Abstract
Both inhibiting ascending nociceptive transmission and activating descending inhibition are involved in the opioid analgesic effect. The spinal dorsal horn is a critical site for modulating nociceptive transmission by descending pathways elicited by opioids in the brain. μ-Opioid receptors (MORs, encoded by Oprm1) are highly expressed in primary sensory neurons and their central terminals in the spinal cord. In the present study, we tested the hypothesis that MORs expressed in primary sensory neurons contribute to the descending inhibition and supraspinal analgesic effect induced by centrally administered opioids. We generated Oprm1 conditional knockout (Oprm1-cKO) mice by crossing AdvillinCre/+ mice with Oprm1flox/flox mice. Immunocytochemcal labeling in Oprm1-cKO mice showed that MORs are completely ablated from primary sensory neurons and are profoundly reduced in the superficial spinal dorsal horn. Intracerebroventricular injection of morphine or fentanyl produced a potent analgesic effect in wild-type mice, but such an effect was significantly attenuated in Oprm1-cKO mice. Furthermore, the analgesic effect produced by morphine or fentanyl microinjected into the periaqueductal gray was significantly greater in wild-type mice than in Oprm1-cKO mice. Blocking MORs at the spinal cord level diminished the analgesic effect of morphine and fentanyl microinjected into the periaqueductal gray in both groups of mice. Our findings indicate that MORs expressed at primary afferent terminals in the spinal cord contribute to the supraspinal opioid analgesic effect. These presynaptic MORs in the spinal cord may serve as an interface between ascending inhibition and descending modulation that are involved in opioid analgesia.
Keywords: opiate, descending inhibition, dorsal root ganglion, primary afferent neuron, periaqueductal gray
INTRODUCTION
Opioids produce analgesia through both inhibiting ascending nociceptive transmission and activating descending inhibition (Clark et al., 1983; Jones and Gebhart, 1988; Chiou and Huang, 1999). μ-Opioid receptors (MORs, encoded by the Oprm1 gene) are extensively expressed in the dorsal root ganglion (DRG) and central nervous system, including the spinal cord, brainstem, and periaqueductal gray (PAG) (Thompson et al., 1993; George et al., 1994; Kalyuzhny et al., 1996; Wang and Wessendorf, 2002; Chen and Pan, 2006a; Sun et al., 2019). The spinal dorsal horn is a critical site involved in processing nociceptive input from primary sensory neurons and in modulating nociceptive transmission by descending input from the brain regions (Jensen, 1997; Kohno et al., 1999; Finnegan et al., 2004; Chen and Pan, 2006b). Blocking MORs at the spinal cord level reduces the inhibitory effect of supraspinal opioids on spinal dorsal horn neurons (Budai and Fields, 1998; Kwok et al., 2014). In the spinal cord, MORs are present presynaptically at the central terminals of DRG neurons and postsynaptically in dorsal horn neurons (Abbadie et al., 2002; Marker et al., 2005; Chen and Pan, 2006a; Zhou et al., 2010). MORs expressed in primary sensory neurons are essential for the full analgesic effect of opioids administered systemically and intrathecally through inhibition of nociceptive input (Chen and Pan, 2006b; Sun et al., 2019). However, it is unclear whether MORs expressed at primary afferent terminals in the spinal cord play a role in the supraspinal opioid analgesic effect.
The midbrain PAG is a key brain site in the descending analgesia circuit. Immunocytochemcal labeling and in situ hybridization show that MORs are expressed extensively in the PAG, especially in the ventrolateral PAG (vlPAG) (Kalyuzhny et al., 1996; Peckys and Landwehrmeyer, 1999; Wang and Wessendorf, 2002). Activation of MORs in the vlPAG produces supraspinal opioid analgesia through a descending pathway involving projections to the rostral ventromedial medulla (RVM) and spinal cord (Smith et al., 1988; Wang and Wessendorf, 2002; Morgan et al., 2014). Microinjection of opioids into the PAG produces analgesia (Rossi et al., 1994; Sohn et al., 2000), whereas PAG lesion reduces the analgesic effect of systemically administered morphine (Deakin and Dostrovsky, 1978). Opioids may stimulate the descending pathway through disinhibition of inhibitory neurons in the PAG (Vaughan and Christie, 1997; Chiou and Huang, 1999; Park et al., 2010). Although endogenous opioids acting via spinal MORs mediate vlPAG-elicited inhibition of dorsal horn neurons (Budai and Fields, 1998), the specific contribution of MORs present in primary sensory neurons to supraspinal opioid analgesia remains unknown.
In the present study, we tested the hypothesis that MORs expressed in primary sensory neurons contribute to the supraspinal analgesic effect of opioids. To this end, we conditionally knocked out MORs from DRG neurons and their presynaptic terminals in the spinal cord and used this Oprm1 conditional knockout mouse line to investigate the role of MORs in primary sensory neurons in the supraspinal opioid analgesic effect. Our findings demonstrate for the first time that presynaptic MORs at primary afferent terminals in the spinal cord contribute significantly to supraspinal opioid analgesia.
