Abstract
Background
Behavior guidance is a technique used to subdue inappropriate behavior by establishing communication that meets the needs of a child. This study aimed to measure the effectiveness of a mobile app (Little Lovely Dentist) compared to the tell-show-do (TSD) technique in managing anxious children during their first dental visit.
Methods
Fifty children (30 boys and 20 girls) without any past dental experience, aged from 7 to 11 years, were randomly allocated into either the dental app group or the TSD group. The pre- and post-operative anxiety of children who underwent prophylactic cleaning was assessed both physiologically and subjectively using a heart rate measurement and the RMS pictorial scale, respectively.
Results
The intragroup comparison of heart rate and RMS scores for children allocated to the dental app group was statistically significant (P value ≤ 0.001). However, a significant reduction only occurred in the RMS scores, but not the heart rate measurements, in the TSD group. Conversely, there was an increase in heart rates in the TSD group.
Conclusion
Educating the child prior to a dental procedure using a smartphone application such as Little Lovely Dentist can significantly alleviate the anticipatory anxiety and engage children in dental treatment during their first visit.
Keywords: Anxiety, Behavior Guidance, Dental Application, First Dental Visit, Tell-Show-Do
INTRODUCTION
Dental anxiety is “an abnormal fear or dreadful feeling of visiting the dentist for preventive care or therapy and unwarranted apprehension over dental procedures.” During their first dental visit, children experience dental anxiety, which has an impact on their future behavior during dental treatment and can lead to dental neglect [1,2].
Dental anxiety is a primary concern for dental care providers, since it can potentially prevent children from seeking dental care and can create a challenging, uncooperative environment for effective treatment [3]. Some children vocalize their fears and anxiety, while others exhibit behaviors such as crying, agitation, cessation of talking or playing, or even attempting to flee. This anxiety is accompanied by a chain of physiological reactions, which in turn leads to significant fluctuations in blood pressure and heart rate [4].
A child's first dental visit is a pivotal moment for the reduction or extension of dental anxiety [5], since they are new to the dental equipment and do not have any previous experience. An unpleasant experience during the child's first visit negatively influences further treatment which in turn can lead to dental anxiety [6,7].
Raadal et al. [8] reported that 19.5% of urban children in the United States aged 5–11 years were found to have high levels of dental anxiety out of a sample of 895. Cuthbert et al. [9] found that the most considerable dental anxiety exists between the ages of 6 and 7 years. Herbertt and Innes [10] found that children aged 8–9 years were the most troubled with dental anxiety and the least cooperative during dental treatment.
The sight of needles and air-turbine drills, the sounds of drilling and screaming, the smell of eugenol and cut dentine, and the sensations of high-frequency vibrations in the dental setting can also trigger anxiety [11]. Treating an anxious patient is stressful for a dentist because reduced cooperation can mean more treatment time and resources will be required, leading to an unpleasant experience for both the patient and the dentist [12]. Thus, anxiety can jeopardize the quality and efficacy of dental care provided to children [13].
Behavior guidance is a teaching technique that requires interactions between the dentist, dental team, patient, and parents. It involves communication and education, which ultimately builds trust and alleviates fear and anxiety [14]. It is the cornerstone of success in pediatric dentistry, since behavior guidance techniques enable children to learn appropriate behavior and coping skills to reduce anxiety, which allows the dentist to deliver effective oral care. Tell-show-do (TSD), modeling, and positive and negative reinforcements are the most frequently used techniques by dentists to alleviate a child's anxiety or fear [15,16]. Of these, pediatric dentists often choose the TSD method, which was introduced by Addelston and relies on the principle of learning theory [17,18].
Currently, children from all age groups interact with mobile phones for playing games, browsing the internet for knowledge, and entertainment. Since dental fear and anxiety is a common problem in children and adolescents worldwide, new strategies are being investigated to manage the challenging situation [19]. Panchal [20] reported that the use of a smartphone application to determine the risk and prevent the development of caries led to a significant improvement in the dietary and oral hygiene habits of the participants.
