Abstract
Current study was to evaluate the prevalence of guideline recommended medications adherence in myocardial infarction (MI) patients postpercutaneous coronary intervention (PCI) and the association of medication nonadherence and major adverse cardiovascular events (MACEs).
MI patients who underwent PCI in the last 12 months were enrolled. Demographic and clinical characteristics were collected and guideline recommended medications were evaluated. Patients were divided into with and without MACEs groups.
Compared to patients without MACEs, those with MACEs were older (54.8 ± 16.4 vs 51.1 ± 15.2 years), more likely to be smoker (40.2% vs 31.9%), have higher body mass index (BMI; 25.0 ± 6.1 vs 23.8 ± 5.7 kg/m2), diabetes (47.5% vs 37.8%), ischemic stroke (34.4% vs 25.6%), and estimated lower glomerular filtration rate (85.4 ± 9.6 vs 92.6 ± 10.7 mL/minute/1.73 m2). Patients with MACEs were also more likely to present with ST-elevation MI (STEMI; 54.1% vs 48.4%) and to undergo urgent PCI (62.3% vs 56.3%). Furthermore, patients with MACEs were less likely to adhere to dual antiplatelet therapy (77.9% vs 85.9%), renin−angiotensin system inhibitor (62.3% vs 69.7%), and beta-blocker (69.7% vs 72.8%) treatment. In unadjusted model, medication nonadherence was associated with 2-fold higher odds of MACEs. After adjustment for demographics, risk factors, comorbidities, and peri-PCI characteristics, medications nonadherence remained independently associated with MACEs, with odds ratio of 1.40 (95% confidence interval: 1.29–1.87).
Medications adherence rate among MI patients post-PCI is suboptimal in China, which is independently associated with MACEs.
Keywords: medications adherence, myocardial infarction, percutaneous coronary intervention
1. Introduction
Myocardial infarction (MI) is one of the leading causes of morbidity and mortality around the world.[1–5] In the past decades, with the advancement of percutaneous coronary intervention (PCI), numerous patients survive MI through undergoing urgent and successful coronary artery revascularization.[6–8] However, a substantial proportion of MI patients would experience recurrent MI or develop congestive heart failure after discharge.[9–12] Therefore, how to improve long-term prognosis of these populations is clinically relevant and important.
In accordance to the guideline recommendations,[13] MI patients post-PCI should take at least 12 months dual antiplatelet therapy (DAPT), lifelong statins, angiotensin converting enzyme inhibitor or angiotensin receptor blocker (ACEI/ARB), and beta-blocker. Nevertheless, prior observational studies show that a substantial proportion of MI patients did not adhere to the guideline recommended medications therapy,[14–17] and these patients had poorer prognosis than those who adhered to medications therapy.[18–20]
Notably, most of prior studies were conducted in Caucasian populations and the data on Chinese MI patients is scare. Herein, we aimed to evaluate the prevalence of guideline recommended medications adherence in MI patients post-PCI in our hospital. In addition, we evaluate the association of nonadherence to guideline recommended medications and major adverse cardiovascular events (MACEs). Hopefully, results from our current study can provide clues to improve medications adherence and improve prognosis of MI patients after PCI therapy in the future.
2. Methods
2.1. Participants’ enrollment
The protocol of current study was approved by the Research Ethic Committee of Qianfoshan Hospital of Shandong University, and informed consent was obtained from participants before enrollment. The inclusion criteria were as follows: prior PCI was underwent at our hospital, prior PCI was performed within the last 12 months due to MI, and patients were follow-up at our hospital with intact information of follow-up medications prescription; and the exclusion criteria were as follows: patients underwent PCI due to other reasons (eg, stable angina), patients had contraindications to guideline recommended medications (eg, angioedema due to ACEI/ARB), or patients underwent PCI more than 12 months ago who was reasonable to discontinue DAPT.
2.2. Demographic, risk factors, and comorbidities collection
Demographics included age and sex, and body mass index (BMI) was calculated by weight in kilogram divided by height in squared meters. Risk factors included history of smoking, hypertension, dyslipidemia, and diabetes. Comorbidities included history of ischemic stroke, peripheral arterial disease, and chronic kidney disease. All these data were collected from electronic medical record.
