Abstract
Objectives:
To compare the effectiveness and safety of epidural anesthesia (EA) with those of local anesthesia (LA) for percutaneous transforaminal endoscopic discectomy (PTED) and provide reference data for clinical decision-making.
Methods:
We searched PubMed, Embase, the Cochrane library, Web of Science, Medline, ScienceDirect, and the China National Knowledge Infrastructure from inception to June 2019 in order to identify randomized and nonrandomized controlled trials comparing EA and LA for PTED. Studies assessing at least 2 of the following indicators were eligible: surgical duration, X-ray exposure time, satisfaction rate, visual analog scale (VAS) scores for pain, Oswestry Disability Index (ODI), and complications. Two assessors evaluated the quality of the literature using the Cochrane Handbook or Newcastle–Ottawa Scale. Meta-analysis was conducted using Review Manager 5.3.3 software.
Results:
Four randomized controlled trials and 4 retrospective cohort studies involving a total of 1000 patients were included. The LA and EA groups included 473 and 527 patients, respectively. Meta-analysis revealed significant intergroup differences in the intraoperative (P < .00001) and postoperative (P < .00001) lumbar VAS scores, intraoperative (P < .00001) and postoperative (P = .001) leg VAS scores, and anesthesia satisfaction rate (P < .00001), with EA being superior to LA in all aspects. There were no significant intergroup differences in the surgical duration, X-ray exposure time, postoperative ODI, and complication rate.
Conclusion:
EA is as safe as LA and produces better anesthetic effects than does LA in patients undergoing PTED. Therefore, it should be promoted as a reliable anesthetic technique for PTED.
Keywords: epidural anesthesia, local anesthesia, lumbar disc herniation, meta-analysis, percutaneous transforaminal endoscopic discectomy
1. Introduction
Lumbar disc herniation (LDH) is considered the main cause of low back pain and sciatica.[1] When conservative treatment is not effective, surgical treatment becomes the final option for relieving pain and restoring function.[2] Of late, PTED has considerably developed because of innovative endoscopic visualization technologies and patient demands for minimally invasive techniques.[3] Its application has even been extended to the treatment of lumbar spinal stenosis and adjacent segmental degeneration after lumbar fusion, with good outcomes.[4,5] In order to minimize the risk of nerve root injury during PTED, awareness and certain motor functions of patients need to be maintained so that the surgeon can communicate with them during the procedure. Therefore, many clinicians prefer to perform PTED under local anesthesia (LA).[6] However, pain control is poor with LA, particularly during expansion of the intervertebral foramen and insertion of the working channel. Some patients are even compelled to give up treatment because they cannot tolerate the pain.[7] In such cases, epidural anesthesia (EA), which involves blockade of the spinal nerve roots below the puncture plane via injection of local anesthetic into the epidural cavity through puncture catheterization, can be used. EA provides good analgesic effects in the surgical area while keeping the patient awake, and it has become a new choice of anesthesia for PTED.[8] However, evidence-based medical evidence regarding the superiority of EA over LA is lacking. Accordingly, we conducted a meta-analysis to compare the effectiveness and safety of EA with those of LA for PTED and provide reference data for clinical decision-making.
2. Materials and methods
2.1. Search strategy
We searched PubMed, Embase, the Cochrane library, Web of Science, Medline, ScienceDirect, and the China National Knowledge Infrastructure from inception to June 2019 and retrieved studies comparing EA and LA for PTED. The search terms included “PTED” or “percutaneous transforaminal endoscopic discectomy” or “transforaminal endoscopic spine system surgery” or “TESSYS,” “EA” or “epidural anesthesia,” and “local anesthesia” or “LA”.
Ethical approval was not necessary because this was a systematic review and meta-analysis based on published data.
2.2. Inclusion criteria
Clinical studies involving adult subjects without a history of lumbar fusion surgery who were treated with PTED were considered eligible. All studies assessed at least 2 of the following parameters: surgical duration, X-ray exposure time, satisfaction with anesthesia, visual analog scale (VAS) scores, Oswestry Disability Index (ODI), and complications.
2.3. Exclusion criteria
Reviews, animal studies, and case reports; studies involving percutaneous endoscopic surgery via nonintervertebral approaches; studies including patients with severe trauma, infection, or tumors; and studies presenting data that were incomplete and/or could not be extracted were excluded.
2.4. Date extraction
Data was extracted and checked by 2 researchers. The extracted data included author names, the publication year, the type of study, the sample size, age, sex, types and doses of anesthetic drugs, the surgical duration, the X-ray exposure time, VAS scores, ODI, rate of satisfaction with anesthesia, and complication rates.