Ongoing research of mobile apps that are used for behavior guidance has led to the development of virtual reality immersion. This is a promising distraction technique for children since it allows them to adapt to the dental operatory while also allowing for excellent communication between the child and clinician [21,22].
Hence, this clinical trial aimed to evaluate the effectiveness of a mobile app (Little lovely Dentist) compared to the TSD technique in the management of dental anxiety and fear in pediatric patients during their first dental visit.
MATERIALS AND METHODS
1. Source of data
This was a trial with a parallel-arm design and a uniform allocation ratio of 1:1. Clearance for the trial was given by the Institutional Ethical Review Committee (NDC/IECC/PEDO/STS/12-18/07), and the trial was conducted in the department of Pediatric and Preventive Dentistry. Signed informed consent was obtained from the parents or guardians of the children after information about the procedures involved in the study were provided. The study was conducted over a period of one month (September 2019).
We initially examined 218 children aged 7-11 years who visited our department. The sample size was calculated according to the formula . The confidence was 0.95, the probability was 0.05, and a sample size of 46 was obtained. However, considering the risk of subjects dropping out, we selected a sample size of 50 children and recruited them randomly into the trial based on the following inclusion criteria:
1. Children without any prior experience with the dental environment or treatment procedures
2. Children without any systemic or mental disorders.
3. Children whose behavior could be rated as positive (+) or negative (−) based on Wright's modification of the Frankl behavior rating scale [16].
4. Children who were willing to participate in the study.
2. Exclusion criteria
1. Children with systemic or mental disorders.
2. Children or parents who refused to participate in the study
3. Children whose behavior could be rated as definitely positive (++) or definitely negative (−−) according to Wright's modification of the Frankl behavior rating scale [16]
3. Randomization and Blinding
Fifty children were randomly selected and allocated into two groups using block randomization (Group I: dental app, and Group II: TSD) with 25 subjects in each group. The children included in the trial were not aware of the type of educational intervention they were going to receive. To prevent selection bias, the size and order of the blocks were also blinded.
“Little Lovely Dentist” is an application developed by Leaf cottage software and Shanghai Edaysoft Co., Ltd. available on the Google Play Store and App Store, respectively. It can be used for playfully educating children about treatment procedures such as prophylactic cleanings, pit and fissure sealants, restorations, and extractions, while also explaining the importance of oral hygiene maintenance through brushing, especially the interdental areas (Fig. 1 & 2). For the TSD technique, the ‘tell’ phase involves a verbal explanation of the procedure appropriate to the developmental level of the child. In the ‘show’ phase, they become familiar with the treatment armamentarium and a demonstration of the procedure in a carefully defined, non-threatening manner (Fig. 3). Finally, in the ‘do’ phase, the dentist begins the treatment without deviating from the explanation and demonstration for the duration of the procedure as shown in Fig. 4 [14].
Fig. 1. Little Lovely Dentist app.
Fig. 2. Educating a child about the procedure using the dental app.
Fig. 3. Conditioning the child using tell-show-do.
Fig. 4. Performing the oral prophylaxis procedure and recording procedural anxiety using a pulse oximeter.
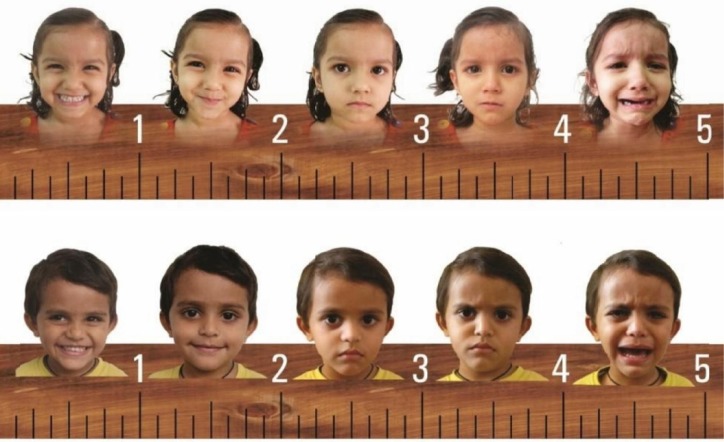
The physiological and subjective measures of the children's anxiety in the operatory period were evaluated and recorded using a pulse oximeter and the RMS pictorial scale, respectively (Fig. 5). The children's preoperative anxiety in both groups was recorded before the initiation of the intervention (during education about the procedure using the dental app or the TSD technique) using both the pulse oximeter and the RMS pictorial scale.