RESULTS
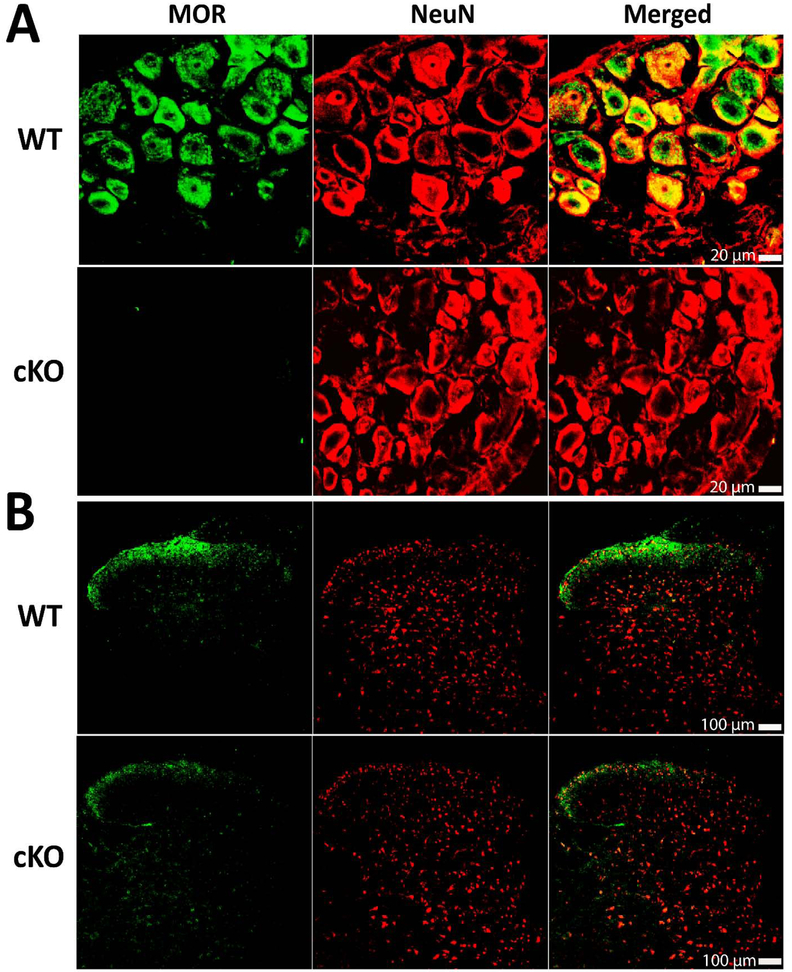
MORs are abrogated in the DRG and reduced in the spinal cord in Oprm1-cKO mice
To determine changes in the distribution of MORs in the DRG and spinal cord in Oprm1-cKO mice, we performed double-immunofluorescence labeling of MORs and NeuN in the DRG and spinal cord tissues. The amount of MORs in brain tissues, including the brainstem and PAG, is not altered in AdvillinCre/+:Oprm1flox/flox mice (Sun et al., 2019). Confocal images show that the MOR-immunoreactivity was present extensively in DRG neurons in WT mice. In contrast, the MOR-immunoreactivity was not detected in the DRG in Oprm1-cKO mice (Figure 1A). Furthermore, the MOR-immunoreactivity was predominantly distributed in the superficial laminae of the spinal dorsal horn in WT mice. However, the MOR-immunoreactivity in the superficial dorsal horn was substantially reduced in Oprm1-cKO mice (Figure 1B).
Figure 1. Oprm1 conditional knockout ablates MORs in all DRG neurons and diminishes the MOR level in the spinal superficial dorsal horn.
A, B: Representative confocal images of double immunofluorescence labeling of MORs and NeuN in the DRG (A) and spinal dorsal horn (B) in WT and Oprm1-cKO mice. All images are single confocal optical sections. Scale bar, 20 μm for DRG sections and 100 μm for spinal cord sections (selected from 3 mice per group).
Ablation of MORs in primary sensory neurons reduces the analgesic effect of intracerebroventricular morphine
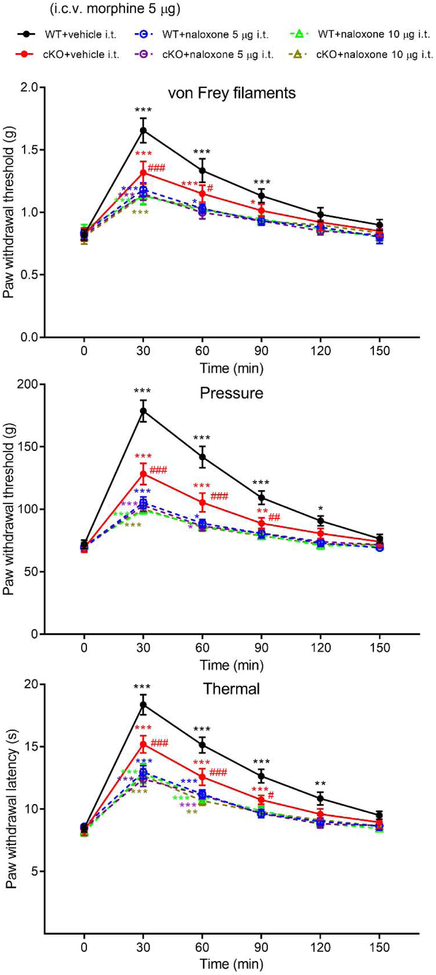
We first used Oprm1-cKO mice to determine whether MORs expressed in primary sensory neurons are involved in the supraspinal analgesic effect produced by intracerebroventricular (i.c.v.) injection of morphine. I.c.v. injection of 5 μg of morphine in WT mice caused a large increase in the paw withdrawal threshold in response to mechanical and heat stimuli (P < 0.0001, F(5,55) = 28.79 for von Frey threshold; P < 0.0001, F(5,55) = 147.70 for pressure threshold; P < 0.0001, F(5,55) = 148.40 for thermal threshold; n = 12 mice; Figure 2). Remarkably, the analgesic effect produced by i.c.v. injection of 5 μg of morphine was significantly attenuated in Oprm1-cKO mice compared with that in WT mice (P < 0.0001, F(5,55) = 12.54 for von Frey threshold; P < 0.0001, F(5,55) = 51.14 for pressure threshold; P < 0.0001, F(5,55) = 29.16 for thermal threshold; n = 12 mice per group, Figure 2).
Figure 2. The analgesic effects of intracerebroventricular injection of morphine in WT and Oprm1-cKO mice.
Time course of the effect of intracerebroventricular (i.c.v.) injection of 5 μg of morphine with or without intrathecal naloxone (5 or 10 μg) on the paw withdrawal thresholds in response to von Frey filaments and noxious pressure and thermal stimuli in WT and Oprm1-cKO mice (n = 12 mice per group). Data are shown as means ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001 compared with the respective baseline. #P < 0.05, ##P < 0.01, ###P < 0.001 compared with the value at the same time point in the WT group. Two-way ANOVA.
Because morphine injected via i.c.v. route may spread caudally via the circulating cerebrospinal fluid to the spinal cord and activate MORs expressed at primary afferent terminals and dorsal horn neurons, we blocked MORs at the spinal cord level by intrathecal injection of 5 μg of naloxone (Chen and Pan, 2006b). When naloxone was injected intrathecally 5 min before morphine, the analgesic effect of i.c.v. administration of 5 μg of morphine was further reduced in Oprm1-cKO mice (Figure 2). However, the reduced analgesic effects of i.c.v. morphine by intrathecal naloxone were similar in WT and Oprm1-cKO mice (n = 12 mice per group, Figure 2).
To exclude the possibility of inadequate spinal MOR blockade by 5 μg of naloxone, we tested a high dose (10 μg) of naloxone injected intrathecally. Naloxone at 5 and 10 μg similarly attenuated the analgesic effect of i.c.v. injection of 5 μg of morphine in both WT and Oprm1-cKO mice (Figure 2).