2.5. Data analysis and statistical methods
All data were subjected to meta-analysis using Review Manager software (version 5.3.3, Cochrane Collaboration). Statistical heterogeneity was assessed by Chi-squared and I2 tests. If the I2 value was >50%, the data were considered to be significantly heterogeneous. A random-effects model was used when significant heterogeneity was observed; otherwise, a fixed effects model was used. Continuous data are represented by mean differences (MDs) and 95% confidence intervals (CIs) while dichotomous data are represented by risk ratios (RRs) and 95% CIs. A P value of <.05 was considered statistically significant.
2.6. Quality assessment
Two researchers independently evaluated the quality of the literature. In case of disagreement, a third party was consulted and a judgment was made. Randomized controlled trials (RCTs) and cohort studies were evaluated using the Cochrane risk-of-bias tool and Newcastle–Ottawa scale, respectively. The authors, institutions, journals, and other relevant information were hidden during the evaluation process in order to avoid subjective experimenter bias that could influence the results.
3. Results
3.1. Search results
A total of 259 studies were retrieved. After elimination of duplicates, 66 studies remained. From these, 47 irrelevant studies were excluded after review of the abstracts. The full text of the remaining 19 studies was evaluated, and studies with missing data were excluded. Eventually, 8 studies were considered eligible for meta-analysis.[3,6–12] The literature screening and study selection flowchart is illustrated in Figure 1.
Figure 1.
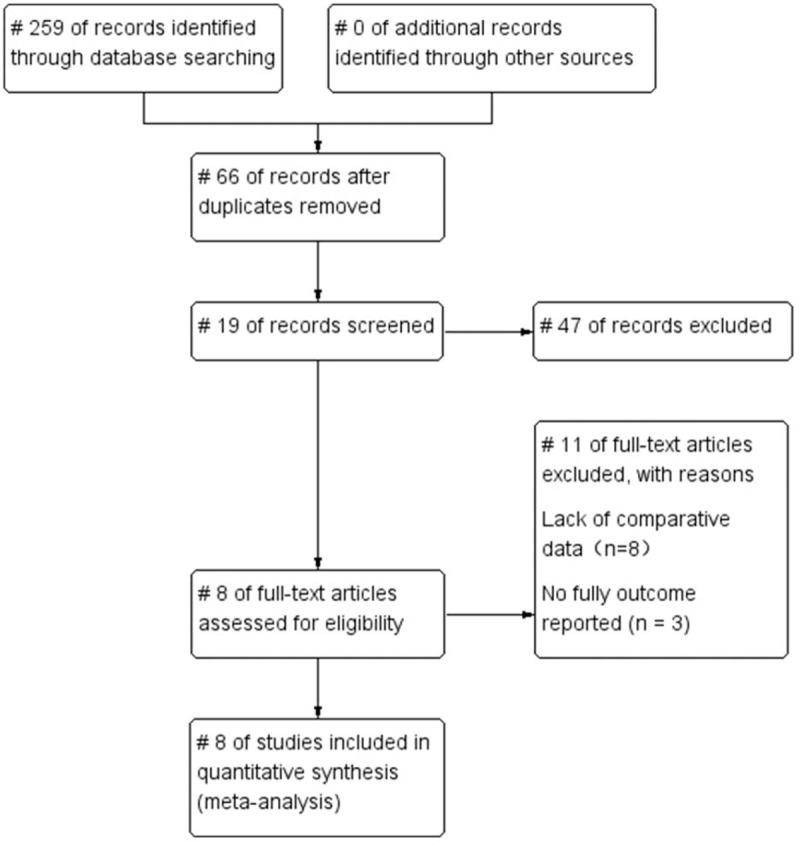
Study flowchart for a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
3.2. Study characteristics
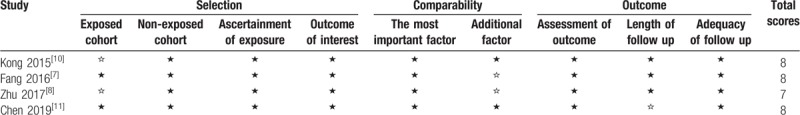
The included studies were published between 2015 and 2019. There were 4 RCTs[3,6,9,12] and 4 retrospective cohort studies[7,8,10,11] with a total of 1000 patients. The LA and EA groups comprised 473 and 527 patients, respectively. The study characteristics are shown in Table 1. The results of the quality evaluation are listed in Figure 2 and Table 2.
Table 1.
