Abstract
The 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol retains focus on recommendations for statin treatment in the original four statin-eligible groups (those with atherosclerotic cardiovascular disease [ASCVD], diabetes, LDL-C ≥190 mg/dL, and higher risk primary prevention) without the use of treatment initiation or target LDL-C levels from the earlier 2013 ACC/AHA guideline, but has several new features. First, patients with primary prevention are divided into those who are at low (<5%), borderline (5-<7.5%), intermediate (7.5-<20%), and high (≥20%) risk based on the atherosclerotic cardiovascular disease (ASCVD) risk estimator. Moreover, the new guideline goes further to consider a wider range of factors (now called “risk enhancers”—premature family history of ASCVD, persistently high LDL-C, chronic kidney disease, metabolic syndrome, conditions specific to women, inflammatory diseases, and high risk ethnicities) that can be used to better inform the treatment decision. Moreover, more detailed recommendations on how the results of coronary calcium scanning can be used to inform the treatment decision are provided, including how it may be used to “de-risk” certain patients for delaying or avoiding the use of statin therapy. There are also specific sections for cholesterol management in other patient subgroups including women, children, certain ethnic groups, those with chronic kidney disease (CKD), chronic inflammatory disorders and HIV, as well as discussing the management of hypertriglyceridemia. Importantly, for persons with known ASCVD, a distinction is made for those who are at “very high risk” based on having had two major ASCVD events or one major event and two or more other high risk conditions, such as diabetes or other major risk factors, or bypass surgery or percutaneous intervention. Finally, the concept of a threshold LDL-C for initiating a non-statin therapy (after considering highest tolerated statin dosage) is provided with ezetimibe recommended as the key non-statin to be added if the LDL-C still remains ≥70 mg/dL for all ASCVD patients, and in those who are at “very high risk”, further consideration for using a PCSK9 inhibitor. While the new guideline does have greater detail (and arguably complexity), the refinements provide a strategy for guiding the clinician to target both statin and non-statin therapy to those most likely to derive benefit.
Keywords: cholesterol, dyslipidemia, guideline, statins, treatment
1. Introduction
The most recent 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol (1) is a substantial collaborative effort among key societies, including authorship from the American Society for Preventive Cardiology (ASPC). While it still retains focus on recommendations for statin treatment in the original four statin-eligible groups from the earlier 2013 ACC/AHA guideline (2), the new guideline goes further to consider a wider range of factors (now called “risk enhancers”) that can be used to better inform the treatment decision, and addresses implications of treatment for other patient subgroups including women, children, certain ethnic groups, those with chronic kidney disease (CKD), chronic inflammatory disorders and HIV, as well as discussing the management of hypertriglyceridemia. Given that its foundations (e.g., focus on statin therapy recommendations and absence of specific initiation or target levels of LDL-C) are not substantially different from the 2013 release, it has attracted far less attention and controversy compared to its predecessor.
At the recent American College of Cardiology Scientific Sessions in March 2019 the revised Primary Prevention of Cardiovascular Disease Guidelines (3) were also presented. These were the first such release focusing on primary prevention in more than a decade and were intended to be a compendium of the recent cholesterol and blood pressure guidelines with an update on lifestyle management, and this time also included guidelines for smoking cessation and updated aspirin guidelines to promote disease prevention as a cornerstone of cardiovascular medicine. They included the primary prevention part of the 2018 cholesterol guidelines release. Central to the Primary Prevention of Cardiovascular Disease Guidelines and relevant to cholesterol management is the strong recommendation for patient centered approaches for comprehensive atherosclerotic cardiovascular disease (ASCVD) prevention, including a team-based approach for control of risk factors for ASCVD (Class I recommendation), shared decision making to guide discussions about the best strategies to reduce ASCVD risk (Class I recommendation), and use of social determinants of health to inform optimal implementation of treatment recommendations for prevention of ASCVD (Class I recommendation).
