Abstract
Background:
The use of the surgical robot has increased annually since its introduction, especially in general surgery. Despite the tremendous increase in utilization, there are currently no validated curricula to train residents in robotic surgery and the effects of robotic surgery on general surgery residency training is not well-defined. In this study, we aim to explore the perceptions of resident and attending surgeons toward robotic surgery education in general surgery residency training.
Methods:
We performed a qualitative thematic analysis of in-person, one-on-one, semi-structured interviews with general surgery residents and attending surgeons at a large academic health system. Convenient and purposeful sampling was performed in order to ensure diverse demographics, experiences, and opinions were represented. Data was analyzed continuously and interviews were conducted until thematic saturation was reached, which occurred after 20 residents and 7 attendings.
Results:
All interviewees agreed that dual consoles are necessary to maximize the teaching potential of the robotic platform and the importance of simulation and simulators in robotic surgery education is paramount. However, further work to ensure proper access to simulation resources for residents is necessary. While most recognize that bedside assist skills are essential, most think its educational value plateaus quickly. Lastly, residents believe that earlier exposure to robotic surgery is necessary and that almost every case has a portion that is level-appropriate for residents to perform on the robot.
Conclusions:
As robotic surgery transitions from novelty to ubiquity, the importance of effective general surgery robotic surgery training during residency is paramount. Through in-depth interviews, this study provides examples of effective educational tools and techniques, highlights the importance of simulation, and explores opinions regarding the role of the resident in robotic surgery education. We hope the insights gained from this study can be used to develop and/or refine robotic surgery curricula.
Keywords: Robotic surgery, general surgery, residency, training, education, qualitative analysis
INTRODUCTION
The number of robot-assisted surgical procedures has increased annually since its introduction (1). Robot-assisted surgery (RAS) has many technical and ergonomic advantages (2–5), but requires large capital investments by hospitals (1, 6, 7). RAS has previously been limited to large medical centers, but the tremendous increase in the number of units sold annually suggest that this is changing (1). However, RAS education, especially for general surgery residents, has lagged behind utilization of RAS.
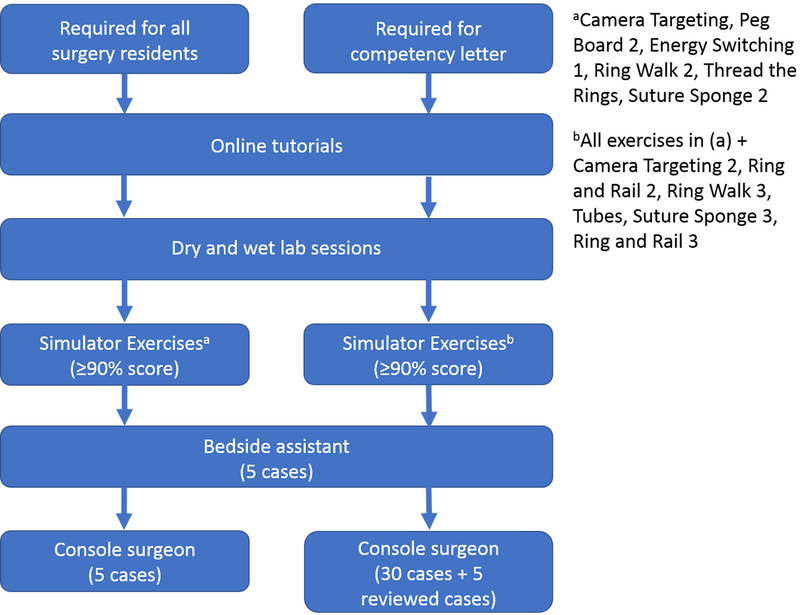
The effect of RAS on general surgery training is an important area of research. RAS presents unique challenges to general surgery training, including its high cost, slow adoption in certain subspecialties (e.g. vascular surgery), and low trainer familiarity. Currently, there are no validated RAS curricula and individual components of curricula are highly variable across the country (8). However, in general, the majority of curricula consist of: 1) online tutorials, 2) “dry” and “wet” simulation laboratory, 3) bedside assist, and 4) console surgeon (4, 9–13). At our institution, we have instituted a similar curriculum (Figure 1).