Characteristics of studies included in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
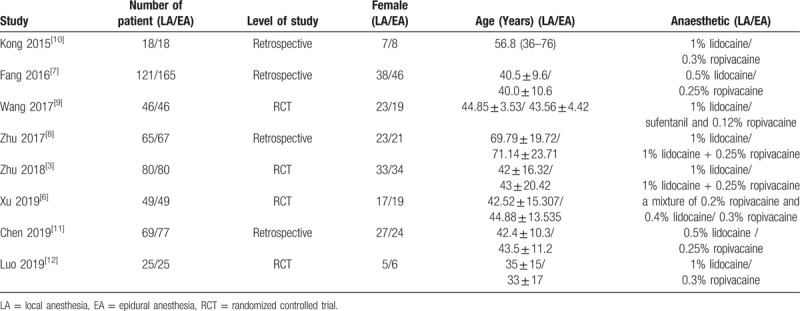
Figure 2.
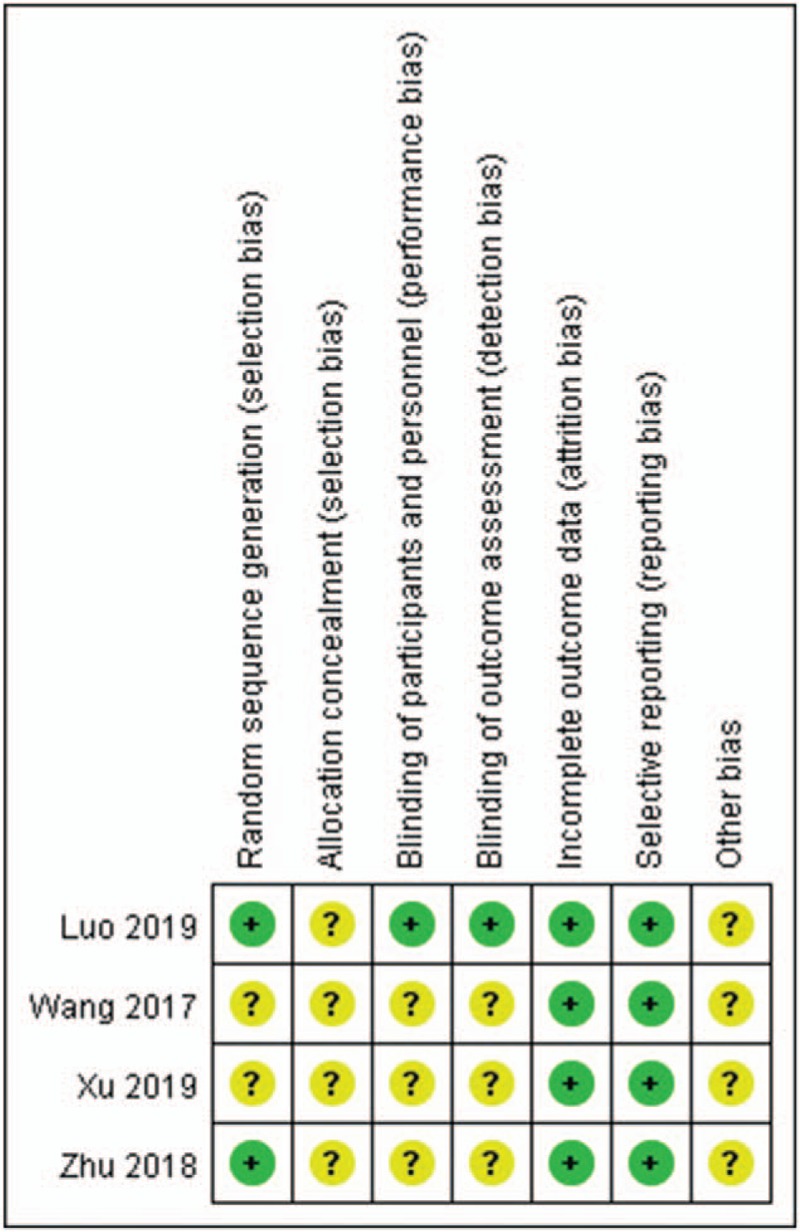
Risk of bias assessment using the Cochrane risk-of -bias tool for randomized controlled trials included in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
Table 2.
Risk of bias assessment using the Newcastle–Ottawa Scale for cohort studies included in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
3.3. Outcomes of meta-analysis
3.3.1. VAS score for lumbar pain
Intra-and postoperative VAS scores for lumbar pain were analyzed in 3 studies including 191 patients in the LA group and 196 patients in the EA group. Both intra- (P < .00001; MD, 4.56; 95%CI, 3.15–5.97; I2 = 99%) and postoperative (P < .00001; MD, 1.87; 95%CI, 1.01–2.73; I2 = 100%; Figure 3) scores were significantly lower in the EA group than in the LA group.
