Abstract
Objective
Income volatility presents a growing public health threat. To our knowledge, no previous study examined the relationship among income volatility, cognitive function, and brain integrity.
Methods
We studied 3,287 participants aged 23–35 years in 1990 from the Coronary Artery Risk Development in Young Adults prospective cohort study. Income volatility data were created using income data collected from 1990 to 2010 and defined as SD of percent change in income and number of income drops ≥25% (categorized as 0, 1, or 2+). In 2010, cognitive tests (n = 3,287) and brain scans (n = 716) were obtained.
Results
After covariate adjustment, higher income volatility was associated with worse performance on processing speed (β = −1.09, 95% confidence interval [CI] −1.73 to −0.44) and executive functioning (β = 2.53, 95% CI 0.60–4.50) but not on verbal memory (β = −0.02, 95% CI −0.16 to 0.11). Similarly, additional income drops were associated with worse performance on processing speed and executive functioning. Higher income volatility and more income drops were also associated with worse microstructural integrity of total brain and total white matter. All findings were similar when restricted to those with high education, suggesting reverse causation may not explain these findings.
Conclusion
Income volatility over a 20-year period of formative earning years was associated with worse cognitive function and brain integrity in midlife.
Changes in income, known as income volatility, have become more frequent in the United States and are at record levels since the 1980s.1,2 More than a third of US households experienced a 25% or more change in income between 2014 and 2015.3 Income volatility presents a growing concern and yet policies intending to smooth unpredictable income changes are being weakened in the United States and many other first-world countries.4 Negative health consequences, such as morbidity and mortality, due to low income and other indicators of social disadvantage have been well-documented.5–8 However, the effect of income volatility over a prolonged period of time on health outcomes remains relatively unexplored.9–12
With people now living longer, healthy aging and the maintenance of cognitive abilities have become more important than ever. Poor socioeconomic conditions, during childhood, adulthood, or cumulatively across the life course, have been associated with cognitive deficits.13–22 However, repeated measures of income over many years are seldom available, even in the few studies that take a life-course approach to characterizing socioeconomic status (SES). As a result, researchers have rarely been able to examine long-term measures of income volatility, especially with respect to cognitive outcomes.15,22 Furthermore, most prior studies have focused on the association between SES and cognitive health at older ages,13–18 while its association with cognitive health earlier in the life course remains relatively underexplored. The latter is especially important as it is becoming increasingly clear that maintaining cognitive health is a lifelong process as old age conditions such as dementia have a long preclinical period.23
The Coronary Artery Risk Development in Young Adults study (CARDIA) is uniquely suited to address several of these gaps in the literature. It is an ongoing prospective study of young to middle-aged adults for whom income data have been collected since the early 1990s, during participants’ formative earning years, and cognitive testing and brain imaging have been ascertained 20 years later in midlife. In this study, we aim to explore the relationship between measures of income volatility from 1990 to 2010 and cognitive function and brain volumes as well as microstructural integrity in 2010.
Methods
Study population
We used data from CARDIA, an ongoing prospective study aiming to examine the development and determinants of cardiovascular disease (CVD) and its risk factors beginning in young adulthood. Details of the study have been published.24 Briefly, 5,115 black and white men and women aged 18–30 years at baseline were recruited in 1985–1986 from 4 field centers: Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. Recruitment was balanced within center by sex, age, race, and education subgroups. The data from one participant who dropped out of the study were removed from the study at his request. Participants were examined at baseline and followed every 2–5 years up to 30 years. In the present study, baseline was defined as the 1990 visit, at time of the first income assessment. Standardized questionnaires were used to collect demographic, socioeconomic, and clinical data at each follow-up visit.
Income volatility from 1990 to 2010
During CARDIA examination years 1990, 1992, 1995, 2000, 2005, and 2010, pretax household income for the last 12 months from all sources was self-reported and recorded in income brackets as follows: $0–$2,500, $2,500–$8,500, $8,500–$14,000, $14,000–$20,500, $20,500–$30,000, $30,000–$42,500, $42,500–$62,500, $62,500–$75,000, and $75,000+. The income category midpoint was chosen as the participant's income for each given exam year.22,25 All incomes in the top (highest) open-ended bracket were coded as $75,000. We limited this analysis to participants with at least 3 repeated measures of income. We then created 2 predictors of interest: (1) the SD of percent change in income and (2) number of income drops.
Primary economic predictors
SD of percent change in income
We followed previous literature12,26 and defined income volatility as the intraindividual SD of the percent change in inflation-adjusted income from 1990 to 2010. To account for inflation between 1990 and 2010, we first deflated all nominal dollars into real 1990 dollars using the consumer price index for each corresponding year.27 Second, we calculated, for each participant, the percent change in inflation-adjusted income between every 2 consecutive examination years as [(Yt2 − Yt1)/0.5 (Yt1 + Yt2)] × 100. Dividing the denominator by 2 helps in restricting the range of the percent change by naturally bounding it to 200% and −200%.26 If a participant was missing an income measure for a given examination year, the income measure at the next available visit was used. Finally, for each participant, we then calculated the SD of those percent changes. This measure of income volatility captures both negative and positive income changes.
