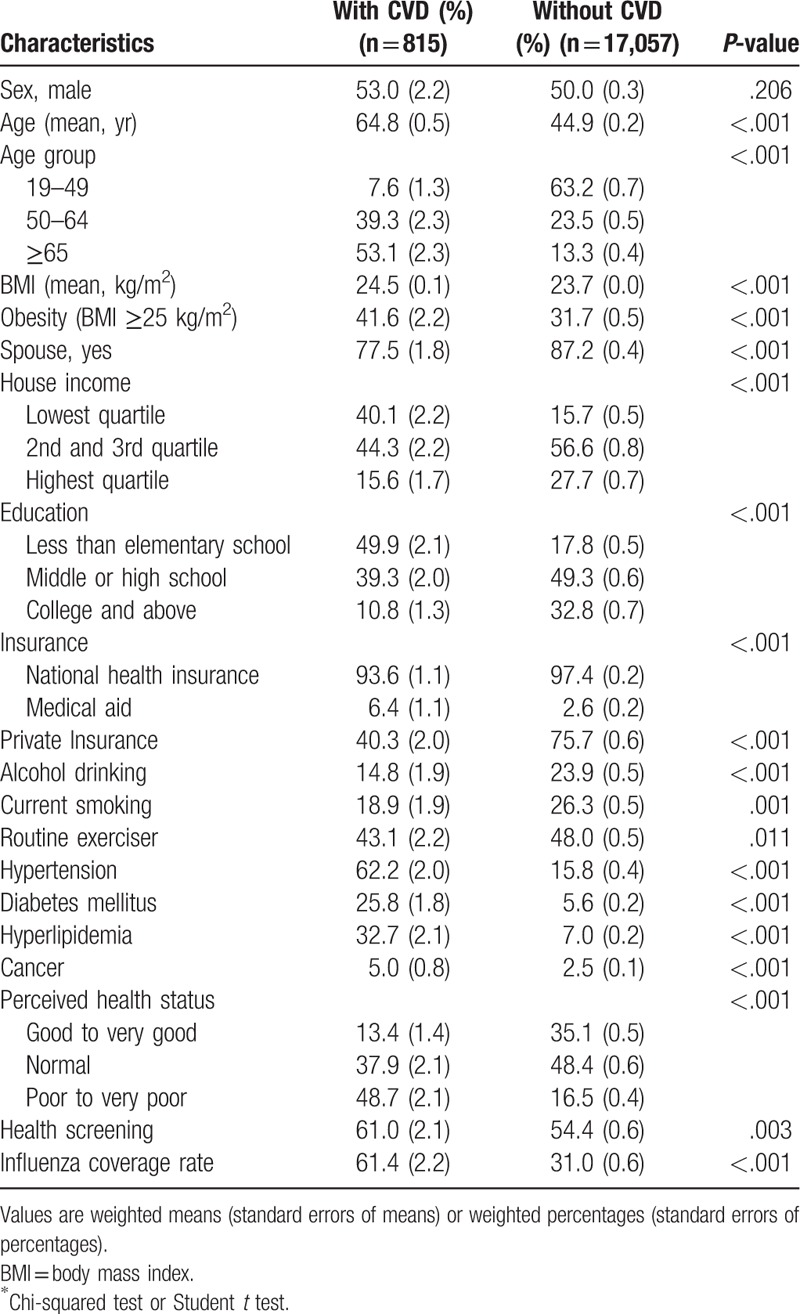
Information regarding CVD and influenza vaccination was available in 17,872 adults involved in the survey. Their clinical characteristics are summarized in Table 1. Higher proportions of old age, obesity, low house income, less education, more medical aid, poorer self-rated health, more health screenings within the last 2 years, and more comorbid diseases (hypertension, diabetes, hyperlipidemia, cancer) were observed in the CVD group than in the non-CVD group.
Table 1.
Characteristics of Korean adults with and without cardiovascular disease (CVD).
Comparisons of influenza vaccination coverage between subjects with and without CVD are shown in Table 2. The overall vaccination rate was significantly higher in the CVD group than in the non-CVD group (61.4% vs 31.0%, P < .001). The subgroup analysis showed that except in the young age group (19–49 years) and those receiving medical aid, the influenza vaccination rate was significantly higher for individuals with CVD.
Table 2.
Influenza vaccination status according to variables in Korean adults with and without cardiovascular disease (CVD).