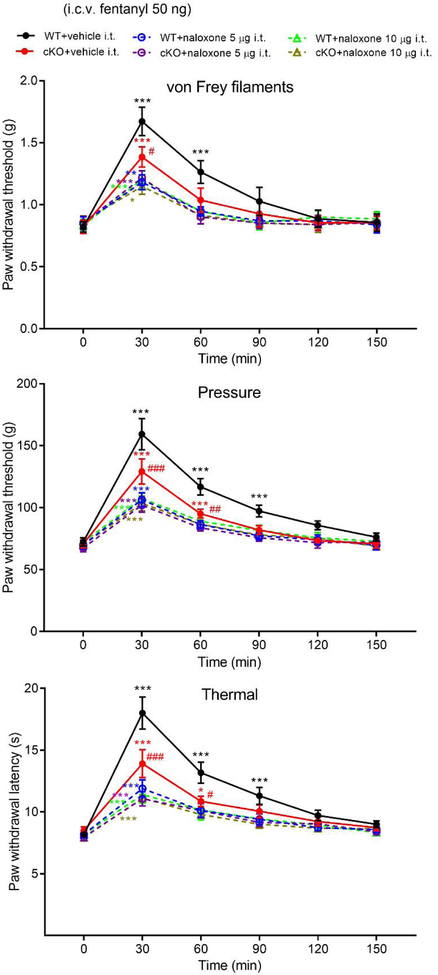
Removal of MORs in primary sensory neurons attenuates the analgesic effect of intracerebroventricular fentanyl
To determine the role of MORs expressed in primary sensory neurons in the supraspinal analgesic effect of another MOR agonist, we compared the analgesic effect produced by i.c.v injection of fentanyl in WT and Oprm1-cKO mice. In WT mice, i.c.v. injection of 50 ng of fentanyl (Raffa et al., 1987) profoundly increased the withdrawal threshold in response to mechanical and thermal stimuli (P < 0.0001, F(5,55) = 45.06 for von Frey threshold; P < 0.0001, F(5,55) = 51.63 for pressure threshold; P < 0.0001, F(5,55) = 71.59 for thermal threshold; n = 12 mice, Figure 3). However, the analgesic effect of i.c.v. injection of 50 ng of fentanyl was significantly attenuated in Oprm1-cKO mice compared with that in WT mice (P = 0.0143, F(5,55) = 5.29 for von Frey threshold; P < 0.0001, F(5,55) = 23.08 for pressure threshold; P < 0.0001, F(5,55) = 24.02 for thermal threshold; n = 12 mice per group, Figure 3).
Figure 3. The analgesic effects of intracerebroventricular injection of fentanyl in WT and Oprm1-cKO mice.
Time course of the effect of i.c.v. injection of 50 ng fentanyl with or without intrathecal naloxone (5, 10 μg) on the paw withdrawal thresholds in response to von Frey filaments and noxious pressure and thermal stimuli in WT and Oprm1-cKO mice (n = 12 mice per group). Data are shown as means ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001 compared with the respective baseline. #P < 0.05, ##P < 0.01, ###P < 0.001 compared with the value at the same time point in WT group. Two-way ANOVA.
When naloxone (5 or 10 μg) was injected intrathecally, it caused a further reduction in the analgesic effect of i.c.v. administration of 50 ng of fentanyl in Oprm1-cKO mice (Figure 3). Nevertheless, this diminished analgesic effect occurred similarly in WT and Oprm1-cKO mice (P = 0.9988, F(5,55) = 5.29 for von Frey threshold; P = 0.9764, F(5,55) = 23.08 for pressure threshold; P = 0.8786, F(5,55) = 24.02 for thermal threshold; n = 12 mice per group, Figure 3). Collectively, these results suggest that MORs expressed in primary sensory neurons contribute to the supraspinal analgesic effect of opioids.
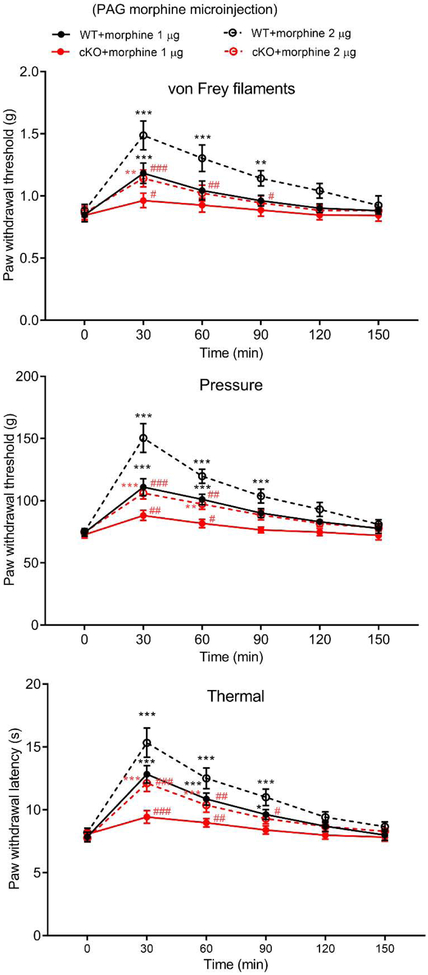
Ablation of MORs in primary sensory neurons reduces the analgesic effect produced by morphine microinjection into the vlPAG
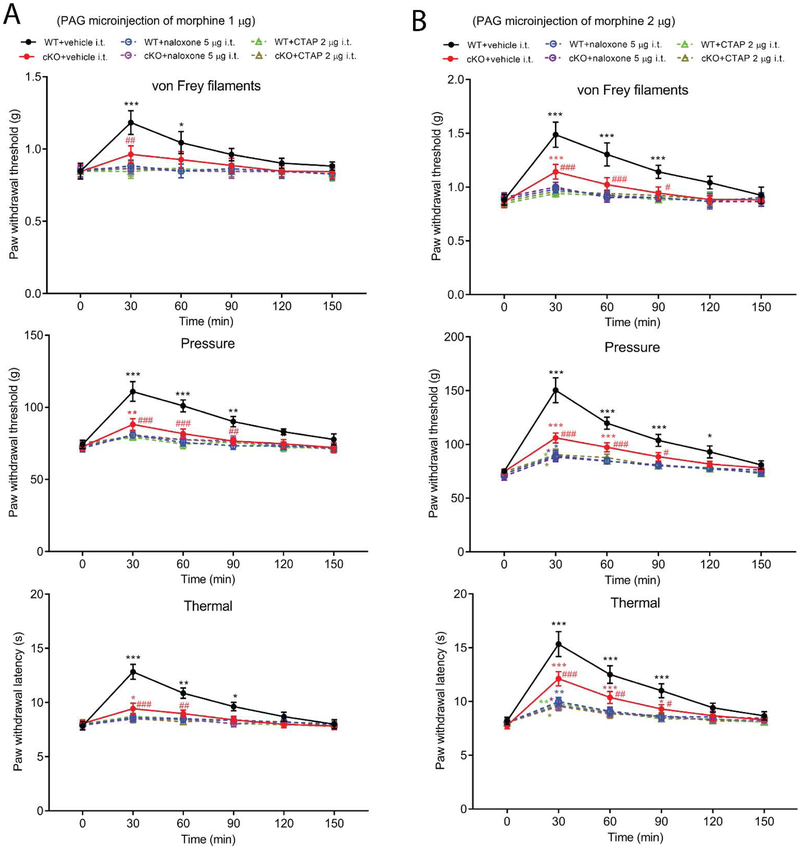
Because i.c.v. injected morphine or fentanyl may spread caudally via the circulating cerebrospinal fluid to the spinal cord, we next determined the role of MORs expressed in primary sensory neurons in the supraspinal analgesic effect produced by direct microinjection of morphine into the vlPAG. MORs are highly expressed in the PAG, and MOR stimulation in the vlPAG is closely involved in the descending inhibition of nociceptive transmission (Jones and Gebhart, 1988; Budai and Fields, 1998). We implanted a cannula into the right vlPAG one week prior to microinjection. Microinjection of 1 or 2 μg of morphine into the vlPAG (Nunes-de-Souza et al., 1991; Mehalick et al., 2013) in WT mice dose-dependently increased the paw withdrawal threshold in response to mechanical and thermal stimuli (P = 0.0002, F(5,45) = 27.31 for von Frey threshold; P < 0.0001, F(5,45) = 54.24 for pressure threshold; P < 0.0001, F(5,45) = 40.82 for thermal threshold; n = 10 mice, Figure 4). However, the analgesic effect produced by microinjection of 1 or 2 μg of morphine into the vlPAG was significantly attenuated in Oprm1-cKO mice compared with that in WT mice (P = 0.0193, F(3,27) = 7.503 for von Frey threshold; P = 0.0030, F(3,27) = 48.22 for pressure threshold; P < 0.0001, F(3,27) = 29.13 for thermal threshold; n = 10 mice per group, Figure 4).
