Abstract
To identify independent factors associated with prolonged hospital length of stay (LOS) in elderly patients undergoing first-time elective open posterior lumbar fusion surgery.
We retrospectively analyzed the data of 303 elderly patients (age range: 60–86 years) who underwent first-time elective open lumbar posterior fusion surgery at our center from December 2012 to December 2017. Preoperative and perioperative variables were extracted and analyzed for all patients, and multivariate stepwise regression analysis was used to determine the variables affecting the LOS and important predictors of LOS prolongation (P < .001).
The mean age of the patients was 67.0 ± 5.5 years, and the mean LOS was 18.5 ± 11.8 days, ranging from 7 to 103 days. Of the total, 166 patients (54.8%) were men and 83 patients (27.4%) had extended LOS. Multiple linear regression analysis determined that age (P < .001), preoperative waiting time ≥7 days (P < .001), pulmonary comorbidities (P = .010), and diabetes (P = .010) were preoperative factors associated with LOS prolongation. Major complications (P = .002), infectious complications (P = .001), multiple surgeries (P < .001), and surgical bleeding (P = .018) were perioperative factors associated with LOS prolongation. Age (P < .001), preoperative waiting time ≥7 days (P < .001), infectious complications (P < .001), and multiple surgeries (P < .001) were important predictors of LOS prolongation.
Extended LOS after first-time elective open posterior lumbar fusion surgery in elderly patients is associated with factors including age, preoperative waiting time, infectious complications, and multiple surgeries. Surgeons should recognize and note these relevant factors while taking appropriate precautions to optimize the modifiable factors, thereby reducing the LOS as well as hospitalization costs.
Keywords: elderly, open posterior lumbar fusion, length of stay, clinical factors, complication, outcome
1. Introduction
As global life expectancy increases, the mean age of patients with painful lumbar degenerative diseases requiring surgery has significantly increased.[1,2] A growing number of elderly patients (age >60 years) have multiple lumbar degenerative diseases, including disc herniation, stenosis, and/or lumbar spondylolisthesis.[3] Lumbar posterior fusion is a commonly used surgical procedure for treating these spine disorders and carries good patient prognosis as well as low morbidity.[4,5] The average cost for patients undergoing lumbar fusion has reportedly doubled over the past decade, and the length of stay (LOS) in the hospital is closely related to patient hospitalization costs.[6,7] Previous studies have reported that LOS prolongation is associated with increased risk of postoperative complications such as postoperative infection, deep vein thrombosis, hospital-acquired infections, and delirium.[8–13] Therefore, it is important to determine the factors that affect the LOS to reduce costs, shorten the LOS, and set a reasonable expectation for patients and providers.
Previous reports in the spine literature on the use of multivariate analysis to determine the factors affecting LOS following revision posterior lumbar fusion surgery found age to be the only significant predictor of longer hospital stays after revision surgery.[14] To the best of our knowledge, there have been no studies using multivariate analysis to determine clinical factors that influence LOS prolongation after elective posterior lumbar fusion in elderly patients. The aim of this study was to determine the independent factors affecting the extended LOS in elderly patients undergoing elective posterior lumbar fusion by using multiple linear regression analysis.
2. Methods
2.1. Patient cohort
The study identified 303 elderly patients (166 males, 137 females) who underwent first-time elective open lumbar posterior fusion surgery at our center between December 2012 and December 2017 and reviewed their electronic medical records and charts in a retrospective, blind manner (see Table, Supplemental Content, which shows the clinical data for the patient population). The primary inclusion criteria included patients aged ≥60 years who were diagnosed with lumbar spondylolisthesis, lumbar spinal stenosis, disc degeneration, or disc protrusion as confirmed by a spine surgeon. In an attempt to generate a more homogeneous population, cases involving tumor, scoliosis, trauma, or infected fusions were excluded, leaving only cases of degenerative conditions. Patients with an anterior/posterior combined approach, minimally invasive technique, or any other unrelated surgical or emergency procedure were excluded from the analysis. In addition, patients undergoing secondary revision surgery or patients with incomplete data were excluded. Patients who met the criteria were pulled out of the electronic record based on a search by procedure codes. The information was entered by one co-investigator and coded to maintain its integrity. All patients who met the criteria of undergoing elective lumbar posterior fusion surgery were included in the database. The institutional review board of our center approved this study.
