Abstract
The aim of this study was to evaluate the safety and efficacy of percutaneous vertebroplasty (PVP) in Kambin triangle approach for the treatment of osteoporotic vertebral compression fractures (OVCFs).
Between November 2017 and September 2018, 109 patients (144 vertebral bodies) with OVCFs, with a mean age of 76.7 ± 9.9 years (55–96 years), underwent PVP in Kambin triangle approach. The time of operation, the volume of bone cement, the incidence of complication, the Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) score, the position of puncture needles, and the spread of polymethylmethacrylate (PMMA) in vertebral body (VB) were recorded.
All patients had been completed the operation successfully and were followed up 9.1 ± 2.9 months. The average operation time of each VB was 24.0 ± 3.5 minutes. The average volume of cement was 4.8 ± 0.6 ml. The mean VAS scores were 8.4 ± 0.7 preoperatively, 1.6 ± 0.6 at the first day postoperatively, and 1.2 ± 0.6 at the last follow-up. The mean ODI scores were 70.97 ± 7.73 preoperatively, 27.99 ± 4.12 at the first day postoperatively, and 19.65 ± 3.49 at the last follow-up. The position of puncture needles in the VB was: 119 vertebral puncture needles reached the midline, 15 were close to the midline, and 10 exceeded the midline. The spread of PMMA in the VB was: type 1 in 81 levels (56.3%), type 2 in 37 (25.7%), type 3 in 18 (12.5%), type 5 in 8 (5.5%), and no case in type 4. One case developed pneumothorax after operation. No other complications (hematoma, cement embolism, spinal cord, and nerve injury) occurred.
Kambin triangle approach in PVP, which can deliver the puncture needle to the midline of VB easily and with excellent cement distribution, is a safe and effective method.
Keywords: Kambin triangle approach, osteoporotic vertebral compression fractures, percutaneous vertebroplasty
1. Introduction
Osteoporosis, which is a systemic and metabolic bone disease, is characterized by low bone content and microarchitectural destruction of bone tissue that can increase the risk of subsequent fracture.[1,2] Osteoporotic vertebral compression fracture (OVCF) is the most common type of fracture in elderly people, and it constitutes a major health problem worldwide. OVCFs reduce the patient's quality of life and increase the burden on the public health care system.[3,4] It has been reported that OVCFs will develop in 20% of men and women older than 50 years of age and in 40% of women at the age of 80 years.[5,6]
In the past, OVCFs had been treated with bed rest, antiosteoporotic treatment, pain relief drugs, bracing, and physical rehabilitation.[7] But conservative management therapies can cause bed rest-related complications, including decubitus ulcer, deep vein thrombosis, acceleration of osteopenia, and respiratory infection.[8,9] Because of these complications, percutaneous vertebroplasty (PVP), as an alternative to conservative treatment, is an effective minimally invasive procedure widely used in the management of OVCFs. In the last decade, a bipedicular approach was the most commonly used in PVP. However, in recent years, a unipedicular approach, which offers advantages such as a shorter operation time and lower x-ray exposure, is widely used in China.[10–13]
When bone cement diffuses across the midline, the stiffness of both sides is increased and biomechanical balance is achieved.[14] However, due to the limitation of pedicle width, the transpedicular puncture needle cannot reach the midline of the vertebral body (VB) and the distribution of bone cement is restricted mainly to the puncture side. Such asymmetric cement distribution leads to an imbalance of stress on both sides. In this study, we introduce a unilateral Kambin triangle approach in PVP for treatment of OVCFs, which aims to provide better cement distribution in the VB through a single puncture.