Figure 3.
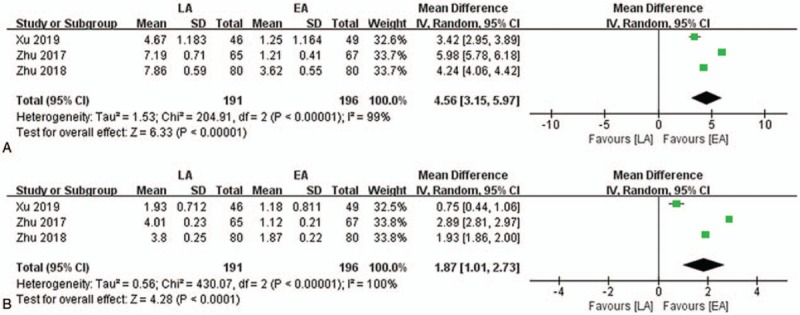
Forest plot of visual analog scale (VAS) scores for lumbar pain in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy. (A) intraoperative VAS score, (B) postoperative VAS score.
3.3.2. VAS score for leg pain
Intraoperative VAS scores for leg pain were analyzed in 5 studies including 285 and 298 patients in the LA and EA groups, respectively, while postoperative VAS scores for leg pain were also analyzed in 5 studies including 232 and 239 patients in the LA and EA groups, respectively. Both intra- (P < .00001; MD, 3.86; 95%CI, 2.90–4.82; I2 = 98%) and postoperative (P = .001; MD, 0.95; 95%CI, 0.38–1.53; I2 = 97%; Fig. 4) scores were significantly lower in the EA group than in the LA group.
Figure 4.
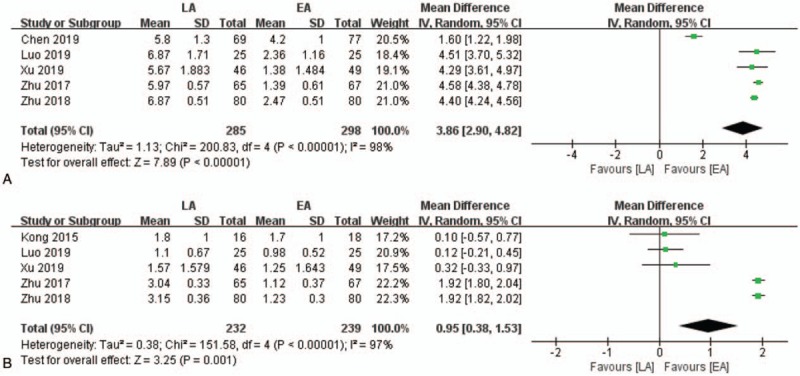
Forest plot of visual analog scale (VAS) scores for leg pain in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy. (A) intraoperative VAS score, (B) postoperative VAS score.
3.3.3. Postoperative ODI
The postoperative ODI was evaluated in 6 studies including 397 patients in the LA group and 453 patients in the EA group. There was no significant difference between the LA and EA groups (P = .61; MD, 0.21; 95%CI, −0.60–1.03; I2 = 66%; Fig. 5).
Figure 5.
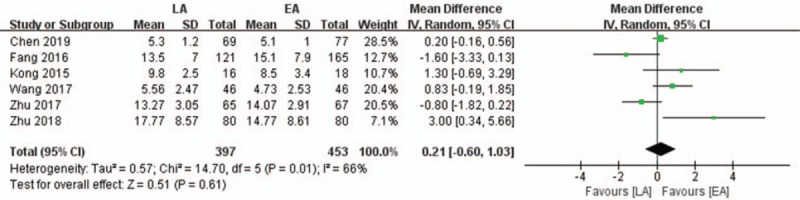
Forest plot of postoperative Oswestry Disability Index (ODI) in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
3.3.4. Rate of satisfaction with anesthesia
The number of patients who were satisfied with anesthesia was evaluated in 4 studies including 284 patients in the LA group and 330 patients in the EA group. The rate of satisfaction with EA was significantly higher than the rate of satisfaction with LA (P < .00001; RR, 0.81; 95%CI, 0.75– 0.88; I2 = 39%; Fig. 6).
Figure 6.
Forest plot of rates of satisfaction with anesthesia in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
3.3.5. Surgical duration
The surgical duration was analyzed in 4 studies including 207 and 214 patients in the LA and EA groups, respectively. There was no significant difference between the LA and EA groups (P = .70; MD, 3.85; 95%CI, −16.00 to 23.71; I2 = 98%; Fig. 7).
Figure 7.