There are some key similarities and differences between the 2013 and 2018, guidelines. Importantly, the 2018 guidelines have kept the original four key statin eligible groups: those with (1) documented atherosclerotic cardiovascular disease (ASCVD), (2) LDL-C ≥190 mg/dl, (3) diabetes, and (4) increased ASCVD risk requiring primary prevention. Within these groups, however, there are further refinements (and arguably, greater complexity) as to the specific recommended therapy needing explanation. Moreover, the clinician/ patient discussion, which was a hallmark of the 2013 guidelines, especially with the use of the risk calculator, is even more important with the introduction of additional “risk enhancers” as well as a greater role for use of results from coronary calcium screening, not only for informing the decision to treat, but also for the first time, identifying patients where perhaps treatment can be withheld or delayed.
2. Lifestyle Management
This remains the cornerstone for prevention of cardiovascular disease and, crucially, a healthy lifestyle is the primary overarching recommendation for all statin eligible patient groups in the cholesterol management guideline. As is the case with the 2013 Lifestyle Management Guideline (4), the recent 2019 Prevention Guidelines also recommend a dietary pattern comprised of increased intake of vegetables, fruits, whole grains, legumes, healthy protein sources, and non-tropical vegetable oils (Class I recommendation), while limiting intake of sweets, sugar-sweetened beverages, and red meats (Class IIa recommendation). Physical activity recommendations state 150 minutes of moderate intensity or 75 minutes of vigorous intensity physical activity per week (or equivalent combination) to reduce ASCVD risk (Class I recommendation).
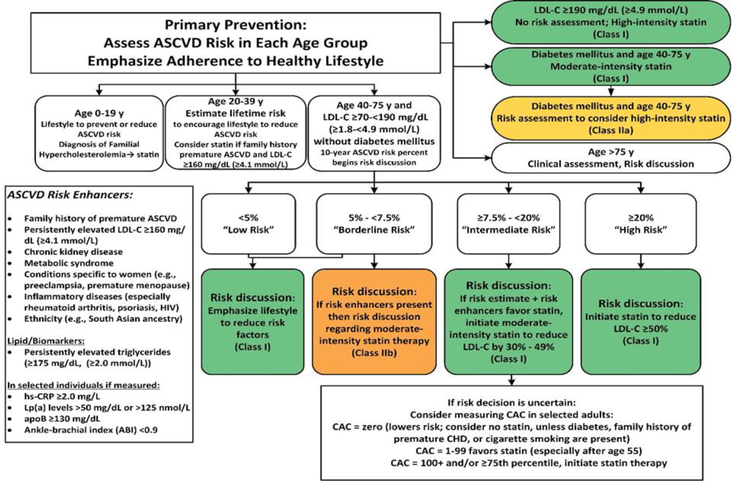
3. Primary Prevention
As in the 2013 guideline, the 2018 cholesterol management guideline divides primary prevention into those with LDL-C of ≥190 mg/dl, persons with diabetes (see section below), and individuals without these conditions. A more detailed algorithm, however, is presented (Figure 1) than what was released in 2013, now with recommendations to consider a statin in those <20 years of age with a diagnosis of familial hypercholesterolemia, or 20–39 years of age with premature family history of ASCVD or LDL-C ≥160 mg/dl (Class IIa recommendation). In those with severe hypercholesterolemia (LDL-C ≥190 mg/dl), high intensity statin is still the key recommendation, without the need for any risk calculation (Class I recommendation). Further, in those achieving less than 50% reduction in LDL-C on maximally tolerated statin and/or with residual LDL-C ≥100 mg/dl, adding ezetimibe is reasonable (Class IIa recommendation). And for those with heterozygous familial hypercholesterolemia, use of PCSK9 inhibitors can be considered if the LDL-C remains ≥100 mg/dl after use of statin and ezetimibe (Class IIb recommendation).
Figure 1.
Primary Prevention Algorithm for Cholesterol Management. Adapted from Grundy et al. (2); reproduced with permission from Medtelligence, Inc.