Number of income drops
To address negative volatility, we also calculated the number of income drops.10,12 An income drop was defined as a decrease of 25% or more in income, compared to the previous study visit’s income, and less than the participant’s average income from 1990 to 2010. Given that inflation alone could result in a 25% income drop for some categories but not others, for this measure we did not adjust income for inflation. The number of those drops between 1990 and 2010 was the predictor of interest and was categorized into 0, 1, or 2+ drops.
Secondary economic predictor
Income trajectories
To help further distinguish the directionality of income volatility (i.e., positive, negative, or both), we created an income trajectory measure with 4 mutually exclusive groups corresponding to income measures from 1990 to 2010: (1) no income changes, (2) at least 1 income increase with no decreases, (3) fluctuating income (at least 1 income increase and 1 income decrease), or (4) at least 1 income decrease with no increases. Income trajectory groups 1 and 2 (no income change/increase only) were then combined because of the small sample size of the group with no income change.
Cognition and brain integrity outcomes in 2010
Cognitive function
In 2010, participants were administered a cognitive battery that included the following 3 cognitive tests: the Rey Auditory Verbal Learning Test (RAVLT, range 0–15) measuring verbal memory and assessing the ability to memorize and retrieve words28; the Digit Symbol Substitution Test (DSST, range 0–133), a subtest of the Wechsler Adult Intelligence Scale measuring processing speed29; and the interference score on the Stroop test (executive skills), measuring the additional amount of processing time needed to respond to one stimulus while suppressing another.30 The Stroop test was scored by seconds to spell out color words printed in a different color plus number of errors. For the RAVLT and the DSST, a higher score (in words or in symbols, respectively) indicates better performance, whereas for the Stroop test, a higher score (seconds + errors) indicates worse performance.
Brain MRI measures
In 2010, the CARDIA Brain MRI Ancillary Study, which included 3 of the 4 CARDIA sites (Birmingham, Minneapolis, and Oakland), enrolled a total of 719 participants. The procedures for the CARDIA MRI Ancillary Study have been described previously.31 Participants underwent a brain MRI on 3T MRI scanners. An automated pipeline was used with preprocessing, intermediate, and postprocessing quality control steps. Using Hammer, T1-weighted images were parcellated into anatomical regions of interest by deformable registration to the Jakob atlas. From T1, T2, and fluid-attenuated inversion recovery scans, white matter lesions were segmented using a multiparametric, automated algorithm. Calculation of fractional anisotropy (FA) was done through custom-developed Insight Toolkit software (itk.org). Results were registered to subject T1 space for segmentation using FSL (https://fsl.fmrib.ox.ac.uk/fsl/fslwiki). Left and right hemispheric measurements were summed to create all FA and volume measures including total intracranial volume (ICV).
Our MRI outcomes of interest included normal tissue volumes of the hippocampus, gray matter, white matter, and total brain (sum of gray and white matter). Each normal tissue volume was standardized by dividing each by ICV. We also examined brain microstructural integrity using FA, also for the hippocampus, gray matter, white matter, and total brain. FA measures the degree to which water diffuses with uniformity in the brain and ranges from 0 to 1, with 0 indicating equal probability of diffusion in all directions (i.e., no structural restriction) and 1 indicating diffusion along one axis in the brain.
Other covariates
At baseline in 1990, participants reported sociodemographic information such as age, sex, race, and education (recoded into less than or equal to high school [HS] education vs more than HS). Marital status (married or not), number of people in the household, and employment status (yes or no) were self-reported. Smoking status was defined as never, current, and former. Body mass index (BMI) in kg/m2 was calculated using measured weight and height. Systolic blood pressure (SBP, mm Hg) was measured while seated using a standard automated blood pressure measurement monitor. Participants also reported use of any antihypertensive medications. Fasting glucose (mg/dL) as well as total cholesterol (mg/dL) were measured from blood samples drawn after an overnight fast. Participants reported the amount of time per week spent in 13 categories of physical activity over the last year, and then the total amount in exercise units was calculated. Symptoms of depression were assessed using the 20-item Center for Epidemiologic Studies Depression Scale (range 0–60) and depression was defined as a score of 16 or higher. Most of these covariates were also collected at every follow-up in addition to the baseline examination.
For categorical covariates collected at every examination, including marital status, unemployment, antihypertensive medications, elevated depressive symptoms, and smoking, we also calculated cumulative measures from 1990 to 2010. Participants were coded as always, sometimes, or never having the condition or behavior from 1990 to 2010 (e.g., always, sometimes, or never married from 1990 to 2010). For continuous covariates collected at every examination, including BMI, SBP, fasting glucose, physical activity, total cholesterol, and number of people in the household, we calculated the average for each of these measures from 1990 to 2010.
