Abstract
To study the safety and efficacy of fluoroscopic removal of self-expandable metallic stent for airway stenosis.
We conducted a retrospective analysis of 67 consecutive patients, 39 male and 28 female, who underwent fluoroscopic stent removal from March 2011 to April 2017. The patients ranged in age from 12 to 85 years. Seventy-six airway stents were implanted, 70 covered stents and 6 bare stents, including 9 stents for second stent implantation after removal. All patients underwent chest computed tomography scans with/without bronchoscopy before stent removal. The indication of stent removal and postinterventional complications were analyzed retrospectively.
Seventy-four of 76 airway stents were successfully removed, only 2 stent showed retained struts after removal, for a technical success rate of 97.4%. Two patients died of complications (1 hemorrhage and 1 respiratory failure), resulting in a clinical success rate of 94.7%. Five stents showed strut fracture and the remaining 71 stents were removed in 1 piece. Indications for stent removal include planned removal (n = 40), excessive granulation tissue (n = 15), intolerance of stenting (n = 6), inadequate expansion and deformation (n = 5), stent migration (n = 5), replacement of bare stent (n = 4), and strut fracture (n = 1). There were 17 complications of stent removal: death from massive bleeding (n = 1), restenosis requires stenting (n = 9), strut fracture or residue (n = 5), dyspnea requires mechanical ventilation (n = 2). The survival rates were 83.8%, 82.1%, and 82.1% for 0.5, 3, and 6 years.
Fluoroscopic removal of airway stent is technically feasible and effective. Stents are recommended for removal within 3 months for treating airway stenosis.
Keywords: airway stenosis, airway stent, complications, fluoroscopy, stent removal
1. Introduction
Airway stenosis is a potentially life-threatening condition, which may be caused by tumor invasion or benign diseases, such as, endotracheal intubation injury, endobronchial tuberculosis, and thoracic trauma. Most of these patients may be too sick to undergo definitive open surgery or may not be willing to undergo surgery under general anesthesia.[1] Conservative treatment simply assists in alleviation of airway symptom, but show no curative effect on airway stenosis. Since first adoption of metal stents to treat bronchial obstruction, the airway stent has become an effective method for airway stenosis[2–5] and has been widely used in clinical practice. Complications of airway stent include stent restenosis caused by tumor or granulation tissue, stent fracture, and stent migration.[6] Stent removal may become necessary if these complications result in airway obstruction or injury. Endoscopic removal of airway stent has been reported in small series.[7,8] However, few studies have described the techniques and complications of fluoroscopic removal of airway stent. The safety and efficacy of fluoroscopic stent removal and the optimal safe duration of stent implantation have not been determined. We report clinical results in fluoroscopic removal of airway stents for airway stenosis over a 6-year period.
2. Materials and methods
2.1. Patients
This study was approved by the Ethics Committee and Medical Records Management Section of our university. The written informed consents were obtained from all patients or their parents if the patients are less than 18 years old. We conducted a retrospective analysis of 67 patients who underwent fluoroscopic stent removal due to patient's refusal of surgery and general anesthesia from March 2011 to April 2017. All the patients were enrolled after chest computed tomography (CT) examination. The inclusion criteria included all patients with benign airway stenosis, and dyspnea had been significantly alleviated and needed planned removal. Following doctor's advice, they admitted to hospital for stents removal to avoid long-term complications, with no obvious symptom or sign (planned removal). Patients show complications after stenting such as intolerance of stenting, stent migration, excessive tissue hyperplasia, inadequate expansion and deformation, and strut fracture. New airway stents are needed to replace the original stents, such as bare stents placed under emergency situation will be removed and the covered airway stents will be replaced when the patient's condition is stable. The exclusion criteria included patients with advanced malignant tumors with a survival time of less than 3 months and no obvious stent complications; patients with severe visceral dysfunction who unable to withstand the stent removal procedure; patients refused to remove the stent (Fig.1).
Figure 1.