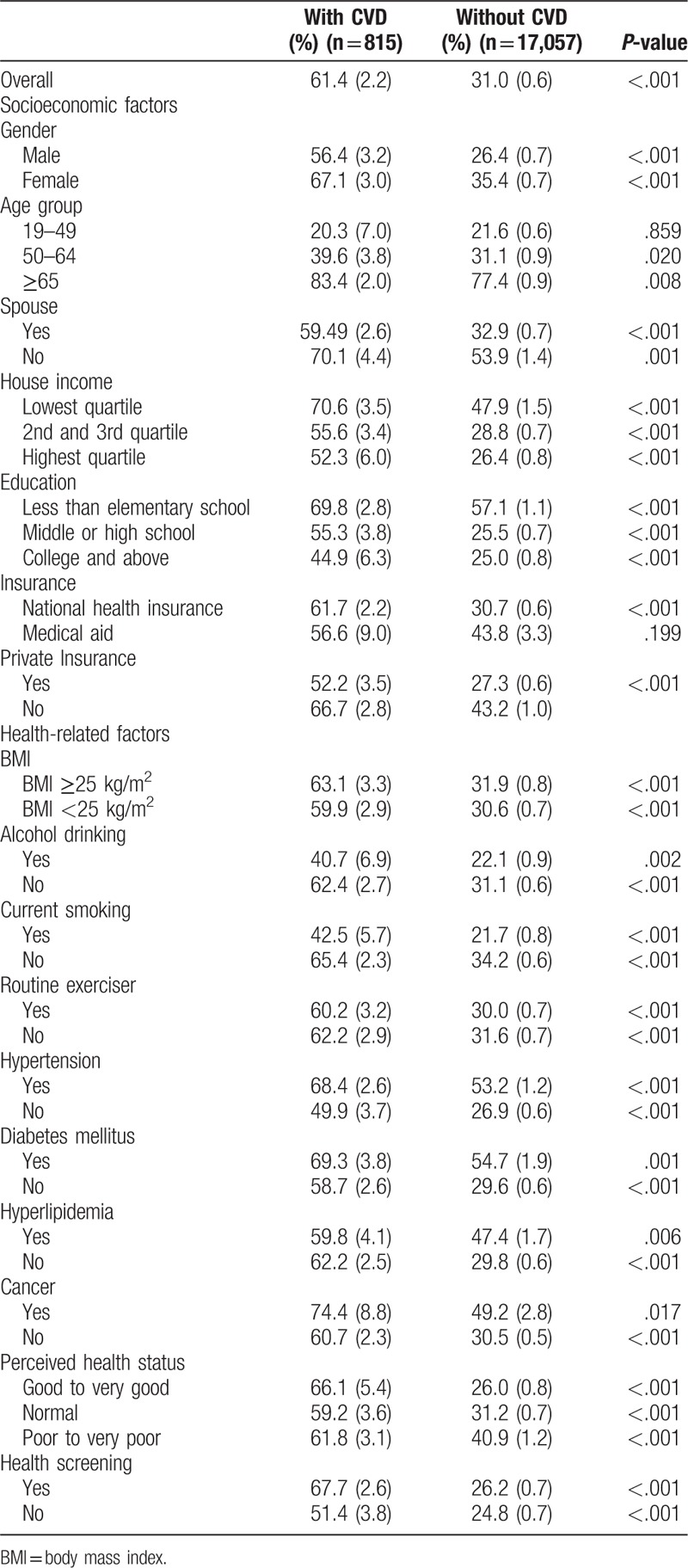
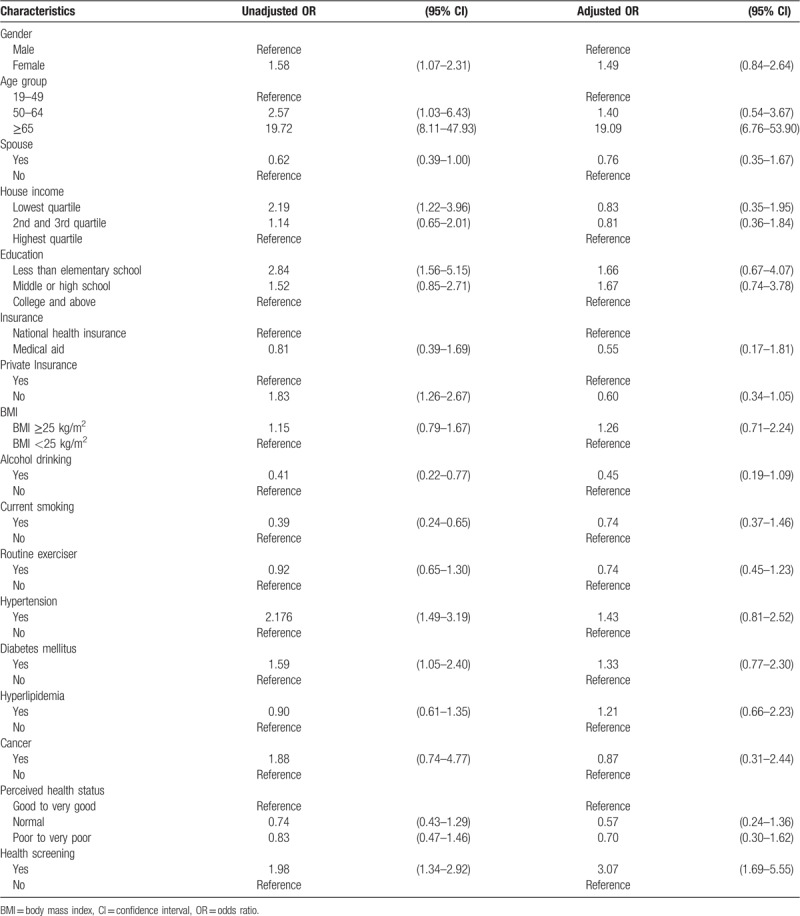
Table 3 shows the univariable and multivariable logistic regression analyses for influenza vaccination coverage among subjects with CVD. Old age (odds ratio [OR], 19.09; 95% confidence interval [95% CI], 6.76–53.90) and recent health screening (OR, 3.07; 95% CI, 1.69–5.55) were independent factors associated with influenza vaccination in the CVD group.
Table 3.
Variables associated with influenza vaccination status among Korean adults with cardiovascular disease.