Figure 1.
Schematic Diagram of Our Current Curriculum. The pathway on the left is required for all residents. If a resident wants to obtain a competency letter, which can used for post-graduate credentialing, he or she will need to complete the extra requirements on the right.
The majority of previous studies on RAS education have been limited to evaluations of curricula based on trainee performance, self-reported competency, or number of cases performed (10, 13, 14). However, opinions of trainees and trainers regarding RAS education has been lacking, hindering the continued development and refinement of RAS curricula. The goal of this study is to use qualitative research methods to provide an in-depth analysis of perceptions among resident and attending surgeons on the role of RAS in general surgery training, to identify barriers to the successful implementation of a RAS curriculum, and to provide potential solutions to the challenges that residents face in this era of robotic surgery.
MATERIALS AND METHODS
Setting and Participants
This study was conducted in an urban, multi-hospital healthcare system consisting of two university hospitals and a Veterans Affairs (VA) hospital. In addition, residents also rotate at a community hospital. All four hospitals have RAS platforms, though resident exposure to RAS is limited at the community hospital due to credentialing policies. Residents also have limited access to a simulation laboratory that have multiple RAS platforms. The two university hospitals and the VA hospital have at least one robot at each site with the da Vinci Surgery Skills Simulator (dVSSS). Our institution has fellowships in minimally-invasive surgery, vascular surgery, breast oncology surgery, and trauma surgery. Attending surgeons interviewed for this study only operate at the two university hospitals and the VA hospital. During the most recent fiscal year, the minimally invasive and colorectal surgery divisions at our institution performed 246 robotic surgery cases, which accounted for 12.8% of all cases performed.
Interviewees included general surgery residents and attendings. There are approximately 50 residents in our 5-year general surgery residency program. After obtaining Institutional Review Board approval, we invited all residents to participate in the study. After an initial round of interviews, purposeful sampling was performed based on resident graduate-year in order to capture opinions regarding RAS education throughout the entire residency program. Residents were categorized into interns (1st-year residents), juniors (2nd- and 3rd-year residents), and seniors (4th- and 5th-year residents). Because of the limited number of attendings who perform robotic surgery, we utilized purposeful sampling to ensure a variety of specialties and opinions were represented. The number of participants were determined by data saturation, defined as when interviews no longer deepened or contradicted previous data (15). We achieved data saturation after 20 resident interviews and 7 attending interviews.
Data Collection
We performed semi-structured interviews with residents and attendings, focusing on their perceptions on robotic surgery education. The interview guide used for all interviews was constructed iteratively among investigators (BZ, JL, and LP). All one-on-one interviews were conducted by the same investigator (BZ) to ensure minimal group effect and maximize confidentiality (16). All resident interviews began with a collection of demographic information, including age, gender, resident level, and surgical subspecialty interest. In attending interviews, demographic information collected included gender, surgical specialty, years since last formal training, years since starting robotic surgery, and approximate number of robotic cases performed. All interviews were audio recorded and transcribed by BZ. All transcripts were anonymized prior to data analysis.
Data Analysis
We performed thematic analysis on all interviews. Each resident interview was coded independently by BZ and LP, with a third coding performed by HH, JL, or AL. This was done to prevent potential bias from group coding and to expand diversity of interpretations. All coders were instructed to code in a line-by-line fashion using descriptive open coding techniques. After each resident interview was coded individually, discussion of the codes commenced, and disagreements were resolved until consensus was reached for each interview. BZ coded all attending interviews because the limited number of attendings who perform RAS at our institution would make it difficult to maintain confidentiality, even with anonymized transcripts. Throughout the coding process, BZ regularly consulted with LP for ongoing feedback on codes and to develop thematic models. Preliminary coding frameworks and themes were developed iteratively. Credibility/validity was maintained by triangulation of data sources, including participant verification, discussion and debriefing by investigators, and themes extracted from the interviews were compared with existing theories on RAS education. The dependability of the study was established by achieving data saturation (15, 17).