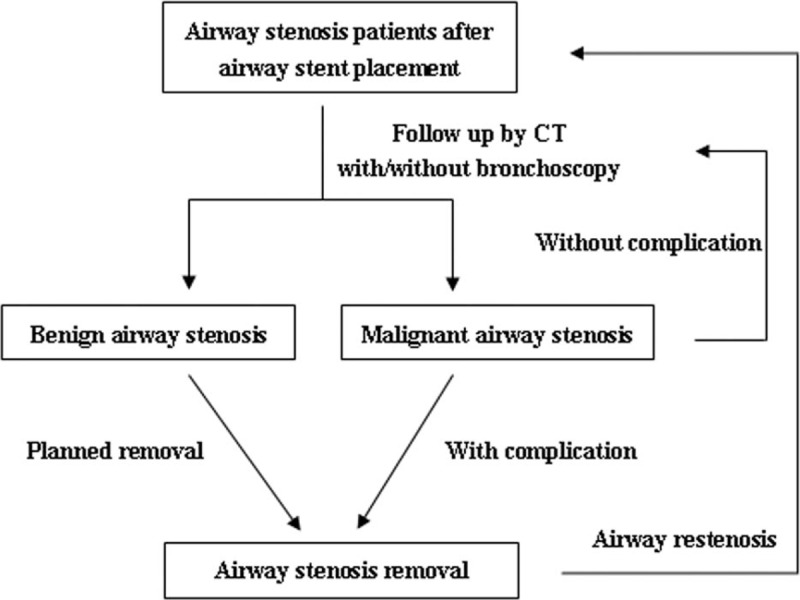
Schematic diagram of this study.
2.2. Technical details of fluoroscopic removal
All patients underwent chest CT scans with/without bronchoscopy before stent removal (Fig. 2). Under conscious situation, balloon dilatation of airway stent was performed immediately after stenting due to insufficient expansion (n = 11) and before stent implantation or removal due to severe airway stenosis (n = 24). All self-expandable metal airway stents were designed and manufactured by Micro-Tech Co Ltd (Nanjing, China). Airway metal stent was woven with a temperature-memory nickel–titanium alloy wire, which was visible on fluoroscopy. In an emergency, we placed 6 bare stents to immediately relieve severe dyspnea and avoid asphyxia. Seventy covered stents were used in nonemergency situations. All airway stents were removed transorally under fluoroscopy and local anesthesia via lidocaine. Bronchoscopy was not performed during the removal, which might use after the operation if removal failed. The patient took the supine position and the head was faced toward the operator to prevent asphyxiation. A 5F vertebral artery catheter (Cook Corporation, Bloomington, IN) was advanced along a 0.035 inch stiff hydrophilic guide wire (Cook Corporation), then 2% lidocaine was injected through vertebral artery catheter for topical anesthesia. A 10-14F long sheath was inserted via the stiff hydrophilic guide wire, and an extractive hook was then inserted. The tip of hook was placed next to the airway stent to withdraw the airway stent (Fig. 3). The sputum aspiration tube was advanced for maintaining airway patency and sputum drainage.
Figure 2.
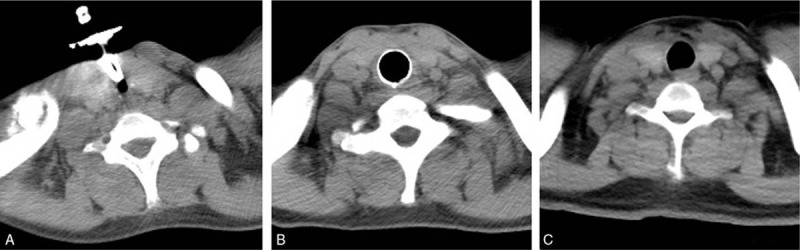
Chest CT scans for airway. A severe stenosis was induced by tracheotomy and tracheal T tube implantation (A), which was dilated after stenting (B) and stent removal (C). CT = computed tomography.
Figure 3.