2.3. Laboratory data
Fasting venous blood was drawn for evaluation of serum levels of fasting plasma glucose, low-density lipoprotein-cholesterol, alanine aminotransferase, and creatinine. Serum creatinine level was used to calculate estimated glomerular filtration rate based on the MDRD formula.[21]
2.4. Characteristics of peri-PCI
Characteristics of peri-PCI including presentation as ST-elevation MI (STEMI) or non-STEMI, underwent urgent or elective PCI, peri-PCI antiplatelet drug loading, and the number and type of stent implanted were documented from electronic medical record. In specific, all these peri-PCI characteristics were collected after patients were enrolled in our current study.
2.5. Medications adherence evaluation
Medications adherence evaluation was based on the outpatient medication prescription system and inpatient medical record system, which allowed us to evaluate the prescription, refill, and change of medications. Medication adherence was evaluated by 2 independent investigators, and patients who did not get medications refill longer than 7 days were considered as medication nonadherence.
2.6. Assessment of MACEs
MACEs in our current study was defined as composite of angina symptoms, MI, targeted vessel revascularization (TVR), and new onset of congestive heart failure. All the outcomes were documented and adjudicated by 2 independent cardiologists.
2.7. Statistical analysis
Continuous variables were presented as mean ± SD and compared by Student t test; categorical variables were presented by proportion and number and compared by the chi-square or Fisher exact test for categorical variables. Logistic regression analyses were performed to evaluate the associations of medications nonadherence and MACEs. Statistical analyze were computed using SPSS 19.0 (SPSS Inc, Chicago, IL). All statistical tests were 2-sided and considered statistically significant when P < .05.
3. Results
3.1. Participants’ enrollment
A total of 648 MI patients were encountered during January of 2018 to December of 2018 at the outpatient department of our hospital. After exclusion of 206 patients, 442 patients were enrolled and divided into with (n = 122) and without (n = 320) MACEs groups (Fig. 1). Among the 122 patients with MACEs, 45 (36.9%), 17 (13.9%), 6 (4.9%), and 54 (44.3%) had experienced angina, MI, TVR, and congestive heart failure post-PCI, respectively.
Figure 1.
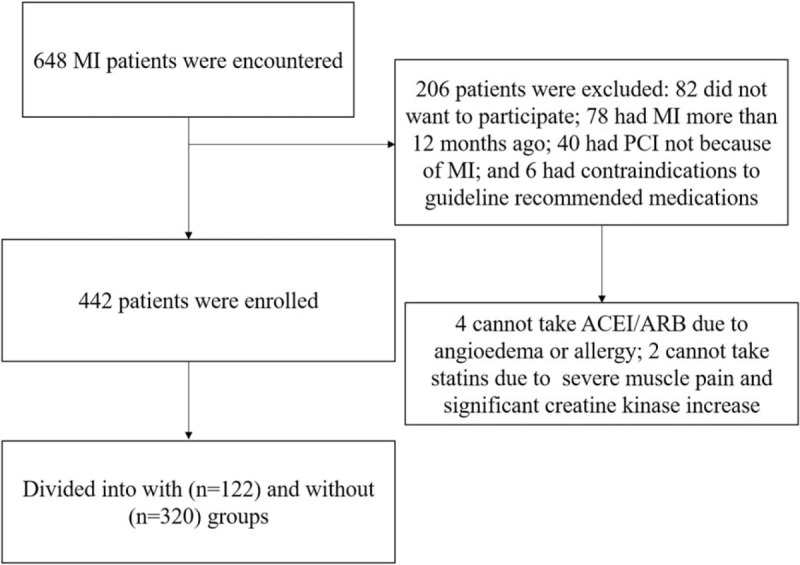
Study flowchart.