RESULTS
We conducted interviews with 20 residents and 7 attendings, whose demographics are shown in Table 1. Data analysis yielded multiple themes, which were organized into four domains: 1) robotic surgery education tools, 2) simulation and simulators, 3) role of the bedside assistant, and 4) maximum resident exposure. Within each domain, residents and attendings discussed the advantages of RAS, the barriers in implementing a successful RAS curriculum, and potential solutions to overcome these challenges.
Table 1.
Demographics of Resident and Attending Interviewees
| Demographics | Number of Interviewees |
|---|---|
| General Surgery Attendings | |
| Gender | |
| Female | 4 |
| Male | 3 |
| Specialty | |
| Colorectal | 4 |
| Minimally Invasive | 2 |
| Surgical Oncology | 1 |
| Mean Years Since Last Training (Range) | 11.7 (2–24) |
| Mean Years Since Starting Robotic Surgery (Range) | 7.7 (1–19) |
| Median Approximate Number of Robotic Cases Performed (Range) | 100 (20–1000) |
| General Surgery Residents | |
| Resident Level | |
| Intern (1st Year Resident) | 4 |
| Junior Resident (2nd/3rd Year Residents) | 9 |
| Senior Resident (4th/5th Year Residents) | 7 |
| Gender | |
| Female | 13 |
| Male | 7 |
| Future Surgical Sub-Specialty | |
| Breast | 1 |
| Cardiothoracic | 1 |
| Colorectal | 3 |
| General | 1 |
| Minimally Invasive | 5 |
| Oncology | 1 |
| Pediatric | 2 |
| Transplant | 1 |
| Trauma | 5 |
Robotic Surgery Education Tools
“Having the dual console is very helpful. Being able to write on the screen to lead you is helpful. I think the ability to take over and say ‘let me show you what I’m talking about’ is nice…it’s nice when I get stuck, the attending says ‘let me show you how to get your third hand in there to retract this way’, you start to see it’s a lot easier.”
(Resident 4, senior resident)
There is general agreement among residents and attendings that screen annotation and dual consoles are necessary to maximize the teaching potential of the robotic platform (Table 2). Dual consoles allow the attending to use multiple teaching tools during surgery (e.g. console control swapping). Some residents also stated that it lowers the barrier for the residents to operate on the robot, because attendings can easily take over the controls, which is a “big difference with laparoscopy, where you have to physically switch positions.” However, some residents expressed that the lack of “console time” does not allow them to take advantage of these tools.
Table 2.
Comments regarding the use of robotic surgery as educational tools
| Representative Comments |
|---|
| “I would think that it’s probably easier [to teach] on the robot. You can take over, you can draw on the screen. One of the things that some of our attendings struggle with is translating what they want you to do into words…but if they say I want you to dissect down this line and they can draw on the screen or they can do one piece of it and hand it over to you, that’s a big difference with laparoscopy, where you have to physically switch positions.” (Resident 1, junior resident) |
| “I know the consoles have so much teaching potential built in. They can draw on the monitor, tell you where to go. It’s easy to teach on the console. And that’s all underutilized.” (Resident 3, intern) |
| “The easiest thing to do is the ability to draw on the screen. When you’re doing laparoscopy, you can’t really do that. You can try to do your best to verbalize what you want, but it’s difficult…there’s also the ability to not swap all the arms. They can keep the third arm and give you a crutch.” (Resident 16, senior resident) |
| “I do use the pointers regularly. Sometimes I’ll move the camera. I’m a stickler for visualization and if I feel like you’re not getting good visualization, then I’ll move the camera in position. And often I’ll just demonstrate something for them.” (Attending 3) |
Simulation and Simulators
“As a first step, doing the sims is better than going straight to the console, or even doing these before going to a pig. I think it’s a very good way to start getting comfortable with the robot.”
(Attending 12, junior resident)
Residents generally believed that the dVSSS was a helpful tool in familiarizing them with the console controls and making it easier to transition to the console in the operating room (Table 3). This sentiment was shared by most attendings as well. However, some residents did note that the feedback from the dVSSS lacked sufficient detail and did not provide concrete ways to improve their performance.
Table 3.