2. Methods
This retrospective follow-up study included 109 patients (144 vertebral bodies) who suffered from single or multiple symptomatic OVCFs from November 2017 to September 2018. All patients complained of back pain and were diagnosed as acute OVCFs with high signal intensity of the fractured vertebra on magnetic resonance imaging (MRI) T2-weighted short tau inversion recovery sequences, and dual energy x-ray absorptiometry examination demonstrated T-score of each patient was <−2.5. Patients met the following criteria were excluded from this study: incurable bleeding disorders; spine infections; neurologic deficits; pathological fractures, and intolerance to surgery. There were 89 female patients and 20 male patients. The average age at surgery was 76.7 ± 9.9 years (range: 55–96 years). There were 83 patients with single vertebral fracture, 18 patients with two vertebral fractures, 7 patients with three vertebral fractures, and 1 patient with four vertebral fractures. The fractured vertebraes were from T6 to L5 (T6 in 2, T7 in 6, T8 in 6, T9 in 1, T10 in 4, T11 in 14, T12 in 23, L1 in 38, L2 in 20, L3 in 14, L4 in 7, and L5 in 9). The fractured vertebra in our patients had an anterior vertebral height decrease of 14% to 53% and kyphotic deformity of 7to 22 degree. All patients in the study underwent PVP using Kambin triangle approach after Institutional Review Board (IRB) approval was received and informed consent was obtained. Each patient was asked to quantify their pain and function on Visual Analog Scale (VAS) and Oswestry Disability Index (ODI), respectively. Patients were also asked to report any adverse effects on the nerve root such as hypesthesia or numbness and any reduction in lower limb muscle strength.
Before the operation, we used axial MRI to measure the distance from the midline to the skin puncture point. The angle of needle insertion was also measured (Fig. 1). The puncture point was established on the horizontal line of the inferior endplate of the upper VB through the skin 5 to 7 cm lateral to the midline. The first target point was the superolateral area of the responsible vertebrae, not beyond the medial margin of the ipsilateral pedicle on the anteroposterior image and the posterosuperior corner of the vertebrae on the lateral image. A trajectory line was drawn between the skin entry point and the target point. All patients were placed in the prone position. Under the guidance of the C-arm x-ray machine, 1% lidocaine was infiltrated into the skin, subcutaneous tissue, and muscles through Kambin triangle up to the periosteum of the target point. Through the route of delivery of local anesthesia, a bone cement needle (11 gauge) was gently placed over the first target point (Fig. 2) and the patient was asked whether he or she experienced any radiating pain. Then, the needle's angle and direction were adjusted to penetrate the cortex, and finally, the needle tip was located at one-third of the VB on the lateral view and approach or crossed the midline on the anteroposterior image (Fig. 3). Polymethylmethacrylate (PMMA) bone cement was continuously injected until symmetric cement distribution was obtained or cement leakage occurred. The trocar needle was not removed until bone cement had hardened (Fig. 4). x-ray film was taken at the first postoperative day (Fig. 5). This approach can be used in multiple vertebral fratrues and thoracic vertebral fracures (Figs. 6–8). All patients took regular antiosteoporosis therapy after operation.
Figure 1.
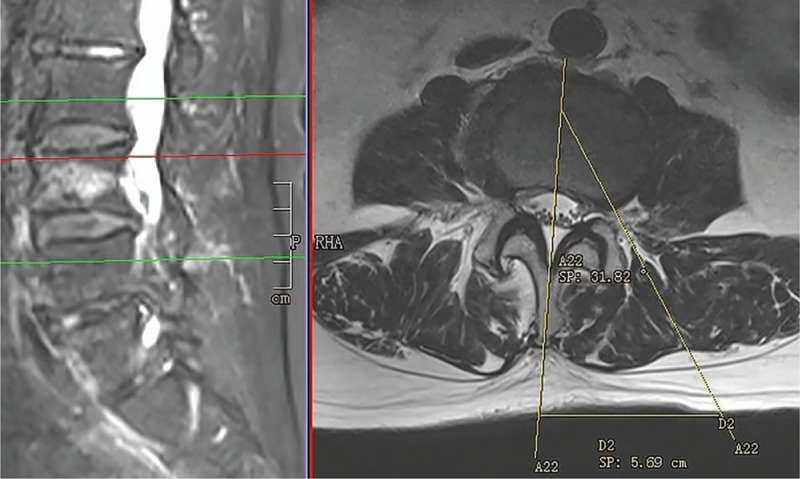
The needle trajectory and the skin entry point were calculated by using preoperative axial magnetic resonance imaging at the target level. The skin entry point was 57 mL lateral to the midline and the angle of needle insertion was about 32 degrees.
Figure 2.