2.2. Clinical data
We evaluated the clinical demographic data of the selected patients, including age, gender, preoperative waiting time, body mass index (BMI), presence or absence of smoking, and alcohol abuse. Other preoperative variables collected included the American Society of Anesthesiologists (ASA) score, levels instrumented, and the history of major medical comorbidities (diabetes and involvement of the cardiovascular, pulmonary, nervous, and urinary systems). The preoperative waiting time was defined as the time from admission to the day of surgery, and was divided into preoperative waiting time more than or equal to the 75th percentile (increased preoperative waiting time) and preoperative waiting time less than the 75th percentile (normal preoperative waiting time) for this cohort. A cardiac comorbidity was defined as a history of hypertension, congestive heart failure (within 30 days before admission), coronary artery disease, myocardial infarction (within 6 months before admission), previous percutaneous coronary intervention or angina (within 1 month before admission), previous cardiac surgery, atrial fibrillation, cardiac murmur, or arrhythmia. A pulmonary comorbidity was defined as a history of chronic obstructive pulmonary disease requiring ventilator-assisted respiration within 48 hours before surgery or current pneumonia, chronic bronchitis, asthma, or pulmonary embolism. A neurological comorbidity was defined as impaired sensorium, coma for more than 24 hours, hemiplegia, paraplegia, quadriplegia, tumors involving the central nervous system, or a history of transient ischemic attacks or cerebrovascular accidents. An urinary system comorbidity was defined as a history of prostate disease, tumor involving the urinary system, or urinary calculi requiring hospitalization.
Perioperative variables collected included operative time, intraoperative estimated blood loss (EBL), multiple surgery, and postoperative complications. Operative time was defined as the time from the first incision to the closure of the postoperative dressing, and was divided into operative time more than or equal to the 75th percentile (extended operative time) and operative time less than the 75th percentile (normal operative time) for this cohort. Intraoperative EBL included blood loss in the dressing and the volume of blood drawn or recovered in the aspiration container, details of which were collected from the anesthesia record. Multiple procedures were defined as the need to return to the operating room due to any complications that occurred after the surgery. Postoperative complications were divided into major complications and infectious complications. Major complications were defined as any organ space infection, respiratory complications (pneumonia, unplanned intubation, or ventilator dependence), cardiac complications (cardiac arrest or myocardial infarction), cerebrovascular accidents with neurological deficits/stroke, sepsis or septic shock, postoperative cerebrospinal fluid leakage, failed back surgery syndrome (FBSS), pulmonary embolism, deep vein thrombosis, acute renal failure, return to the operating room, or death. Infectious complications include urinary tract infections and superficial or deep wound infections.
2.3. Length of stay
The study endpoint was the hospital LOS, defined as the number of calendar days from admission to discharge. For univariate analysis, patient LOS was classified as normal LOS (<75th percentile LOS) or extended LOS (≥75th percentile LOS).[15] For multivariate analysis, the LOS was considered a continuous variable so that the magnitude of the impact of each predictor on the LOS could be determined.
2.4. Statistical analysis
SPSS Statistics Version 22.0 (IBM, Chicago, IL) was used for all statistical analyses. Descriptive statistics are expressed as mean and standard deviation. Univariate analysis of the hospitalization time of the two groups using independent sample t tests, comparison of the hospitalization time of multiple groups using variance analysis or Brown-Forsythe analysis, and pairwise comparison using Bonferroni correction or the Tamhane test were performed. The Brown-Forsythe test determines whether the mean of each group is equal using the statistics of the Brown-Forsythe distribution. The Brown-Forsythe distribution has no requirement for the homogeneity of the variance. When the distribution of the dependent variables does not meet the requirements for homogeneity of variance, the Brown-Forsythe test is more suitable than the analysis of variance. The Tamhane test is a nonparametric test that applies to the unequal variance of the 2 populations.[16] The hospitalization time extension rates were compared using the chi-square test and the Fisher's exact test was used when the chi-square test was not satisfactory; Bonferroni correction was further used for pairwise comparisons. Multivariate linear stepwise regression analysis was performed using LOS as a continuous outcome variable. All tests were 2-tailed and factors with a P value < .05 were considered statistically significant and were included as potential risk factors in multivariate analysis to determine significant independent risk factors for extended LOS.[8]
3. Results
3.1. General information and clinical data
The average age of the 303 patients was 67.0 ± 5.5 years (mean ± standard deviation), ranging from 60 to 86 years. The average LOS was 18.5 ± 11.8 days, ranging from 7 to 103 days. According to the definition of extended LOS as greater than or equal to the 75th percentile LOS, 83 patients (27.4%) were classified as having extended LOS. Table 1 shows the clinical characteristics of the patient population, including demographic characteristics and patient comorbidities.