3.1. ASCVD Risk Categorization and Risk Enhancers
General primary prevention without diabetes or severe hypercholesterolemia starts with 10-year ASCVD risk estimation using the Pooled Cohort Risk Estimator (which is valid for those aged 40–79 years of age) (Class I recommendation), but now subdivides risk categories as follows: low (<5%), borderline (5-<7.5%), moderate (7-<20%), and high (≥20%) of a hard ASCVD event, including myocardial infarction and stroke. Unlike the 2013 guidelines in which one was statin-eligible if the 10-year ASCVD risk was ≥7.5%, the updated guidelines more clearly note the appropriateness of lifestyle only for persons with 10-year ASCVD risk < 5%, and statin therapy to reduce LDL-C at least 50% plus lifestyle therapy for those with a 10-year risk ≥20%. For those with a 10-year risk of ASCVD between 5% and 20%, a larger number of “risk enhancers” is introduced (Figure 1), which should be considered in the clinician/patient discussion concerning the pertinence of statin therapy (Class IIa recommendation). This is an update from the four factors introduced in 2013—premature family history of ASCVD, coronary calcium score ≥300 or ≥75th percentile, high sensitivity CC-reactive protein >2 mg/L, or an ankle brachial index <0.9, which were proposed then to inform the treatment decision. The inclusion of conditions specific to women (e.g., premature menopause, pre-eclampsia), inflammatory diseases, chronic kidney disease, and certain high-risk ethnicities (e.g., South Asians) to inform the treatment decision, is particularly welcome. However, it is not clear whether any single condition in the case of someone in the 5% to <20% risk level automatically makes the person statin eligible, although arguably a severe elevation in any one risk factor would stratify one’s risk upward to justify statin therapy. As such, this judgement is up to the clinician who may consider both number and severity of any risk enhancers present when discussing with the patient the risks and benefits of starting or intensifying statin therapy.
3.2. Role of Coronary Artery Calcium Screening
Perhaps the most noticeable addition to the 2018 guidelines for the primary prevention patient is the role of coronary calcium scoring in risk assessment and treatment decisions In the new guidelines, rather than being one of four factors used to inform treatment decisions indecisions previous guidelines, results from coronary calcium scoring are recommended if the treatment decision is still uncertain after considering the risk enhancing factors described above, and only for those in the borderline (5-<7.5%) and intermediate (7.5-<20%) 10-year risk categories (Class IIa recommendation) where the results of coronary calcium can be used to withhold, postpone, or initiate statin therapy, based on published evidence of its utility in providing further risk stratification over the Pooled Cohort Risk Scores (5). This is an upgraded recommendation from 2013 where CAC scoring was given a class IIb recommendation. In the case of the new guidelines, for the first time, a zero calcium score is identified as a rationale for withholding or delaying statin therapy (unless there is a family history of premature CHD, diabetes, or cigarette smoking), a score of 1–99 “favors” statin therapy, and a score of ≥100 or ≥75th percentile for age and sex is an impetus for statin therapy (the previous 2013 guideline did not recommend coronary calcium to upgrade risk unless the score was ≥300 or ≥75th percentile, nor was there any recommendation to de-risk the patient if the score was 0). The “de-risking” of those with a 0 calcium score is a particularly bold move, supported mainly by observational data from the MESA study, noting those with a 0 score to have an ASCVD risk below the 7.5% threshold where net clinical benefit was demonstrated in the 2013 guidelines and where in these persons the number needed to treat to prevent a CHD event is excessive (5).
4. Diabetes Mellitus
As in the prior 2013 guideline, the 2018 guidelines recommend at least a moderate intensity statin for all persons aged 40–79 years with diabetes mellitus (DM) (Class I recommendation), and now without the previously specified LDL-C range of 70–189 mg/dl for initiating a statin. There is continued emphasis on use of the risk calculator for identifying those at highest risk indicated for more intensive statin therapy (Class IIa recommendation). However, in considering a high intensity statin, instead of being uniformly recommended for those with ≥7.5% risk, the new guideline suggests this would be appropriate for those with DM who have two or more risk factors, with ezetimibe is now a consideration (with high intensity statin therapy) for those with ≥20% 10-year ASCVD risk (Class IIb recommendation). It should be noted, that while ezetimibe provided additional benefit beyond statin therapy among persons with DM in the IMPROVE-IT trial (6), this was of course in addition to all enrollees having a recent (<10 days) acute coronary syndrome as the primary inclusion criterion.