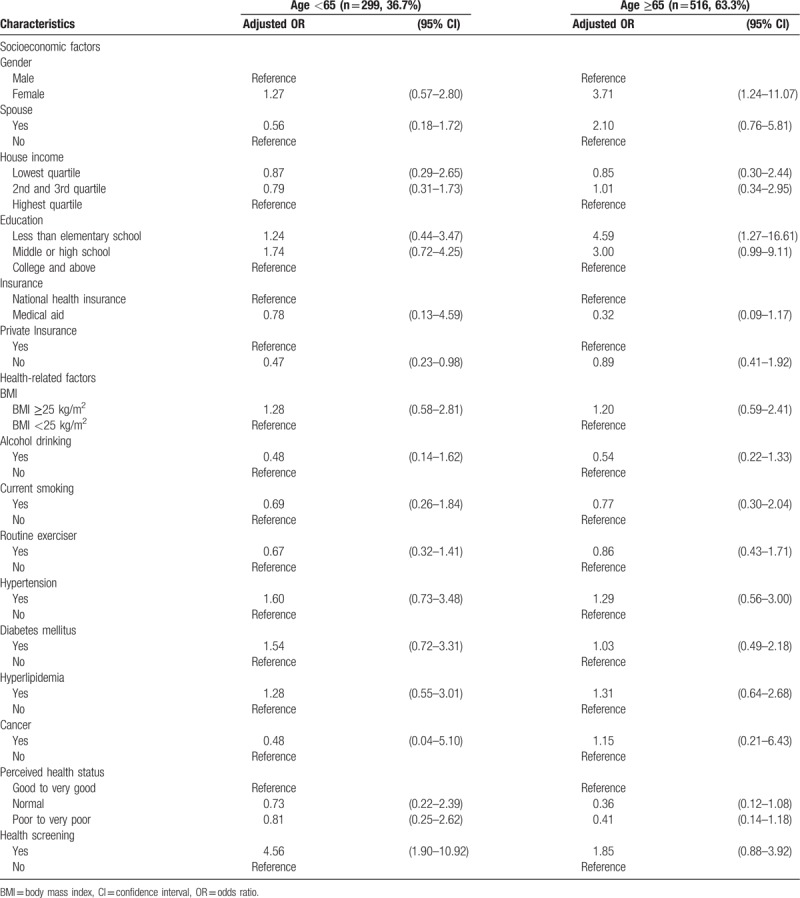
After stratification for age (<65 years and ≥65 years), the significant predictors of influenza vaccination were slightly different (Table 4); for subjects aged <65 years, lack of private insurance (OR, 0.47; 95% CI, 0.23–0.98), recent health screening (OR, 4.56; 95% CI, 1.90–10.92) were independent factors associated with vaccination status. Whereas in individuals ≥65 years, female sex (OR, 3.71; 95% CI, 1.24–11.07) and less education (OR, 4.59; 95% CI, 1.27–16.61) were independent factors associated with influenza vaccination coverage.