Fig. 5. RMS pictorial scale used for assessing pre- and post-operative anxiety.
Children in the dental app group used the “Little Lovely Dentist” app where they were educated about the prophylactic cleaning procedure. The child was then encouraged to act as a dentist and perform dental treatment virtually on the dental app. Alternatively, the children in the TSD group received information about the prophylactic cleaning procedure through an explanation and demonstration of the instruments in a non-threatening fashion. After conditioning, the children in both groups received prophylactic cleaning by the same trained dentist.
Anxiety levels during the treatment procedure were assessed by recording the heart rate (physiologic measurement) using a portable finger pulse oximeter device. Post-operative anxiety was measured using both a pulse oximeter and the RMS pictorial scale (which is different for male and female children). A single dentist who was blinded to each participant's group allocation recorded both the heart rate and the RMS scores for all the children.
4. Outcomes measured
1. The primary outcome measured was the heart rate, which is a physiological representation of anxiety or fear
2. The secondary outcome measured was the anxiety score using the RMS pictorial scale
5. Statistical methods
All statistical analyses were performed using a standard software (SPSS 20.0 for Windows, SPSS Inc., Chicago, USA). A paired t-test was performed for intergroup and intragroup heart rate comparisons. To analyze the difference in anxiety scores between the two groups according to the RMS scale, the Mann-Whitney test was used. A P value < 0.05 was considered statistically significant.
RESULTS
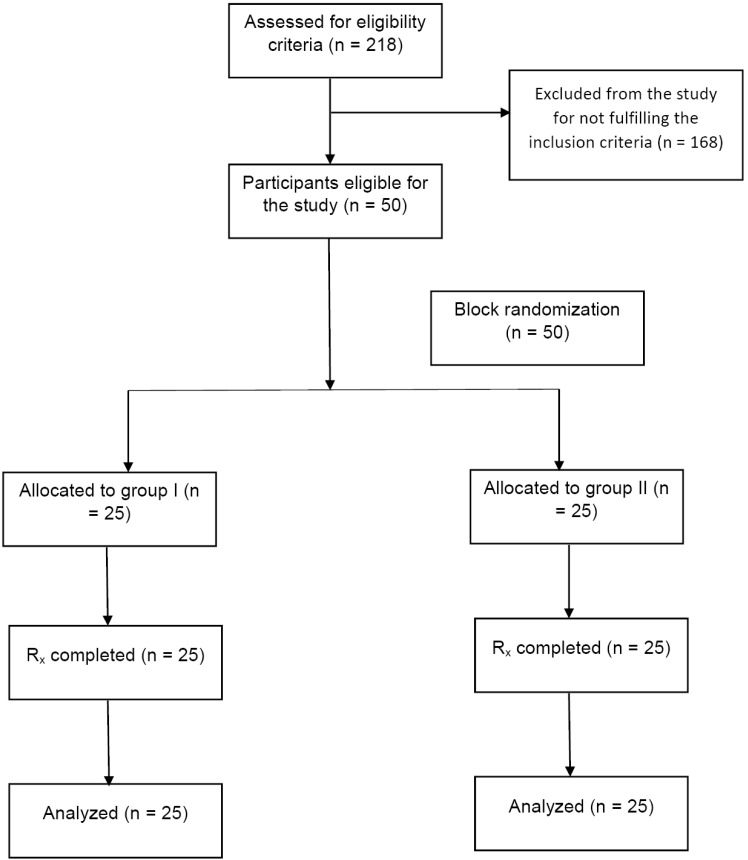
A total of 30 boys and 20 girls were randomly recruited and allocated into two groups, which is represented in the CONSORT flow diagram (Fig. 6). There was an equal distribution of male and female children in both groups (15 boys and 10 girls in each group) (Table 1). The intragroup comparison demonstrated a statistically significant reduction in heart rate for the children recruited to the dental app group at all three points of the procedure: before vs during (P value ≤ 0.001), before vs after (P value ≤ 0.001), and during vs after (P value = 0.007). In contrast, for the children in the TSD group, there was no significant reduction in heart rate (Table 2).