Table 1.
General information and clinical characteristics of patients after posterior lumbar fusion.
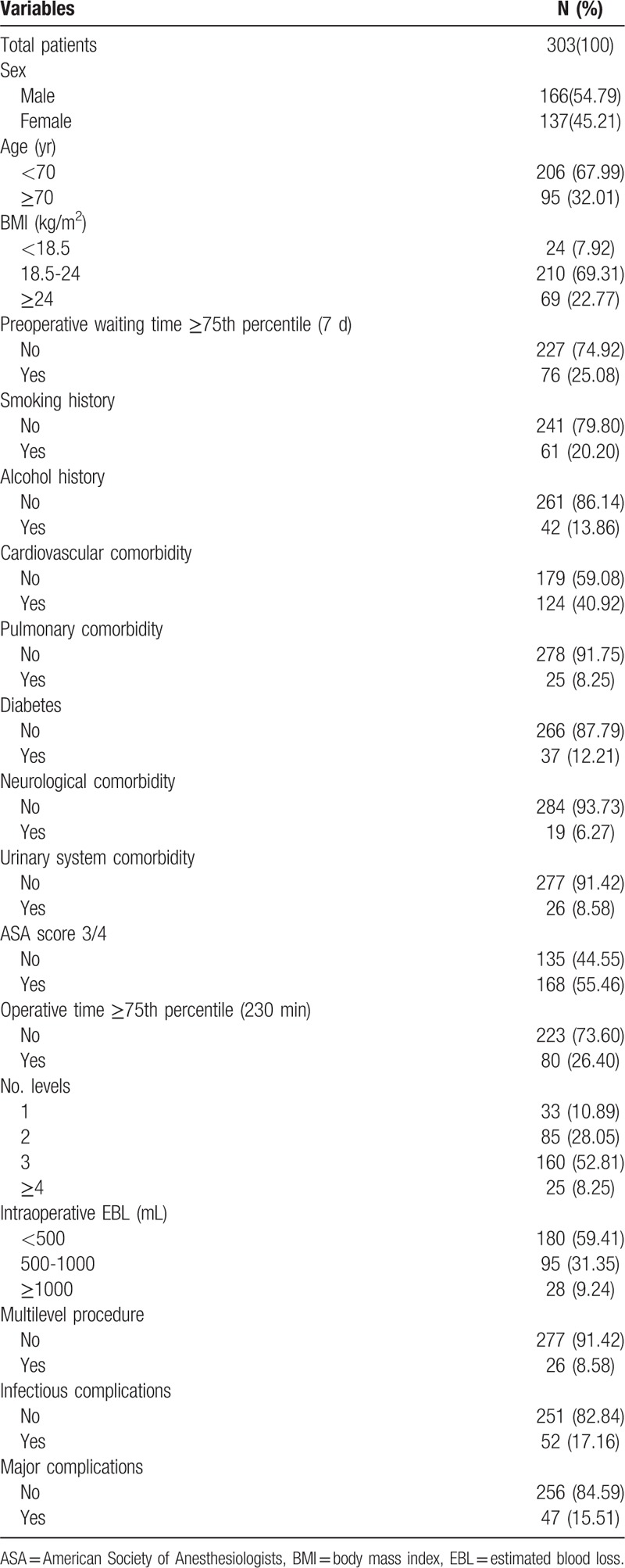
Comorbid conditions included cardiovascular comorbidity (n = 124, 40.9%), pulmonary comorbidity (n = 25, 8.3%), diabetes (n = 37, 12.2%), neurological comorbidity (n = 19, 6.3%), urinary system comorbidity (n = 26, 8.3%). Postoperative complications occurred in 74 patients (24.4%), including 47 patients (15.5%) with major complications and 52 patients (17.2%) with infectious complications.