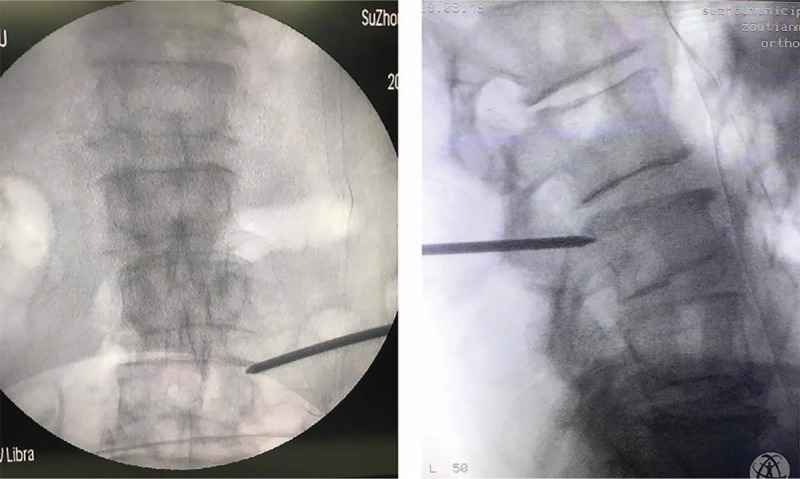
The needle was placed over the first target point. The needle tip was located in the superolateral area of the vertebral body on the anteroposterior image, and it was located at the posterosuperior side of the vertebra on the lateral image.
Figure 3.
The needle tip crossed the midline on the anteroposterior image, and it was located at one-third of the vertebral body on the lateral view.
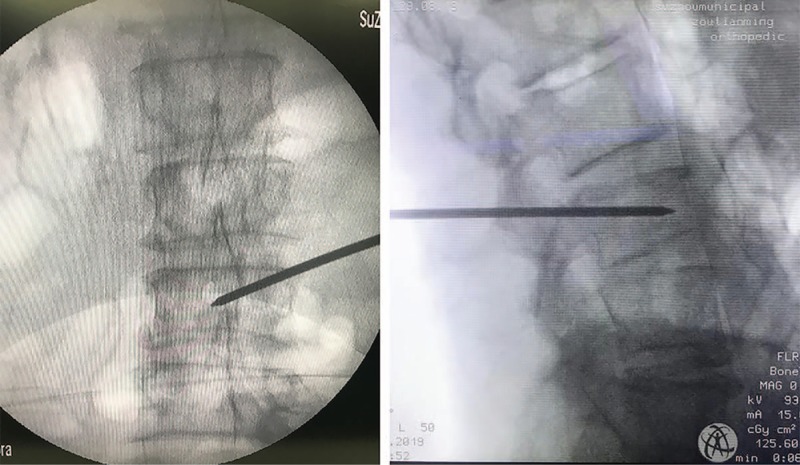
Figure 4.
Cement augmentation crossed the midline and filled the nonpunctured side.
Figure 5.
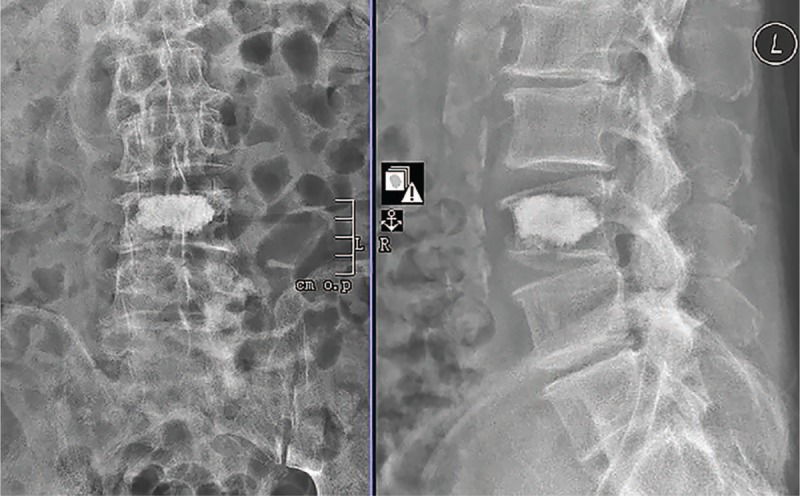
Postoperative plain radiograph showed a symmetrical cement distribution and cement leakage was not noticed.