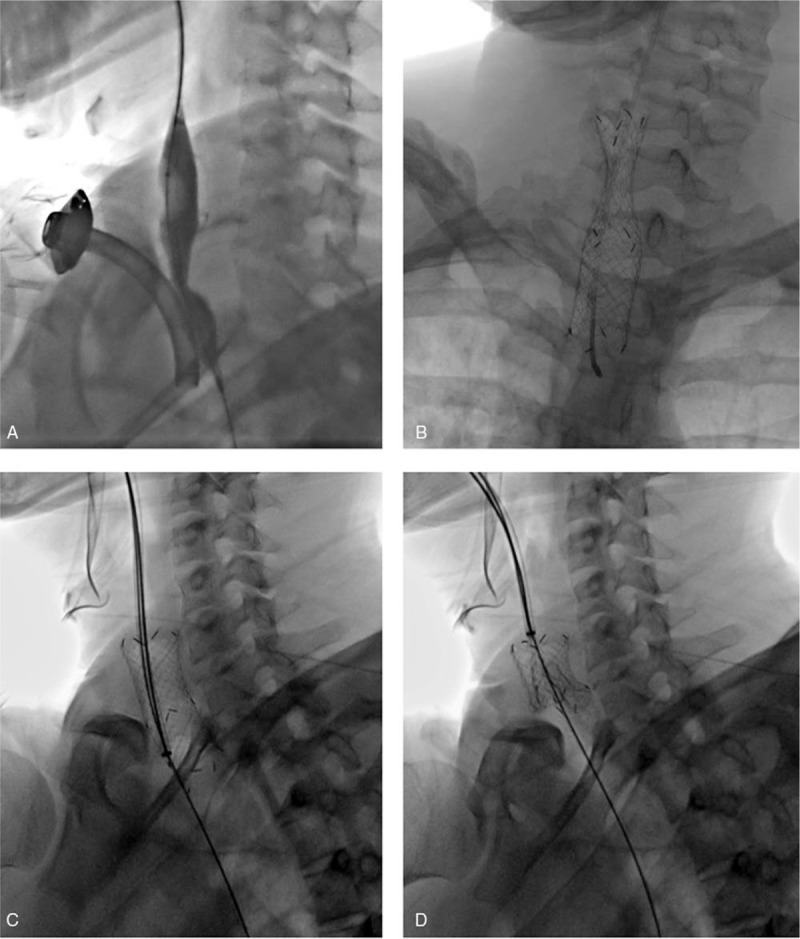
Fluoroscopic treatments for airway stenosis with airway stents. Pre-dilation of severe stenosis caused by tracheotomy with a balloon (A), and then a straight airway stent was implanted (B). A long sheath was inserted via the stiff hydrophilic guide wire, and an extractive hook was then inserted, with the tip of hook was placed next to the airway stent (C). Airway stent was withdrawn successfully by extractive hook (D).
2.3. Complications of stent removal and follow up
All complications were scored and analyzed. Patients were followed up once a month within 3 months after stent placement, and every 2 months thereafter. If symptoms flared as needed, patients were asked to admit to hospital at any time. All patients underwent chest CT scans after stent placement, and bronchoscopy was used for some patients if necessary. Telephone follow up was used for patients did not admit to hospital.
2.4. Statistical analysis
Data were expressed as mean ± standard error and analyzed using Student t test and analysis of variance. Qualitative data were expressed as the percentage, and analyzed by Fisher exact test. Patency rate was compared using the Log-rank (Mantel-Cox) Test (GraphPad Software, Inc San Diego, USA). Statistical significance was considered when P < .05.
