Abstract
Background
There is limited empirical integration between peer clustering theory and the Gateway framework. The goal of the present study was to test the hypothesis that friendship associations partly predict gateway escalations in the use of drugs from adolescence to adulthood.
Method
This longitudinal study analyzed 3 waves of data from a community sample of 711 male and female participants without a history of illicit drug use reporting drug use at age 17, 22, and 27. Substance use assessments including tobacco, alcohol, cannabis, onset and abuse/dependence tendency of illicit drugs other than cannabis (i.e., cocaine, methamphetamine, and opiates), and friends’ reported use of illicit drugs. Structural equation modeling was used to test the hypothesized model.
Results
Participants’ cannabis use level at age 17 was positively associated with perceived friends’ drug use at age 22, which in turn predicted participants’ onset of illicit drug use between ages 22 and 27. Moreover, progression of tobacco use throughout age 17 to 22 was associated with an increased onset of illicit drug use between ages 22 and 27. Apart for an effect of cannabis use at age 22 on abuse and dependence tendency to various drugs at age 28, results were similar.
Conclusions
During this period of development, the availability and selection of drug-using friends contributes to the progression to potentially more rewarding and damaging illicit drugs. These findings suggest the need to attend to the peer ecology in prevention and support the common practice of using abstaining peers in treatment for drug dependence.
Keywords: Gateway Model, Peer Clustering, Cannabis, Illicit Drugs
1. Introduction
Drug use and dependence continues to be one of the leading causes of distress and mortality in the United States (Brady and Li, 2014, Degenhardt et al., 2005). Next to legal drugs such as alcohol, tobacco and (to a certain extent) cannabis; cocaine, methamphetamine, and opiates are among the most pernicious illegal drugs because of the addictive quality, personal disruption, and mortality potential (Degenhardt and Hall, 2012, Van Amsterdam et al., 2015). Recent results of the national school-based Youth Risk Behavior Survey showed that 5.5% of students reported having used cocaine derivatives (e.g., powder, crack, freebase) one or more times during their life, 3.2% of students reported use of methamphetamines at least once, and 2.2% of students reported using heroin (Kann et al., 2014). Because of the potential for addiction and adverse effects from these drugs, a body of research attempts to delineate the developmental pattern describing the movement from legal drugs (e.g., including alcohol, tobacco, and now cannabis) to illegal, and potentially more addictive and disruptive drugs (including cocaine, methamphetamine, and opiates) in late adolescence and adulthood.
The gateway hypothesis (GH) is the most influential framework for research on developmental progressions in drug use (Kandel, 1975, Kandel and Kandel, 2015). The GH posits that addiction is learned in the brain within the experiential context of sampling drug effects. From this perspective, adolescent use of alcohol, cigarettes, and cannabis may progress to more severe levels of use of these drugs, yet also to the use of other sometimes more rewarding and damaging drugs (Kandel and Kandel, 2014, 2015). Accordingly, one way of preventing serious drug use and addiction is to restrict access and motivation for adolescent use of alcohol, cigarettes and cannabis. With respect to cigarette and alcohol use, empirical support for the GH is robust (Kandel and Kandel, 2014, Woodcock et al., 2015). For instance, among 18- to 34-year-olds, 96.9% of individuals first started either smoking or drinking before they started using cocaine. Only 0.8% initiated their drug use with cocaine (SAMSHA, 2012).
Animal models of addiction provide strong support for biological mechanisms underlying the GH. For instance, Kandel and Kandel (2014) suggest that exposure to nicotine in mice significantly elevated (by 98%) the locomotor response to cocaine, whereas cocaine did not change the baseline activity of nicotine. In addition, studies showed that repeated exposure to tetrahydrocannabinol (one of the main psychoactive ingredients of cannabis) enhances the sensitivity of the reward system to other drugs (Schenk, 2002, DiNieri and Hurd, 2012), referred to as cross-sensitization. These findings suggest that, if left unfettered, youth will progress naturally from alcohol, cigarettes, and cannabis to other drugs in ecologies where both legal and illegal drugs are readily available.
Within the traditional GH framework, cannabis takes a central role in the progression to use of other drugs, partly because of its controversial status with respect to legalization. However, what remains unclear is its unique status as a gateway drug relative to alcohol and tobacco use. First, the majority of people who use cannabis actually do not go on to use other more addictive drugs (Hall and Lynskey, 2005). Second, in some cases, cannabis use precedes the use of alcohol and tobacco (Golub and Johnson, 2002). For example, in a nationwide survey, 35% of individuals reported that they either started cannabis first or started cannabis and drinking/smoking at the same time (SAMSHA, 2012). Third, posing cannabis as the core link between the legal and illicit drug use may be oversimplifying the human dynamics of drug use progressions (Kleinig, 2014). It is argued that experimentation and progression of illicit drug use among humans is more complex than in animal models, which neglect the social ecology.