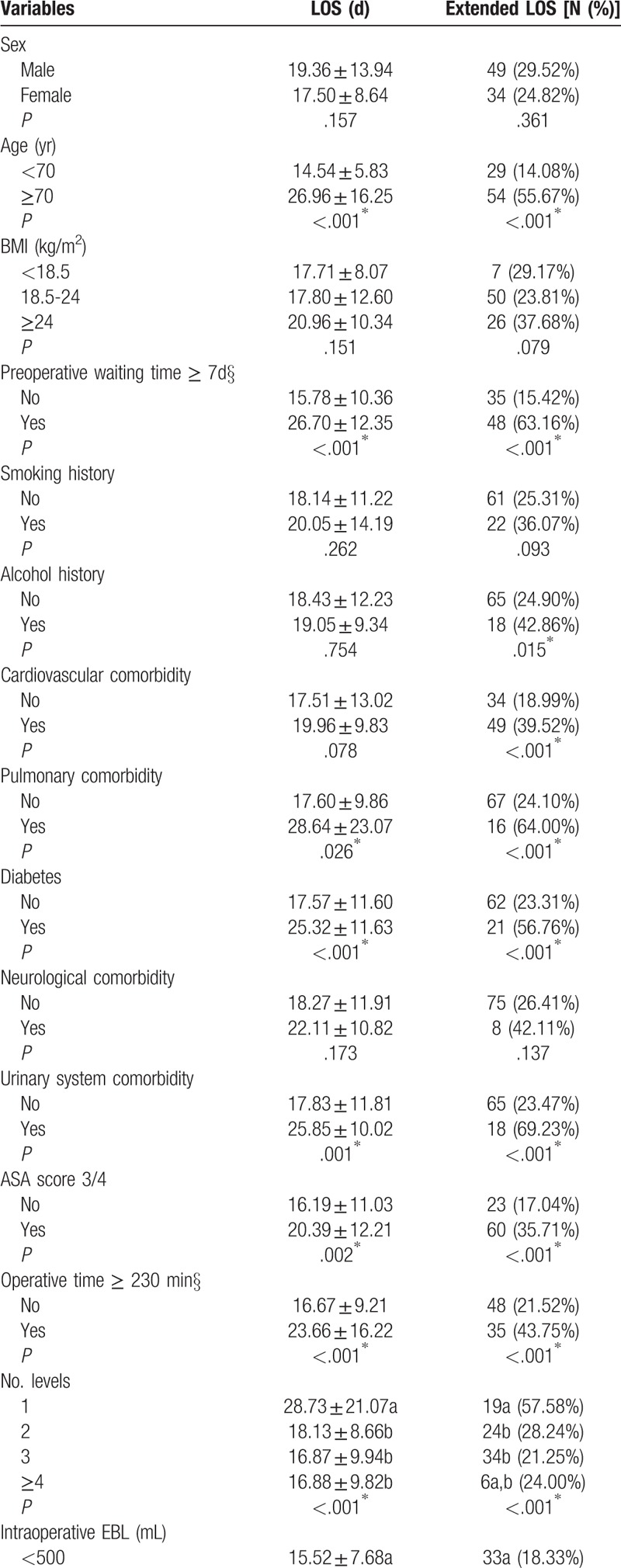
3.2. Univariate analysis
A non-adjusted univariate correlation analysis of patient LOS and LOS extension rate was performed to test the effect of each preoperative variable and perioperative variable on the LOS. The results of all analyses can be seen in Table 2 . From the univariate analysis, the important risk factors for extended LOS were age ≥70 years, preoperative waiting time ≥7 days, diabetes history, cardiovascular complications, pulmonary comorbidities, urinary tract comorbidities, alcohol abuse, extended surgery time, levels instrumented, intraoperative EBL, ASA score, multiple surgeries, and postoperative complications (Table 2 ).
Table 2.
Clinical characteristics of patient population and univariate association with LOS and LOS extension rate.