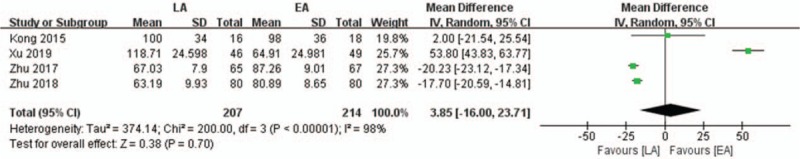
Forest plot of surgical durations in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
3.3.6. Fluoroscopy duration
The fluoroscopy duration was analyzed in only 2 studies (145 patients in the LA group and 147 patients in the EA group), with no significant difference between the 2 groups (P = .13; MD, 2.83; 95%CI, −0.85–6.51; I2 = 94%; Fig. 8).
Figure 8.
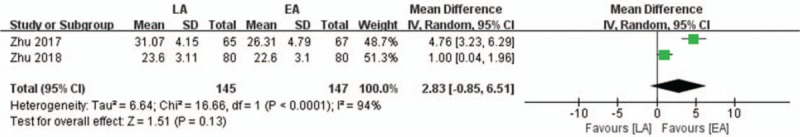
Forest plot of fluoroscopy durations in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
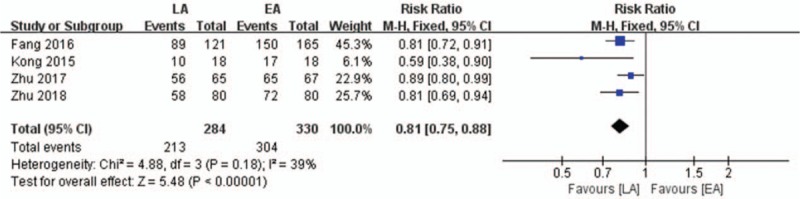
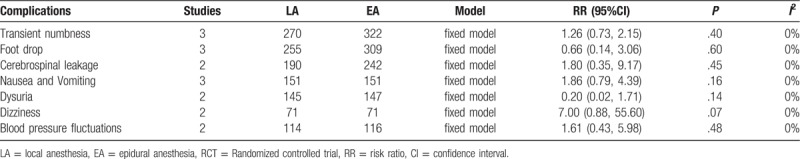
3.3.7. Complications
Complications were documented in all 8 studies. There was no significant difference in the total complication rate between the LA and EA groups (P = .45; RR, 1.29; 95%CI, 0.66–2.52; I2 = 57%; Fig. 9). Individual complications were also assessed, and no intergroup difference was found (Table 3).
Figure 9.
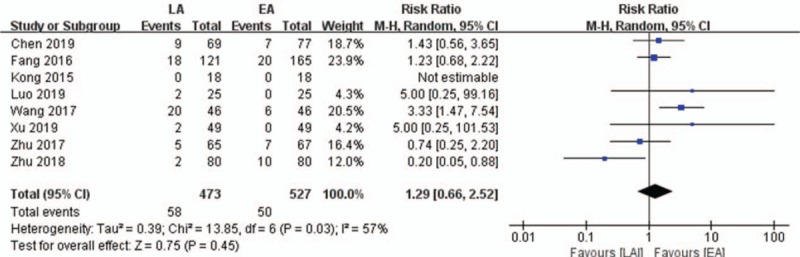
Forest plot of total complication rates in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
Table 3.
Analysis of individual complications recorded in studies included in a meta-analysis on the efficacy and safety of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy.
3.4. Sensitivity analysis and publication bias
To confirm the stability of the meta-analysis, sensitivity analysis was utilized to sequentially omit the content included in each article. No significant change was observed in the results after the exclusion of any single study; thus, the stability of the results was credible. Because of the limited number of studies (<10), the statistical reliability of the funnel plot asymmetry test for distinguishing chance from real asymmetry was considered too low, and publication bias was not assessed.
4. Discussion
Through the present meta-analysis, we found that EA is a superior anesthetic technique when compared with LA for PTED, with equivalent safety. To the best of our knowledge, this is the first meta-analysis on the efficacy and safety of EA and LA for PTED.