3.2. Baseline characteristics comparisons
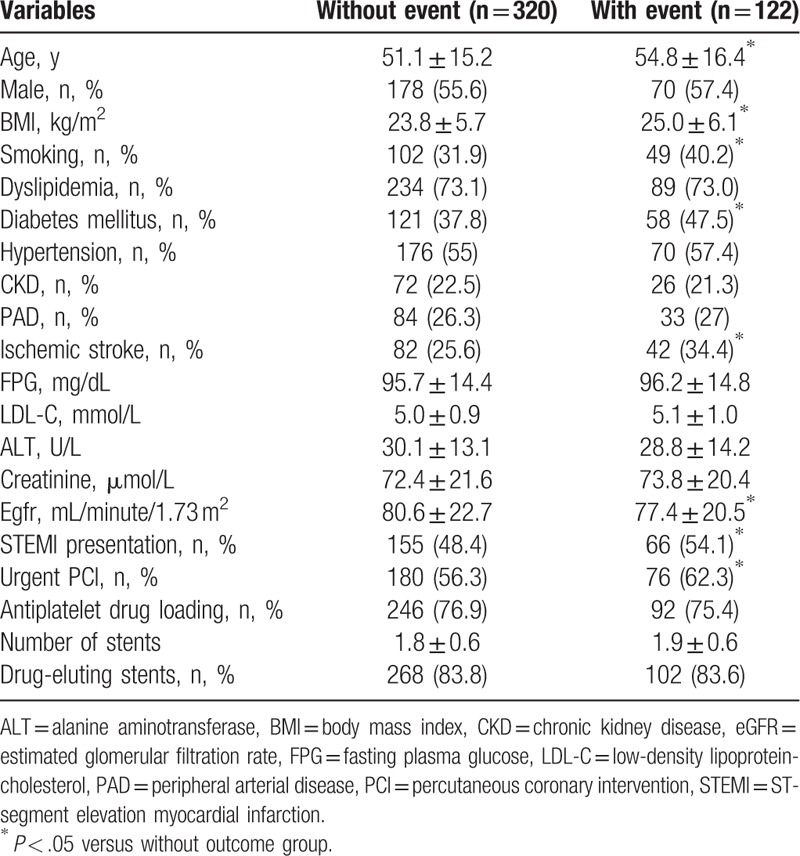
Baseline characteristics were compared and as presented in Table 1, compared to patients without MACEs, those with MACEs were older (54.8 ± 16.4 vs 51.1 ± 15.2 years), more likely to be smoker (40.2% vs 31.9%), have higher BMI (25.0 ± 6.1 vs 23.8 ± 5.7 kg/m2), diabetes (47.5% vs 37.8%), ischemic stroke (34.4% vs 25.6%), and lower estimated glomerular filtration rate (85.4 ± 9.6 vs 92.6 ± 10.7 mL/minute/1.73 m2). In addition, patients with MACEs were also more likely to present with STEMI (54.1% vs 48.4%) and to undergo urgent PCI (62.3% vs 56.3%).
Table 1.
Baseline characteristics comparisons.
3.3. Guideline recommended medications adherence comparisons
At the time of participant's enrollment, adherence to guideline recommended medications was evaluated. As presented in Figure 2, the prevalence of overall adherence to guideline recommended medications in our study's population was 83.7% (DAPT), 67.6% (ACEI/ARB), 81.8% (statins), and 71.9% (beta-blocker), respectively.
Figure 2.
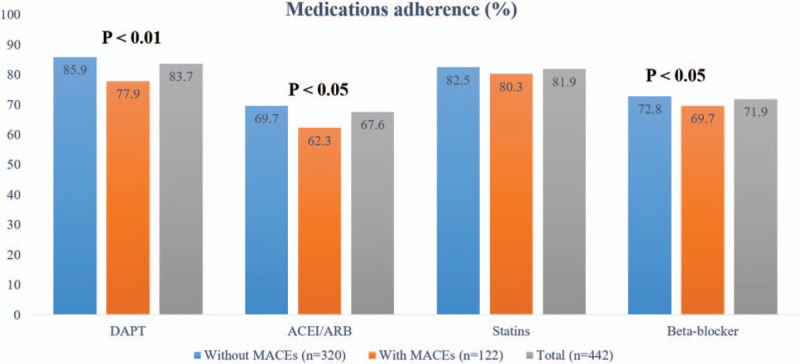
Medications adherence evaluation. ACEI/ARB = angiotensin converting-enzyme inhibitor/angiotensin receptor blocker, DAPT = dual antiplatelet therapy.
Compared to those without MACEs, patients with MACEs were less likely to adhere to DAPT (77.9% vs 85.9%), ACEI/ARB (62.3% vs 69.7%), and beta-blocker (69.7% vs 72.8%) treatment.