For example, the strongest correlate of drug use initiation is exposure to substance-using peers (Dishion and Loeber, 1985, Kandel, 1973). Attitudes towards drug use are a salient dimension for youth clustering into friendship groups (Kandel, 1978, Otten, Wanner, Vitaro, & Engels, 2008). Moreover, peer clustering is a robust predictor of progressions from early drug experimentation to escalating use and dependence by early adulthood (Van Ryzin and Dishion, 2014). If the social norms of illicit substance use suggest acceptability and harmlessness, then experimentation will likely ensue (Hawkin et al., 2002). As friendships evolve through adolescence, the dynamics embedded in selection and influence increase accessibility, opportunities, and an ecology more favorable to use and abuse of illicit drugs (Dishion and Owen, 2002).
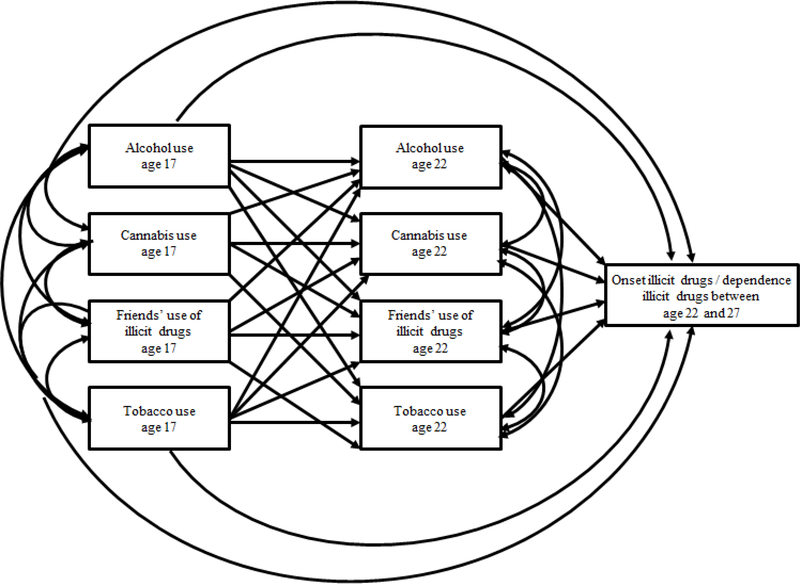
However, to date there is limited empirical integration between peer clustering theory and the GH framework (Vanyukov et al., 2012). Hence, the main goal of the present study is to examine peer influence in the context of the GH framework: (1) replicating the findings of the gateway hypothesis by examining whether cannabis use mediates the link between alcohol and tobacco use and illicit drug use onset and abuse/dependence tendency; and (2) extending the GH by investigating whether affiliation with friends who use illicit drugs can increase the likelihood of illicit drug use onset and abuse/dependence tendency (Figure 1). We expect that, in addition to the well-established mediating effect of cannabis use, affiliation of drug-using peers will emerge as another gateway to other illicit drug use.
Figure 1:
Conceptual model for onset and dependence of illicit drugs between age 22 and 27
2. Material and methods
2.1. Participants
The initial sample consisted of 998 adolescents and their families from a large randomized control trial of the Family Check-Up (FCU) intervention (Dishion and Stormshack, 2007). Participants were recruited from the sixth grade (age 11) of three public middle schools in the Pacific Northwest of the United States. Parents were approached for participation, 90% of them consented to participate. The Institutional Review Board at the University of Oregon approved the study procedures. Participants included 47.3% females and were ethnically diverse (42.4% Caucasians, 29.2% African Americans, 6.8% Hispanics, 5.2% Asian Americans, and 16.4% other). Gross annual household income ranged from $5,000 to more than $90,000, with a median household income between $30,000 and $40,000. The longitudinal retention was on average 80% of those participants assessed at baseline through age 27.
Among the 998 participants, 79 participants with missing data on all study variables, 150 participants who reported use of illicit drugs other than cannabis at age 22, and 58 participants who had missing data on those drugs at age 22 were excluded. The final sample for analysis included 711 participants. Compared to participants who did not report any use of illicit drugs other than cannabis at age 22, those who did report having used drugs at age 22 came from higher income families (t = 4.596, p < .001), reported higher levels of cannabis use at age 17 (t = 9.641, p < .001), higher levels of tobacco use (t = 7.208, p < .001), and higher levels of alcohol use (t = 9.199, p < .001). Moreover, they were more likely to have friends who reported lifetime use of illicit drugs at age 17 (χ2(1) = 20.041, p < .001) and age 22 (χ2(1) = 172.442, p < .001).
2.2. Procedure
Participants were assessed by a questionnaire administered primarily through the schools at age 17, and then by mail in adulthood. All respondents were assured of the confidentiality of their responses. Participants were adequately compensated for their participation.