Comments regarding the role of simulation and simulators in robotic surgery education
| Representative Comments | |
|---|---|
| Skills Simulator | |
| “I think learning about the console and how it works and how to control, learning how to clutch and change instruments, I think that’s all fine. I think they actually put together a pretty decent simulator.” (Resident 1, junior resident) | |
| “The exercises, like the simulations, where you move a ring across a line…it helps get you comfortable with moving the camera and the position. I feel like the best utilization of it is that our attendings have been very helpful in letting us on the console if you’ve shown that you’ve done the exercises.” (Resident 4, senior resident) | |
| “When you’re on the simulation, you’re doing all the same movements as if you’re in the case. You can simulate open surgery with plastic, but on the robot, you’re getting used to using the instruments. It’s a much more realistic scenario when using the simulated robot. When you’re tying knots on a table, the sensation is a lot different. While on the robot, it’s pretty much the same.” (Resident 17, junior resident) | |
| “I think some of the feedback on the modules were not very good. You failed because your efficiency wasn’t high enough, but it didn’t tell me how to increase my efficiency.” (Resident 19, junior resident) | |
| “I do like the sim modules, I enjoy them, they were actually useful. I can relate them to real situations.’ (Attending 2) | |
| “It would start with the sim modules. I think they’re super helpful not just for robotic surgery, but really helpful for open surgery. I think they teach a lot of techniques, like economy of motion, tension on tissue, which we have a hard time teaching to residents.” (Attending 6) | |
| “It would have to involve, before they step into the OR, doing the online modules and getting yourself on the simulator for a few of them, even if it’s just one day.” (Attending 7) | |
| Simulation Lab | |
| “I actually did bedside in the OR first…and then doing them in the dry lab did help to know how to maneuver the instruments, so I think that’s necessary. It’s probably better to do them in the dry lab first.” (Resident 5, senior resident) | |
| “It’s kind of difficult in lab because there’s not a ton of attendings around to give you specific instructions. We were just playing around with how to use it. We weren’t getting specific ways on how to use it the right way…there was a time there was a fellow that was walking us through things, it was really good.” (Resident 10, junior resident) | |
| “I don’t think we have a very well-established robotic curriculum for the residents. I think it essentially is messing around in the pig lab when you get a chance to.” (Resident 11, junior resident) | |
| “I like the hands-on labs we have, the introductions to them. I like the animal labs, I think they’re helpful. I think it would be helpful if we could get the more junior residents to complete the online curriculum and the exercises earlier in their residency. Perhaps during the labs, we can have protected time to actually complete those training modules, instead of just going in to play around. Go in with the goal to actually completing the curriculum.” (Resident 15, senior resident) | |
| “We had two pigs and no faculty, the MIS fellow was the only one there. I had the device reps change the instruments for me. So, I just got on to try to do a roux-en-Y with no direction. So that was the most operating I got to do on the robot and that was really fun. I actually did a couple more after that with more people and more instruction. It was nice to have someone to actually instruct but free-play was kind of nice because there was no one to tell you what to do, and it’s really different.” (Resident 19, junior resident) | |
| “Starting in the skills lab is the best. Just to start getting comfortable with the controls, and the movements, and subtle things like adjusting the camera without moving the instruments. Those are all good skills to learn in the skills center, and that’s what I did as a fellow.” (Attending 1) | |
| “I think [residents] would spend time in the [simulation lab], so they can learn about the robot. I think that should be done by the Intuitive rep, to show them the data on the robot, how it works, this is the arms. Their initial training would be about exchanging the instruments, then training on the simulator.” (Attending 4) | |
| Access Problems | |
| “I don’t even know where I would go to do [the simulation modules].” (Resident 3, intern) | |
| “I know there’s a bunch of modules I need to do, but I just haven’t had time to get on the console and do them.” (Resident 5, senior resident) | |
| “Usually, there’s not a lot of time on the vast majority of rotations to step away and go and find a robot to use.” (Resident 8, junior resident) | |
| “It would be nice to have the console readily available…it seems like robotic education would be great, but I’m not sure if we the strongest administrative support for that.” (Resident 14, senior resident) | |
| “I definitely would [use the simulation modules more]. Especially on the night rotation, definitely. During the day, I don’t know of any rotations that I had enough time. That’s the other problem, I can’t even imagine doing the sim packs during the day. Getting to the [simulation lab] is impossible.” (Resident 17, junior resident) | |
| “My theory is that if we had better access to [simulation resources] and a better system in place, that we were better trained on it, then we would be able to get to do more in the OR.” (Resident 19, junior resident) |
“I think without the labs, there’s no way to transition to the OR as a resident…I can sit down and be able to know how to switch between my two instruments, being able to understand which pedals I’m pushing, to use electrocautery, I think it’s very valuable.”