Fig. 6. CONSORT flow diagram of the study design.
Table 1. Demographic distribution of male and female participants.
| Group | Male | Female | Total participants |
|---|---|---|---|
| Group I (Dental app) | 15 | 10 | 25 |
| Group II (TSD) | 15 | 10 | 25 |
TSD: tell-show-do
Table 2. Intragroup comparison of heart rates in the dental app and TSD groups.
| Group | Intragroup comparison | Pulse rate | P-value |
|---|---|---|---|
| Mean ± SD | |||
| Group I (Dental app) | Before vs during | 108.2 ± 12.8 vs 100.4 ± 13.6 | ≤0.001** |
| Before vs after | 108.2 ± 12.8 vs 97.4 ± 12.3 | ≤0.001** | |
| During vs after | 100.4 ± 13.6 vs 97.4 ± 12.3 | 0.007* | |
| Group II (TSD) | Before vs during | 95.9 ± 10.0 vs 98.3 ± 9.3 | 0.106 NS |
| Before vs after | 95.9 ± 10.0 vs 97.2 ± 12.3 | 0.32 NS | |
| During vs after | 98.3 ± 9.3 vs 97.2 ± 9.7 | 0.45 NS |
TSD: tell-show-do; SD: standard deviation; P-value: **Very highly significant; *Significant; NS: Non-significant
The comparison of intragroup subjective anxiety using the RMS scores demonstrated a significant reduction in anxiety (P value ≤ 0.001) for all the children in both groups (Table 3). However, there was no significant difference in the intergroup comparison (Table 4).
Table 3. Intragroup comparison of RMS scores in both groups.
| Group | Dental app group | Mean ± SD | P-value* |
|---|---|---|---|
| Group I (Dental app) | Before the procedure | 3.20 ± 1.04 | ≤ 0.001** |
| After the procedure | 1.32 ± 0.5 | ||
| Before vs after | 3.20 ± 1.04 vs 1.32 ± 0.5 | ||
| Group II (TSD) | Before the procedure | 2.6 ± 0.8 | ≤ 0.001** |
| After the procedure | 1.5 ± 0.6 | ||
| Before vs after | 2.6 ± 0.8 vs 1.5 ± 0.6 |
TSD: tell-show-do; SD: standard deviation; P-value: **Very highly significant
Table 4. Intergroup comparison of heart rates and RMS scores for both groups.
| Parameters | Intergroup comparison | Dental app | TSD | P-value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Pulse rate | Before the procedure | 108.2 ± 12.8 | 95.9 ± 10.0 | ≤ 0.001** |
| During the procedure | 100.4 ± 13.6 | 98.3 ± 9.3 | 0.51 | |
| After the procedure | 97.4 ± 12.3 | 97.2 ± 9.7 | 0.93 | |
| RMS scale | Before the procedure | 3.20 ± 1.04 | 2.6 ± 0.8 | 0.02 |
| After the procedure | 1.32 ± 0.5 | 1.5 ± 0.6 | 0.34 |
RMS: RMS pictorial scale; SD: standard deviation; TSD: tell-show-do; P-value: **Very highly significant
Although there was no significant difference in heart rate measurements between the two groups during the procedure (P value = 0.51) and after the procedure (P value = 0.93), a clear reduction in the mean heart rates was evident in the dental app group. In the TSD group, there was an increase in the mean heart rate during the procedure, which decreased slightly after the procedure was completed (Table 4).