Statistical analysis
From the total 5,114 CARDIA participants, 3,385 participants had data for at least one cognitive test in 2010. Of those, 3,287 had at least 3 income measures between 1990 and 2010, and were thus included in the cognitive analysis. For the MRI analysis, of the 719 participants enrolled in the MRI substudy, 707 participants had income volatility measures available.
Using the main cognitive analytical sample, participant characteristics at baseline in 1990 were compared across the number of income drops using analysis of variance and χ2 tests to assess differences in means and proportions, respectively. Similarly, participant characteristics were compared across tertiles of income volatility.
The associations of income volatility with cognitive performances on the RAVLT, DSST, and Stroop test, all measured in 2010, were analyzed separately using linear regression models. Similar models were used to examine the associations between income volatility and brain MRI metrics (normal tissue volumes and FA). After checking for normality, the Stroop test, total brain FA, gray matter FA, and hippocampal FA were log-transformed to account for their skewed distributions. The estimates were then back-transformed and can be interpreted as the percentage change in the score for each unit increase in the predictor. Three different models were estimated to account for possible confounding. Potential confounders were chosen a priori based on the literature of social determinants of cognitive aging. The first model was adjusted for baseline (year 1990) age, sex, race, more than HS education, marital status, number of people in the household, and study site. The second model was additionally adjusted for BMI, SBP, hypertension medication, total cholesterol, fasting glucose, physical activity, smoking status, and depression, all measured in 1990, except for fasting glucose, which was first measured in 1992. Finally, the third model was additionally adjusted for year 1990 income and employment status.
We performed the following 6 sensitivity analyses: first, to further investigate whether the relationship between income volatility as SD of percent change and cognitive function is indeed linear, we modelled income volatility using restricted cubic splines regression. Second, to address the fact that many covariates, measured during the income volatility period from 1990 to 2010, also vary over time, we repeated our original analyses while adjusting for cumulative covariates from 1990 to 2010, instead of just baseline. Third, since we do not have measures of cognitive function at baseline, we attempted to address potential reverse causation (i.e., that low cognitive function at baseline resulted in income volatility) by rerunning the main analyses restricted to participants with more than HS education at baseline (n = 2,249). Fourth, we repeated the main cognitive analysis applying inverse probability of censoring weights (IPCW), to account for attrition between baseline (in 1990) and the time of cognitive assessment (in 2010). Fifth, we repeated our cognitive models using our secondary economic predictor (income trajectories). Sixth, to examine whether the relation between income volatility and cognitive function varies according to income level, we tested for statistical interactions between income volatility and each level of baseline income and average income. Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).32
Standard protocols approval, registrations, and patient consent
Appropriate informed consent was obtained from study participants, and the study was approved by the institutional review boards from each field center and the coordinating center.
Data availability
CARDIA facilitates data sharing through formal data use agreements. Any investigator is welcome to access the CARDIA data through this process.
Results
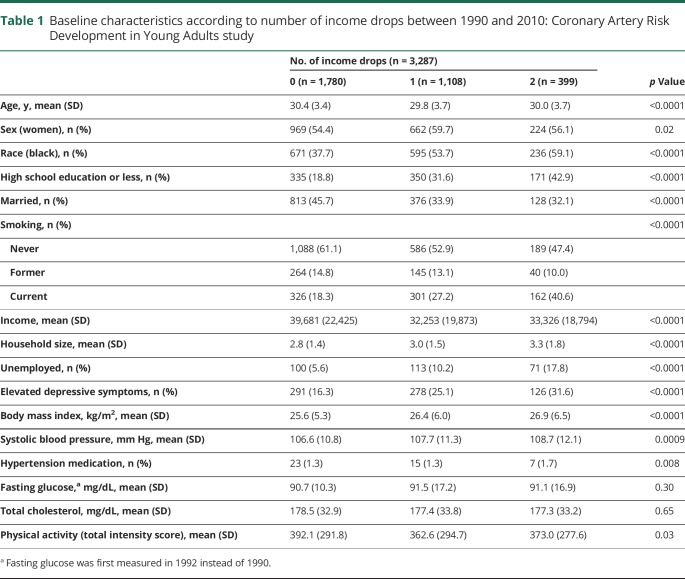
A description of baseline characteristics according to the number of income drops is shown in table 1. Similarly, this description according to tertiles of income volatility is presented in table e-1 (doi.org/10.5061/dryad.9nm0697). In general, participants with more income drops were more likely to be black, less educated, unmarried, and smokers, and with lower income and unemployed at baseline. Those with more income drops also had more elevated depressive symptoms, had higher mean BMI and SBP, and were less physically active. Similar repartitions were found across tertiles of income volatility.
Table 1.