The intervertebral foramen is a natural channel between the vertebral bodies. During PTED, the spinal canal is penetrated through the intervertebral foramen for effective release and decompression of the nerve roots. Patients who receive PTED exhibit faster postoperative recovery because the procedure avoids paravertebral muscle dissection and damage to the posterior structure of the lumbar spine. Of late, PTED has become a common treatment for LDH.[13,14] Inufusa et al performed sectional autopsy and computed tomography and observed that the height of the intervertebral disc in the sagittal position decreased by different degrees in the presence of dehydration and degeneration of the nucleus pulposus. Moreover, the superior articular process of the lower vertebral body in the lesion segment was displaced in the ventral and cephalad directions, which resulted in narrowing of the intervertebral foramen.[15] Therefore, in PTED, foraminoplasty is necessary for enlargement of the intervertebral foramen in the diseased segment. This facilitates smooth insertion of the working channel into the spinal canal and simultaneous enlargement of the surgical space under the microscope.[16] Considering the presence of numerous nerves and blood vessels in the intervertebral foramen and the fact that foraminoplasty cannot be performed under direct vision, clinicians generally opt to complete the surgery under LA in order to ensure appropriate intraoperative communication with the patient and minimize the probability of collateral nerve damage.[17]
However, LA is not effective in controlling the pain caused by foraminoplasty and nerve root traction, and some patients forego the procedure because they cannot tolerate the pain.[7] Therefore, it is sometimes necessary to increase the use of opioid analgesics with LA, which results in increased adverse reactions such as nausea and vomiting.[18] On the other hand, painful stimuli can increase the heart rate and blood pressure, consequently increasing the surgical risk in patients with high blood pressure and/or coronary heart disease.[6] Taking these factors in account, some investigators use anesthesia techniques such as EA, spinal-EA, and general anesthesia.[19,20] However, the sensory and motor functions of the lower limbs are completely inhibited under spinal anesthesia and general anesthesia; consequently, accidental injury to nerve roots during the separation of adhesions and exposure of intervertebral discs cannot be easily detected.
EA with low concentrations of ropivacaine produces an excellent sensory–motor block separation effect, which effectively blocks sensory transmission with little effect on the motor nerves. As a result, the surgeon can determine whether nerve root damage has occurred by observing the movement of the patient's limbs in awake and pain-free conditions.[3] Luo et al performed PTED under EA with 15 ml of 0.3% ropivacaine in 25 patients, all of whom exhibited a modified Bromage score of 0 and no motor blockade.[12] Ropivacaine has low central nervous system toxicity and cardiotoxicity and is currently the safest long-acting local anesthetic for clinical applications.[21] In cases where the surgeons are not skilled enough or the surgical duration is too long, appropriate dosages of ropivacaine can be added as required through the epidural catheter.
We attempted to address 2 important questions in the present study: “can EA completely replace LA for PTED? and “how does EA compare with LA in terms of efficacy and safety? In Fang's study, epidural anesthesia was associated with a higher satisfaction rate, and there was no significant difference in neurological complications between EA and LA.[7] In contrast, Zhu reported that EA can result in more complications while exhibiting a superior analgesic effect.[3]
Anesthesia is used for pain control during surgery and ensures that the procedure is smoothly completed. Accordingly, VAS was considered an appropriate tool for evaluating and comparing the pain-relieving effects of the 2 anesthetic techniques during surgery. In the present meta-analysis, intraoperative VAS scores for lumbar pain and leg pain were significantly lower in the EA group than in the LA group. In Kong study, 2 cases in the LA group could not tolerate the pain and were switched to EA for completion of the procedure.[10] In Xu study, 1 patient in the LA group could not tolerate the pain, while another developed respiratory alkalosis because of severe intraoperative pain, necessitating termination of the surgery. In yet another patient, the blood pressure increased to 200/170 mm Hg because of intraoperative pain stimulation, necessitating emergency suspension of the surgery.[6] These findings suggest that EA achieves better pain control during PTED than does LA, facilitating smooth operation and increasing the success rate.
Postoperative VAS scores for lumbar pain and leg pain were also significantly lower in the EA group than in the LA group. It should be noted that VAS scores would have been recorded at different time points after surgery in different studies. In some studies, VAS was even recorded at multiple time points after surgery. For our meta-analysis, we selected the first scores obtained after surgery in all studies, although the differences in the timing of VAS assessments may have some influence on our results.
We found that a significantly larger number of patients was satisfied with EA than with LA. This indicates that EA increases patient comfort during surgery. In addition, 2 studies documented postoperative satisfaction using the Macnab criteria and found a higher number of patients with “excellent” and “good” ratings in the EA group, although the difference between the LA and EA groups was not statistically significant.[3,8]
ODI is widely used to evaluate the degree of functional dysfunction in patients with low back pain.[22] A comparison of postoperative ODI scores between the 2 groups indicated whether epidural anesthesia caused more dysfunction than local anesthesia in the waist region. In fact, it indirectly reflected the safety of the 2 anesthetic techniques. We found that the postoperative ODI showed no significant difference between the LA and EA groups. This shows that both groups recovered well after surgery, consistent with the findings in previous studies.[3,8,9,11]
Our meta-analysis also found no significant differences in the surgical duration and X-ray exposure time between the 2 groups, although the average X-ray exposure time was shorter in the EA group of 2 studies. In Xu study, the EA group exhibited a shorter surgical duration and lower X-ray dose.[6] In Fang's study, the average X-ray exposure time was 14.7 seconds (2–60 seconds) and 16.0 seconds (2–50 seconds) in the LA and EA groups, respectively, with no significant difference between groups. However, because no standard deviation value was provided, the data could not be used for meta-analysis.[7] Consequently, only 2 studies had data for analysis of the surgical duration and X-ray exposure time, and the obtained results were limited. In addition, it should be noted that the surgical duration and X-ray exposure time were also related to the learning curve for the surgeon and anesthetist in each study.