A statistically significant difference in both the physiological and subjective measures of anxiety was demonstrated only in the children who were educated using the dental app. For the children who were educated using the TSD technique, there was a significant difference (P value ≤ 0.001) for the RMS scores but not for the heart rate.
DISCUSSION
For many years, dental anxiety has been recognized as a crucial source of trouble in managing children during dental treatment [23,24]. It can be a major hurdle to adequate dental care and the early detection of pathological processes, which may significantly affect the psychological well-being of the child [25].
Children who are visiting a dentist for the first time often exhibit poor behavior at their appointment [26]. Anxiety during dental treatment can hamper the effective delivery of oral care [27] since it can manifest in diverse ways, often as disruptive or interruptive behaviors [28].
The emotional quality of the first dental visit can have more effect on anxiety than the number of previous visits, since positive dental experiences may lead to less apprehension at future visits [26]. The dental team should provide effective and efficient treatment through instilling a positive attitude in the child during their first dental visit by utilizing appropriate behavior guidance [29]. Most comprehensive approaches aim to help develop communication between the child, dentist, and parents by understanding their cognitive, emotional, and social development [30,31]. Therefore, a comprehensive approach is more beneficial than the individualization of techniques in eventually building trust through alleviating fear and anxiety [14].
TSD is the most common technique for the effective management of children's anxiety at their pretreatment visit. It familiarizes them with new procedures, thus reducing their anticipatory anxiety [32].
In the world Smartphone market, India is the third largest in end users [33]. Research has shown that, in India, the frequency of mobile phone use was 68.6% and the rate of use by children was 56.6%. Rates also show that around 40% of children aged 10 years use a smartphone and this number increases gradually with age [34]. The World Health Organization has proposed the new term mobile Health, which is a component of eHealth, and defined as “medical and public health practice strengthened by mobile devices, such as mobile phones, patient monitoring devices and personal digital assistants” [35]. Therefore, healthcare professionals have been discovering novel ways of providing services and teaching patients using mobile applications designed for use in the medical and dental fields [36]. These applications can be used to reduce patients' anxiety by educating patients about dental treatment and encouraging them to appropriately cope with the treatment [37].
Due to the limited availability of information regarding the use of smartphones in the reduction of anxiety, this study was conducted to assess the efficacy of smartphone applications to reduce anxiety during a child's first dental visit.
Anxiety developed during dental treatment can significantly affect systolic and diastolic blood pressures and heart rates even while the patient maintains a steady oxygen saturation level [38]. Therefore, physiological measures such as heart rate can be utilized to assess dental anxiety appropriately and is a safe physiological measurement to use during dental treatment [39,40].
All the children who participated in the present study exhibited anxiety since they did not have any prior exposure to dental treatment for various reasons. One of the significant reasons could have been exposure to another child or a relative who had an unpleasant dental experience.
A significant reduction in heart rate was elicited only for the children in the dental app group, which indicates a decrease in anxiety levels. This reduction of anticipatory anxiety can be attributed to exposure to the procedure in an interactive, joyful, and playful manner through the dental app called “Little Lovely Dentist.” Another important aspect that may have aided in the reduction of anxiety could have been exposure to the process and the sounds of the procedure during the virtual procedure simulation.
Conversely, the heart rates of the children in the TSD group did not decrease significantly. Even though the children in the TSD group were educated using appropriate language in a non-threatening fashion, it was not playful and interactive, which could have contributed to the increase in heart rate in this group.
The RMS scores decreased for all the children in both the groups, before and after the treatments. The significant decrease in RMS scores in the TSD group can be attributed to the potentially counterproductive effect of elaborate explanation about the dental procedures before the treatment.