(Resident 18, junior resident)
The simulation lab is also very important in robotic surgery education (Table 3). Most residents agreed that it provides the ideal introduction for residents to the robotic platform and should be done prior to using the robot in the operating room (OR). The simulation lab not only allows the resident to practice on the console, but also develops their bedside-assist skills. Most residents agreed that “wet” labs are more beneficial than “dry” labs. However, there was a divergence of opinion regarding “directed” versus “free-play” sessions. Lastly, one attending believed that there may be a role for industry in educating residents.
“I’ve only used those [sim] packs when we all went to practice at the [simulation lab]. It would be great to have a lot of time, like having a dedicated day to go practice on the machines. But to go on your own time, it’s very hard.”
(Resident 12, junior resident)
Poor access to the dVSSS and simulation lab were frequent complaints by residents (Table 3). Some did not know where they can practice on the dVSSS modules, while others lacked the time and schedule flexibility to do the exercises because it was something “to do on your own time.” Some residents also thought that the robotics labs were too infrequent, leading to skill atrophy as robotics exposure in general surgery training remains limited to certain rotations (e.g. minimally-invasive surgery, colorectal surgery).
Role of the Bedside Assistant
“I still learn things when I’m bedside assisting. It definitely helps you learn how to set up the robot. And how to use the different arm attachments, what the limitations are, and how to trouble-shoot some of the issues…there’s some educational value, but certainly it would be better as a senior resident to be spending more time on the console.” (Resident 15, senior resident) “I think everyone feels like it’s a drag to do the bedside assist, but I feel like it’s a very important thing to know how to properly connect the robot to the ports, burp the robot. There’s a lot of subtleties to it that would make the case go better if you knew to do that.”
(Attending 1)
Residents had very strong opinions regarding the role of the bedside assistant in RAS education (Table 4). While most recognized that bedside-assist skills are an essential part of RAS, the general consensus among residents is that the educational benefit of bedside-assisting plateaus very quickly. This opinion was mirrored by attendings as well. However, attendings tended to focus on how a “good” bedside assistant can “make the case go better”. Lastly, residents recognized that the role of bedside assistant also incorporates laparoscopic skills via the assist port.
Table 4.
Comments regarding the role of bedside assist in robotic surgery education
| Representative Comments |
|---|
| “I think [bedside assisting] helps you understand the tools available and how the robot functions, and the limitations. Because you can see the camera and arms swinging around and how it translates onto the screen.” (Resident 3, intern) |
| “Being proficient in setting up the robot and understanding what instruments or how they’re using the instruments, and exchanging instruments, I feel like all of that is helpful in understanding how to use the robot.” (Resident 10, junior resident) |
| “I do think we should do [bedside assist] here and there, so we have the ability to do it, but I don’t think there’s a lot to be learned from it. I think there’s a peak, but beyond that, there’s not a lot of utility in us doing it.” (Resident 11, junior resident) |
| “I think there’s some value [in bedside assisting]. Of course, ultimately, we want to be the surgeon at the console. But the surgeon at the console need to instruct what the bedside assist is doing so I think it’s an integral part of your education to be the bedside.” (Resident 12, junior resident) |
| “I think [bedside assisting] is more pertinent as a more junior resident. Probably switching out the instruments is less thrilling as you progress in residency, where you want to be operating more.” (Resident 13, intern) |
| “Bedside assisting, once you’ve learned how to dock the robot and exchange instruments, the learning curve is like 3 cases. And then you plateau. After that, it’s just laparoscopic skills in terms of getting instruments to help. I don’t know if you need to do it that many times.” (Resident 17, junior resident) |
| “In terms of instrument exchange, maybe 3 or 4 [times to get comfortable]. At least 2 for each robot type. In terms of understanding how to be that assist port, it takes more experience in laparoscopic surgery.” (Resident 18, junior resident) |
| “I think the bedside assistance is not really part of robotic training. I think you definitely need to do it once, but then there’s no learning curve after that.” (Attending 2) |
| “You have to know how to exchange instruments, dock the robot. And it’s got to go fast, robotic cases take a long time. If you don’t have a good smooth team to keep things moving.” (Attending 3) |
| “I don’t know if it’s necessary to do the bedside assisting before getting on the console. You can do it at the same time.” (Attending 6) |
Maximum Resident Exposure
“I think any robotic case is good for the resident to get on…I think there are parts of any case that the resident can do. So, if you want the resident to do the entire case…the [robotic] hernias and gallbladders would be good because they already know how to do that case laparoscopically. But in a rectal dissection, there’s still the mobilization off the wall that the resident can do.”