At age 11, participants were randomly assigned at the individual level to control (middle school as usual) or to the family-centered intervention. Within the intervention, at-risk families were offered a Family Check-Up (FCU). Dishion and Kavanagh detail the description of the FCU intervention (Dishion and Kavanagh, 2003). The focus of this study is not to examine the effect of FCU intervention on this proposed developmental substance progression model. Recent research suggests that random assignment to the FCU at age 11 was linked to modest reductions in cannabis use by age 24 using an intent-to-treat analysis, and to moderate to large effects on cannabis, tobacco, and alcohol use when intervention engagement was a moderator (Véronneau et al., 2016). Because of the modest effects on young adult cannabis use, the intervention group assignment was included as a covariate in the model.
2.3. Measures
Cannabis Use
Participants at age 17 and 22 reported on their cannabis use in the past three months by using an 8-point Likert scale (0 = “Never”; 1 = “Once or twice”; 2 = “Once a month”; 3 = “Once every 2–3 weeks”; 4 = “Once a week”; 5 = “2–3 times a week”; 6 = “Once a day” 7 = “2–3 times or more a day”) (Piehler et al., 2012).
Tobacco Use
Participants at age 17 and 22 reported on their tobacco use in the past three months by using the same 8-point Likert scale as used for cannabis use (Piehler et al., 2012).
Alcohol Use
Participants at age 17 and 22 reported on their alcohol use over the previous three months separately for these three questions: “How often did you drink beer in the past three months?” “How often did you drink wine/wine coolers in the past three months?” and, “How often did you drink hard liquor in the past three months?” (Piehler et al., 2012). We created a composite of these alcohol use measures by taking the average.
Perception of Friend’s use of illicit drugs
At age 22, participants reported whether a friend had used illicit drugs other than cannabis (i.e., speed/amphetamine, heroin/opioids, or cocaine/crack) over the last three months (no/yes). Perception of friends’ lifetime use of illicit drugs was also measured at age 17 as a covariate (no/yes).
Own use of Illicit Drugs
At age 22 and 27, participants reported on their lifetime use of illicit drugs (i.e., speed/amphetamine, heroin/opioids, and cocaine/crack). As discussed, to predict the onset of illicit drug use other than cannabis between ages 22 to 27, we excluded participants who reported any use of these drugs at age 22.
Drug abuse and dependence tendency was measured by four dichotomous (yes/no) items that participants answered for each of the drugs (i.e., speed/amphetamine, heroin/opioids, and cocaine/crack): (1) “Have you ever tried to stop using_______ (drug name) and found you could not?” (2) “Have you found that you can’t get as high on_______ (drug name) as you used to?” (3) “Have you ever gone to school or work when you were high on_______ (drug name)?” and (4) “Have you ever had any problems related to school or work, such as not doing assignments or forgetting things because of_______ (drug name)?” We first calculated the means of these items for each of the illicit drugs. Those individuals who were one standard deviation above the mean were classified as those who have illicit drug abuse and dependence tendency.
2.4. Strategy for Analyses
First, we computed descriptive statistics of all study variables, and we examined the changes in tobacco, alcohol, and cannabis use from age 17 to 22 using paired-samples t-tests. Second, we examined bivariate correlations between the study variables. Third, employing structural equation modeling the hypothesized model was tested. Gender, income, and intervention condition were included as covariates in the model. As the tobacco, alcohol, and cannabis use variables at age 22 were ordinal categorical and the outcome variable was binary, we used the WLSMV estimator in Mplus Version 7 (Muthén and Muthén, 1998–2015). Finally, mediated effects were tested by using the joint significant test. If the effect of the independent variable on the mediator (i.e., alpha path) and the effect of the mediator on the dependent variable (i.e., beta path) are jointly significant at an alpha level of 0.05, then a statistically significant indirect effect is presumed. The joint significant test provides excellent balance of Type I error and statistical power (MacKinnon et al., 2001). Missing data was handled by full information maximum likelihood (FIML) under missing at random assumption.
3. Results
Table 1 shows descriptive statistics of the main study variables. The frequency of cannabis, tobacco, and alcohol use increased significantly from age 17 to 22 (resp. tcannabis = 6.544, p < 0.001; ttobacco = 10.011, p < 0.001; talcohol = 25.584, p < 0.001). Perception of friends’ use of illicit drugs also increased (tfriends’ use of illicit drugs = 2,787, p < 0.01). At age 27, 15.5% of participants had used illicit drugs between age 22 and 27 and 9.8% showed a tendency for abuse/dependence to either one of the illicit drugs between ages 22 and 27.
Table 1.