According to the results of the present study, in terms of physiological and subjective measures, educating a child using a dental app is an effective method to reduce anticipatory anxiety during their first dental visit compared to the TSD technique. These results are similar to the findings of Patil et al. [41] and Shah et al. [42]. Additionally, Lee et al. [43] claimed that engaging a child with smartphone applications can be a distraction in the behavior guidance technique and suggested that smartphones were modest and effective in reducing preoperative anxiety in children.
A small sample size and unequal distribution of the children's ages can be a possible limitation of this study. Since the treatment in this study was limited to a non-invasive procedure (prophylactic cleaning), future studies with invasive procedures using local anesthesia such as restorations or extractions should be conducted using the dental app as a behavior guidance technique to confirm its efficacy.
From the above interpretations, behavior guidance using a dental app is more effective than TSD in managing the anxiety of a child without any past dental experience by educating him/her about the procedure and virtually simulating the treatments in an interactive manner prior to the treatment. Thus, a dental app is worth utilizing in pediatric dentistry to guide the behavior of children during their first dental visit by reducing their anticipatory anxiety.
ACKNOWLEDGEMENTS
The authors did not receive any financial aid for the purpose, authorship, and/or publication of this research article. The authors declare no conflicts of interest. We are thankful for the children and parents who agreed to participate in this study.
Footnotes
AUTHOR CONTRIBUTIONS: Sainath Reddy Elicherla: Data curation.
Sujatha Bandi Supervision: Writing - review & editing.
Sivakumar Nuvvula: Project administration, Supervision, Writing - review & editing.
Rama Subbareddy Challa: Supervision, Writing - review & editing.
Kanamarlapudi Venkata Saikiran: Conceptualization, Methodology.
Vaka Jeevan Priyanka: Formal analysis, Supervision.
References
- 1.Shetty RM, Khandelwal M, Rath S. RMS Pictorial Scale (RMS-PS): An innovative scale for the assessment of child's dental anxiety. J Indian Soc Pedod Prev Dent. 2015;33:48–52. doi: 10.4103/0970-4388.149006. [DOI] [PubMed] [Google Scholar]
- 2.Rantavuori K, Zerman N, Ferro R, Lahti S. Relationship between children's first dental visit and their dental anxiety in the Veneto Region of Italy. Acta Odontol Scand. 2002;60:297–300. doi: 10.1080/00016350260248274. [DOI] [PubMed] [Google Scholar]
- 3.Roshan NM, Virupaxi SG, Bharath KP, Poornima P, Nagaveni NB, Neena IE. A comparative study of filmed modeling and tell-show-do technique on anxiety in children undergoing dental treatment. J Oral Health Comm Dent. 2018;12:20–24. [Google Scholar]
- 4.Darrow CW. Physiological and clinical tests of autonomic function and autonomic balance. Physiol Rev. 1943;23:1–36. [Google Scholar]
- 5.Milgrom P, Mancl L, King B, Weinstein P. Origins of childhood dental fear. Behav Res Ther. 1995;33:313–319. doi: 10.1016/0005-7967(94)00042-i. [DOI] [PubMed] [Google Scholar]
- 6.Locker D, Shapiro D, Liddell A. Negative dental experiences and their relationship to dental anxiety. Community Dent Health. 1996;13:86–92. [PubMed] [Google Scholar]
- 7.Alwin NP, Murray JJ, Britton PG. An assessment of dental anxiety in children. Br Dent J. 1991;171:201–207. doi: 10.1038/sj.bdj.4807661. [DOI] [PubMed] [Google Scholar]
- 8.Raadal M, Milgrom P, Weinstein P, et al. The prevalence of dental anxiety in children from low-income families and its relationship to personality traits. J Dent Res. 1995;74:1439–1443. doi: 10.1177/00220345950740080201. [DOI] [PubMed] [Google Scholar]