Figure 6.
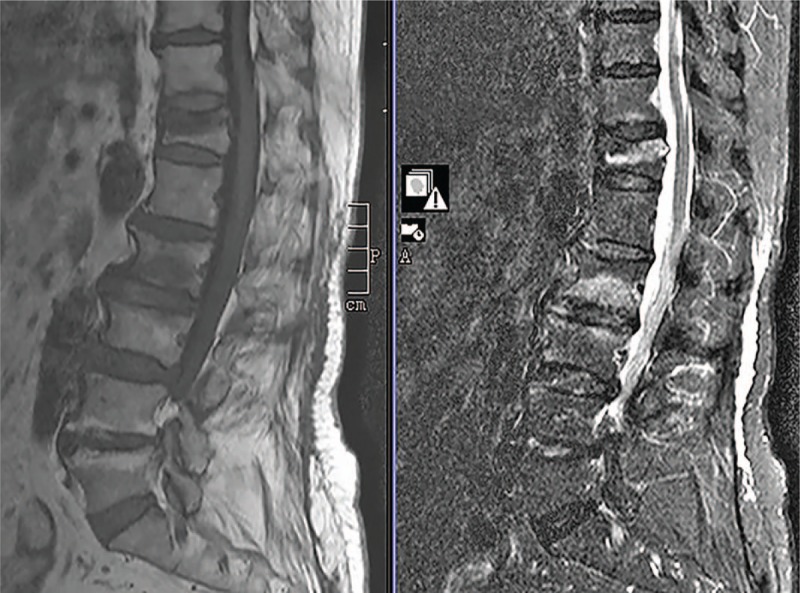
T12 and L2 had low signal intensity on T1-weighted image and high signal intensity on T2-weighted STIR image.
Figure 8.
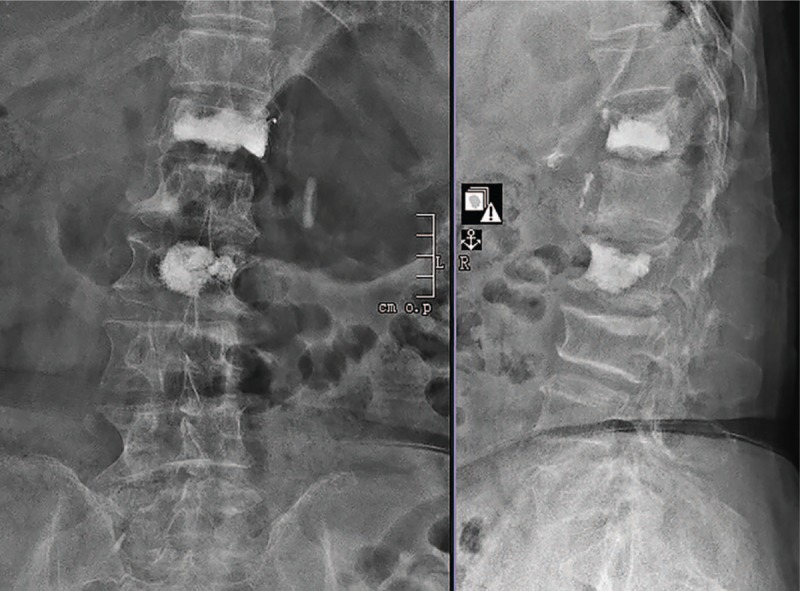
Postoperative plain radiograph showed cement distribution was symmetrical with no cement leakage.