Descriptive statistics
| Study variables | Numbers (percentages) | ||
|---|---|---|---|
| Sex | Male | 353 (49.7%) | |
| Intervention group | Intervention | 347 (48,9%) | |
| Control | 363 (51,1%) Age 17 | Age 22 | |
| Cannabis use | Never | 486 (81.8%) | 477 (72,9%) |
| Once or twice | 51 (8,6%) | 47 (7,2%) | |
| Once a month | 6 (1.0%) | 14 (2,1%) | |
| Once every 2–3 weeks | 13 (2,2%) | 17 (2,6%) | |
| Once a week | 5 (0,8%) | 11 (1,7%) | |
| 2–3 times a week | 17 (2,9%) | 24 (3,7%) | |
| Once a day | 8 (1,3%) | 27 (4,1%) | |
| 2–3 times/day or more | 8 (1,3%) | 37 (5,7%) | |
| Tobacco use | Never | 497 (83,5%) | 402 (61,5%) |
| Once or twice | 21 (3,5%) | 47 (7,2%) | |
| Once a month | 1 (0,2%) | 7 (1,1%) | |
| Once every 2–3 weeks | 10 (1,7%) | 19 (2,9%) | |
| Once a week | 6 (1,0%) | 15 (2,3%) | |
| 2–3 times a week | 9 (1,5%) | 22 (3,4%) | |
| Once a day | 5 (0,8%) | 15 (2,3%) | |
| 2–3 times/day or more | 46 (7,7%) | 127 (19,4%) | |
| Alcohol use | Never | 394 (66,7%) | 115 (17,9%)_ |
| Once or twice | 113 (19,1%) | 99 (15,4%) | |
| Once a month | 20 (3,4%) | 49 (7,6%) | |
| Once every 2–3 weeks | 34 (5,8%) | 98 (15,2%) | |
| Once a week | 16 2,7%) | 112 (17,4%) | |
| 2–3 times a week | 14 (2,4%) | 148 (23,0%) | |
| Once a day | 0 (0,0%) | 15 (2,3%) | |
| 2–3 times/day or more | 0 (0,0%) | 7 (1,1%) | |
| Perception of friends’ use of illicit drugs | No | 694 (97,6%) | 674 (94,8) |
| Yes | 17 (2,4%) | 37 (5,2) | |
Note. Due to missings the numbers do not sum up to 711.
Table 2 shows correlations between all study variables. Except for the unrelated link between alcohol use at age 22 and tobacco use at age 17, all substance use variables were correlated in the expected direction. Perceived friends’ use at age 17 was significantly correlated with tobacco, alcohol, and cannabis use at age 17, but not with substance use at age 22. Perceived friends’ use at age 22 was correlated with alcohol and cannabis use at age 17 and 22. Perceived use of friends at age 17 was not correlated with perceived use at age 22. Onset of use and dependence at age 22 was associated with all measures, but not with perceived use of friends at age 17. Higher income was associated with less tobacco use at age 22, with more alcohol use at age 17 and 22, with cannabis use at age 22, with perceived use of friends at age 22, and onset of illicit drugs. Being female was negatively correlated with alcohol use at age 22, and with the tendency to abuse or become dependent on various substances. Random assignment to the FCU was correlated with less cannabis use at age 22, and with more friends’ use at age 22.