Figure 4. The analgesic effects of microinjection of morphine into the vlPAG in WT and Oprm1-cKO mice.
Time course of the effect of microinjection of 1 or 2 μg of morphine into the vlPAG on the paw withdrawal thresholds in response to von Frey filaments and noxious pressure and thermal stimuli in WT and Oprm1-cKO mice (n = 10 mice per group). Data are shown as means ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001 compared with the respective baseline. #P < 0.05, ##P < 0.01, ###P < 0.001 compared with the value at the same time point in WT group. Two-way ANOVA.
We then determined the role of spinally expressed MORs (including both presynaptic and postsynaptic MORs) in the analgesic effects produced by microinjection of morphine into the vlPAG. We blocked MORs at the spinal cord level by intrathecal injection of 5 μg naloxone or 2 μg CTAP (in 5 μl), a highly specific MOR antagonist (Pelton et al., 1986; Kramer et al., 1989; Chen and Pan, 2006b). When naloxone or CTAP was injected intrathecally 5 min before morphine, subsequent microinjection of 2 μg morphine into the vlPAG failed to produce a significant analgesic effect in Oprm1-cKO mice (n = 10 mice, Figure 5A). Nevertheless, intrathecal naloxone or CTAP diminished the analgesic effect of morphine similarly in WT and Oprm1-cKO mice (P = 0.9996, F(5,45) = 7.455 for von Frey threshold; P = 0.9999, F(5,45) = 71.05 for pressure threshold; P = 0.9837, F(5,45) = 17.23 for thermal threshold; n = 10 mice per group, Figure 5B). These results suggest that MORs expressed at spinal primary afferent terminals participate in the supraspinal analgesic effect of morphine.
Figure 5. The analgesic effects of microinjection of morphine into the vlPAG with or without intrathecal naloxone or CTAP in WT and Oprm1-cKO mice.
A, B: Time course of the effect of microinjection of 1 (A) or 2 (B) μg of morphine into the vlPAG with or without intrathecal 5 μg naloxone or 2 μg CTAP on the paw withdrawal thresholds in response to von Frey filaments and noxious pressure and thermal stimuli in WT and Oprm1-cKO mice (n = 10 mice per group). Data are shown as means ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001 compared with the respective baseline. #P < 0.05, ##P < 0.01, ###P < 0.001 compared with the value at the same time point in WT group. Two-way ANOVA.
Removal of MORs in primary sensory neurons attenuates the analgesic effect produced by fentanyl microinjection into the vlPAG
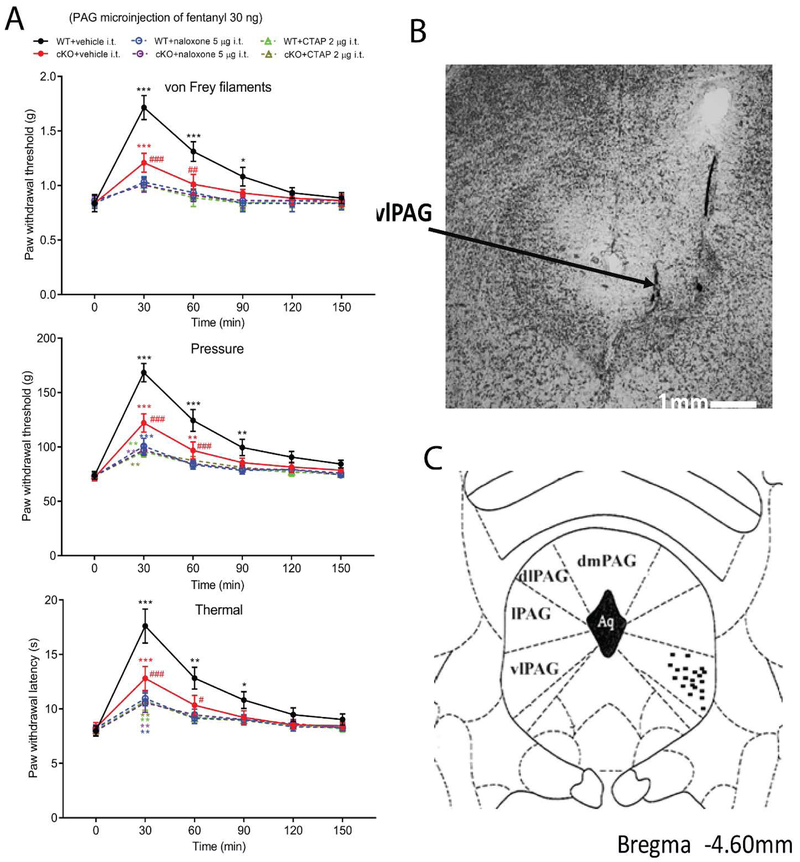
We also determined whether MORs expressed in primary sensory neurons mediate the supraspinal analgesic effect of fentanyl, another potent MOR agonist, microinjected into the vlPAG. Microinjection of 30 ng of fentanyl into the vlPAG in WT mice substantially increased the paw withdrawal threshold in response to mechanical and thermal stimuli (P < 0.0001, F(5,35) = 10.39 for von Frey threshold; P < 0.0001, F(5,35) = 68.19 for pressure threshold; P < 0.0001, F(5,35) = 22.05 for thermal threshold; n = 8 mice per group, Figure 6A). However, the analgesic effect of fentanyl microinjected to the vlPAG was significantly attenuated in Oprm1-cKO mice compared with that in WT mice (P < 0.0001, F(5,35) = 12.71 for von Frey threshold; F(5,35) = 27.58 for pressure threshold; F(5,35) = 20.23 for thermal threshold; n = 8 mice per group, Figure 6A).