Baseline characteristics according to number of income drops between 1990 and 2010: Coronary Artery Risk Development in Young Adults study
Income volatility from 1990 to 2010 and cognitive function in 2010
In the minimally adjusted model 1, higher income volatility (per 1 SD difference) was associated with worse performance on the DSST and the Stroop test (table 2); these associations were slightly attenuated but remained significant in the further-adjusted models 2 and 3 (In model 3, DSST: β = −1.09, 95% confidence interval [CI] −1.73 to −0.46; Stroop: β = 2.53, 95% CI 0.60–4.39). For reference, these associations per 1 SD in income volatility were greater than a 1-year increment in age estimate (age β for DSST association −0.71, 95% CI −0.86 to −0.56; age β for Stroop association 1.41, 95% CI 0.96 to 1.87). Income volatility was not associated with performance on the RAVLT. When modeling income volatility using restricted cubic splines (figure e-1, doi.org/10.5061/dryad.9nm0697), we generally observed a linear relationship, which is in support of how we modeled income volatility (per 1 SD) in the main analyses.
Table 2.
Multivariable adjusted associations of income volatility and number of income drops (1990–2010) with cognitive scores in 2010: Coronary Artery Risk Development in Young Adults study
Compared to having no income drops, having 1 or 2+ income drops was associated with worse performance on the DSST (1 drop: β = −1.74, 95% CI −2.87 to −0.61; 2+ drops: β = −3.74, 95% CI −5.35 to −2.12) from fully adjusted models (table 2). Compared to no income drops, having 2+ income drops was associated with worse performance on the Stroop (β = 8.04, 95% CI 2.94–13.31) from fully adjusted models. Number of income drops was not associated with performance on the RAVLT.
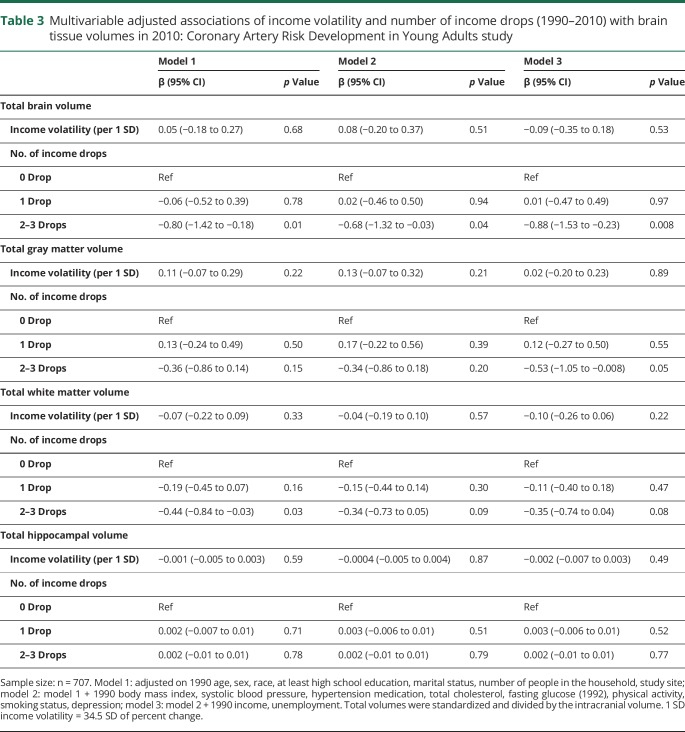
Income volatility from 1990 to 2010 and brain MRI markers in 2010
Compared to no income drops, having 2+ income drops was associated with smaller total brain volume (β = −0.88, 95% CI −1.53 to −0.23) from fully adjusted models (table 3). Having 2+ income drops was also associated with smaller white matter volume, but only in the minimally adjusted model (β = −0.44, 95% CI −0.84 to −0.03); this association was attenuated and became nonsignificant in further adjusted models. Number of income drops was not associated with gray matter volume or hippocampal volume. Income volatility (per 1 SD higher) was not associated with MRI volumes.
Table 3.