- 9.Cuthbert MI, Melamed BG. A screening device: children at risk for dental fears and management problems. ASDC J Dent Child. 1982;49:432–436. [PubMed] [Google Scholar]
- 10.Herbertt RM, Innes JM. Familiarization and preparatory information in the reduction of anxiety in child dental patients. ASDC J Dent Child. 1979;46:319–323. [PubMed] [Google Scholar]
- 11.Oosterink FM, de Jongh A, Aartman IH. What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting. Eur J Oral Sci. 2008;116:44–51. doi: 10.1111/j.1600-0722.2007.00500.x. [DOI] [PubMed] [Google Scholar]
- 12.Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007;17:391–406. doi: 10.1111/j.1365-263X.2007.00872.x. [DOI] [PubMed] [Google Scholar]
- 13.Li HC, Lopez V. Children's Emotional Manifestation Scale: development and testing. J Clin Nurs. 2005;14:223–229. doi: 10.1111/j.1365-2702.2004.01031.x. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Pediatric Dentistry. Behavior guidance for the pediatric dental patient. Pediatr Dent. 2017;39:246–259. [PubMed] [Google Scholar]
- 15.Wright GZ, Stigers JI. Non-pharmacologic management of children's behaviors. In: Dean JA, Avery DR, McDonald RE, editors. Dentistry for the Child and Adolescence. 9th ed. St. Louis: CV Mosby Co.; 2011. pp. 30–31. [Google Scholar]
- 16.Townsend JA. Behaviour guidance of the paediatric dental patient. In: Casa Massimo PS, Fields HW, McTigue DJ, Nowak AJ, editors. Paediatric Dentistry: Infancy through Adolescence. 5th ed. Philadelphia: Elsevier Saunders; 2013. p. 358. [Google Scholar]
- 17.Addleston HK. Child patient training. Fortnightly Rev Chicago Dental Soc. 1959;38:27–29. [Google Scholar]
- 18.Fields HW, Jr, Machen JB, Murphy MG. Acceptability of various management techniques relative to types of dental treatment. Ped Dent. 1984;6:199–203. [PubMed] [Google Scholar]
- 19.Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, Montedori A, et al. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017;18:121–130. doi: 10.23804/ejpd.2017.18.02.07. [DOI] [PubMed] [Google Scholar]
- 20.Panchal V, Gurunathan D, Shanmugaavel AK. Smartphone application as an aid in determination of caries risk and prevention: A pilot study. Eur J Dent. 2017;11:469–474. doi: 10.4103/ejd.ejd_190_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nuvvula S, Alahari S, Kamatham R, Challa RR. Effect of audiovisual distraction with 3D video glasses on dental anxiety of children experiencing administration of local analgesia: a randomised clinical trial. Eur Arch Paediatr Dent. 2015;16:43–50. doi: 10.1007/s40368-014-0145-9. [DOI] [PubMed] [Google Scholar]
- 22.Nunna M, Dasaraju RK, Kamatham R, Mallineni SK, Nuvvula S. Comparative evaluation of virtual reality distraction and counter-stimulation on dental anxiety and pain perception in children. J Dent Anesth Pain Med. 2019;19:277–288. doi: 10.17245/jdapm.2019.19.5.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Milgrom P, Weinstein P, Kleinknecht R, Getz T. Treating fearful dental patients: a clinical handbook. New York: Appleton; 1985. [Google Scholar]
- 24.Chellappah NK, Vignehsa H, Milgrom P, Lam LG. Prevalence of dental anxiety and fear in children in Singapore. Community Dent Oral Epidemiol. 1990;18:269–271. doi: 10.1111/j.1600-0528.1990.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 25.Davila JM, Menendez J. Relaxing effects of music in dentistry for mentally handicapped patients. Spec Care Dentist. 1986;6:18–21. doi: 10.1111/j.1754-4505.1986.tb00943.x. [DOI] [PubMed] [Google Scholar]