4.1. Younger persons with DM
New to the 2018 guidelines for DM management is consideration of statin therapy for those under age 40 years for those who have had Type 1 DM for at least 20 years or Type 2 DM for at least 10 years, CKD, albuminuria, retinopathy, neuropathy, or an ABI <0.9, although only with a Class IIb recommendation. In fact, Rana and colleagues (7) recently showed those with DM for more than 10 years can be considered a coronary heart disease risk equivalent.
4.2. Coronary Calcium Screening in Diabetes
While CAC as a risk enhancing factor is not mentioned here for persons with DM (although a CAC score of 0 is not recommended for de-risking a patient who has DM), CAC has been shown to be a robust risk stratifier in patients with DM where it has been previously shown that those with CAC scores of ≥400 have 10 times the risk of CHD events as those with scores of 0 (8). Moreover, a CAC score of ≥100 indicates an ASCVD risk of at least 2% per year (e.g., 20% in 10-years) based on longer follow-up in a more recent paper (9), where like with those with a >20% 10-year ASCVD risk as noted in the guidelines, a high intensity statin therapy with ezetimibe if needed could be potentially recommended. And for those with Type 1 DM, the Epidemiology of Diabetes Interventions and Complications study recently showed that CAC significantly improves risk prediction for ASCVD events (10).
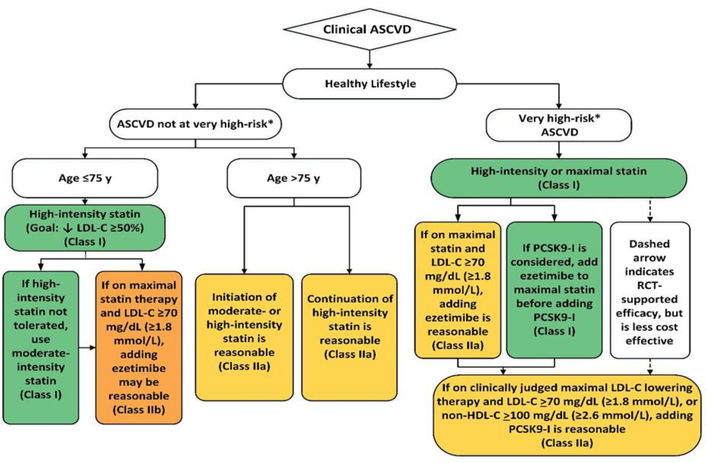
5. Secondary Prevention
5.1. New “Very High Risk” Categorization
The most important change to the recommendations for treatment of persons with pre-existing ASCVD is the categorization of those at versus not at “very high risk” (Figure 2). Those at very high risk are defined specifically as those with multiple major ASCVD events (recent acute coronary syndrome [ACS] within the past 12 months, history of myocardial infarction (other than recent ACS within 12 months), history of ischemic stroke, symptomatic peripheral arterial disease, or one of these major ASCVD events and multiple high risk conditions consisting of one of the following: age ≥65 years, heterozygous familial hypercholesterolemia, history of prior coronary artery bypass graft (CABG) or percutaneous coronary intervention (PCI), hypertension, CKD based on an eGFR of 15–59 mL/min/1.73 m2, current smoking, persistently elevated LDL-C ≥100 mg/dL despite maximally tolerated statin ± ezetimibe, or a history of congestive heart failure (Table). The intent here is to identify those at greatest absolute risk who would derive the greatest absolute risk reduction from the addition of non-statin therapies. Similarly, those with stable ASCVD for year that have well-treated risk factors may accrue only modest additional benefit from these therapies. While in most cases such a categorization would identify those at highest risk, one could argue that certain situations may warrant greater clinical judgment to decide whether a patient is very high risk or not. For instance, the individual with a recent ACS who has heterozygous familial hypercholesterolemia only might be actually considered by some to be “very high risk” although would by the current guideline be classified as “not as very high risk” due to not having multiple high risk conditions in addition to the single major ASCVD event. And conversely, someone with a prior myocardial infarction, who had a PCI, stabilized for 5 years and with mild hypertension would technically fall in the very high-risk group, but might actually be considered by some to be at lower risk than the example above. Again, the clinician needs to consider carefully the severity as well as timing (more recent would suggest higher risk) of both these major ASCVD events and high risk conditions.