Multivariable adjusted associations of income volatility and number of income drops (1990–2010) with brain tissue volumes in 2010: Coronary Artery Risk Development in Young Adults study
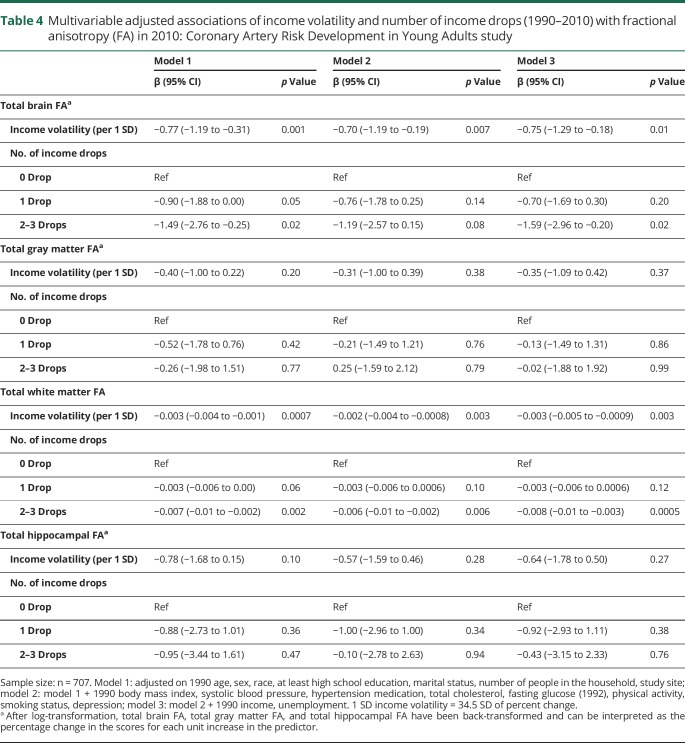
Associations with microstructural brain integrity, as FA, are presented in table 4. In general, we found that higher income volatility (per 1 SD higher) was associated with lower total brain FA (β = −0.75, 95% CI −1.29 to −0.18) and lower white matter FA (β = −0.003, 95% CI −0.005 to −0.0009) in fully adjusted models. Similarly, compared to no income drops, having 2+ income drops was associated with lower total brain FA (β = −1.59, 95% CI −2.96 to −0.20) and lower white matter FA (β = −0.008, 95% CI −0.01 to −0.003) from fully adjusted models. Higher income volatility (per SD higher) and number of income drops were not associated with gray matter and hippocampal FA.
Table 4.
Multivariable adjusted associations of income volatility and number of income drops (1990–2010) with fractional anisotropy (FA) in 2010: Coronary Artery Risk Development in Young Adults study
Sensitivity analyses
Results from sensitivity analyses adjusted for cumulative measures (1990–2010) (table e-2, doi.org/10.5061/dryad.9nm0697) or restricted to participants with more than HS education (table e-3) were similar to the findings from the primary analyses. Then, results accounting for selective attrition using inverse probability weights were also similar to the main results (table e-4). Then, results from the sensitivity analysis using the income trajectories predictor (table e-5) showed that compared with individuals whose income did not change or only increased from 1990 to 2010, those with income that fluctuated had worse DSST and Stroop scores. Finally, interactions between income volatility and income level were all nonsignificant at a p value of 0.10. As such, we can say that the relation of income volatility with cognition does not vary according to income level.
Discussion
Our results suggest that income volatility during young and middle adulthood was negatively associated with cognitive function and some brain MRI measures at midlife, independent of socioeconomic and major cardiovascular risk factors. Higher income volatility and higher number of income drops over 20 years were associated with worse performance in executive functioning and processing speed but not significantly associated with delayed memory after adjustment for baseline risk factors. Moreover, higher income volatility was associated with smaller total brain volume and lower total brain and white matter FA; compared to no income drop, having 2+ drops was associated with smaller total brain volume and lower total brain and white matter FA. While the associations between income volatility and cognition remained similar when restricted to participants with high educational level at baseline, we cannot rule out the possibility of reverse causation. This exploratory study provides evidence that income volatility over a prolonged period of time during formative earning years is associated with unhealthy aging at midlife. Due to the exploratory nature of this work, we have examined an extended set of cognitive measures, volumetric brain markers, and markers of microstructural integrity; thus additional studies are needed to validate our results. Furthermore, these outcomes do not represent an underlying construct but rather are seen as markers of vulnerability to cognitive decline and brain aging.
There are several explanations as to why income volatility may influence cognitive aging. Volatility implies income drops and episodes of lower income. Exposure to low income and other socioeconomic disadvantages has been associated with unhealthy habits, such as alcohol use, smoking, and low physical activity.33–35 These behavioral factors are in turn known risk factors of poor cognitive function and risk of dementia.36,37 Income volatility and disadvantaged socioeconomic conditions may also increase exposure to depression, or cardiovascular risk factors such as obesity and hypertension, which are in turn associated with poor cognitive health.9,11,25 However, in this study, accounting for health behaviors and CVD risk factors only slightly attenuated the associations. Another possible mechanism that may explain our findings is that fluctuation in income may lead to financial strains, financial insecurity, and a greater exposure to stressors.6,38,39 Indeed, perceived stress has been shown to affect cognitive function, dementia risk, and other age-related health outcomes.40,41 In addition, individuals with reported financial difficulties may have lower access to high-quality health care,42 which may result in worse disease management and management of risk factors for cognitive function. For example, individuals experiencing income volatility or financial strains may be less likely to visit a doctor or take their medication, consequently resulting in increased risk of brain-related diseases such as stroke.4,43 Moreover, educational attainment may also directly or indirectly, through occupation, living environment, or health behaviors, influence cognitive functioning.44 Finally, participants with income volatility and income loss may have lower participation in cognitively demanding leisure activities, which are thought to enhance cognitive function.45
There is growing evidence that income volatility may have pervasive effects on health, including worse mental health, overall health quality, and all-cause mortality9,10,12; however, its relation with cognitive and brain aging remains relatively unexplored. In our study, income volatility was associated with processing speed, executive function, and total brain and white matter FA, which may be indicative of underlying CVD processes occurring over the life course. We did not find an association between income volatility and verbal memory, likely due to the relatively young age of this cohort. Overall, our results are consistent with studies examining life course SES in relation to cognitive health during late life.13–18 In previous research, higher education and late-life income were associated with higher memory function and lower decline in US representative populations.13 Other studies reported higher cognitive performance with more advantageous SES during adulthood among Mexican Americans,14,17 Finnish individuals,21 and professional women.18 However, these studies often defined SES as a composite score, and most of them relied on a single measurement of each SES component, including income. A recent study from CARDIA reported a graded association between sustained poverty and perceived financial difficulty measured over 20 years with cognitive function.22 In line with our results, this implies that the longer one experiences financial difficulties, the worse it is for the brain. Our results add to the prior literature suggesting that fluctuations in income and income losses over the course of young adulthood into midlife also have adverse influences on cognition, and that these associations can be observed as early as midlife. Enhancing the stability of income across the life course may thus play a beneficial role towards healthy cognitive aging.