Figure 6. The analgesic effects of microinjection of fentanyl into the vlPAG with or without intrathecal naloxone or CTAP in WT and Oprm1-cKO mice.
A: Time course of the effect of microinjection of 30 ng of fentanyl into the vlPAG with or without intrathecal 5 μg naloxone or 2 μg CTAP on the paw withdrawal thresholds in response to von Frey filaments and noxious pressure and thermal stimuli in WT and Oprm1-cKO mice (n = 8 mice per group). Data are shown as means ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001 compared with the respective baseline. #P < 0.05, ##P < 0.01, ###P < 0.001 compared with the value at the same time point in WT group. Two-way ANOVA. B, C: Representative brain tissue section image (B) and schematic drawing (C) show the microinjection sites in the vlPAG. Scale bar, 1 mm. dmPAG, dorsomedial PAG; dlPAG, dorsolateral PAG; lPAG, lateral PAG; vlPAG, ventrolateral PAG.
Furthermore, when 5 μg naloxone or 2 μg CTAP was injected intrathecally 5 min before fentanyl, the analgesic effect produced by fentanyl microinjected to vlPAG was largely blocked in Oprm1-cKO mice. However, this diminished analgesic effect of fentanyl by intrathecal naloxone or CTAP was similar in both WT and Oprm1-cKO mice (P = 0.9997, F(5,35) = 12.71 for von Frey threshold; P = 0.9927, F(5,35) = 27.58 for pressure threshold; P = 0.9943, F(5,35) = 20.23 for thermal threshold; n = 8 mice per group, Figure 6A). Successful vlPAG cannula placement was confirmed by examining PAG-containing brain sections in all mice (Figure 6B,C). These data suggest that MORs expressed presynaptically at primary afferent terminals in the spinal cord are involved in the supraspinal analgesic effect of fentanyl.
DISCUSSION
The most important finding of our study is that MORs present in primary sensory neurons contribute significantly to the supraspinal opioid analgesic effect. We generated AdvillinCre/+:Oprm1flox/flox mice to genetically ablate MORs expressed in primary sensory neurons and their central terminals in the spinal cord. The reduced MOR level in the dorsal spinal cord of Oprm1-cKO mice indicates that a substantial proportion of MORs in the spinal cord is transported from DRG somas to their central terminals (Stevens and Seybold, 1995; Abbadie et al., 2002; Chen and Pan, 2006a; Sun et al., 2019). The MOR expression level in brain tissues, such as the brainstem and PAG, is not altered by Oprm1-cKO (Sun et al., 2019). We found unexpectedly that the analgesic effect of i.c.v. injection of morphine or fentanyl was considerably smaller in Oprm1-cKO mice than in WT mice, suggesting that MORs expressed in primary sensory neurons are involved the supraspinal opioid analgesic effect. Furthermore, we showed that the analgesic effect produced by i.c.v. morphine or fentanyl was further reduced in Oprm1-cKO mice when MORs at the spinal cord level were blocked by naloxone. When spinal MORs were blocked, the remaining analgesic effect of i.c.v. injection of morphine and fentanyl did not differ between WT and Oprm1-cKO mice. Our findings indicate that the supraspinal opioid analgesic effect depends on both presynaptic and postsynaptic MORs present in the spinal dorsal horn. The residual analgesic effect produced by i.c.v. opioids in the presence of spinal MOR blockade is likely mediated by concurrent activation of MORs that are present in various brain regions, including the PAG, RVM, amygdala, and locus coeruleus (Kalyuzhny and Wessendorf, 1998; Wang and Wessendorf, 2002; Finnegan et al., 2004; Pan et al., 2004; Finnegan et al., 2005).
Because i.c.v. injected opioids can spread to the spinal cord through circulating cerebrospinal fluid, we microinjected morphine and fentanyl directly into the vlPAG to elicit descending inhibition and supraspinal opioid analgesia. It has been shown that microinjection of opioids into the vlPAG suppresses nociceptive transmission at the spinal cord level via descending projections from the rostral ventromedial medulla (RVM) to spinal cord (Wang and Wessendorf, 2002; Kwok et al., 2014; Kim et al., 2018). We showed that the analgesic effect produced by microinjection of morphine or fentanyl into the vlPAG was diminished by blocking spinal MORs with naloxone or CTAP, indicating that that the analgesic effect of stimulation of MORs in the vlPAG is mediated via descending inhibition involving MORs at the spinal cord level. MORs at the spinal cord level are essential for the inhibitory effect of systemically administered opioids on pain and dorsal horn projection neurons (Chen et al., 2005; Chen and Pan, 2006b). Centrally expressed MORs are mainly involved in analgesia produced by high doses of systemically administered MOR agonists (Marker et al., 2005; Sun et al., 2019). Importantly, we demonstrated that the analgesic effect of microinjection of morphine or fentanyl into the vlPAG was significantly reduced when MORs were ablated in primary sensory neurons in Oprm1-cKO mice. Our findings indicate that presynaptic MORs present at primary afferent terminals in the spinal cord contribute importantly to the supraspinal opioid analgesia.
Although vlPAG has a significant role in supraspinal opioid analgesia and in descending control of nociceptive transmission via connections with the RVM and spinal cord (Lewis and Gebhart, 1977; Thorn et al., 1989; Wang and Wessendorf, 2002), it is not clear as to how stimulation of MORs in the PAG leads to descending inhibition to activate MORs at the spinal cord level. Stimulation of MORs in the vlPAG may act on inhibitory interneurons (disinhibition) to promote endogenous opioid peptide release from descending fibers to the spinal dorsal horn (Jensen, 1997; Budai and Fields, 1998; Kalyuzhny and Wessendorf, 1998; Chiou and Huang, 1999; Park et al., 2010), which then activates spinal presynaptic and postsynaptic MORs to attenuate nociceptive transmission.