3. Results
3.1. The patients’ characteristics
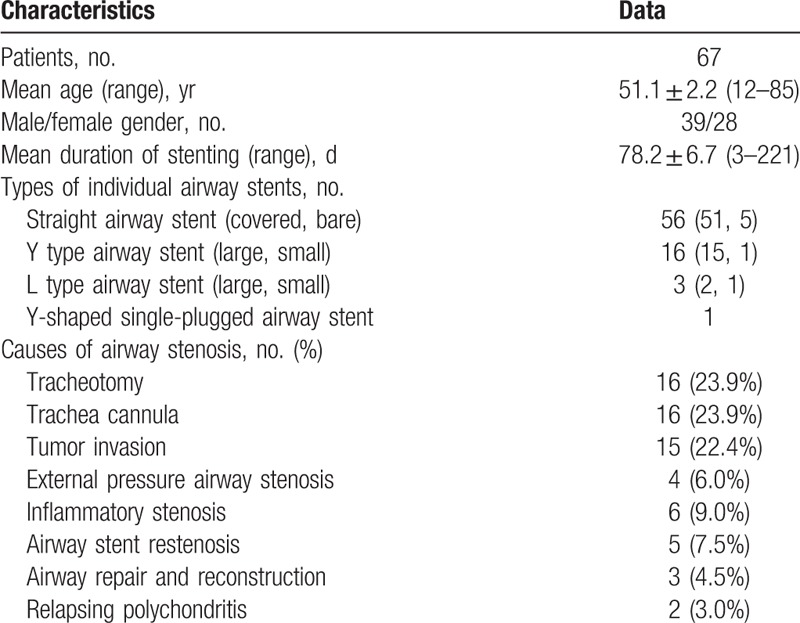
The 67 patients, 39 male and 28 female, ranged in age from 12 to 85 years, with a mean age of 51.1 ± 2.2 years. Seventy-six airway stents were implanted in 67 consecutive patients over a 6-year period, of which, 9 patients underwent second stent implantation after removal. The mean procedure time for stent implantation and removal were 26.8 ± 1.9 minutes and 23.3 ± 2.0 minutes, respectively. The mean fluoroscopic time for stent implantation and removal were 18.6 ± 1.1 minutes and 17.3 ± 1.2 minutes, respectively. Types of individual airway stents were shown in Table 1. Causes of airway stenosis included tracheotomy in 16 cases, trachea cannula in 16 cases, tumor invasion in 15 cases, external pressure airway stenosis in 4 cases, inflammatory stenosis in 6 cases (4 tuberculosis and 2 pulmonary infection), airway stent restenosis in 5 cases, airway repair and reconstruction in 3 cases (2 trachea trauma and 1 airway hemangioma), and relapsing polychondritis in 2 cases.
Table 1.
The patients’ characteristics.
Sixteen Y-shaped airway stents were placed in the trachea and bilateral main bronchi. A total of 55 tubular stents were placed in the middle and upper trachea (n = 47), the middle trachea (n = 4), and the middle and lower trachea (n = 4). Two L-shaped airway stents were placed in the trachea and left main bronchus. Their stents were placed in trachea-right main bronchus, right main bronchus and left main bronchus. Before stent placement, 66 patients had dyspnea in varying degrees, including 16 patients with cough and expectoration, and 2 patients with hemoptysis. Dyspnea classification was 3.6 ± 0.7 before stent placement according to the American Thoracic Association Dyspnea Classification Standard, which decreased significantly to 0.6 ± 1.4 after stent placement and dyspnea symptoms were significantly alleviated.
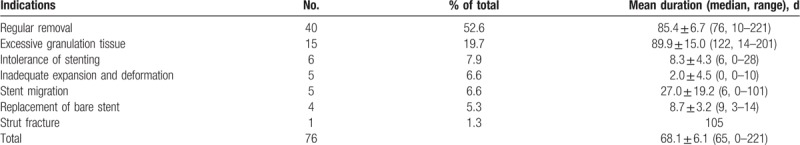
3.2. Indications for stent removal
The indications for stent removal were shown in Table 2, which included planned removal (n = 40), excessive granulation tissue (n = 15), intolerance of stenting (n = 6), inadequate expansion and deformation (n = 5), stent migration (n = 5), replacement of bare stent (n = 4), and strut fracture (n = 1). Six bare stents were emergency implanted for severe airway stenosis, of which, 3 stents were removed and replaced by covered stents, with a mean duration of 8.7 ± 3.2 days, and 1 stent was replaced by tracheal T tube. The remained 2 patients refused to replace the bare stents with covered stents, and the bare stents were removed due to severe stenosis after more than 3 months. Stent migration, intolerance of stenting, and inadequate expansion and deformation were the main indications for early stent removal. Excessive granulation tissue was the most common indication for later stent removal, with a mean duration of 89.9 ± 15.0 days. One case underwent stent removal due to strut fracture 105 days after stenting.
Table 2.
Indications for airway stent removal.
3.3. Complications of stent removal
As shown in Table 3, 74 of 76 airway stents were successfully removed from 67 consecutive patients, 5 stents showed strut fracture, only 2 stent showed retained struts after removal, for a technical success rate of 97.4% (74/76). Before stent removal, 29 patients had dyspnea in varying degrees, including 6 patients with cough and expectoration. Dyspnea classification was 1.4 ± 1.7 before stent removal, which decreased significantly to 0.8 ± 0.9 after stent removal and dyspnea symptoms were significantly alleviated.