Income volatility is of particular interest since there are straightforward policy options to reduce income volatility, such as unemployment insurance, or short-term income supports. Unemployment and wage insurance have been suggested and implemented as short-term strategies to offset the burdens of income shocks such as loss of a job.46 In the United States, the Earned Income Tax Credit, which provides an income subsidy to low-income employed adults, is another such policy: most households receiving a credit greater than $1,000 actually use these allocations to pay bills and debt incurred during financial emergencies.47 Further, the US Supplemental Nutritional Assistance Program has also been shown to smooth food consumption patterns among low-income households during times of income shocks.48 Although a growing body of work links these policies to various domains of physical or behavioral health,49,50 our study findings of an association among income volatility, cognitive function, and brain integrity reinforce the need for studies examining the role of such social policies on brain aging.
This study has some limitations worth noting. First, our income volatility measure relies on self-reported income collected in brackets rather than actual or exact number. As we use the midpoint of an income bracket, this may have resulted in a loss of precision and misclassification of our exposure. For example, large income changes within income brackets were not detected. Likewise, small income changes occurring close to bracket thresholds could be detected as income category changes. Despite this, on average, such misclassification is likely to be nondifferentially distributed across the study population, and therefore any potential effect on the effect size estimates would be biased towards the null. Second, although our analysis restricted to participants with more than a HS degree showed similar results, we cannot exclude reverse causation as an explanation of our results. Also, as participants needed to be alive by 2010 when cognitive function was assessed, there is a possibility of a selection of the study population. Yet when accounting for attrition throughout the study period using IPCW, the associations remained similar. Because our sample was restricted to individuals with at least 1 cognitive measure and with 3 or more measures of income, our results may not be generalizable to the original target population but only to those included in our analytical sample. Moreover, the limited set of cognitive tests did not allow us to explore additional cognitive domains. Third, cognitive function and brain structure may be ongoing parallel processes, and thus an evolution of cognitive function may indeed be the result of changes in brain structure. Due to the small size of the MRI subsample, we were unable to adjust for MRI markers in models of cognitive function. Future studies should investigate the relation between measures of cognitive change and changes in brain structure. Finally, even though we adjusted our analyses for major risk factors for cognitive impairment, residual confounding may remain due to unmeasured confounders. We attempted to address this by accounting for cumulative exposure to covariates during the income volatility period, and results were only slightly attenuated.
Despite these limitations, this study has important strengths and contributes to the sparse literature on income volatility and cognitive function and brain volumes. The CARDIA study provides an adequate setting to investigate income volatility with a long follow-up and repeated measures of income. More importantly, this study enabled us to assess income over 2 decades of these participants’ lives, at an age where most adults are in the workforce. Moreover, our income volatility measure included the recession period, when greater financial difficulties could have been encountered. Our results were consistent regardless of how income volatility was conceptualized (SD of percent change, number of income drops, income trajectory), thus reinforcing our conclusions. Finally, our associations were robust even after adjusting for potential confounders/mediators during the exposure period including socioeconomic, behavioral, and cardiovascular risk factors, which could potentially interfere in the relation between income volatility and cognition.
This work provides evidence of an association between income volatility and income declines with cognitive health and brain integrity in midlife. Further studies need to investigate subsequent cognitive decline and changes in brain structures to further understand its effect on cognitive aging in older age.