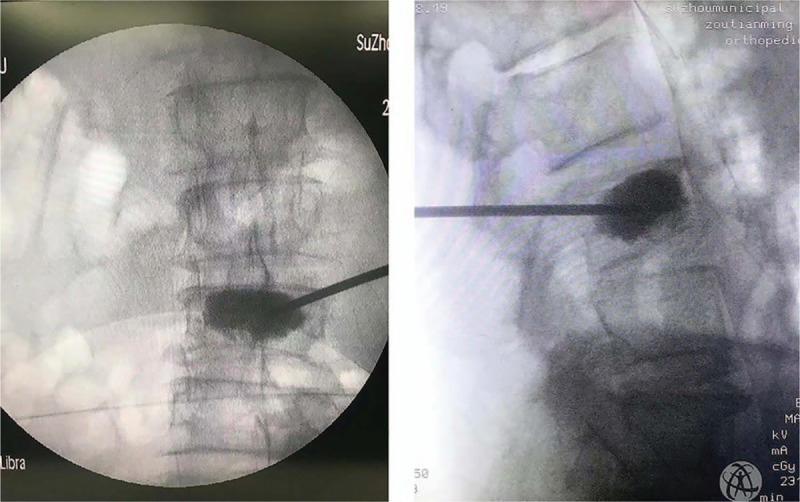
Figure 7.
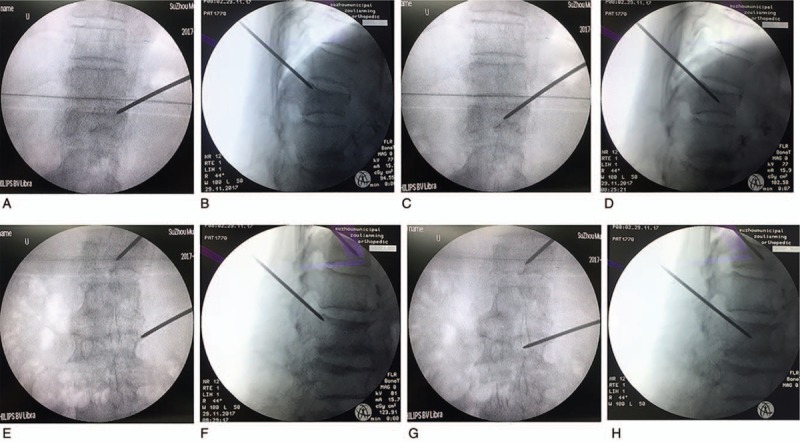
(A–H) T12 and L2 were punctured through Kambin triangle approach step by step. The puncture needle finally reached the midline of T12 and L2 on the anteroposterior image.
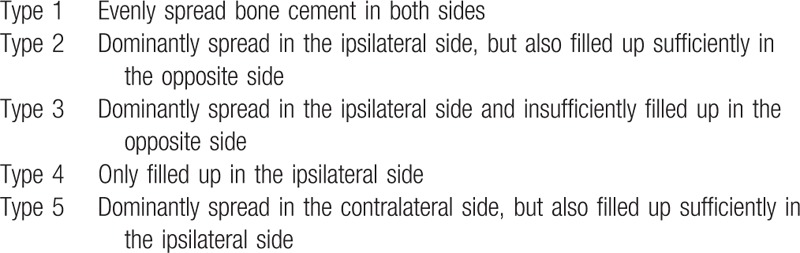
The time of operation, the volume of bone cement, the incidence of complications, the VAS and ODI score, the position of puncture needles, and the type of PMMA spread in the VB[15] (see Table 1) were recorded. Data are presented as the mean value ± standard deviation. The SPSS statistical package (version 23.0, IBM SPSS Statistics) was used for statistical analyses. P value <0.001 was considered statistically significant.
Table 1.
Classification of the type of spread of polimethylomethylacrylate in vertebral body (Ryu et al,[15] 2009).
3. Results
All patients successfully underwent the operation, and they were followed up for 9.1 ± 2.9 months. The average operation time for each VB was 24.0 ± 3.5 minutes (range: 15–35 minutes). The mean volume of PMMA cement was 4.8 ± 0.6 mL (range: 3.5–6 mL). The mean scores of VAS were 8.4 ± 0.7 preoperatively, 1.6 ± 0.6 at the first postoperative day, and 1.2 ± 0.6 at the last follow-up. The mean ODI scores were 70.97 ± 7.73 preoperatively, 27.99 ± 4.12 at the first postoperative day, and 19.65 ± 3.49 at the last follow-up. VAS and ODI scores showed a statistically significant decrease on the first postoperative day and the last follow-up (P < .001).