In summary, our study provides new in vivo evidence that MORs expressed at primary afferent terminals in the spinal cord play an important role in the supraspinal opioid analgesic effect. MORs at primary afferent terminals in the spinal cord may serve as an interface between ascending nociceptive inhibition and descending nociceptive modulation that are involved in opioid analgesia. This new information extends our understanding of the role of MORs present in primary sensory neurons in opioid analgesic actions.
METHODS AND MATERIALS
Animal Models
All experimental procedures and protocols were approved by the Institutional Animal Care and Use Committee and were performed in accordance with the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. To genetically delete MORs in primary sensory neurons, we crossed Oprm1flox/flox mice (Weibel et al., 2013) with AdvillinCre/+ mice (Zhou et al., 2010; da Silva et al., 2011). Oprm1flox/flox mice were obtained from The Jackson Laboratory (Stock #030074, Bar Harbor, ME), and AdvillinCre/+mice were provided by Dr. F. Wang (Duke University, Durham, NC). All of the mutant mice were backcrossed onto the C57BL/6J background for at least eight generations. Male AdvillinCre/+ mice were crossed with female Oprm1flox/flox mice to obtain male AdvillinCre/+:Oprm1flox/+ mice, which were crossed again to female Oprm1flox/flox mice to generate AdvillinCre/+:Oprm1flox/flox mice, referred to as Oprm1 conditional knockout (Oprm1-cKO) mice. Mice were earmarked 21 days after birth, and tail biopsies were used for PCR genotyping. Mice were kept in a temperature-controlled, specific-pathogen-free environment. Adult Oprm1-cKO mice used in our final experiments were age-and sex-matched with their wild-type (WT) littermates (8–10 weeks of age).
Double Immunofluorescence Labeling of MORs and NeuN in the DRG and spinal cord
To detect MORs in the DRG and spinal cord, double-immunofluorescence labeling of MORs and NeuN (a neuronal marker) was performed in L4 and L5 DRGs and the lumbar spinal cord from three WT and three cKO mice. The tissue sections were rinsed in 0.1 M phosphate buffered saline (PBS) and blocked in 4% normal goat serum in PBS for 1 h. Sections were then incubated with a mixture of primary antibodies (rabbit anti-MOR, #RA10104, dilution 1:1000, Neuromics, Minneapolis, MN; mouse anti-NeuN, #AB104224, dilution 1:300, Abcam, Cambridge, MA) diluted in PBS solution containing 2% normal goat serum and 0.3% Triton X-100 for 2 h at 26°C and then overnight at 4 °C. Sections were rinsed in PBS and incubated with a secondary antibody mixture (Alexa Fluor-488 conjugated to goat anti-rabbit IgG, #AB150077; Alexa Fluor-594 conjugated to goat anti-mouse IgG, #A11032; Molecular Probes, Eugene, OR; dilution: 5 μg/ml) for 1.5 h. Finally, the sections were rinsed in PBS for 30 min, mounted on slides, dried, and coverslipped. The specificity of the anti-MOR antibody has been validated in our previous studies (Chen and Pan, 2006a; Sun et al., 2019). The tissue sections were examined on a laser scanning confocal microscope (Zeiss, Jena, Germany).
Drug Administration and Cannula Placement
Morphine sulfate (West Ward Pharmaceuticals, Eatontown, NJ), fentanyl (Sigma-Aldrich, St. Louis, MO), naloxone hydrochloride (Sigma-Aldrich), D-Phe-Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH2 (CTAP) (Sigma-Aldrich) were diluted with normal saline and injected intrathecally, intracerebroventricularly (i.c.v.), or through an implanted cannula in the ventrolateral periaqueductal gray (vlPAG).
I.c.v. injection was carried out as previously described with some modification (Kim et al., 2016). In brief, scalp pre-shaved mice were briefly anesthetized with 2% isoflurane. The i.c.v. injection (5 μl of drug solution) was done using a 30.5–gauge needle connected to a 10-μl Hamilton syringe, and the puncture point was about 2 mm to the bregma and 3 mm to the middle line. The needle depth was 3 mm from the skull surface. Successful i.c.v. injection was confirmed by injection of a blue dye before the mice were killed.
Intrathecal injection was carried out using a lumbar puncture technique, as previously described (Hylden and Wilcox, 1980). Mice were briefly anesthetized with 2% isoflurane and placed in a prone position with a small tube under the abdomen to enlarge the lumbar vertebral space between L5 and L6. Lumbar puncture was performed with a 30.5 gauge needle connected to a 10-μl Hamilton syringe. Successful intrathecal injection (5 μl of drug solution) was indicated by brisk tail movement.
vlPAG injection was carried out via a cannula implanted in the right vlPAG (Mehalick et al., 2013). In brief, mice were anesthetized with 2% isoflurane and placed in a prone position and fixed in a stereotactic frame. A cannula (internal diameter, 0.64 mm) was placed to the right vlPAG according to the following stereotactic coordinates: 4.60 mm caudal to the bregma, 0.5 mm lateral to the midline, and 2.6 mm ventral to the dura. vlPAG injection (0.5 μl of drug solution) was performed using a 1-μl Hamilton syringe, and the nociceptive behavior was tested at least one week after the cannula placement. Successful vlPAG cannula placement was confirmed by examining the PAG tissues sections under the microscope at the end of the experiments.
Nociceptive Behavioral Tests
Three behavioral tests were performed to measure nociception in mice. An acclimatization period of 30–45 min was given before the mice were tested. To measure the tactile withdrawal threshold, mice were placed in individual plastic boxes on a mesh floor and allowed to acclimate for 30 min. A series of calibrated von Frey filaments was applied vertically to the plantar surface of the hindpaw with sufficient force to bend the filaments for 6 s, and a brisk paw withdrawal or flinching was considered a positive response. In the absence of a response, the filament of next greater force was applied. If a response occurred, the filament of next lower force was applied. The tactile stimulus producing a 50% likelihood of withdrawal was determined using the “up-down” method (Chaplan et al., 1994).
The mechanical nociception (Randall-Selitto test) was determined as previously described (Chen and Pan, 2006b; Chen et al., 2007). The hindpaw withdrawal threshold in response to a noxious pressure stimulus was measured using a paw pressure Analgesy-Meter (Ugo Basile Biological Research, Comerio, Italy). When the mice showed a painful response by the hindpaw withdrawal, the pressure device was immediately released. The withdrawal threshold was read directly from the scale. A cut-off of 200 g was used to prevent potential tissue injury.