Figure 2.
Cholesterol Management Algorithm for Secondary Prevention
Adapted from Grundy et al. (2); reproduced with permission from Medtelligence, Inc.
Table.
Criteria for Very High Riska Classification in Persons with Known Atherosclerotic Cardiovascular Disease (ASCVD)
| Major ASCVD Events |
| Recent ACS (within the past 12 months) |
| History of MI (other than recent ACS event listed above) |
| History of ischemic stroke |
| Symptomatic PAD (history of claudication with ABI <0.85, or previous revascularization or amputation) |
| High-Risk Conditions |
| Age ≥65 years |
| Heterozygous familial hypercholesterolemia |
| History of prior CABG or PCI outside of the major ASCVD event(s) |
| Diabetes mellitus |
| Hypertension |
| CKD (eGFR 15–59 mL/min/1.73 m2) |
| Current smoking |
| Persistently elevated LDL-C (LDL-C ≥100 mg/dL [≥2.6 mmol/L]) despite maximally tolerated statin therapy and ezetimibe |
| History of congestive HF |
Very High-Risk is defined as multiple major ASCVD events or one major ASCVD event and multiple high risk conditions. Adapted from Grundy et al. (2)
ABI ankle-brachial index, ACS acute coronary syndromes, CABG coronary artery bypass graft surgery, CKD chronic kidney disease, eGFR estimated glomerular filtration rate, HF heart failure, LDL-C low density lipoprotein-cholesterol, PAD peripheral arterial disease, PCI percutaneous coronary intervention.
5.2. Use of LDL-C Thresholds
Rather than the use of targets for initiation of therapy, the new guidelines note specific “thresholds” for LDL-C levels for when to initiate certain non-statin therapies. For instance, in those not at very high risk, ezetimibe (although only a class IIb recommendation) is given and only if high intensity statin does not lower the LDL-C below 70 mg/dL. In those at very high-risk the initiation of ezetimibe is considered at a threshold LDL-C of 70 mg/dL on maximal statin therapy. A PCSK9 monoclonal antibody (mAb) is only considered (as a class IIa recommendation) after adding ezetimibe to maximal statin therapy if the LDL-C is still ≥70 mg/dL or non-HDL-C ≥100 mg/dl. While the decision to consider ezetimibe more broadly than the population studied in IMPROVE-IT (recent ACS within 10 days) may in part be due to its generic status, the opposite may be the case for the PCSK9 mAb therapies being recommended now to a more limited “very high risk” ASCVD patient population, which is narrower than the more heterogenous ASCVD population studied in FOURIER and ODYSSEY trials, possibly because of the high cost of these products, which were not discounted substantially until the guidelines were already finalized.