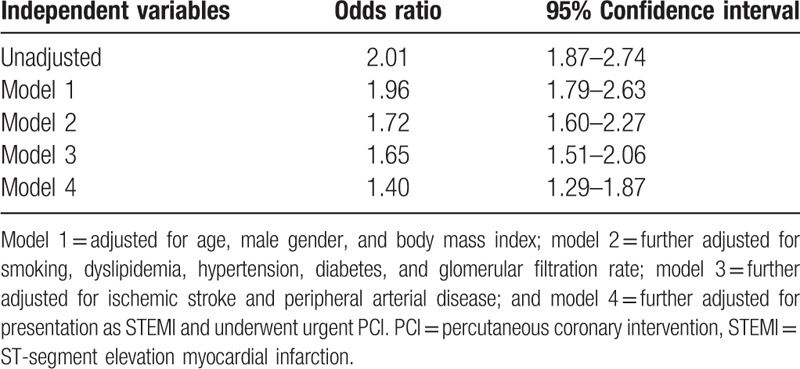
3.4. Associations of medications nonadherence and MACEs
Logistic regression analysis was conducted to evaluate the association of medication nonadherence and MACEs. As presented in Table 2, in the unadjusted model, medication nonadherence was associated with 2-fold higher odds of MACEs. After adjustment for demographics, the associations were attenuated slightly. Although adjustment for risk factors, the odds were attenuated by 24% (from 1.96 to 1.72). In the model 3, adjustment for comorbidities also attenuated the odds slightly. However, with further adjustment for peri-PCI characteristics, the odds were attenuated by 25% (from 1.65 to 1.40). These findings together indicated that medications nonadherence was independently associated with MACEs in MI patients post-PCI therapy.
Table 2.
Associations of medication nonadherence and composite cardiovascular events.
4. Discussion
To our knowledge, the current analysis should be the first few studies to evaluate the prevalence of guideline recommended medications adherence in Chinese MI patients post-PCI therapy. Our results show that the prevalence of medications adherence was suboptimal. Compared to those without MACEs, patients with MACEs are more likely to nonadherence to guideline recommended medications therapy. In addition, after adjustment for covariates, medications nonadherence remains independently associated with MACEs.
Notably, DAPT, ACEI/ARB, statins, and beta-blocker are standard of care for MI patients post-PCI therapy. Prior randomized controlled trials have demonstrated that compared to placebo, these medications can reduce cardiovascular events and improve patients’ prognosis.[22–24] Nevertheless, numerous studies have shown that a substantial proportion of patients did not adhere to guideline recommended medications therapy and these patients were at higher risk of experiencing angina, recurrent MI, in-stent restenosis, and congestive heart failure.[25–29] These findings together demonstrate that how to improve patients’ adherence to guideline recommended medications therapy is a good opportunity to reduce health and economic burden in China.[22]
In the past decades, the incidence of MI in China increased dramatically and PCI was also routinely applied to MI patients. However, the data on guideline recommended medications adherence post-PCI therapy was scare. Our current study for the first time showed that at the first 12 months post-PCI therapy, the overall adherence to DAPT, ACEI/ARB, statins, and beta-blocker therapy was 83.7%, 67.6%, 81.8%, and 71.9%, respectively. Since we had excluded those who were contraindicative to these medications treatment, therefore, theoretically, all these patients should be necessary to take the guideline recommended medications. However, it might be possible that after PCI, some patients developed medications related side effects such as bleeding events, hypotension, or bradycardia, which resulted in premature discontinuation of these medications.
Regardless of the reason for the premature discontinuation of guideline recommended medications, our results support the notion that among MI patients post-PCI therapy, nonadherence to guideline recommended medications therapy was associated with MACEs. Our findings were consistent with prior reports. For example, Moalem et al[26] reported that approximately 1 in 10 patients disrupts DAPT due to nonadherence, which resulted in higher risk for ischemic events. Bangalore et al[27] reported that among MI patients, maintenance on beta-blocker treatment was associated with reduced risk of recurrent MI and angina symptoms. Kalsekar et al[28] reported that among MI patients, those who adhered to ACEI treatment was less likely to develop congestive heart failure than those who did not adhere to ACEI treatment. In our current analysis, through stepwise adjustment for potential covariates including demographics, risk factors, comorbidities, and peri-PCI characteristics, medication nonadherence remained independently associated with MACEs. In current study, we defined MACEs as composite of angina symptoms, MI, TVR, and congestive heart failure because these events were strongly associated with guideline recommended medications discontinuation. In specific, among the 122 patients with MACEs, 45 (36.9%), 17 (13.9%), 6 (4.9%), and 54 (44.3%) had experienced angina, MI, TVR, and congestive heart failure post-PCI, respectively. We observed that compared to those without MACEs, the rate of nonadherence to DAPT, ACEI/ARB, and beta-blocker was significantly higher in patients with MACEs. These findings collectively demonstrate that nonadherence to guideline recommended medications therapy is common in Chinese PCI patients, and concerted efforts are needed to improve patients’ adherence to guideline recommended medications therapy.