Thermal nociception in mice were tested using a radiant heat device (IITC Life Sciences, Woodland Hills, CA). The temperature of the glass surface was maintained constant at 30°C. A mobile radiant heat source was beamed to the hindpaw, and the withdrawal latency was recorded by a timer. A cut-off of 30 s was used to prevent potential tissue damage. For all the three tests described above, we measured the withdrawal thresholds in both hindpaws and averaged threshold data from both hindpaws. The investigators performing the behavioral tests were blinded to the drug treatment and mouse genotypes.
Study Design and Statistical Analysis
Data are expressed as means ± standard errors of the mean (SEM). Although no specific methods were used to predetermine sample sizes for this study, our sample sizes were similar to those generally employed in the field. We did not exclude any animals from data analysis and did not use any test for outliers on the data. The behavioral test data were analyzed with two-way ANOVA followed by Tukey’s post-hoc test. Statistical analyses were performed using Prism software (v7.0, GraphPad Software Inc., La Jolla, CA). A P value of less than 0.05 was considered to be statistically significant.
Highlights.
The spinal dorsal horn is a key site for descending inhibition and opioid analgesia
Blocking spinal opioid receptors diminishes supraspinal opioid analgesic effects
Opioid receptor ablation in primary sensory neurons reduces supraspinal analgesia
Presynaptic opioid receptors in spinal cords mediate supraspinal opioid analgesia
Acknowledgments
This work was supported by the National Institutes of Health (Grant #R01 DA041711) and the N.G. and Helen T. Hawkins Endowment (to H.-L.P.).
List of abbreviations:
- cKO
conditional knockout
- CTAP
D-Phe-Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH2
- DRG
dorsal root ganglion
- i.c.v.
intracerebroventricular
- MOR
μ-opioid receptor
- PAG
periaqueductal gray
- RVM
rostral ventromedial medulla
- vlPAG
ventrolateral periaqueductal gray
- WT
wild-type
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors declare that they have no conflicts of interest with the contents of this study.
References
- Abbadie C, Lombard MC, Besson JM, Trafton JA, Basbaum AI (2002) Mu and delta opioid receptor-like immunoreactivity in the cervical spinal cord of the rat after dorsal rhizotomy or neonatal capsaicin: an analysis of pre- and postsynaptic receptor distributions. Brain Res 930:150–162. [DOI] [PubMed] [Google Scholar]
- Budai D, Fields HL (1998) Endogenous opioid peptides acting at mu-opioid receptors in the dorsal horn contribute to midbrain modulation of spinal nociceptive neurons. J Neurophysiol 79:677–687. [DOI] [PubMed] [Google Scholar]
- Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63. [DOI] [PubMed] [Google Scholar]
- Chen SR, Pan HL (2006a) Loss of TRPV1-expressing sensory neurons reduces spinal mu opioid receptors but paradoxically potentiates opioid analgesia. J Neurophysiol 95:3086–3096. [DOI] [PubMed] [Google Scholar]
- Chen SR, Pan HL (2006b) Blocking mu opioid receptors in the spinal cord prevents the analgesic action by subsequent systemic opioids. Brain Res 1081:119–125. [DOI] [PubMed] [Google Scholar]
- Chen SR, Prunean A, Pan HM, Welker KL, Pan HL (2007) Resistance to morphine analgesic tolerance in rats with deleted transient receptor potential vanilloid type 1-expressing sensory neurons. Neuroscience 145:676–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YP, Chen SR, Pan HL (2005) Systemic morphine inhibits dorsal horn projection neurons through spinal cholinergic system independent of descending pathways. J Pharmacol Exp Ther 314:611–617. [DOI] [PubMed] [Google Scholar]
- Chiou LC, Huang LY (1999) Mechanism underlying increased neuronal activity in the rat ventrolateral periaqueductal grey by a mu-opioid. J Physiol 518 (Pt 2):551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark SL, Edeson RO, Ryall RW (1983) The relative significance of spinal and supraspinal actions in the antinociceptive effect of morphine in the dorsal horn: an evaluation of the microinjection technique. Br J Pharmacol 79:807–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva S, Hasegawa H, Scott A, Zhou X, Wagner AK, Han BX, Wang F (2011) Proper formation of whisker barrelettes requires periphery-derived Smad4-dependent TGF-beta signaling. Proc Natl Acad Sci U S A 108:3395–3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deakin JF, Dostrovsky JO (1978) Involvement of the periaqueductal grey matter and spinal 5-hydroxytryptaminergic pathways in morphine analgesia: effcts of lesions and 5-hydroxytryptamine depletion. Br J Pharmacol 63:159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finnegan TF, Chen SR, Pan HL (2005) Effect of the {mu} opioid on excitatory and inhibitory synaptic inputs to periaqueductal gray-projecting neurons in the amygdala. J Pharmacol Exp Ther 312:441–448. [DOI] [PubMed] [Google Scholar]
- Finnegan TF, Li DP, Chen SR, Pan HL (2004) Activation of mu-opioid receptors inhibits synaptic inputs to spinally projecting rostral ventromedial medulla neurons. J Pharmacol Exp Ther 309:476–483. [DOI] [PubMed] [Google Scholar]
- George SR, Zastawny RL, Briones-Urbina R, Cheng R, Nguyen T, Heiber M, Kouvelas A, Chan AS, O’Dowd BF (1994) Distinct distributions of mu, delta and kappa opioid receptor mRNA in rat brain. Biochem Biophys Res Commun 205:1438–1444. [DOI] [PubMed] [Google Scholar]
- Hylden JL, Wilcox GL (1980) Intrathecal morphine in mice: a new technique. Eur J Pharmacol 67:313–316. [DOI] [PubMed] [Google Scholar]
- Jensen TS (1997) Opioids in the brain: supraspinal mechanisms in pain control. Acta Anaesthesiol Scand 41:123–132. [DOI] [PubMed] [Google Scholar]
- Jones SL, Gebhart GF (1988) Inhibition of spinal nociceptive transmission from the midbrain, pons and medulla in the rat: activation of descending inhibition by morphine, glutamate and electrical stimulation. Brain Res 460:281–296. [DOI] [PubMed] [Google Scholar]
- Kalyuzhny AE, Wessendorf MW (1998) Relationship of mu- and delta-opioid receptors to GABAergic neurons in the central nervous system, including antinociceptive brainstem circuits. J Comp Neurol 392:528–547. [PubMed] [Google Scholar]