Glossary
- BMI
body mass index
- CARDIA
Coronary Artery Risk Development in Young Adults study
- CI
confidence interval
- CVD
cardiovascular disease
- DSST
Digit Symbol Substitution Test
- FA
fractional anisotropy
- HS
high school
- ICV
intracranial volume
- IPCW
inverse probability of censoring weights
- RAVLT
Rey Auditory Verbal Learning Test
- SBP
systolic blood pressure
- SES
socioeconomic status
Appendix. Authors

Footnotes
Editorial, page 873
Study funding
Supported by grants from the NIH, National Institute on Aging (NIA) K01AG047273. The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201800003I, HHSN268201800004I, HHSN268201800005I, HHSN268201800006I, and HHSN268201800007I from the National Heart, Lung, and Blood Institute (NHLBI). CARDIA was also partially supported by the Intramural Research Program of the NIA and an intra-agency agreement between NIA and NHLBI (AG0005). This manuscript has been reviewed and approved by CARDIA P&P for scientific content.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Dynana KE, Elmendorf DW, Sichel DE. The evolution of household income volatility. Washington, DC: Federal Reserve Board; 2007. [Google Scholar]
- 2.Hardy B. Income instability and the response of the safety net. Contemp Econ Pol 2017;35:312–330. [Google Scholar]
- 3.The Pew Charitable Trusts. How income volatility interacts with American families’financial security. 2017. Available at: www.pewtrusts.org/-/media/assets/2017/03/incomevolatility_and_financialsecurity.pdf. Accessed July 31, 2018. [Google Scholar]
- 4.Basu S. Income volatility: a preventable public health threat. Am J Public Health 2017;107:1898–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Subramanian SV, Kawachi I. Income inequality and health: what have we learned so far? Epidemiol Rev 2004;26:78–91. [DOI] [PubMed] [Google Scholar]
- 6.Lynch J, Smith GD, Harper S, et al. Is income inequality a determinant of population health? Part 1: a systematic review. Milbank Q 2004;82:5–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dowd JB, Albright J, Raghunathan TE, Schoeni RF, Leclere F, Kaplan GA. Deeper and wider: income and mortality in the USA over three decades. Int J Epidemiol 2011;40:183–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pool LR, Burgard SA, Needham BL, Elliott MR, Langa KM, Mendes de Leon CF. Association of a negative wealth shock with all-cause mortality in middle-aged and older adults in the United States. JAMA 2018;319:1341–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prause J, Dooley D, Huh J. Income volatility and psychological depression. Am J Community Psychol 2009;43:57–70. [DOI] [PubMed] [Google Scholar]
- 10.Rohde N, Tang KK, Osberg L, Rao P. The effect of economic insecurity on mental health: recent evidence from Australian panel data. Soc Sci Med 2016;151:250–258. [DOI] [PubMed] [Google Scholar]
- 11.Matthews KA, Kiefe CI, Lewis CE, et al. Socioeconomic trajectories and incident hypertension in a biracial cohort of young adults. Hypertension 2002;39:772–776. [DOI] [PubMed] [Google Scholar]
- 12.Elfassy T, Swift SL, Glymour MM, et al. Associations of income volatility with incident cardiovascular disease and all-cause mortality in a US cohort: 1990 to 2015. Circulation 2019;139:850–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marden JR, Tchetgen Tchetgen EJ, Kawachi I, Glymour MM. Contribution of socioeconomic status at 3 life-course periods to late-life memory function and decline: early and late predictors of dementia risk. Am J Epidemiol 2017;186:805–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haan MN, Zeki Al-Hazzouri A, Aiello AE. Life-span socioeconomic trajectory, nativity, and cognitive aging in Mexican Americans: the Sacramento Area Latino Study on Aging. J Gerontol B Psychol Sci Soc Sci 2011;66(suppl 1):i102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lynch JW, Kaplan GA, Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med 1997;337:1889–1895. [DOI] [PubMed] [Google Scholar]
- 16.Karlamangla AS, Miller-Martinez D, Aneshensel CS, Seeman TE, Wight RG, Chodosh J. Trajectories of cognitive function in late life in the United States: demographic and socioeconomic predictors. Am J Epidemiol 2009;170:331–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeki Al Hazzouri A, Haan MN, Kalbfleisch JD, Galea S, Lisabeth LD, Aiello AE. Life-course socioeconomic position and incidence of dementia and cognitive impairment without dementia in older Mexican Americans: results from the Sacramento Area Latino Study on Aging. Am J Epidemiol 2011;173:1148–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee S, Buring JE, Cook NR, Grodstein F. The relation of education and income to cognitive function among professional women. Neuroepidemiology 2006;26:93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaplan GA, Turrell G, Lynch JW, Everson SA, Helkala EL, Salonen JT. Childhood socioeconomic position and cognitive function in adulthood. Int J Epidemiol 2001;30:256–263. [DOI] [PubMed] [Google Scholar]
- 20.Osler M, Avlund K, Mortensen EL. Socio-economic position early in life, cognitive development and cognitive change from young adulthood to middle age. Eur J Public Health 2013;23:974–980. [DOI] [PubMed] [Google Scholar]