Table 4.
Multivariable logistic regression analysis for influenza vaccination status in Korean adults with CVD according to age.
4. Discussion
We demonstrated that influenza vaccination coverage was significantly higher in subjects with CVD than in those without CVD. Furthermore, old age (≥65 years) and recent health screening were independent predictors of influenza vaccination in Korean adults with CVD. Our study showed that 83.4% of elderly (≥65 years) CVD patients received influenza vaccinations. However, the vaccination rates of young (19–49 years) and middle-aged (50–64 years) individuals with CVD were only 20.3% and 39.6%, respectively. This finding is in contrast to current recommendations for individuals with CVD to receive the influenza vaccination, regardless of age, to prevent serious morbidity and mortality. In the young age group, the influenza vaccination rate was not significantly different in subjects with and without CVD. Thus, Korea requires a policy to increase influenza vaccine uptake in risk groups, especially in CVD patients younger than 65 years old.
High levels of influenza vaccination uptake among older individuals may be explained by Korean policies with offer influenza vaccination free of charge to the elderly but not younger individuals. The Ministry of Health and Welfare, together with the KCDC, offers free influenza immunization for the elderly (≥65 years). Furthermore, older individuals are more likely to suffer from chronic illnesses such as diabetes and hypertension, which can lead to more physician visits and follow up and increases the likelihood of a receiving an immunization recommendation.[5,15] After stratification for age in subjects with CVD, female sex and less education were significant indicators for influenza vaccination coverage in the old age group (≥65 years) and presence of private insurance and recent health screenings were independently associated with influenza vaccination in the young age group (<65 years). The present study did not show that health-related factors except recent health screening was associated with influenza vaccination rates, whereas other studies have shown that regular exercise is a positive predictor of vaccination uptake.[20]
Based on the prevalence of influenza vaccine uptake in CVD patients, this study suggests that public health policy should target groups according to age. The low vaccination rate among young CVD patients suggests the need for social and financial support for this population. In addition to the typical barriers (availability of vaccine, cost), young CVD patients may not perceive the need for vaccination. Thus, healthcare workers should encourage the use of the influenza vaccination in CVD patients, especially for those <65 years of age.
This study has several limitations. First, some response bias may have been introduced when subjects were asked questions about influenza vaccination. This survey explored whether participants were vaccinated during the past year, so there is a potential for recall bias as well. Furthermore, this question could not reflect previous vaccine history and the reason why they vaccinated or not. Second, the cross-sectional study design was inherently constrained by the retrospective use of an existing health data set which did not assess severity of CVD. Nonetheless, the results of this study are reliable and of value because the study was conducted using nationally representative, population-based data.
5. Conclusions
In conclusion, it is important to improve influenza vaccination coverage for Korean adults with CVD, especially in non-elderly individuals. For non-elderly CVD patients, significant predictors for influenza vaccination are the presence of private insurance and recent health screening. This finding could help establish public health policy to promote influenza vaccine uptake rates in this population to decrease mortality and morbidity at the risk of influenza infection.
Author contributions
Conceptualization: Pyung Chun Oh.
Data curation: Eun Young Kim.
Formal analysis: Eun Young Kim.
Funding acquisition: Eun Young Kim.
Methodology: Eun Young Kim, Young Saing Kim.
Resources: Eun Young Kim, Young Saing Kim.
Validation: Eun Young Kim, Pyung Chun Oh.
Writing – original draft: Eun Young Kim, Jae Ho Ko.
Writing – review & editing: Eun Young Kim, Jae Ho Ko, Young Saing Kim, Pyung Chun Oh.
Young Saing Kim orcid: 0000-0003-0207-2617
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, CVD = cardiovascular disease, KCDC = Korean Center for Disease Control and Prevention, KNHANES = Korea National Health and Nutrition Examination Survey, OR = odds ratio.
How to cite this article: Kim EY, Ko JH, Kim YS, Oh PC. Prevalence and associated factors of influenza vaccination coverage in Korean adults with cardiovascular disease. Medicine. 2020;99:1(e18540).
EYK and JHK contributed equally to this work and share first authorship.
This research was supported by MD-PhD research through the Korea Research-Driven Hospital (grant 2018-5287) and the National research foundation of Korea (grant NRF-2018R1C1B5086352).
The authors have no conflicts of interest to disclose.