- Kalyuzhny AE, Arvidsson U, Wu W, Wessendorf MW (1996) mu-Opioid and delta-opioid receptors are expressed in brainstem antinociceptive circuits: studies using immunocytochemistry and retrograde tract-tracing. J Neurosci 16:6490–6503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HY, Lee DK, Chung BR, Kim HV, Kim Y (2016) Intracerebroventricular Injection of Amyloid-beta Peptides in Normal Mice to Acutely Induce Alzheimer-like Cognitive Deficits. J Vis Exp 109:doi: 10.3791/53308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Gangadharan G, Byun J, Choi EJ, Lee CJ, Shin HS (2018) Yin-and-yang bifurcation of opioidergic circuits for descending analgesia at the midbrain of the mouse. Proc Natl Acad Sci U S A 115:11078–11083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohno T, Kumamoto E, Higashi H, Shimoji K, Yoshimura M (1999) Actions of opioids on excitatory and inhibitory transmission in substantia gelatinosa of adult rat spinal cord. J Physiol 518 ( Pt 3):803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer TH, Shook JE, Kazmierski W, Ayres EA, Wire WS, Hruby VJ, Burks TF (1989) Novel peptidic mu opioid antagonists: pharmacologic characterization in vitro and in vivo. J Pharmacol Exp Ther 249:544–551. [PubMed] [Google Scholar]
- Kwok CH, Devonshire IM, Bennett AJ, Hathway GJ (2014) Postnatal maturation of endogenous opioid systems within the periaqueductal grey and spinal dorsal horn of the rat. Pain 155:168–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis VA, Gebhart GF (1977) Evaluation of the periaqueductal central gray (PAG) as a morphine-specific locus of action and examination of morphine-induced and stimulation-produced analgesia at coincident PAG loci. Brain Res 124:283–303. [DOI] [PubMed] [Google Scholar]
- Marker CL, Lujan R, Loh HH, Wickman K (2005) Spinal G-protein-gated potassium channels contribute in a dose-dependent manner to the analgesic effect of mu- and delta- but not kappa-opioids. J Neurosci 25:3551–3559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehalick ML, Ingram SL, Aicher SA, Morgan MM (2013) Chronic inflammatory pain prevents tolerance to the antinociceptive effect of morphine microinjected into the ventrolateral periaqueductal gray of the rat. J Pain 14:1601–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan MM, Reid RA, Stormann TM, Lautermilch NJ (2014) Opioid selective antinociception following microinjection into the periaqueductal gray of the rat. J Pain 15:1102–1109. [DOI] [PubMed] [Google Scholar]
- Nunes-de-Souza RL, Graeff FG, Siegfried B (1991) Strain-dependent effects of morphine injected into the periaqueductal gray area of mice. Braz J Med Biol Res 24:291–299. [PubMed] [Google Scholar]
- Pan YZ, Li DP, Chen SR, Pan HL (2004) Activation of mu-opioid receptors excites a population of locus coeruleus-spinal neurons through presynaptic disinhibition. Brain Res 997:67–78. [DOI] [PubMed] [Google Scholar]
- Park C, Kim JH, Yoon BE, Choi EJ, Lee CJ, Shin HS (2010) T-type channels control the opioidergic descending analgesia at the low threshold-spiking GABAergic neurons in the periaqueductal gray. Proc Natl Acad Sci U S A 107:14857–14862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peckys D, Landwehrmeyer GB (1999) Expression of mu, kappa, and delta opioid receptor messenger RNA in the human CNS: a 33P in situ hybridization study. Neuroscience 88:1093–1135. [DOI] [PubMed] [Google Scholar]
- Pelton JT, Kazmierski W, Gulya K, Yamamura HI, Hruby VJ (1986) Design and synthesis of conformationally constrained somatostatin analogues with high potency and specificity for mu opioid receptors. J Med Chem 29:2370–2375. [DOI] [PubMed] [Google Scholar]
- Raffa RB, Mathiasen JR, Jacoby HI (1987) Colonic bead expulsion time in normal and mu-opioid receptor deficient (CXBK) mice following central (ICV) administration of mu- and delta-opioid agonists. Life Sci 41:2229–2234. [DOI] [PubMed] [Google Scholar]
- Rossi GC, Pasternak GW, Bodnar RJ (1994) Mu and delta opioid synergy between the periaqueductal gray and the rostro-ventral medulla. Brain Res 665:85–93. [DOI] [PubMed] [Google Scholar]
- Smith DJ, Perrotti JM, Crisp T, Cabral ME, Long JT, Scalzitti JM (1988) The mu opiate receptor is responsible for descending pain inhibition originating in the periaqueductal gray region of the rat brain. Eur J Pharmacol 156:47–54. [DOI] [PubMed] [Google Scholar]
- Sohn JH, Lee BH, Park SH, Ryu JW, Kim BO, Park YG (2000) Microinjection of opiates into the periaqueductal gray matter attenuates neuropathic pain symptoms in rats. Neuroreport 11:1413–1416. [DOI] [PubMed] [Google Scholar]
- Stevens CW, Seybold VS (1995) Changes of opioid binding density in the rat spinal cord following unilateral dorsal rhizotomy. Brain Res 687:53–62. [DOI] [PubMed] [Google Scholar]
- Sun J, Chen SR, Chen H, Pan HL (2019) mu-Opioid receptors in primary sensory neurons are essential for opioid analgesic effect on acute and inflammatory pain and opioid-induced hyperalgesia. J Physiol 597:1661–1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RC, Mansour A, Akil H, Watson SJ (1993) Cloning and pharmacological characterization of a rat mu opioid receptor. Neuron 11:903–913. [DOI] [PubMed] [Google Scholar]
- Thorn BE, Applegate L, Johnson SW (1989) Ability of periaqueductal gray subdivisions and adjacent loci to elicit analgesia and ability of naloxone to reverse analgesia. Behav Neurosci 103:1335–1339. [DOI] [PubMed] [Google Scholar]
- Vaughan CW, Christie MJ (1997) Presynaptic inhibitory action of opioids on synaptic transmission in the rat periaqueductal grey in vitro. J Physiol 498 (Pt 2):463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Wessendorf MW (2002) Mu- and delta-opioid receptor mRNAs are expressed in periaqueductal gray neurons projecting to the rostral ventromedial medulla. Neuroscience 109:619–634. [DOI] [PubMed] [Google Scholar]
- Weibel R, Reiss D, Karchewski L, Gardon O, Matifas A, Filliol D, Becker JA, Wood JN, Kieffer BL, Gaveriaux-Ruff C (2013) Mu opioid receptors on primary afferent nav1.8 neurons contribute to opiate-induced analgesia: insight from conditional knockout mice. PLoS One 8:e74706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou HY, Chen SR, Chen H, Pan HL (2010) Opioid-induced long-term potentiation in the spinal cord is a presynaptic event. J Neurosci 30:4460–4466. [DOI] [PMC free article] [PubMed] [Google Scholar]