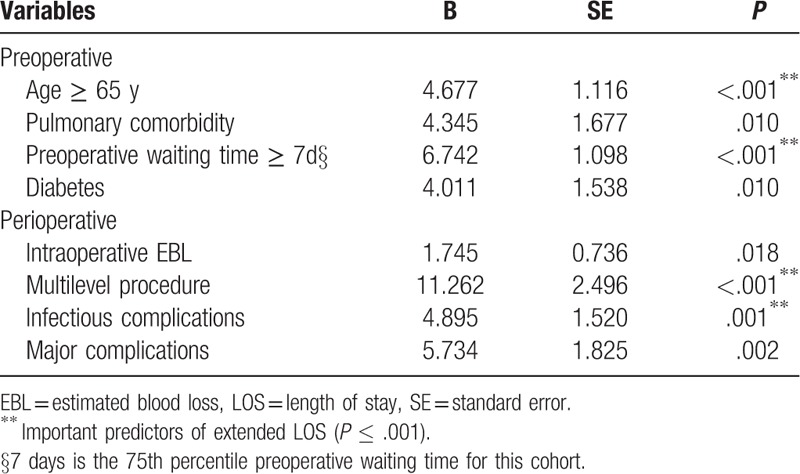
3.3. Multivariate analysis
The variables with P value < .05 in the univariate analysis were selected for multivariate analysis. The collinearity diagnosis was performed using a variance inflation factor for multicollinearity, and the result was 0 < VIF < 10, so there was no collinearity between the respective variables. The least-squared mean length of hospital stay for relevant factors in the multivariate analysis was 18.6 ± 9.4 days. In assessing LOS, multivariate analysis showed that the variables shown in Table 3 were significant predictors of LOS prolongation when controlled for other variables. Preoperative factors associated with extended LOS included age (P < .001), preoperative waiting time ≥7 days (P < .001), pulmonary comorbidities (P = .010), and diabetes (P = .010). Perioperative factors associated with extended LOS included major complications (P = .002), infectious complications (P = .001), multiple surgeries (P < .001), and intraoperative EBL (P = .018). ASA, operative time, and levels instrumented did not predict the LOS, probably due to the tilt of the first-order case in our sample.
Table 2 (Continued).
Clinical characteristics of patient population and univariate association with LOS and LOS extension rate.
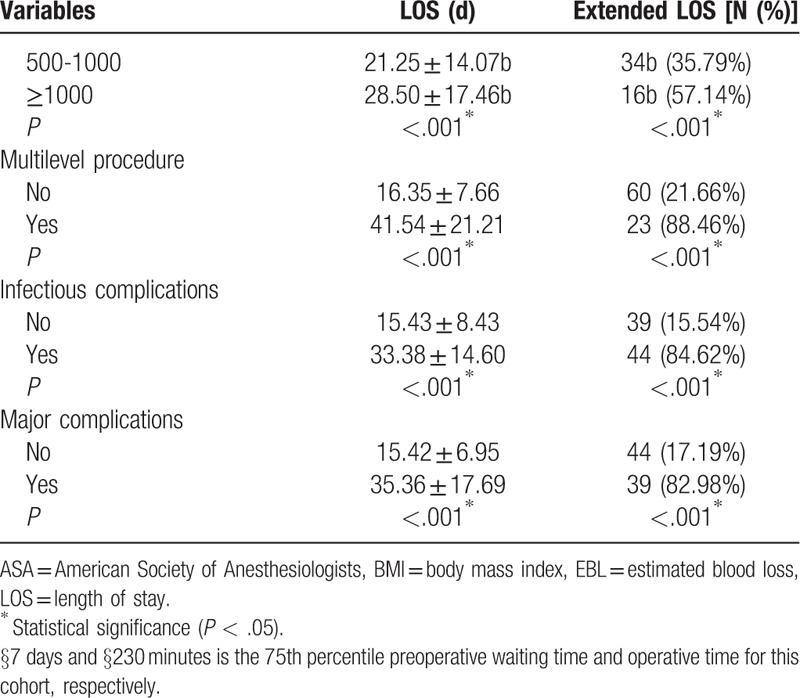
Table 3.
Multiple linear regression analysis for extended LOS after posterior lumbar fusion.
4. Discussion
With the advent of global aging, degenerative lumbar diseases are more prevalent in elderly patients (≥60 years) and have become the most common indication for spinal surgery in them.[17] The total prevalence of degenerative lumbar diseases in men and women aged 40 and over in China is about 29.4%.[18] Elective lumbar posterior fusion is the most common spinal surgery for the treatment of degenerative lumbar disease, which can significantly improve pain, mobility, and daily life.[4,5] The LOS is an important clinical variable and a major determinant of hospitalization costs. This study was designed to determine the independent factors affecting LOS prolongation in elderly patients undergoing first-time elective open posterior lumbar fusion surgery. In this study, age, preoperative waiting time ≥7 days, infectious complications, and multiple surgeries were important predictors of LOS prolongation.
LOS prolongation after elective posterior lumbar fusion is mainly due to the following aspects:
-
1.
basic comorbidities of the patient,
-
2.
postoperative complications that may require further medical and/or surgical intervention, and
-
3.
differences in physician and/or hospital practice.