6. Hypertriglyceridemia
Unlike the 2013 guidelines, the updated 2018 guidelines give specific guidance for persons with hypertriglyceridemia. While lifestyle management remains the emphasis for most persons with moderate hypertriglyceridemia, those with more elevated triglycerides (≥500 mg/dL) are considered as candidates for other measures such as statin therapy (among those aged 40–75 years with 10-year ASCVD risk of ≥7.5%) (class IIa recommendation) as well as consumption of omega-3 fatty acids, a very low-fat diet, avoidance of refined carbohydrates and alcohol, and, if needed, fibrate therapy to prevent acute pancreatitis (class IIa recommendation). However, since the guidelines were written, the landmark results of the REDUCE-IT trial (11) demonstrated the value of icosapent ethyl in reducing ASCVD events by a remarkable 25% beyond statin therapy in persons with known ASCVD or diabetes and at least 1 risk factor who had triglycerides of 135–400 mg/dL. Further clinical trial evidence, such as results pending from the ongoing trials of other omega-3 fatty acid preparations and fibrates may influence future guideline releases regarding the use of non-statin therapies. Of note, however, the 2019 American Diabetes Association Standards of Medical Care have now updated their recommendations for consideration of icosapent ethyl for persons with diabetes who have ASCVD or other risk factors with a class A recommendation (12).
7. Other Special Populations
The 2018 guideline has notably gone further than its predecessor in addressing appropriateness of statin therapy for other patient populations besides the original four statin eligible groups. Additional specific guidance is now provided for older persons, children and adolescents, high risk ethnic groups, women, persons with CKD, and persons with chronic inflammatory conditions, including HIV.
7.1. Older Persons
As in the prior guidelines, it is noted in persons aged 75 years and over, that starting with a moderate intensity statin is reasonable (class IIa recommendation). The updated 2019 guideline, however, recommends stopping a statin in cases of functional decline, multimorbidity, frailty, or reduced life expectancy, because such conditions may limit the potential benefits of the statin (class IIa recommendation). And for the first time, in those aged 76–80 years of age, a CAC scan is noted to be reasonable to identify those with a 0 calcium score where statin therapy may be withheld (class IIa recommendation).
7.2. Children and Adolescents
In children and adolescents, it is recommended that lipids as early as age 2 years can be used to identify FH in those with a family history of early ASCVD or significant hypercholesterolemia, and consideration should be given to measure lipids at least once between the ages of 9 and 11 in all others. Further, statin use is recommended in those at least age 10 with an LDL-C of ≥190 mg/dL, or LDL-C is ≥160 with a clinical history consistent with familial hypercholesterolemia (class IIa recommendation).
7.3. High Risk Ethnicities
For the first time, guidance is given to consider adjusting statin dosages according to race/ethnic features which include differences in lipids and genetic polymorphisms in hepatic clearance pathways between Asian, South Asian, African-Americans, and Hispanics. The importance of taking into account racial/ethnic preferences in heart-healthy diet counseling also noted (class IIa recommendation).
7.4. Women
Of interest, the new guidelines give specific guidance to better inform treatment decisions in women, especially among those with early menopause or certain pregnancy-related conditions such as preeclampsia are considered, all of which correlate with increased cardiovascular risk enhancers that favor statin treatment where there is uncertainty (class I recommendation). Additional guidance is also given to those who are sexually active or plan to become pregnant.
7.5. Chronic Kidney Disease and Dialysis
For the first time the ACC/AHA guidelines provide guidance for persons with CKD not receiving dialysis. Among such patients with CKD aged 40–75 years of age with an LDL-C of 70–189 mg/dL, treatment with a moderate intensity statin alone or in combination with ezetimibe may be appropriate (Class IIa recommendation). Among those with CKD and on dialysis, while it is not appropriate to start a statin, a statin can be continued among those already on a statin or if they also have ischemic heart disease.
7.6. Chronic Inflammatory Conditions and HIV
Finally, addition to the current guidelines are recommendations for those with chronic inflammatory conditions and HIV. In such persons aged 40–75 with an LDL-C of 70–189 mg/dL, a moderate or high intensity statin is favored (Class IIa recommendation). In addition, a fasting lipid profile should be performed before and after starting any anti-inflammatory or antiretroviral therapy.