With respect to the position of puncture needles in the VB, 119 vertebral puncture needles reached the midline, 15 were close to the midline, and 10 crossed the midline.
The spread of PMMA in the VB was classified into the following 5 types on the anteroposterior image postoperatively: type 1 in 81 VBs (56.3%), type 2 in 37 VBs (25.7%), type 3 in 18 VBs (12.5%), type 4 in none of the VBs, and type 5 in 8 VBs (5.5%).
One case developed pneumothorax after the operation; however, no other complications, such as hematoma, cement embolism, spinal cord, and nerve injury, occurred.
4. Discussion
PVP is a safe and effective procedure in the treatment of OVCFs, which allows the patients to resume their normal daily lives as early as possible. Being a minimally invasive procedure, the standard technique is performed via the transpedicular approach. In the early stage, a bipedicular approach was typically used for the procedure. Owing to the advantages such as a shorter operative time, less radiation exposure, a unilateral approach has also been widely accepted.[11,16–19] However, with the limitation of pedicle width, the puncture needle is restricted between the midline and the ipsilateral pedicle. It is difficult to achieve satisfactory bone cement distribution through a unipedicular approach. When bone cement diffuses across the midline, both sides of the VB display a significant increase in stiffness, and biomechanical balance of stress on both sides is achieved.[14] Therefore, the puncture angle has been intentionally increased to ensure symmetrical distribution of bone cement. However, use of this approach may increase the risks of pedicle fracture, spinal cord and nerve root injury, and bone cement leakage.[20] Some researchers have used an extrapedicular approach through the transverse process in the lumbar vertebra and the costovertebral joint in the thoracic vertebra to increase the puncture angle.[21–22] But, the skin entry point in this approach totally depends on the costovertebral joint and the transverse process, which are not clearly displayed during surgery, and use of this approach may cause fracture of the transverse process and injury to the ligament complex and segmental artery.[15,23]
It is well known that the hypotenuse of Kambin triangle is the exiting nerve root and the base is the superior endplate of the caudal VB,[24] our approach through Kambin triangle to first target point which is between the lateral edge of the VB and the medial margin of the ipsilateral pedicle, is free of nerves and arteries. Heo et al reported an approach above the midline of the pedicle can avoid injury to the segmental artery.[23] In the process of puncture needle to the vertebra surface, it is kept in mind that the needle tip is located above the superior margin line of ipsilateral pedicle, which is the used method in our operation team to avoid segmental vessels.
In our study, the puncture needle was located in the soft tissue when it was placed in the safe working zone. Thus, we could adjust the puncture angle and direction so that the needle entered the VB more widely. The results showed that 129 of the 144 (89.6%) vertebral puncture needles reached or even crossed the midline, and the PMMA spread in 126 of the 144 VBs (87.5%) showed a symmetrical distribution on both sides of the VB. This confirmed that the unilateral Kambin triangle approach could easily place the puncture at the midline of the VB, along with excellent cement distribution to obtain a biomechanical balance.
The volume of bone cement injected into the fractured vertebra has been found to be closely related to the strength and stiffness of the vertebra. Molloy et al's study[25] demonstrated that restoration of VB strength and stiffness required VB volumes of 16.2% and 29.8%, respectively. Belkoff et al considered that 2 mL PMMA was enough to restore the strength of the VB. To restore stiffness, the thoracic and thoracolumbar levels required 4 ml of PMMA, whereas the lumbar region required 6 mL of PMMA.[26] Recently, a prospective cohort study by Sun et al discovered that 4 to 6 mL of PMMA could relieve the pain quickly, and cement volume accounting for 19.78% of the volume of the VB achieved satisfactory cement distribution. Nonetheless, the risk of cement leakage would also increase with the increase in cement volume.[27] The aveErage volume of bone cement used in our study was 4.8 ± 0.6 mL, which was close to the volumes reported. The mean VAS and ODI score decreased from 8.4 ± 0.7, 70.97 ± 7.73 preoperatively to 1.6 ± 0.6, 27.99 ± 4.12 on the first postoperative day; thus, VAS and ODI score showed a significant decrease on the first postoperative day (P < .001). With rapid relief of pain, the patient's quality of life was greatly improved. No severe complications, such as cement embolism, spinal cord, and nerve injury, occurred in our study. Only an early patient developed pneumothorax due to injury to the pleura. The reasons for this occurrence were as follows: the distance from the midline was too long and the angle of the puncture needle was steep. After this occurrence, lines were drawn on preoperative axial MRI to determine the entry point on the skin and the puncture angle to effectively avoid such a complication.