Table 3.
Complications of stent removal.
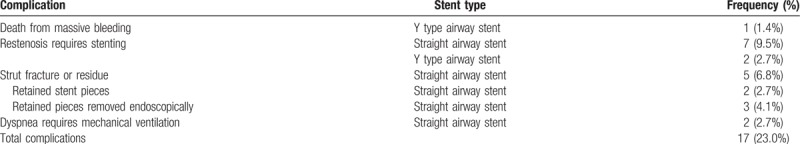
Two patients died of complications (1 hemorrhage and 1 respiratory failure), resulting in a clinical success rate of 94.7% (72/76) and 30-day mortality of 2.6%. The 3 retained stent pieces were successfully removed by endoscope; the remaining 71 stents were removed in 1 piece. There were 17 complications of stent removal: death from massive bleeding (n = 1), restenosis requires stenting (n = 9), strut fracture and retained stent pieces (n = 5), and dyspnea requires mechanical ventilation (n = 2).
The most common complications were restenosis caused by excessive granulation tissue and strut fracture, after a mean duration of 93.3 ± 14.5 days (Fig. 4 and Table 4). A 52-year male patient developed airway stenosis and esophageal airway fistula after resection of esophageal carcinoma, a Y type airway stent was implanted but had to remove immediately due to intolerance of stent. This patient died of spontaneous massive hemoptysis might cause by esophageal airway fistula 3 days after stent removal. In most of patients, mild hemoptysis was found, without need for medication. During stent removal, 4 patients showed dyspnea with decreased pulse oxygen, and 2 cases needed mechanical ventilation. The symptoms were relieved in 1 patient and then endotracheal tube was removed within 4 hours. A 43-year female patient with relapsing polychondritis showed bad respiratory condition before stent placement, the opening of the left upper lobe bronchus is partially blocked by the left branch of the second Y type stent. She died of respiratory failure 2 days after stent implant.
Figure 4.
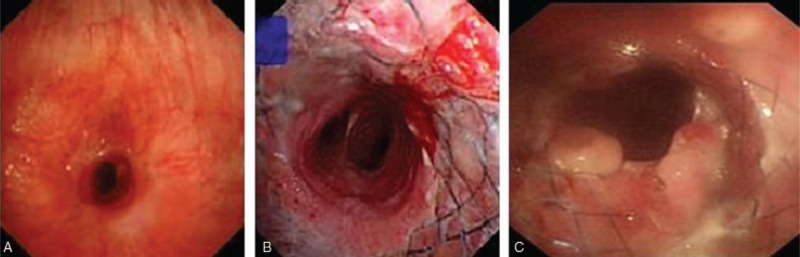
The flexible bronchoscopy examination before and after stenting. (A) A severe stenosis was shown, which was too narrow to pass through bronchoscope. (B) Airway stent was patency without obvious complication 15 d after stenting. (C) Excessive granulation tissue shown 106 d after stenting, stent removal performed thereafter.
Table 4.
Second stenting after removal of airway stent.
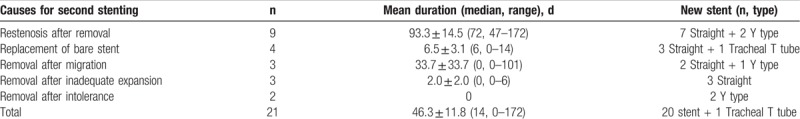
3.4. Second stenting after removal and follow up
As shown in Table 4, 20 airway stents, 15 straight airway stents, and 5 Y type airway stents, were implanted again after removal for replacement of bare stents (n = 4), or due to restenosis (n = 9), migration (n = 3), inadequate expansion (n = 3), and intolerance (n = 2). Chest CT and bronchoscopy were performed during post-removal admission to prevent long-term compilation. During follow up, 1 patient died of respiratory failure 1 month after removal, and 2 patients died of tumor progression 42 days and 6 months after removal. Two patients underwent tracheotomy and tracheal T tube implantation 1 to 2 years after stent removal. Survival rate follow up. The survival rates were 83.8%, 82.1%, and 82.1% for 0.5, 3, and 6 years (Fig. 5).