8. Economic Value Considerations
The new guidelines also noted in patients with ASCVD that the use of PCSK9 mAbs provides mAbs provides a “low cost value” based on mid-2018 list prices where costs exceeded $150,000 per quality adjusted life year (QALY) saved, with <$50,000 per QALY considered to be good cost value. For those with familial hypercholesterolemia without ASCVD, the cost value is uncertain. Since the publication of these guidelines, however, there have been dramatic cost reductions of approximately 60% in both of the PCSK9 mAb therapies, which based on the cost-effectiveness analysis done by the guideline authors, would amount to costs per QALY much lower, but not below the $50,000 threshold, where further discounts would likely be needed. Such estimates of economic value, however, are highly dependent on the method of analysis, type of patients and duration of treatment. For example, the FOURIER trial has shown greater absolute benefit in certain types of patients such as those with peripheral artery disease, multiple prior MI’s, more recent MI, and those with multiple high-risk features as well as duration of treatment, and likewise ODYSSEY outcomes trial showed a greater benefit in those with baseline LDL-C ≥100 mg/dL (13). It is likely that reserving these drugs for those at highest risk (e.g., the “very high risk” subgroup of ASCVD patients) and only after the incremental addition of ezetimibe, as noted in the updated guidelines, is due to these cost considerations and the greater clinical efficacy (e.g., lowest number needed to treat) in those at highest risk.
9. Conclusions
The new multi-society cholesterol management guidelines provide further useful guidance for both the appropriate application of well-grounded statin therapy in primary prevention, as well as which patients should be considered for receive non-statin therapies, particularly ezetimibe and PCSK9 mAbs given their proven efficacy for incremental ASCVD risk reduction in certain populations. It has also landmark for providing recommendations for a broad range of special populations, particularly ethnic groups, women, children and adolescents, and those with CKD and chronic inflammatory conditions and HIV. Additional updates will likely consider not only the changing landscape with respect to new evidence-based therapies for reduction of ASCVD risk (e.g., icosapent ethyl and other emerging therapies), but also changing costs of newer medications (e.g., PCSK9 mAb therapies) as well as emerging risk enhancing measures that significantly impact treatment decisions.
Key Points.
The 2018 Guideline on the Management of Blood Cholesterol provides greater risk stratification for primary prevention, considering the use of a wide range of risk enhancers and detailed recommendations on how results from coronary calcium scoring can be used to better inform the treatment decision.
Specific guidelines are provided for cholesterol management in women, children, older persons, those with inflammatory conditions or HIV, as well as hypertriglyceridemia.
Persons with known ASCVD are classified according to whether they are at “very high risk” based on having multiple ASCVD events or a single event with other high risk conditions, with threshold LDL-C levels noted for the consideration of non-statin therapy.
Acknowledgments
FUNDING: No external funding was used in the preparation of this manuscript.
Footnotes
CONFLICT OF INTEREST:
Nathan D. Wong, PhD has received research support through the University of California, Irvine from Amgen, Amarin, Novo Nordisk, and Boehringer Ingelheim, speaking fees from Amarin and Sanofi, and consulting from Amarin and Novartis. Peter Toth, MD, PhD notes speaking fees from Amarin, Amgen, Kowa, Nova Nordisk, Regeneron, and Sanofi and consultant/advisory board for Amarin, Amgen, Kowa, Nova Nordisk, Regeneron, and Sanofi. Christie Ballantyne, MD has received speaking fees from Akcea, Amgen, Esperion, Novartis, Regeneron, Sanofi-Synthelabo (all paid to institution, not individual); Consulting fees or honorarium from Akcea, Amarin, Amgen, Arrowhead, AstraZeneca, Boehringer Ingelheim, Esperion, Intercept, Janssen, Matinas BioPharma Inc., Merck, Novartis, Novo Nordisk, Regeneron, and Sanofi-Synthelabo. Ezra A. Amsterdam, MD, Amit Khera, MD, and Khurram Nasir, MD, MPH, declare no potential conflicts of interest that might be relevant to this manuscript.