There are some limitations of our current study. First of all, this is an observational study and findings from our study cannot establish causal relationship between medications nonadherence and MACEs. However, our study provided insight into the association of medication nonadherence and MACEs in Chinese PCI patients. Second, despite we have extensively adjusted for potential covariates, unmeasured and undetected covariates remained possible to influence the association between medications nonadherence and MACEs. Last but not the least, this is a single center study and findings from our current study may not be able to extrapolate to other population groups. Further studies in China are needed to corroborate our findings.
5. Conclusion
In summary, our current study shows that guideline recommended medications adherence rate among MI patients post-PCI is suboptimal in China and medication nonadherence is independently associated with MACEs. Further studies are warranted to investigate how to improve medications adherence rate in China.
Acknowledgments
The authors thank the help of Dr James K Wang provided to authors.
Author contributions
Conceptualization: Yunfeng Hou, Shumin Jiang.
Data curation: Yunfeng Hou, Yifeng Yue, Meiling Zhao.
Formal analysis: Yifeng Yue.
Funding acquisition: Yunfeng Hou, Shumin Jiang.
Methodology: Meiling Zhao.
Resources: Yifeng Yue, Meiling Zhao.
Supervision: Meiling Zhao, Shumin Jiang.
Validation: Yifeng Yue, Meiling Zhao, Shumin Jiang.
Writing – original draft: Yunfeng Hou.
Writing – review & editing: Shumin Jiang.
Footnotes
Abbreviations: ACEI/ARB = angiotensin converting enzyme inhibitor or angiotensin receptor blocker, DAPT = dual antiplatelet therapy, MACE = major adverse cardiovascular event, MI = myocardial infarction, PCI = percutaneous coronary intervention, STEMI = ST-elevation MI, TVR = targeted vessel revascularization.
How to cite this article: Hou Y, Yue Y, Zhao M, Jiang S. Prevalence and association of medication nonadherence with major adverse cardiovascular events in patients with myocardial infarction. Medicine. 2019;98:44(e17826).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Li J, Li X, Wang Q, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet 2015;385:441–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Joshi P, Islam S, Pais P, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007;297:286–94. [DOI] [PubMed] [Google Scholar]
- [4].Paudel R, Beridze N, Aronow WS, et al. Association of chest pain versus dyspnea as presenting symptom for coronary angiography with demographics, coronary anatomy, and 2-year mortality. Arch Med Sci 2016;12:742–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ramos C, Brito R, González-Montero J, et al. Effects of a novel ascorbate-based protocol on infarct size and ventricle function in acute myocardial infarction patients undergoing percutaneous coronary angioplasty. Arch Med Sci 2017;13:558–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Chiarito M, Sardella G, Colombo A, et al. Safety and efficacy of polymer-free drug-eluting stents. Circ Cardiovasc Interv 2019;12:e007311. [DOI] [PubMed] [Google Scholar]
- [7].Sadowski M, Gutkowski W, Raczyński G, et al. Acute myocardial infarction due to left main coronary artery disease in men and women: does ST-segment elevation matter. Arch Med Sci 2015;11:1197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Yannopoulos D, Bartos JA, Aufderheide TP, et al. The evolving role of the cardiac catheterization laboratory in the management of patients with out-of-hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation 2019;139:e530–52. [DOI] [PubMed] [Google Scholar]
- [9].Cai A, Li X, Zhong Q, et al. Associations of high HDL cholesterol level with all-cause mortality in patients with heart failure complicating coronary heart disease. Medicine (Baltimore) 2016;95:e3974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013;128:e240–327. [DOI] [PubMed] [Google Scholar]