Table 2.
Bivariate Pearson’s Correlations of Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Tobacco use age 17 | 1 | |||||||||||
| 2. Tobacco use age 22 | 0.44** | 1 | ||||||||||
| 3. Alcohol use age 17 | 0.26** | 0.19** | 1 | |||||||||
| 4. Alcohol use age 22 | −0.02 | 0.20** | 0.30** | 1 | ||||||||
| 5. Cannabis use age 17 | 0.32** | 0.30** | 0.46** | 0.22** | 1 | |||||||
| 6. Cannabis use age 22 | 0.10* | 0.31** | 0.29** | 0.28** | 0.37** | 1 | ||||||
| 7. Friends’ use age 17 | 0.13* | 0.06 | 0.12** | 0.06 | 0.10* | 0.00 | 1 | |||||
| 8. Friends’ use age 22 | −0.01 | 0.04 | 0.12** | 0.15** | 0.12* | 0.09* | 0.01 | 1 | ||||
| 9. Onset illicit drugs | 0.12** | 0.23** | 0.13** | 0.20** | 0.11* | 0.20* | −0.04 | 0.21* | 1 | |||
| 10. Abuse/dependence tendency | 0.15** | 0.28** | 0.25** | 0.10* | 0.19** | 0.28** | −0.02 | 0.15* | 0.41** | 1 | ||
| 11. Income | −0.07 | −0.17** | 0.13** | 0.28** | −0.06 | 0.10* | −0.03 | 0.17** | 0.10* | −0.03 | 1 | |
| 12. Sex | 0.05 | −0.06 | 0.06 | −0.17** | 0.04 | −0.06 | 0.05 | −0.06 | −0.07 | −0.11* | 0.03 | 1 |
| 13. Treatment condition | −0.02 | −0.03 | 0.00 | 0.03 | 0.01 | −0.08* | 0.01 | −0.03 | −0.03 | 0.02 | 0.00 | 0.02 |
p < 0.05
p < 0.01
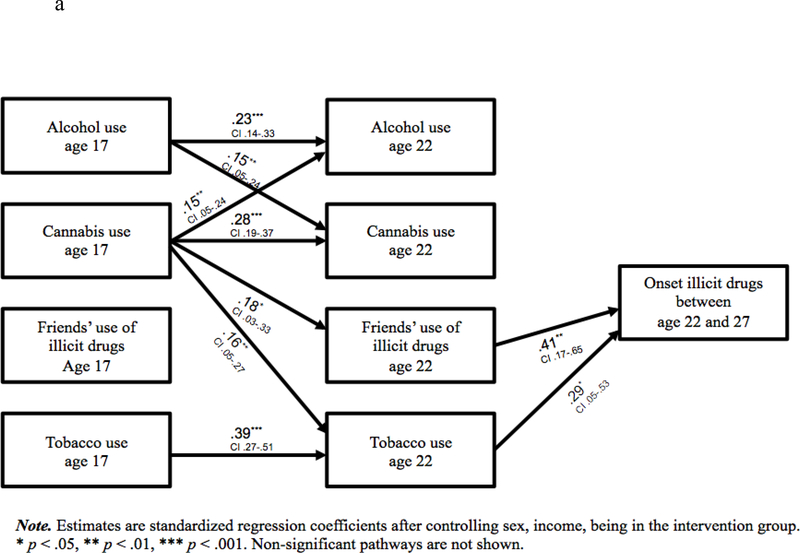
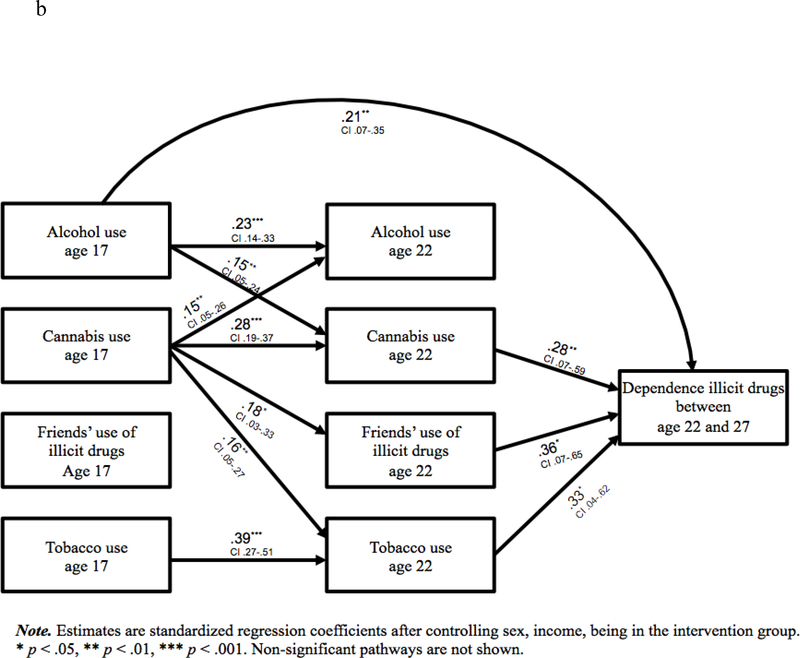
Figure 1a presents findings of the addictive illicit drug use onset model and Figure 1b presents findings of the drug abuse/dependence tendency. Both models were saturated.
In the illicit drug onset model, alcohol and cannabis use at age 17 were positively associated with cannabis use and alcohol use at age 22. Tobacco use at age 22 was predicted by cannabis use at age 17. Perceived use of drug by friends at age 22 was predicted by cannabis use at age 17. Finally, tobacco use and perceived use of drugs by friends at age 22 were associated with higher odds for onset of illicit drug use at age 27. Regarding covariates, females were less likely to use tobacco (β = −0.10, p < 0.05), alcohol (β = −0.21, p < 0.001), or cannabis at age 22 (β = −0.09, p < 0.05). Higher income was associated with alcohol use (β = 0.25, p < 0.001), cannabis use (β = 0.20, p < 0.001), and perceived friend’s drug use at age 22 (β = 0.36, p < 0.001) but with less smoking (β = −0.14, p < 0.01). Being in the intervention condition was predictive of less cannabis use at age 22 (β = 0.09, p < 0.05), and higher perceived use of drugs by friends (β = −0.16, p < 0.05), after controlling for all other study variables.