COMPLIANCE WITH ETHICAL STANDARS: Not applicable (this is a review paper)
REFERENCES
- 1.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, et al. 2018. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2018 November 10:CIR0000000000000625. doi: 10.1161/CIR.0000000000000625. [Epub ahead of print]. [DOI] [Google Scholar]
- 2.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH,et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014. July 1;63(25 Pt B):2889–934. doi: 10.1016/j.jacc.2013.11.002. Epub 2013 Nov 12. Erratum in: J Am Coll Cardiol. 2015 Dec 22;66(24):2812. J Am Coll Cardiol. 2014 Jul 1;63(25 Pt B):3024–3025. [DOI] [PubMed] [Google Scholar]
- 3.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ,et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019. March 17. pii: S0735–1097(19)33876–8. doi: 10.1016/j.jacc.2019.03.009. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014. July 1;63(25 Pt B):2960–84. doi: 10.1016/j.jacc.2013.11.003. Epub 2013 Nov 12. Erratum in: J Am Coll Cardiol. 2014 Jul 1;63(25 Pt B):3027–3028. [DOI] [PubMed] [Google Scholar]
- 5.Nasir K, Bittencourt MS, Blaha MJ, Blankstein R, Agatson AS, Rivera JJ, et al. Implications of Coronary Artery Calcium Testing Among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2015. October 13;66(15):1657–68. doi: 10.1016/j.jacc.2015.07.066. Erratum in: J Am Coll Cardiol. Dec 15;66(23):2686. Miemdema, Michael D [corrected to Miedema, Michael D]. [DOI] [PubMed] [Google Scholar]
- 6.Giugliano RP, Cannon CP, Blazing MA, Nicolau JC, Corbalán R, Špinar J, et al. ; IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) Investigators. Benefit of Adding Ezetimibe to Statin Therapy on Cardiovascular Outcomes and Safety in Patients With Versus Without Diabetes Mellitus: Results From IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial). Circulation. 2018. April 10;137(15):1571–1582. doi: 10.1161/CIRCULATIONAHA.117.030950. Epub 2017 Dec 20. [DOI] [PubMed] [Google Scholar]
- 7.Rana JS, Liu JY, Moffet HH, Jaffe M, Karter AJ. Diabetes and Prior Coronary Heart Disease are Not Necessarily Risk Equivalent for Future Coronary Heart Disease Events. J Gen Intern Med. 2016. April;31(4):387–93. doi: 10.1007/s11606-015-3556-3. Epub 2015 Dec 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malik S, Budoff MJ, Katz R, Blumenthal RS, Bertoni AG, Nasir K, et al. Impact of subclinical atherosclerosis on cardiovascular disease events in individuals with metabolic syndrome and diabetes: the multi-ethnic study of atherosclerosis. Diabetes Care. 2011. October;34(10):2285–90. doi: 10.2337/dc11-0816. Epub 2011 Aug 15. PubMed PMID: 21844289; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malik S, Zhao Y, Budoff M, Nasir K, Blumenthal RS, Bertoni AG, et al. Coronary Artery Calcium Score for Long-term Risk Classification in Individuals With Type 2 Diabetes and Metabolic Syndrome From the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol. 2017. December 1;2(12):1332–1340. doi: 10.1001/jamacardio.2017.4191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Budoff M, Backlund JC, Bluemke DA, Polak J, Bebu I, Schade D, et al. ; DCCT/EDIC Research Group. The Association of Coronary Artery Calcification With Subsequent Incidence of Cardiovascular Disease in Type 1 Diabetes: The DCCT/EDIC Trials. JACC Cardiovasc Imaging. 2019. March 8. pii: S1936–878X(19)30143–3. doi: 10.1016/j.jcmg.2019.01.014. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. ; REDUCE-IT Investigators. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019. January 3;380(1):11–22. doi: 10.1056/NEJMoa1812792. Epub 2018 Nov 10. [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association. Living Standards of Medical Care in Diabetes. Avaiilable online from http://care.diabetesjournals.org/living-standards [Accessed April 21, 2019]
- 13.Wong ND, Shapiro MD. Interpreting the findings from the recent PCSK9 monoclonal antibody cardiovascular outcomes trials. Front Cardiovasc Med 2019; doi 10.3389/fcvm.2019/00014 [DOI] [PMC free article] [PubMed] [Google Scholar]