- 26.Wright GZ, Alpern GD. Variables influencing children's co-operative behaviour at first dental visit. ASDC J Dent Child. 1971;38:124–128. [PubMed] [Google Scholar]
- 27.Aartman IH, Hoogstraten J, Schuurs AH. Self-report measurements of dental anxiety and fear in children: a critical assessment. ASDC J Dent Child. 1998;65:252–258. [PubMed] [Google Scholar]
- 28.Ayer WA, Jr, Domoto PK, Gale EN, Joy ED, Jr, Melamed BG. Overcoming dental fear: strategies for its prevention and management. J Am Dent Assoc. 1983;107:18–27. doi: 10.14219/jada.archive.1983.0184. [DOI] [PubMed] [Google Scholar]
- 29.Wright GZ, Strakey PE, Gardner DE. Managing Children's behavior in the dental office. St. Louis: Mosby; 1983. [Google Scholar]
- 30.Feigal R. Pediatric behavior management through nonpharmacologic methods. Gen Dent. 1995;43:327–332. [PubMed] [Google Scholar]
- 31.Rosenberg HM. Behavior modification for the child dental patient. ASDC J Dent Child. 1974;41:111–114. [PubMed] [Google Scholar]
- 32.McKnight-Hanes C, Myers DR, Dushku JC, Davis HC. The use of behaviour management techniques by dentists across practitioner type, age, and geographic region. Pediatr Dent. 1993;15:267–271. [PubMed] [Google Scholar]
- 33.Vellody A, Sarda K, Pratap R, Thota H. Mobile Social Media, Proceedings of Mobile India, 6th International conference on COMmunication and NETwork. Jan 7–10; 2014. [Last accessed on 08-11-2019]. from URL: https://www.comsnets.org/archive/2014/doc/MI%202014_Session%204_Ashvin%20Vellody.pdf.
- 34.Children's use of mobile phones-An international comparison Published in 2010 by the GSM Association and the Mobile Society Research Institute within NTT DOCOMO Inc, Japan, 2011. [Google Scholar]
- 35.Vardeh D, Edwards RR, Jamison RN, Eccleston C. There's an app for that: mobile technology - Is a new advantage in managing chronic pain. Pain Clin Updates. 2013;21:1–8. [Google Scholar]
- 36.Khatoon B, Hill KB, Walmsley AD. Instant message in dental education. J Dent Educ. 2015;79:1471–1478. [PubMed] [Google Scholar]
- 37.Alklayb SA, Assery MK, Alqahtani A, Alanazi M, Pani SC. Comparison of the effectiveness of a mobile phone-based education program in educating mothers as oral health providers in two regions of Saudi Arabia. J Int Soc Prev Community Dent. 2017;7:110–115. doi: 10.4103/jispcd.JISPCD_95_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Myers DR, Kramer WS, Sullivan RE. A study of the heart action of the child dental patient. ASDC J Dent Child. 1972:99–106. [PubMed] [Google Scholar]
- 39.Pinkham JR. Fear of dentistry: a discussion of its usefulness to certain child dental patients. ASDC J Dent Child. 1983;50:111–113. [PubMed] [Google Scholar]
- 40.Simpson WJ, Ruzicka RL, Thomas NR. Physiologic responses of children to initial dental experience. ASDC J Dent Child. 1974;41:465–470. [PubMed] [Google Scholar]
- 41.Patil VH, Vaid K, Gokhale NS, Shah P, Mundada M, Hugar SM. Evaluation of effectiveness of dental apps in management of child behaviour: A pilot study. Int J Pedod Rehabil. 2017;2:14–18. [Google Scholar]
- 42.Shah HA, Nanjunda Swamy KV, Kulkarni S, Choubey S. Evaluation of dental anxiety and hemodynamic changes (Sympatho-Adrenal Response) during various dental procedures using smartphone applications v/s traditional behaviour management techniques in pediatric patients. Int J Appl Res. 2017;3:429–433. [Google Scholar]
- 43.Lee JH, Jung HK, Lee GG, Kim HY, Park SG, Woo SC. Effect of behavioral intervention using smartphone application for preoperative anxiety in pediatric patients. Korean J Anesthesiol. 2013;65:508–518. doi: 10.4097/kjae.2013.65.6.508. [DOI] [PMC free article] [PubMed] [Google Scholar]