In our research, the Kambin triangle approach in PVP offered significant advantages. First, the approach through Kambin triangle to the safe working zone could avoid injury to the exiting nerve and segmental artery. Second, we could adjust the puncture angle and direction so as to enter the VB more widely. Hence, the puncture needle could easily reach the midline and cement augmentation crossed the midline and filled both sides of the VB. Third, the operation was performed through a unilateral approach, which could reduce the time of surgery and radiation exposure.
The limitations of our study are its retrospective design and lack of a control group. Thus, further prospective randomized controlled studies are required to prove these results.
In conclusion, Kambin triangle approach in PVP, which can deliver the puncture needle to the midline of VB easily and with excellent cement distribution, is a safe and effective method.
Author contributions
Data curation: Ye-Feng Wang, Suo-Yuan Li.
Formal analysis: Ye-Feng Wang, Suo-Yuan Li.
Investigation: Ye-Feng Wang, Xiao Yu, Tian-Ming Zou.
Project administration: Tian-Ming Zou.
Resources: Ye-Feng Wang, Jun Shen, Tian-Ming Zou.
Writing – original draft: Ye-Feng Wang, Jun Shen, Suo-Yuan Li.
Writing – review & editing: Ye-Feng Wang, Jun Shen.
Footnotes
Abbreviations: MRI = magnetic resonance imaging, ODI = Oswestry Disability Index, OVCFs = osteoporotic vertebral compression fractures, PMMA = polymethylmethacrylate, PVP = percutaneous vertebroplasty, STIR = short tau inversion recovery, VAS = Visual Analog Scale, VB = vertebral body.
How to cite this article: Yefeng W, Jun S, Suoyuan L, Xiao Y, Tianming Z. Kambin's triangle approach in percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures. Medicine. 2019;98:44(e17857).
YW and JS contributed equally to this work as co-first authors.
The authors report no conflicts of interest.
References
- [1].Yang SP, Chen CX, Wang HL, et al. A systematic review of unilateral versus bilateral percutaneous vertebroplasty/percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Acta Orthop Traumatol Turc 2017;51:290–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Pan CY, Liu XY, Li T, et al. Kinetic of bone turnover markers after osteoporotic vertebral compression fractures in postmenopausal female. J Orthop Surg Res 2018;13:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bergland A, Thorsen H, Karesen R. Association between generic and disease-specific quality of life questionnaires and mobility and balance among women with osteoporosis and vertebral fractures. Aging Clin Exp Res 2011;23:296–303. [DOI] [PubMed] [Google Scholar]
- [4].Shi C, Zhang M, Cheng AY, et al. Percutaneous kyphoplasty combined with zoledronic acid infusion in the treatment of osteoporotic thoracolumbar fractures in the elderly. Clin Interv Aging 2018;13:853–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Zhang L, Wang Q, Wang L, et al. Bone cement distribution in the vertebral body affects chances of recompression after percutaneous vertebroplasty treatment in elderly patients with osteoporotic vertebral compression fractures. Clin Interv Aging 2017;12:431–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].He ZW, Zhai QP, Hu ML, et al. Bone cements for percutaneous vertebroplasty and balloon kyphoplasty: Current status and future developments. J Orthop Translat 2015;3:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Tan E, Wang T, Pelletier MH, et al. Effects of cement augmentation on the mechanical stability of multilevel spine after vertebral compression fracture. J Spine Surg 2016;2:111–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sun HL, Li CD. Comparison of unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a systematic review and meta-analysis. J Orthop Surg Res 2016;11:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Zhang ZF, Huang H, Chen S, et al. Comparison of high- and low-viscosity cement in the treatment of vertebral compression fractures: A systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lin D, Hao J, Li L, et al. Effect of bone cement volume fraction on adjacent vertebral fractures after unilateral percutaneous kyphoplasty. Clin Spine Surg 2017;30:E270–5. [DOI] [PubMed] [Google Scholar]