Overall results of the analysis of the drug abuse/dependence tendency model were consistent with the illicit drug use onset model, with the exception that alcohol use at age 17 directly predicted abuse/dependence of hard drugs (β = 0.21, p < .01). Regarding covariates in this model, income was associated with a lower likelihood for drug abuse/dependence tendency (β = −0.33, p < .05). As a secondary outcome, we tested a stringent model of illicit drug abuse/dependence as an outcome using the World Health Organization Composite International Diagnostic Interview (CIDI 3.0 (Kessler and Ustun, 2004)). Diagnostic criteria of illicit drug abuse and dependence in CIDI are based upon the Diagnostic and Statistical Manual for Mental Disorders (4th ed., text rev,; DSM-IV). In total 57 participants (9.8%) met the criteria for abuse or dependence diagnosis of cocaine, opioids, or stimulant drugs between ages 22 to 27. When we included this outcome in the model we found significant predictions from cannabis use at age 22 (B = 0.28, p < 0.01), and alcohol use at age 17 (B = 0.21, p < 0.01), in addition to friends’ use of drugs.
4. Discussion
To fully understand individual differences in the progression to illicit drug use, we included perception of friends’ drug use within the gateway framework in the context of a longitudinal study of a community sample of multiethnic youth. In line with the traditional gateway hypothesis (Kandel, 1975, Kandel and Kandel, 2015), it was found that alcohol use at age 17 predicted higher levels of cannabis use at age 22, which, in turn, was associated with increased likelihood of illicit drug dependence between ages 22 and 27 (i.e., mediation). Moreover, the links between tobacco use and cannabis use at age 17 and abuse/dependence tendency of illicit drug use were mediated by tobacco use at age 22. Cannabis use at age 17 was predictive of later alcohol, cannabis, tobacco use, and also of friends’ use of illicit drugs at age 22. Not surprisingly, we found that the gateway progression had a social context, in that the reported drug-using patterns of peers contributed uniquely to escalations to illicit drugs. Cannabis use at age 17, and both onset and abuse/dependence tendency of illicit drug use between ages 22 and 27 were significantly mediated by affiliation with drug-using peers at age 22.
Consistent with the GH, cannabis appears to serve an important role, particularly in abuse/dependence of other illicit drugs. Neurobiologically, activation of cannabinoid 1 receptors (CB1) can induce drug-seeking behaviors as it releases dopamine, the primary neurotransmitter in the reward system (De Vries and Schoffelmeer, 2005, Wiskerke et al., 2008). Prolonged cannabis use can potentially sensitize these receptors, causing individuals who repeatedly use cannabis to engage in more novelty driven and reward-seeking impulsive behaviors such as experimenting with more addictive drugs. In addition to its indirect effect on illicit drugs, early cannabis use also seems to affect later use of alcohol, tobacco and cannabis. This is remarkable, as the traditional GH has a progressive nature in a way that most studies only focus on how cannabis use can affect illicit drug use. This study shows that the effect of cannabis use is not limited to illicit drugs.
It is quite noteworthy that more frequent cannabis use significantly predicted reported drug-use by peers which in turn, was associated with increased addictive drug-use onset and abuse/dependence tendency. This social mechanism was observed in previous research, showing that cannabis use at aged 15 to 16 predicted selection of cannabis-using friends at ages 17 to 18 (Dishion and Owen, 2002). The finding of this new gateway process is supported by the argument made previously that cannabis users have more opportunities to experiment with other illicit drugs because both cannabis and other drugs are often available in a peer culture with more tolerance to drug use in general (Hall and Lynskey, 2005). It is possible that affiliating with drug-using friends could facilitate this drug experimentation. In this respect, cannabis use may be liable for escalating to more serious drug use through this social mechanism.
Consistent with prior findings (Dishion and Stormshack, 2007), we found that assignment to the FCU at age 11 was linked to modest reductions (p < .05) in cannabis use by age 22, controlling for all study variables. However, these findings differ from previous analyses, as in the present study participants using illicit drugs at age 22 and earlier were excluded from the model. Moreover, the test of the FCU was an encouragement design, so not all families in the intervention group engaged in the intervention. Therefore, more advanced longitudinal models (Jo, 2002) are needed to evaluate the impact of engagement on intervention effects.
4.1. Implications
Movement of cannabis legalization in the U.S. is controversial. Although permitting cannabis use for medical purposes has not led to an increase of use (Hasin et al., 2015), it is possible that legalization of recreational cannabis use could lead to an increase in cannabis use, especially among adolescents (Volkow et al., 2014). For instance, a recent study among high school seniors showed that 10% of those who have never used cannabis reported an intention to use cannabis recreationally if legalized, while lifetime cannabis users reported an intention to use it more frequently (Palamar et al., 2014). This shows that legalizations of cannabis may lead a shift in the development of illicit drug use onset, as perceptions on cannabis use may also shift. Another recent report suggests that prevalence rates significantly increased in Colorado and Washington State after legalization of recreational cannabis use (NSDUH, 2013). The findings of the present study imply that an increase of cannabis use among adolescents may elevate the probability of initiating and depending on other illicit drugs through biological and social mechanisms. A future study that compares the current model between states that legalized recreational use of cannabis and states that did not can provide further insights into the effects of changes in cannabis use.