Previous studies have shown that many independent variables affect LOS in all types of spinal surgery patients. Preoperative factors associated with extended LOS include age, morbid obesity, diabetes, metabolic syndrome, preoperative comorbidities, opioid use, and unemployment.[19–23] Perioperative factors associated with extended LOS include open surgery, use of fibrin sealants, intraoperative complications, intraoperative fluid administration, and drain use.[24–26] Moreover, postoperative factors including blood transfusion and complications are also associated with extended LOS.[14] Therefore, it is significantly important to further understand the extent to which patient-based comorbidities and postoperative complications contribute to LOS prolongation.
Previous studies have shown that increase in age is an important predictor of LOS prolongation after lumbar fusion.[14,19] Zheng et al[14] used a multivariate analysis of 112 patients who underwent revision lumbar fusion between 1992 and 1999 and found that age-related increase was the only significant predictor of LOS prolongation. Furthermore, Nie et al[19] reported significant differences in the LOS between elderly and middle-aged patients after lumbar discectomy. Our study also shows that age is an important predictor of the LOS, and an increase in age will significantly lead to prolonged LOS in patients. Zheng et al[14] confirmed that the number of baseline comorbidities in elderly patients increased significantly, and the incidence of postoperative complications may be higher.
In the literature on lumbar fusion surgery, there is a lack of research on the preoperative variable of “preoperative waiting time.” Our study is the first to explore the effect of preoperative waiting time on LOS prolongation after lumbar fusion and found that an increase in preoperative waiting time (≥7 days) was another important predictor of LOS prolongation. Orosz et al's prospective cohort study of 1206 hip fractures found that early surgery after admission failed to improve the patient's survival rate or postoperative mobility, but could effectively reduce the time of severe pain and the occurrence of stress ulcers while reducing patient LOS (about 1.94 days).[27] Therefore, reducing the preoperative waiting time can effectively shorten the patient's LOS, reduce hospitalization costs, speed up the utilization of medical resources, and reduce patient suffering to improve patient quality of life.
In addition, our study also showed that infectious complications and multiple surgeries are important predictors of LOS prolongation in elderly patients. Gruskay et al's study of 103 patients of all ages undergoing posterior lumbar surgery found that the average LOS for patients with a complication was greater than that for patients without a complication (5.1 days vs 2.9 days).[28] In our study, the average LOS for patients with and without infectious complications was 33.38 ± 14.60 days and 15.43 ± 8.43 days, respectively, and the average LOS was significantly prolonged in patients with infectious complications. Furthermore, infectious complications are significantly associated with multiple surgeries. The main cause of multiple surgeries in most patients is a postoperative infectious complication such as wound infection requiring debridement and primary or secondary wound closure. Therefore, both of these factors were found to be important predictors in the final multivariate analysis.
Previous studies have shown that ASA, operative time, and levels instrumented are associated with extended LOS after lumbar fusion.[14,27] Although these variables do not predict LOS in our study, it is worth noting that all of these variables are important in univariate analysis, and surgeons still should be aware of and avoid these factors as much as possible.
Although we have found the important predictors of LOS prolongation after elective posterior lumbar fusion in elderly patients, there are still some limitations in this study. First, this is a retrospective single-center study that could be influenced by the common shortcomings of retrospective analysis, including limitations that can potentially be affected by information and patient selection bias. Second, the sample size was small. Although we have identified an association, this does not mean causality. Future multi-center studies with larger cohorts should be conducted to identify different relevant factors to guide the surgeon in preoperative planning. Other potential limitations include differences in national health care systems, patient inclusion guidelines, surgeons’ techniques, patients, and the medical environment background. Although these are potential weaknesses, this study is the first to identify important predictors of LOS prolongation in elderly patients undergoing elective open posterior lumbar fusion surgery.
5. Conclusion
In conclusion, the important predictors of LOS prolongation after elective posterior lumbar fusion in elderly patients are age, preoperative waiting time ≥7 days, infectious complications, and multiple operations. Spinal surgeons should recognize and note these risk factors while taking appropriate precautions to optimize the modifiable factors, thereby reducing LOS and hospitalization costs, and utilize the non-optimizable factors for patient counseling and postoperative planning.
Acknowledgments
We greatly appreciate the patient and her family for allowing us to use the medical documents and information that led to the present article. We would like to thank Editage for English language editing.