Seven types of complications were mentioned in each included study; these included transient numbness, foot drop, nausea and vomiting, cerebrospinal leakage, dysuria, dizziness, and blood pressure fluctuations. We found no significant difference between the EA and LA groups in terms of the overall complication and individual complication rates. These findings indicate that EA is as safe as LA. The most frequent complication is transient numbness due to intraoperative nerve root traction. This also highlights the importance of keeping the patient awake during PTED.
This study had some limitations. First, the number of eligible studies was small, and only 4 RCTs were included. Second, the types and concentrations of the anesthetic drugs and the follow-up period varied among studies. Third, the 8 studies included in this review were all conducted in China. The possible reasons are as follows. In other countries, percutaneous transforaminal endoscopic discectomy is often performed by pain specialists or outpatient physicians without the assistance of an anesthesiologist, with the exception of cases requiring general anesthesia. On the other hand, in China, this procedure is usually performed by a multidisciplinary team including orthopedic surgeons and anesthesiologists, regardless of the anesthetic technique. Percutaneous transforaminal endoscopic discectomy under epidural anesthesia often requires the cooperation of the surgeon and anesthesiologist. Therefore, research on this topic in other countries is currently lacking. Considering these limitations, the conclusions of this study should be cautiously applied. In the future, more RCTs should be conducted for the generation of more reliable medical evidence via the integration of multicenter and large-scale data.
In conclusion, the findings of our meta-analysis suggest that EA is as safe as LA and produces better anesthetic effects than does LA in patients undergoing PTED. Therefore, it should be promoted as a reliable anesthetic technique for PTED.
Author contributions
Conceptualization: Jian Sun.
Data curation: Jian Sun, Chao Fang.
Formal analysis: Jian Sun, Fei Gao.
Investigation: Fei Gao, Laifu Wei.
Methodology: Jian Sun, Chao Fang, Jun Qian.
Software: Jian Sun, Chao Fang.
Supervision: Jun Qian.
Writing – original draft: Jian Sun, Jun Qian.
Writing – review & editing: Jian Sun, Jun Qian.
Footnotes
Abbreviations: CI = confidence interval, EA = epidural anesthesia, LA = local anesthesia, LDH = lumbar disc herniation, MD = mean difference, ODI = Oswestry Disability Index, PTED = percutaneous transforaminal endoscopic discectomy, RR = risk ratio, VAS = visual analog scale.
How to cite this article: Sun J, Fang C, Gao F, Wei L, Qian J. Comparison of effectiveness and safety between epidural anesthesia versus local anesthesia for percutaneous transforaminal endoscopic discectomy: a systematic review and meta-analysis. Medicine. 2020;99:1(e18629).
The authors declare that they have no competing interests.
This study did not receive funding from any source.