4.2. Limitations
Several limitations should be taken into account. First, in order to test the GH, we covered a timeframe that would be long enough to allow a moderate number of people to start using drugs. We de-selected people who reported lifetime use of illicit drugs at age 22, thus potentially leaving out an important group that is likely to be a normative reflection of this specific age group. To examine a more accurate process of drug use progression and its underlying mechanisms, a greater number of frequent assessments are desirable as is including individuals who started using drugs at an earlier age. Second, although previous literature suggests that anonymous self-reported drug use is generally reliable and valid (Brener et al., 2003), the present study relied exclusively on self-reported drug use and perception of friends’ drug use, and therefore may not adequately reflect the actual levels of drug use. Third, to assess substance use we used straightforward measures of frequency, rather than more standardized measures (e.g. such as the AUDIT) or measures that tap in to the quantity of use. Fourth and finally, the sample for this study came from the United States. In order to ensure generalizability of the findings, replications are required by using samples from other countries with diverse cultural backgrounds and different legal policies on cannabis use (e.g., The Netherlands).
5. Conclusions
The traditional gateway drug framework is based primarily on a biological perspective that suggests that progression to other illicit drugs is a consequence of neurological alterations of using cannabis. However, this framework largely ignores the social mechanism of progressing to illicit drugs. In addition to the traditional gateway drug hypothesis model, we included a peer clustering hypothesis and found another gateway for progression to illicit drugs, which is through affiliation with peers who use drugs. Findings suggest that prevention of illicit drug use could benefit from an integrative approach focusing on individuals’ cannabis use and peers’ drug use, as each predicts progression to illicit drug use in early adulthood (Onrust et al., 2016).
Figure 2a:
Model for onset illicit drugs between age 22 and 27
Figure 2b:
Model for dependence illicit drugs between age 22 and 27
Highlights.
The proposed model combines the traditional gateway hypothesis with peer clustering.
Results show partial support for the traditional gateway drug hypothesis model.
A second gateway runs through affiliation with peers who use drugs.
Prevention of illicit drug use could benefit from an integrative approach.
Acknowledgements
This work was supported by grants from the National Institute on Drug Abuse (DA 07031, DA 13773, and DA 16110 to T.J.D.) and a 2015 National Institute on Drug Abuse INVEST Research Fellowship to R.O. The authors acknowledge the contribution of the Project Alliance Staff, the study families, and participating schools, all of whom made this study possible.
Statement 1: Role of Funding Sources
Funding for this study was provided by NIDA grants DA 07031, DA 13773, and DA 16110 to TJD and a 2015 National Institute on Drug Abuse INVEST Research Fellowship to RO. NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript.
Footnotes
Statement 3: Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Brady JE, Li G Trends in alcohol and other drugs detected in fatally injured drivers in the United States, 1999–2010. Am J Epidemiol 2014; 179(6): 692–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Billy JO, Grady WR Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health 2003; 33(6): 436–57. [DOI] [PubMed] [Google Scholar]
- De Vries TJ, Schoffelmeer AN (August 2005). “Cannabinoid CB1 receptors control conditioned drug seeking.” Trends in Pharmacological Sciences 26 (8): 420–6. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W Extent of illicit drug use and dependence, and their contribution to the global burden of disease. The Lancet 2012; 379(9810): 55–70. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Whiteford H, Hall W, Vos T Estimating the burden of disease attributable to illicit drug use and mental disorders: what is ‘Global Burden of Disease 2005’ and why does it matter? Addiction 2009; 104(9): 1466–71. [DOI] [PubMed] [Google Scholar]
- DiNieri JA, Hurd YL Rat models of prenatal and adolescent cannabis exposure. Methods Mol Biol 2012; 829: 231–42. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Kavanagh K Intervening in adolescent problem behavior: A family-centered approach. Guilford Press; 2003. [Google Scholar]
- Dishion TJ, Loeber R Adolescent marijuana and alcohol use: The role of parents and peers revisited. Am J Drug Alcohol Abuse 1985; 11(1–2): 11–25. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Owen LD A longitudinal analysis of friendships and substance use: bidirectional influence from adolescence to adulthood. Dev Psychol 2002; 38(4): 480. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Stormshak EA Intervening in children’s lives: An ecological, family-centered approach to mental health care. American Psychological Association; 2007. [Google Scholar]
- Golub A, Johnson BD Substance use progression and hard drug use in inner-city New York. Stages and pathways of drug involvement: Examining the Gateway Hypothesis. 2002; 4: 90–112. [Google Scholar]