Author contributions
Data curation: Huaen Xu, Hangjun Chen.
Formal analysis: Xiaolong Yu, Qiang Xu.
Investigation: Haibo Zhan, Huaen Xu, Qiang Xu, Hangjun Chen.
Methodology: Xuqiang Liu, Xiaolong Yu, Min Dai, Bin Zhang.
Project administration: Min Dai, Bin Zhang.
Resources: Runsheng Guo, Xuqiang Liu.
Supervision: Runsheng Guo.
Writing – original draft: Haibo Zhan.
Writing – review & editing: Haibo Zhan, Runsheng Guo, Min Dai, Bin Zhang.
Bin Zhang orcid: 0000-0001-6368-8357.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, BMI = body mass index, COPD = chronic obstructive pulmonary disease, EBL = estimated blood loss, LOS = length of stay.
How to cite this article: Zhan H, Guo R, Xu H, Liu X, Yu X, Xu Q, Chen H, Dai M, Zhang B. Hospital length of stay following first-time elective open posterior lumbar fusion in elderly patients: A retrospective analysis of the associated clinical factors. Medicine. 2019;98:44(e17740).
HZ, RG, and HX contributed to the work equally and should be regarded as co-first authors.
The study protocol was approved by the Ethical Institutional Review Board of the First Affiliated Hospital of Nanchang University, and written informed consent was obtained from all study participants.
The consent for publication of the manuscript and the related images from the patient and/or his relatives has been obtained by the First Affiliated Hospital of Nanchang University.
This study was supported by Science Technology Plan of Jiangxi Provincial Health Planning Commission (20175112), Gan-Po Talents Project 555 of Jiangxi Province, Jiangxi Provincial Department of Science and Technology (20171BAB205059, 20171ACG70006), Jiangxi provincial department of education (GJJ160127). The funding bodies had no role in the design of the study, data collection, analysis, and interpretation of data or in writing the manuscript.
The authors have no conflicts of interest to disclose.
The dataset supporting the conclusions of this article is included within Additional file 1. Anonymized datasets are available from the corresponding author on request following a data sharing and transparency policy.
References
- [1].Brown CHt, LaFlam A, Max L, et al. Delirium after spine surgery in older adults: incidence, risk factors, and outcomes. J Am Geriatr Soc 2016;64:2101–8. doi: 10.1111/jgs.14434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Cassinelli EH, Eubanks J, Vogt M, et al. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976) 2007;32:230–5. doi: 10.1097/01.brs.0000251918.19508.b3. [DOI] [PubMed] [Google Scholar]
- [3].Kilincer C, Steinmetz MP, Sohn MJ, et al. Effects of age on the perioperative characteristics and short-term outcome of posterior lumbar fusion surgery. J Neurosurg Spine 2005;3:34–9. doi: 10.3171/spi.2005.3.1.0034. [DOI] [PubMed] [Google Scholar]
- [4].Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Yone K, Sakou T, Kawauchi Y, et al. Indication of fusion for lumbar spinal stenosis in elderly patients and its significance. Spine (Phila Pa 1976) 1996;21:242–8. [DOI] [PubMed] [Google Scholar]
- [6].Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Epstein NE, Schwall G, Reillly T, et al. Surgeon choices, and the choice of surgeons, affect total hospital charges for single-level anterior cervical surgery. Spine (Phila Pa 1976) 2011;36:905–9. doi: 10.1097/BRS.0b013e3181e6c4d8. [DOI] [PubMed] [Google Scholar]
- [8].Gruskay JA, Fu M, Basques BA, et al. Factors affecting length of stay and complications after elective anterior cervical discectomy and fusion: a study of 2164 patients from the american college of surgeons National Surgical Quality Improvement Project Database (ACS NSQIP). Clin Spine Surg 2016;29:E34–42. [DOI] [PubMed] [Google Scholar]
- [9].Gephart MG, Zygourakis CC, Arrigo RT, et al. Venous thromboembolism after thoracic/thoracolumbar spinal fusion. World Neurosurg 2012;78:545–52. doi: 10.1016/j.wneu.2011.12.089. [DOI] [PubMed] [Google Scholar]