- [11].AlFaleh H, Elasfar AA, Ullah A, et al. Acute heart failure with and without acute coronary syndrome: clinical correlates and prognostic impact (from the HEARTS registry). BMC Cardiovasc Disord 2016;16:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lu Y, Cheng Z, Zhao Y, et al. Efficacy and safety of long-term treatment with statins for coronary heart disease: a Bayesian network meta-analysis. Atherosclerosis 2016;254:215–27. [DOI] [PubMed] [Google Scholar]
- [13].Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction. Circulation 2018;138:e618–51. [DOI] [PubMed] [Google Scholar]
- [14].Hirsh BJ, Smilowitz NR, Rosenson RS, et al. Utilization of and adherence to guideline-recommended lipid-lowering therapy after acute coronary syndrome: opportunities for improvement. J Am Coll Cardiol 2015;66:184–92. [DOI] [PubMed] [Google Scholar]
- [15].Huber CA, Meyer MR, Steffel J, et al. Post-myocardial infarction (MI) care: medication adherence for secondary prevention after MI in a large real-world population. Clin Ther 2019;41:107–17. [DOI] [PubMed] [Google Scholar]
- [16].Brieger D, Chow C, Gullick J, et al. Improving patient adherence to secondary prevention medications 6 months after an acute coronary syndrome: observational cohort study. Intern Med J 2018;48:541–9. [DOI] [PubMed] [Google Scholar]
- [17].Aronow WS. Lipid-lowering therapy in older persons. Arch Med Sci 2015;11:43–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Faridi KF, Peterson ED, McCoy LA, et al. Timing of first postdischarge follow-up and medication adherence after acute myocardial infarction. JAMA Cardiol 2016;1:147–55. [DOI] [PubMed] [Google Scholar]
- [19].Knežević B, Musić L, Batrićević G, et al. Optimizing prevention and guideline-concordant care in Montenegro. Int J Cardiol 2016;217Suppl:S32–6. [DOI] [PubMed] [Google Scholar]
- [20].Tra J, van der Wulp I, Appelman Y, et al. Adherence to guidelines for the prescription of secondary prevention medication at hospital discharge after acute coronary syndrome: a multicentre study. Neth Heart J 2015;23:214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and, stratification. Am J Kidney Dis 2002;392 Suppl 1:S1–266. [PubMed] [Google Scholar]
- [22].Hamood H, Hamood R, Green MS, et al. Effect of adherence to evidence-based therapy after acute myocardial infarction on all-cause mortality. Pharmacoepidemiol Drug Saf 2015;24:1093–104. [DOI] [PubMed] [Google Scholar]
- [23].Choudhry NK, Setoguchi S, Levin R, et al. Trends in adherence to secondary prevention medications in elderly post-myocardial infarction patients. Pharmacoepidemiol Drug Saf 2008;17:1189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 2007;297:177–86. [DOI] [PubMed] [Google Scholar]
- [25].Czarny MJ, Nathan AS, Yeh RW, et al. Adherence to dual antiplatelet therapy after coronary stenting: a systematic review. Clin Cardiol 2014;37:505–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Moalem K, Baber U, Chandrasekhar J, et al. Incidence, predictors, and outcomes of DAPT disruption due to non-compliance vs. bleeding after PCI: insights from the PARIS Registry. Clin Res Cardiol 2019;108:643–50. [DOI] [PubMed] [Google Scholar]
- [27].Bangalore S, Makani H, Radford M, et al. Clinical outcomes with β-blockers for myocardial infarction: a meta-analysis of randomized trials. Am J Med 2014;127:939–53. [DOI] [PubMed] [Google Scholar]
- [28].Kalsekar I, Koehler J, Mulvaney J. Impact of ACE inhibitors on mortality and morbidity in patients with AMI: does tissue selectivity matter. Value Health 2011;14:184–91. [DOI] [PubMed] [Google Scholar]
- [29].Hickson RP, Robinson JG, Annis IE, et al. Changes in statin adherence following an acute myocardial infarction among older adults: patient predictors and the association with follow-up with primary care providers and/or cardiologists. J Am Heart Assoc 2017;6: pii: e007106. [DOI] [PMC free article] [PubMed] [Google Scholar]