Figure 5.
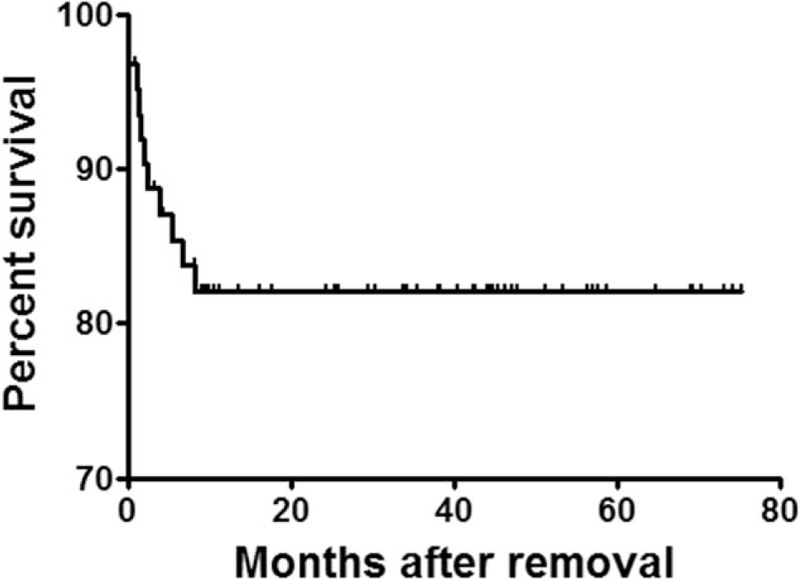
Survival rate follow up. The survival rates were 83.8%, 82.1%, and 82.1% for 0.5, 3, and 6 yr.
4. Discussion
The airway stent has become an effective method for the treatment of airway stenosis,[2–5] and has been widely used in clinical practice. However, long term implantation of airway stents may cause several complications, such as, strut fracture, stent migration, and excessive granulation hyperplasia. Stent removal is necessary to avoid these complications.[9] At present, endoscopic removal of airway stent has been reported in small series,[7,8] which often performed under general anesthesia[10–14] or local anesthesia in a few reports.[15,16] Fluoroscopic removal of airway stent is rarely reported for airway stenosis. In this study, 74 of 76 airway stents were successfully removed, with a technical success rate of 97.4%. Compared with stent removal with rigid alligator forceps, in which 73% of stents were removed piecemeal.[10] In our study, only 2 stent showed retained struts after removal and 3 retained stent pieces were successfully removed by endoscope, the remaining 71 stents were removed in 1 piece. Our data indicate that fluoroscopic removal of airway stents is effective and feasible for airway stenosis.
The details provided in previous reports varied widely and almost with no detailed discussions in complications. Our study is the few study to report techniques and complications of fluoroscopic removal of airway stents. Although the process of fluoroscopic removal is quite short in our study (less than 30 minutes), there are also risks during removal. These serious complications include bleeding, tissue laceration, airway obstruction, and even death.[10,17,18] In our study, there were 2 deaths, 1 patient of airway stenosis and esophageal airway fistula died of massive hemoptysis 3 days after stent removal; the other patient of relapsing polychondritis died of respiratory failure 2 days after stent implant. The 2 patients might die of etiology rather than stenting procedure. In addition, the total incidence of complications was 23.0% (17/74), similar as that previously reported by using of bronchoscope.[10,11,16,17]
Excessive granulation tissue may cause difficulty or failure of removal.[15] As indwelling time increase, the incidence of granulation tissue hyperplasia and stent fracture increase.[19–21] The endothelialization appear 2 months after stenting,[18] stents are difficult to be removed after 10 months.[10] So, 6 months[22] or earlier[23] is regarded as the optimal indwelling time for removal. However, the most suitable indwelling time for airway stenosis is still inconclusive. In our study, stents are recommended for removal within 3 months to avoid excessive granulation tissue. Silicon stents are more suitable for patients with benign disorders caused airway obstruction, especially young and little patients. Patients received stent placement of metallic stents rather than silicon stent to relieve dyspnea caused by severe airway stenosis due to their refusal of surgery and general anesthesia. In this study, covered stents were used for these patients to avoid excessive tissue growth into stent, and for the convenience of removing the stent. Radiologic placement and removal of metallic stents are suitable for old patients with an age more than 70; patient with severe co-morbidities; or patient's refusal of surgery and general anesthesia.