- [10].White RH, Zhou H, Romano PS. Length of hospital stay for treatment of deep venous thrombosis and the incidence of recurrent thromboembolism. Arch Intern Med 1998;158:1005–10. [DOI] [PubMed] [Google Scholar]
- [11].Trouillet JL, Chastre J, Vuagnat A, et al. Ventilator-associated pneumonia caused by potentially drug-resistant bacteria. Am J Respir Crit Care Med 1998;157:531–9. doi: 10.1164/ajrccm.157.2.9705064. [DOI] [PubMed] [Google Scholar]
- [12].Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis 2000;31 Suppl:S131–8. doi: 10.1086/314079. [DOI] [PubMed] [Google Scholar]
- [13].Fineberg SJ, Nandyala SV, Marquez-Lara A, et al. Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine (Phila Pa 1976) 2013;38:1790–6. doi: 10.1097/BRS.0b013e3182a0d507. [DOI] [PubMed] [Google Scholar]
- [14].Zheng F, Cammisa FP, Jr, Sandhu HS, et al. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine (Phila Pa 1976) 2002;27:818–24. [DOI] [PubMed] [Google Scholar]
- [15].Owoicho A, Desai SA, Vuong VD, et al. Extended length of stay in elderly patients after lumbar decompression and fusion surgery may not be attributable to baseline illness severity or postoperative complications. World Neurosurg 2018;116:e996–1001. [DOI] [PubMed] [Google Scholar]
- [16].Guillermo V, Manuel A. Modified brown-forsythe procedure for testing interaction effects in split-plot designs. Multivar Behav Res 2006;41:549–78. [DOI] [PubMed] [Google Scholar]
- [17].Taylor VM, Deyo RA, Cherkin DC, et al. Low back pain hospitalization. Recent United States trends and regional variations. Spine (Phila Pa 1976) 1994;19:1207–12. discussion 1213. [DOI] [PubMed] [Google Scholar]
- [18].Tian W, Lv YW, Liu YJ, et al. The high prevalence of symptomatic degenerative lumbar osteoarthritis in Chinese adults: a population-based survey. Spine (Phila Pa 1976) 2014;39:1301–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Nie H, Hao J, Peng C, et al. Clinical outcomes of discectomy in octogenarian patients with lumbar disc herniation. J Spinal Disord Tech 2013;26:74–8. doi: 10.1097/BSD.0b013e318236b92d. [DOI] [PubMed] [Google Scholar]
- [20].Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine (Phila Pa 1976) 2012;37:982–8. doi: 10.1097/BRS.0b013e31823bbeef. [DOI] [PubMed] [Google Scholar]
- [21].Browne JA, Cook C, Pietrobon R, et al. Diabetes and early postoperative outcomes following lumbar fusion. Spine (Phila Pa 1976) 2007;32:2214–9. doi: 10.1097/BRS.0b013e31814b1bc0. [DOI] [PubMed] [Google Scholar]
- [22].Memtsoudis SG, Kirksey M, Ma Y, et al. Metabolic syndrome and lumbar spine fusion surgery: epidemiology and perioperative outcomes. Spine (Phila Pa 1976) 2012;37:989–95. doi: 10.1097/BRS.0b013e31823a3a13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Walid MS, Robinson EC, Robinson JS., Jr Higher comorbidity rates in unemployed patients may significantly impact the cost of spine surgery. J Clin Neurosci 2011;18:640–4. doi: 10.1016/j.jocn.2010.08.029. [DOI] [PubMed] [Google Scholar]
- [24].Lee KH, Yue WM, Yeo W, et al. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 2012;21:2265–70. doi: 10.1007/s00586-012-2281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Yeom JS, Buchowski JM, Shen HX, et al. Effect of fibrin sealant on drain output and duration of hospitalization after multilevel anterior cervical fusion: a retrospective matched pair analysis. Spine (Phila Pa 1976) 2008;33:E543–7. doi: 10.1097/BRS.0b013e31817c6c9b. [DOI] [PubMed] [Google Scholar]
- [26].Street JT, Lenehan BJ, DiPaola CP, et al. Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients. Spine J 2012;12:22–34. doi: 10.1016/j.spinee.2011.12.003. [DOI] [PubMed] [Google Scholar]
- [27].Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA 2004;291:1738–43. doi: 10.1001/jama.291.14.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Gruskay JA, Fu M, Bohl DD, et al. Factors affecting length of stay after elective posterior lumbar spine surgery: a multivariate analysis. Spine J 2015;15:1188–95. doi: 10.1016/j.spinee.2013.10.022. [DOI] [PubMed] [Google Scholar]