References
- [1]. National Bureau of Statistics, Republic of Korea. Annual report on the cause of death statistics. Seoul, Republic of Korea, 2011. [Google Scholar]
- [2].World Health Organization. Cardiovascular diseases (CVDs) [Data file]. Available at: http://www.who.int/mediacentre/factsheets/fs317/en/index.html Accessed: August, 9 2019. [Google Scholar]
- [3].Barnes M, Heywood AE, Mahimbo A, et al. Acute myocardial infarction and influenza: a meta-analysis of case-control studies. Heart 2015;101:1738–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Caldeira D, Ferreira JJ, Costa J. Influenza vaccination and prevention of cardiovascular disease mortality. Lancet (London, England) 2018;391:426–7. [DOI] [PubMed] [Google Scholar]
- [5].Chung JH, Kim TH, Han CH. Factors influencing influenza vaccination among South Korean adult asthma patients: a nationwide population-based cross-sectional study. J Asthma 2018;55:294–9. [DOI] [PubMed] [Google Scholar]
- [6].WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63. [DOI] [PubMed] [Google Scholar]
- [7].Grohskopf LA, Sokolow LZ, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices - United States, 2017-18 influenza season. MMWR Recommend Rep 2017;66:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gross PA, Hermogenes AW, Sacks HS, et al. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann Intern Med 1995;123:518–27. [DOI] [PubMed] [Google Scholar]
- [9].Kwon DS, Kim K, Park SM. Factors associated with influenza vaccination coverage among the elderly in South Korea: the Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV). BMJ Open 2016;6:e012618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Liu X, Wang Y, Zhang H, et al. Evaluation of fractional flow reserve in patients with stable angina: can CT compete with angiography? European radiology 2019;29:3669–77. [DOI] [PubMed] [Google Scholar]
- [11].MacIntyre CR, Mahimbo A, Moa AM, et al. Influenza vaccine as a coronary intervention for prevention of myocardial infarction. Heart 2016;102:1953–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Oh MG, Han MA, Yun NR, et al. A population-based, nationwide cross-sectional study on influenza vaccination status among cancer survivors in Korea. Int J Environ Res Public Health 2015;12:10133–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Osaki Y, Ino A, Matsushita S, et al. Reliability and validity of the alcohol use disorders identification test - consumption in screening for adults with alcohol use disorders and risky drinking in Japan. Asian Pac J Cancer Prev 2014;15:6571–4. [DOI] [PubMed] [Google Scholar]
- [14].Reichert TA, Simonsen L, Sharma A, et al. Influenza and the winter increase in mortality in the United States. Am J Epidemiol 2004;160:492–502. [DOI] [PubMed] [Google Scholar]
- [15].Ryu SY, Kim SH, Park HS, et al. Influenza vaccination among adults 65 years or older: a 2009-2010 community health survey in the Honam region of Korea. Int J Environ Res Public Health 2011;8:4197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Shin HY, Chung JH, Hwang HJ, et al. Factors influencing on influenza vaccination and its trends of coverage in patients with diabetes in Korea: a population-based cross-sectional study. Vaccine 2018;36:91–7. [DOI] [PubMed] [Google Scholar]
- [17].Shin HY, Hwang HJ, Chung JH. Factors influencing influenza vaccination among patients with chronic obstructive pulmonary disease: a population-based cross-sectional study. Asia-Pacific J Public Health 2017;29:560–8. [DOI] [PubMed] [Google Scholar]
- [18].Simonsen L, Clarke MJ, Williamson GD, et al. The impact of influenza epidemics on mortality: introducing a severity index. Am J Public Health 1997;87:1944–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Warren-Gash C, Smeeth L, Hayward AC. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: a systematic review. Lancet Infect Dis 2009;9:601–10. [DOI] [PubMed] [Google Scholar]
- [20].Wu S, Yang P, Li H, et al. Influenza vaccination coverage rates among adults before and after the 2009 influenza pandemic and the reasons for non-vaccination in Beijing, China: a cross-sectional study. BMC Public Health 2013;13:636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Xu L, Huang X, Ma J, et al. Value of three-dimensional strain parameters for predicting left ventricular remodeling after ST-elevation myocardial infarction. The international journal of cardiovascular imaging 2017;33:663–73. [DOI] [PubMed] [Google Scholar]
- [22].Zhang N, Yang G, Gao Z, et al. Deep Learning for Diagnosis of Chronic Myocardial Infarction on Nonenhanced Cardiac Cine MRI. Radiology 2019;291:606–17. [DOI] [PubMed] [Google Scholar]