- Hall WD, Lynskey M Is cannabis a gateway drug? Testing hypotheses about the relationship between cannabis use and the use of other illicit drugs. Drug Alcohol Rev 2005; 24: 39–48. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM et al. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry 2015; 2(7): 601–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Hill KG, Guo J, Battin-Pearson SR Substance use norms and transitions in substance use: Implications for the gateway hypothesis Stages and pathways for drug involvement: Examining the Gateway Hypothesis. Cambridge University Press; 2002: 42–64. [Google Scholar]
- Jo B Statistical power in randomized intervention studies with noncompliance. Psychol Methods 2002. June;7(2):178. [DOI] [PubMed] [Google Scholar]
- Kandel D Adolescent marijuana use: Role of parents and peers. Science 1973; 181(4104): 1067–70. [DOI] [PubMed] [Google Scholar]
- Homophily Kandel D. B., selection, and socialization in adolescent friendships. Am J Sociol 1978; 427–36. [Google Scholar]
- Kandel D Stages in adolescent involvement in drug use. Science 1975; 190: 912–14. [DOI] [PubMed] [Google Scholar]
- Kandel D, Kandel E The Gateway Hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatrica 2015; 104: 130–37. [DOI] [PubMed] [Google Scholar]
- Kandel ER, Kandel DB A molecular basis for nicotine as a gateway drug. N Engl J Med 2014; 371(10): 932–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, Kinchen S, Shanklin SL, Flint KH, Kawkins J, Harris WA, Lowry R, Olsen EO, McManus T, Chyen D, Whittle L Youth risk behavior surveillance—United States, 2013. MMWR Surveill Summ 2014; 63(4): 1–68. [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004; 13: 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinig J Ready for Retirement: The Gateway Drug Hypothesis. Subst Use Misuse 2015; 50: 971–975. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2001; 7(1): 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- National Survey on Drug Use and Health: Comparison of 2011–2012 and 2012–2013 Model-Based Prevalence Estimates (50 States and the District of Columbia). Accessed August 2, 2016 at http://www.samhsa.gov/data/sites/default/files/NSDUHStateEst2012-2013-p1/ChangeTabs/NSDUHsaeShortTermCHG2013.htm..
- Otten R, Wanner B, Vitaro F, & Engels RC Own and friends’ smoking attitudes and social preference as early predictors of adolescent smoking. Clin Child Adolesc Psychol 2008; 37(4): 808–19. [DOI] [PubMed] [Google Scholar]
- Onrust SA, Otten R, Lammers J, Smit F School-based programmes to reduce and prevent substance use in different age groups: What works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev 2016; 44: 45–59. [DOI] [PubMed] [Google Scholar]
- Palamar JJ, Ompad DC, Petkova E Correlates of intentions to use cannabis among US high school seniors in the case of cannabis legalization. Int J Drug Policy 2014; 25(3): 424–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piehler TF, Véronneau MH, Dishion TJ Substance use progression from adolescence to early adulthood: Effortful control in the context of friendship influence and early-onset use. J Abnorm Child Psychol 2012; 40(7): 1045–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubino T, Prini P, Piscitelli F, Zamberletti E, Trusel M, Melis M, et al. Adolescent exposure to THC in female rats disrupts developmental changes in the prefrontal cortex. Neurobiol Dis 2015; 73: 60–9. [DOI] [PubMed] [Google Scholar]
- Schenk S Sensitization as a process underlying the progression of drug use via gateway drugs In Kandel DB, ed. Stages and pathways of drug involvement: Examining the gateway hypothesis. Cambridge, England: Cambridge University Press; 2002. p. 318–36. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2012 National Survey on Drug Use and Health: summary of national findings. 2013; Rockville, MD. [Google Scholar]
- van Amsterdam J, Nutt D, Phillips L, van den Brink W European rating of drug harms. J. Psychopharmacol 2015; 29(6). [DOI] [PubMed] [Google Scholar]
- Van Ryzin MJ, Dishion TJ Adolescent deviant peer clustering as an amplifying mechanism underlying the progression from early substance use to late adolescent dependence. J Child Psychol Psychiatry 2014; 55(10): 1153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ,… Neale MC. Common liability to addiction and “gateway hypothesis”: Theoretical, empirical and evolutionary perspective. Drug Alcohol Depend 2012; 123: S3–S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Véronneau MH, Dishion TJ, Connell AM, Kavanagh K A randomized, controlled trial of the family check-up model in public secondary schools: Examining links between parent engagement and substance use progressions from early adolescence to adulthood. J Consult Clin Psychol. 2016; 84(6): 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR Adverse Health Effects of Marijuana Use. New Engl J Med 2014; 370(23): 2219–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiskerke J, Pattij T, Schoffelmeer AN, De Vries TJ (June 2008). “The role of CB1 receptors in psychostimulant addiction.” Addiction Biology 13 (2): 225–38. [DOI] [PubMed] [Google Scholar]
- Woodcock EA, Lundahl LH, Stoltman JJ, Greenwald MK Progression to regular heroin use: examination of patterns, predictors, and consequences. Addict Behav 2015; 45: 287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]