References
- [1].Yu H, Zhou Z, Lei X, et al. Mixed reality-based preoperative planning for training of percutaneous transforaminal endoscopic discectomy: a feasibility study. World Neurosurg 2019; 10.1016/j.wneu.2019.06.020 [DOI] [PubMed] [Google Scholar]
- [2].Burkhardt BW, Grimm M, Schwerdtfeger K, et al. The microsurgical treatment of lumbar disc herniation - a report of 158 patients with a mean follow-up of more than 32 years. Spine 2019; 10.1097/BRS.00000000000003113 [DOI] [PubMed] [Google Scholar]
- [3].Zhu Y, Zhao Y, Fan G, et al. Comparison of 3 anesthetic methods for percutaneous transforaminal endoscopic discectomy: a prospective study. Pain Physician 2018;21:E347–53. [PubMed] [Google Scholar]
- [4].Hu D, Fei J, Chen G, et al. Treatment for lumbar spinal stenosis in elderly patients using percutaneous endoscopic lumbar discectomy combined with postoperative three-dimensional traction. Expert Rev Med Devices 2019;16:317–23. [DOI] [PubMed] [Google Scholar]
- [5].Gu G, Wang C, Gu X, et al. Percutaneous transforaminal endoscopic discectomy for adjacent segment disease after lumbar fusion in elderly patients over 65 years old. World Neurosurg 2018;112:e830–6. [DOI] [PubMed] [Google Scholar]
- [6].Xu T, Tian R, Qiao P, et al. Application of continuous epidural anesthesia in transforaminal lumbar endoscopic surgery: a prospective randomized controlled trial. J Int Med Res 2019;47:1146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Fang G, Ding Z, Song Z. Comparison of the effects of epidural anesthesia and local anesthesia in lumbar transforaminal endoscopic surgery. Pain Physician 2016;19:E1001–4. [PubMed] [Google Scholar]
- [8].Zhu Y, Zhao Y, Fan G, et al. Comparison of the effects of local anesthesia and epidural anesthesia for percutaneous transforaminal endoscopic discectomy in elderly patients over 65 years old. Int J Surg 2017;48:260–3. [DOI] [PubMed] [Google Scholar]
- [9].Wang SJ, Chen BH, Wang P, et al. The effect of percutaneous endoscopic lumbar discectomy under different anesthesia on pain and immunity of patients with prolapse of lumbar intervertebral disc. European review for medical and pharmacological sciences 2017;21:2793–9. [PubMed] [Google Scholar]
- [10].Kong WJ, Liao WB, Tan JP, et al. Curative effects of percutaneous transforaminal endoscopic discectomy on lumbar disc herniation treament in different anesthesia. J Zunyi Med Univ 2015; 10.14169/j.cnki.zunyixuebao.2015.0044 [DOI] [Google Scholar]
- [11].Chen H, Yuan Y, Wang SH, et al. Comparison of epidural anesthesia and local anesthesia in percutaneous endoscopic lumbar surgery. J Hebei Med Univ 2019; 10.3969/j.issn.1007-3205.2019.04.025 [DOI] [Google Scholar]
- [12].Luo M, Geng LC, Gao T. The application of low concentration ropivacaine epidural anesthesia in the operation of transforaminal endoscopic. Chin J Surg Integr Tradition Western Med 2019; 10.3969/j.issn.1007-6948.2019.01.010 [DOI] [Google Scholar]
- [13].Ahn Y, Jang IT, Kim WK. Transforaminal percutaneous endoscopic lumbar discectomy for very high-grade migrated disc herniation. Clin Neurol Neurosurg 2016;147:11–7. [DOI] [PubMed] [Google Scholar]
- [14].Liu W, Li Q, Li Z, et al. Clinical efficacy of percutaneous transforaminal endoscopic discectomy in treating adolescent lumbar disc herniation. Medicine 2019;98:e14682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Inufusa A, An HS, Lim TH, et al. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion-extension movement. Spine 1996;21:2412–20. [DOI] [PubMed] [Google Scholar]
- [16].Henmi T, Terai T, Nagamachi A, et al. Morphometric changes of the lumbar intervertebral foramen after percutaneous endoscopic foraminoplasty under local anesthesia. J Neurol Surg A Cent Eur Neurosurg 2018;79:19–24. [DOI] [PubMed] [Google Scholar]
- [17].Sairyo K, Chikawa T, Nagamachi A. State-of-the-art transforaminal percutaneous endoscopic lumbar surgery under local anesthesia: discectomy, foraminoplasty, and ventral facetectomy. J Orthop Sci 2018;23:229–36. [DOI] [PubMed] [Google Scholar]
- [18].Fan Y, Gu G, Fan G, et al. The effect of preoperative administration of morphine in alleviating intraoperative pain of percutaneous transforaminal endoscopic discectomy under local anesthesia: A STROBE compliant study. Medicine 2017;96:e8427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hua W, Zhang Y, Wu X, et al. Outcomes of discectomy by using full-endoscopic visualization technique via the interlaminar and transforaminal approaches in the treatment of L5-S1 disc herniation: an observational study. Medicine 2018;97:e13456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Mao S, Zhu C, Chang Y. Effects of different anesthesia methods on postoperative transient neurological syndrome in patients with lumbar disc herniation. Exp Ther Med 2017;14:3112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Graf BM. The cardiotoxicity of local anesthetics: the place of ropivacaine. Curr Top Med Chem 2001;1:207–14. [DOI] [PubMed] [Google Scholar]
- [22].Arpinar VE, Gliedt JA, King JA, et al. Oswestry Disability Index scores correlate with MRI measurements in degenerating intervertebral discs and endplates. Eur J Pain 2019; 10.1002/ejp.1490 [DOI] [PubMed] [Google Scholar]