Securing the airway is a major step and first step and priority in any interventional bronchology procedure. The placement or removal of the stent under general anesthesia appears to be safer than under local anesthesia in patients with airway stenosis. However, according to our clinical experience, patients with severe airway stenosis are at high risk for endotracheal intubation and anesthesia. In our center, emergency endotracheal intubation can be performed under fluoroscopy guidance and local anesthesia for patients with acute dyspnea or asphyxia. Besides, vocal cords are the narrowest part in airway and a stent can injure or even completely block the airway at vocal cords during stent removal procedure. According to our experience, the tip of hook was placed next to the airway stent and captured the stent firmly throughout the whole procedure of removal to avoid the drop of stent and life threatening complication of airway block. The stent should be pulling out slowly and carefully to minimize the injury to vocal cords and tracheal.
There are several limitations of the study. The pathological changes and optimal removal duration of stent after placement need confirm in further animal study. In addition, surgical placement and removal of the metallic stents under general anesthesia with rigid bronchoscope remain gold standard and airway stents removal often requires a variety of technologies,[24] we removed stent solely under radiology guidance.
5. Conclusions
Fluoroscopic removal of airway stent is technically feasible and effective. Stents are recommended for removal within 3 months for treating airway stenosis to avoid complications such as excessive granulation tissue formation in stent.
Author contributions
Conceptualization: Yonghua Bi, Gang Wu, Xinwei Han, Jianzhuang Ren.
Data curation: Yonghua Bi, Zepeng Yu.
Formal analysis: Yonghua Bi, Gang Wu, Zepeng Yu.
Investigation: Yonghua Bi, Gang Wu, Zepeng Yu.
Methodology: Gang Wu.
Project administration: Gang Wu, Xinwei Han, Jianzhuang Ren.
Software: Zepeng Yu.
Supervision: Gang Wu, Xinwei Han, Jianzhuang Ren.
Validation: Xinwei Han.
Writing – original draft: Yonghua Bi, Gang Wu, Zepeng Yu.
Writing – review and editing: Xinwei Han, Jianzhuang Ren.
Footnotes
Abbreviation: CT = computed tomography.
How to cite this article: Bi Y, Wu G, Yu Z, Han X, Ren J. Fluoroscopic removal of self-expandable metallic airway stent in patients with airway stenosis. Medicine. 2020;99:1(e18627).
XH and JR contributed equally to this work and share co-corresponding authors.
The authors have no conflicts of interest to disclose.
References
- [1].Fernando HC, Sherwood JT, Krimsky W. Endoscopic therapies and stents for benign airway disorders: where are we, and where are we heading? Ann Thorac Surg 2010;89:S2183–7. [DOI] [PubMed] [Google Scholar]
- [2].Stockton PA, Ledson MJ, Hind CR, et al. Bronchoscopic insertion of Gianturco stents for the palliation of malignant lung disease: 10 year experience. Lung Cancer 2003;42:113–7. [DOI] [PubMed] [Google Scholar]
- [3].Prasad M, Bent JP, Ward RF, et al. Endoscopically placed nitinol stents for pediatric tracheal obstruction. Int J Pediatr Otorhinolaryngol 2002;66:155–60. [DOI] [PubMed] [Google Scholar]
- [4].Han X, Al-Tariq Q, Zhao Y, et al. Customized hinged covered metallic stents for the treatment of benign main bronchial stenosis. Ann Thorac Surg 2017;104:420–5. [DOI] [PubMed] [Google Scholar]
- [5].Ma J, Han X, Wu G, et al. Outcomes of temporary partially covered stent placement for benign tracheobronchial stenosis. Cardiovasc Intervent Radiol 2016;39:1144–51. [DOI] [PubMed] [Google Scholar]