- 21.Turrell G, Lynch JW, Kaplan GA, et al. Socioeconomic position across the lifecourse and cognitive function in late middle age. J Gerontol B Psychol Sci Soc Sci 2002;57:S43–S51. [DOI] [PubMed] [Google Scholar]
- 22.Zeki Al Hazzouri A, Elfassy T, Sidney S, Jacobs D, Perez Stable EJ, Yaffe K. Sustained economic hardship and cognitive function: the Coronary Artery Risk Development in Young Adults study. Am J Prev Med 2017;52:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Launer LJ. The epidemiologic study of dementia: a life-long quest? Neurobiol Aging 2005;26:335–340. [DOI] [PubMed] [Google Scholar]
- 24.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41:1105–1116. [DOI] [PubMed] [Google Scholar]
- 25.Elfassy T, Glymour MM, Kershaw KN, et al. Association between sustained poverty and changes in body mass index from 1990 to 2015: the Coronary Artery Risk Development in Young Adults study. Am J Epidemiol 2018;187:1240–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dynan K, Elmendorf D, Sichel D. The evolution of household income volatility. BE J Econ Anal Pol 2012;12:1–42. [Google Scholar]
- 27.CPI Inflation Calculator. Bureau of Labor Statistics. United States Department of Labor. Available at: www.bls.gov/data/inflation_calculator.htm. Accessed June 1, 2015. [Google Scholar]
- 28.Rosenberg SJ, Ryan JJ, Prifitera A. Rey Auditory-Verbal Learning Test performance of patients with and without memory impairment. J Clin Psychol 1984;40:785–787. [DOI] [PubMed] [Google Scholar]
- 29.Weschler D. Wechsler Adult Intelligence Scale-III (WAIS-III). San Antonio, TX: Psychological Corporation; 1997. [Google Scholar]
- 30.MacLeod CM. Half a century of research on the Stroop effect: an integrative review. Psychol Bull 1991;109:163–203. [DOI] [PubMed] [Google Scholar]
- 31.Launer LJ, Lewis CE, Schreiner PJ, et al. Vascular factors and multiple measures of early brain health: CARDIA brain MRI study. PLoS One 2015;10:e0122138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.SAS Software [computer program]. Cary, NC: SAS Institute Inc.; 2012. [Google Scholar]
- 33.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med 1997;44:809–819. [DOI] [PubMed] [Google Scholar]
- 34.Yang S, Lynch JW, Raghunathan TE, Kauhanen J, Salonen JT, Kaplan GA. Socioeconomic and psychosocial exposures across the life course and binge drinking in adulthood: population-based study. Am J Epidemiol 2007;165:184–193. [DOI] [PubMed] [Google Scholar]
- 35.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med 2008;34:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anstey KJ, von Sanden C, Salim A, O'Kearney R. Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol 2007;166:367–378. [DOI] [PubMed] [Google Scholar]
- 37.Sabia S, Fayosse A, Dumurgier J, et al. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 2018;362:k2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav 2006;47:17–31. [DOI] [PubMed] [Google Scholar]
- 39.Brunner E. Stress and the biology of inequality. BMJ 1997;314:1472–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aggarwal NT, Wilson RS, Beck TL, et al. Perceived stress and change in cognitive function among adults 65 years and older. Psychosom Med 2014;76:80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johansson L, Guo X, Waern M, et al. Midlife psychological stress and risk of dementia: a 35-year longitudinal population study. Brain 2010;133:2217–2224. [DOI] [PubMed] [Google Scholar]
- 42.Towne SD, Probst JC, Hardin JW, Bell BA, Glover S. Health & access to care among working-age lower income adults in the great recession: disparities across race and ethnicity and geospatial factors. Soc Sci Med 2017;182:30–44. [DOI] [PubMed] [Google Scholar]
- 43.Bartfeld J, Gundersen C, Smeeding T, Ziliak J. SNAP Matters: How Food Stamps Affect Health and Well-Being. 1st ed. Stanford, CA: Stanford University Press; 2015. [Google Scholar]
- 44.Zahodne LB, Stern Y, Manly JJ. Differing effects of education on cognitive decline in diverse elders with low versus high educational attainment. Neuropsychology 2015;29:649–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Foubert-Samier A, Catheline G, Amieva H, et al. Education, occupation, leisure activities, and brain reserve: a population-based study. Neurobiol Aging 2012;33:423 e415–425. [DOI] [PubMed] [Google Scholar]
- 46.Mitman K, Rabinovich S. Optimal unemployment insurance in an equilibrium business-cycle model. J Monetary Econ 2015;71:99–118. [Google Scholar]
- 47.Mendenhall R, Edin K, Crowley S, et al. The role of earned income tax credit in the budgets of low-income households. Soc Serv Rev 2012;86:367–400. [Google Scholar]
- 48.Blundell R, Pistaferri L. Income volatility and household consumption: the impact of food assistance programs. J Hum Resour 2003;38:1032–1050. [Google Scholar]
- 49.Cylus J, Glymour MM, Avendano M. Health effects of unemployment benefit program generosity. Am J Public Health 2015;105:317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rehkopf DH, Strully KW, Dow WH. The short-term impacts of Earned Income Tax Credit disbursement on health. Int J Epidemiol 2014;43:1884–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
CARDIA facilitates data sharing through formal data use agreements. Any investigator is welcome to access the CARDIA data through this process.