- [11].Zhang L, Liu Z, Wang J, et al. Unipedicular versus bipedicular percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a prospective randomized study. BMC Musculoskelet Disord 2015;16:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Xu JC, Wu GH, Zhou LL, et al. Two unilateral puncturation comparative analyses of multiple-level fresh osteoporotic vertebral body compression fractures treated with percutaneous vertebroplasty guided by C-arm fluoroscopy or in senile patients. Eur Rev Med Pharmacol Sci 2017;21:1456–61. [PubMed] [Google Scholar]
- [13].Yan L, He B, Guo H, et al. The prospective self-controlled study of unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty. Osteoporos Int 2016;27:1849–55. [DOI] [PubMed] [Google Scholar]
- [14].Chen BL, Li YQ, Xie DH, et al. Comparison of unipedicular and bipedicular kyphoplasty on the stiffness and biomechanical balance of compression fractured vertebrae. Eur Spine J 2011;20:1272–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ryu KS, Huh HY, Jun SC, et al. Single-balloon kyphoplasty in osteoporotic vertebral compression fractures: far-lateral extrapedicular approach. J Korean Neurosurg Soc 2009;45:122–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zhai WF, Jia YW, Wang JJ, et al. The clinical application and efficacy of percutaneous kyphoplasty via unilateral pedicularapproach guided by CT image measurement. Int J Clin Exp Med 2015;8:20861–8. [PMC free article] [PubMed] [Google Scholar]
- [17].Chen Q, Liu L, Liang G. Distribution characteristics of bone cement used for unilateral puncture percutaneous vertebroplasty in multiple planes. Orthopade 2018;47:585–9. [DOI] [PubMed] [Google Scholar]
- [18].Hui TC, Tan GZ, Tan AK, et al. The use of cone beam CT in achieving unipedicular spinal augmentation. Br J Radiol 2016;89:20160030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tan GQ, Li F, Zhou DS, et al. Unilateral versus bilateral percutaneous balloon kyphoplasty for osteoporotic vertebral compression fractures-A systematic review of overlapping meta-analyses. Medicine (Baltimore) 2018;97:e11968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Li H, Yang L, Tang J, et al. An MRI-based feasibility study of unilateral percutaneous vertebroplasty. BMC Musculoskelet Disord 2015;16:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ringer AJ, Bhamidipaty SV. Percutaneous access to the vertebral bodies: a video and fluoroscopic overview of access techniques for trans-, extra-, and infrapedicular approaches. World Neurosurg 2013;80:428–35. [DOI] [PubMed] [Google Scholar]
- [22].Robinson Y, Heyde CE, Försth P, et al. Kyphoplasty in osteoporotic vertebral compression fractures--guidelines and technicalconsiderations. J Orthop Surg Res 2011;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Heo DH, Cho YJ. Segmental artery injury following percutaneous vertebroplasty using extrapedicular approach. J Korean Neurosurg Soc 2011;49:131–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hoshide R, Feldman E, Taylor W. Cadaveric Analysis of the Kambin's Triangle. Cureus 2016;8:e475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Molloy S, Mathis JM, Belkoff SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine (Phila Pa 1976) 2003;28:1549–54. [PubMed] [Google Scholar]
- [26].Belkoff SM, Mathis JM, Jasper LE, et al. The biomechanics of vertebroplasty: the effect of cement volume on mechanical behavior. Spine (Phila Pa 1976) 2001;26:1537–41. [DOI] [PubMed] [Google Scholar]
- [27].Sun HB, Jing XS, Liu YZ, et al. The Optimal volume fraction in percutaneous vertebroplasty evaluated by pain relief, cement dispersion, and cement leakage: a prospective cohort study of 130 patients with painful osteoporotic vertebral compression fracture in the thoracolumbar vertebra. World Neurosurg 2018;114:e677–88. [DOI] [PubMed] [Google Scholar]