- [6].Freitag L, Ernst A, Unger M, et al. A proposed classification system of central airway stenosis. Eur Respir J 2007;30:7–12. [DOI] [PubMed] [Google Scholar]
- [7].Miyazawa T, Yamakido M, Ikeda S, et al. Implantation of ultraflex nitinol stents in malignant tracheobronchial stenoses. Chest 2000;118:959–65. [DOI] [PubMed] [Google Scholar]
- [8].Gaissert HA, Grillo HC, Wright CD, et al. Complication of benign tracheobronchial strictures by self-expanding metal stents. J Thorac Cardiovasc Surg 2003;126:744–7. [DOI] [PubMed] [Google Scholar]
- [9].Han XW, Wu G, Li YD, et al. Overcoming the delivery limitation: results of an approach to implanting an integrated self-expanding Y-shaped metallic stent in the carina. J Vasc Interv Radiol 2008;19:742–7. [DOI] [PubMed] [Google Scholar]
- [10].Lunn W, Feller-Kopman D, Wahidi M, et al. Endoscopic removal of metallic airway stents. Chest 2005;127:2106–12. [DOI] [PubMed] [Google Scholar]
- [11].Noppen M, Stratakos G, D’Haese J, et al. Removal of covered self-expandable metallic airway stents in benign disorders: indications, technique, and outcomes. Chest 2005;127:482–7. [DOI] [PubMed] [Google Scholar]
- [12].Dooms C, De Keukeleire T, Janssens A, et al. Performance of fully covered self-expanding metallic stents in benign airway strictures. Respiration 2009;77:420–6. [DOI] [PubMed] [Google Scholar]
- [13].Chan AL, Juarez MM, Allen RP, et al. Do airway metallic stents for benign lesions confer too costly a benefit? BMC Pulm Med 2008;8:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Filler RM, Forte V, Chait P. Tracheobronchial stenting for the treatment of airway obstruction. J Pediatr Surg 1998;33:304–11. [DOI] [PubMed] [Google Scholar]
- [15].Chung FT, Chen GY, Chou CL, et al. Remove airway ultraflex stents by flexible bronchoscope. Am J Med Sci 2012;343:267–72. [DOI] [PubMed] [Google Scholar]
- [16].Fruchter O, Raviv Y, Fox BD, et al. Removal of metallic tracheobronchial stents in lung transplantation with flexible bronchoscopy. J Cardiothorac Surg 2010;5:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gottlieb J, Fuehner T, Dierich M, et al. Are metallic stents really safe? A long-term analysis in lung transplant recipients. Eur Respir J 2009;34:1417–22. [DOI] [PubMed] [Google Scholar]
- [18].Murthy SC, Gildea TR, Mehta AC. Removal of self-expandable metallic stents: is it possible? Semin Respir Crit Care Med 2004;25:381–5. [DOI] [PubMed] [Google Scholar]
- [19].Chung FT, Lin SM, Chen HC, et al. Factors leading to tracheobronchial self-expandable metallic stent fracture. J Thorac Cardiovasc Surg 2008;136:1328–35. [DOI] [PubMed] [Google Scholar]
- [20].Chung FT, Lin SM, Chou CL, et al. Factors leading to obstructive granulation tissue formation after ultraflex stenting in benign tracheal narrowing. Thorac Cardiovasc Surg 2010;58:102–7. [DOI] [PubMed] [Google Scholar]
- [21].Chung FT, Chen HC, Chou CL, et al. An outcome analysis of self-expandable metallic stents in central airway obstruction: a cohort study. J Cardiothorac Surg 2011;6:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Madden BP, Park JE, Sheth A. Medium-term follow-up after deployment of ultraflex expandable metallic stents to manage endobronchial pathology. Ann Thorac Surg 2004;78:1898–902. [DOI] [PubMed] [Google Scholar]
- [23].Husain SA, Finch D, Ahmed M, et al. Long-term follow-up of ultraflex metallic stents in benign and malignant central airway obstruction. Ann Thorac Surg 2007;83:1251–6. [DOI] [PubMed] [Google Scholar]
- [24].Chawla RK, Madan A, Singh I, et al. Removal of self expandable metallic airway stent: a rare case report. Lung India 2013;30:64–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