(Resident 5, senior resident)
“I think an inguinal hernia is a great way for someone to just get actual principles of surgery techniques down, and they can apply that to a colon resection and all these other things.”
(Attending 7)
Residents discussed methods to increase resident exposure in all aspects of RAS education (Table 5). Most residents advocated for earlier exposure to robotic surgery, either in the simulation lab or the OR. Multiple residents pointed out that most procedures have portions that may be level-appropriate for junior residents. Residents argued that allowing junior residents on the console for these portions of the procedures can help build the foundations to develop their console skills before they are senior residents. Many attendings advocated for the use of “simpler” cases for training purposes. The most common examples of “simple” cases included robotic cholecystectomy, appendectomy, inguinal hernia, and colectomy.
Table 5.
Comments regarding how to maximize resident exposure to robotic surgery
| Representative Comments |
|---|
| “I go in to these colorectal cases with the assumption that the attending is going to do the robotic portion. So just changing the culture, getting residents to assume that they will get to do some of the robotic portion would be good. Or even just being more inclusive in getting more junior residents exposure to it. Even if residents are doing it, it would be the chiefs or upper-levels who are doing any part of it.” (Resident 3, intern) |
| “I think if we had better integration [of the curriculum] into the residency program, if you can get console time earlier, you would be better off…it’s hard to get on the console until you’re a fourth year…but it would nice if we could get on the console earlier.” (Resident 6, senior resident) |
| “I think there’s not really any harm in exposing yourself to a lot of things as a junior resident…I feel like it would help as a senior resident doing robotic cases to have experienced them as a junior resident.” (Resident 13, intern) |
| “The robotic hernias, especially with attendings who let you do more, are a great way to get into those cases, so you get into some of the bigger robotic cases later. The robotic hernias are nice because the stakes are low, you’re only on the abdominal wall, there’s no bowel in the way so it’s easy.” (Resident 17, junior resident) |
| “I think [using simpler cases is] a good idea, I think that’s the best way to train. Understanding, that’s the reason you’re using it is for training.” (Attending 1) |
| “I think the reason to do robotic cholecystectomy is for training…residents would be great at it, attendings will be great at it. We’ll be good at the robot, and then we would be able to do big complex cases with the robot more easily.” (Attending 2) |
| “I would say it’s more [important to do] the steps. Isolate out the individual steps or parts of the procedure and get [residents] going on that.” (Attending 3) |
| “It was a great experience to learn using the robot on [cholecystectomies]. There’s very few opportunities to get too frustrated. All the things that make it difficult to learn robotic surgery. You’re staying in one place, you’re just learning which instruments to use, and how to switch instruments. I think the robotic chole as a learning tool is very helpful.” (Attending 6) |
DISCUSSION
This qualitative study of 20 residents and 7 attendings, encompassing over 9 hours of interviews, has provided valuable insight in the training of general surgery residents in the era of robotic surgery.
Robotic Surgery Education Tools
The importance of the dual console to robotic surgery education is apparent in interviews with both residents and attendings. Integration of dual consoles in a robotic training program can improve education without a significant increase in operative time or patient morbidity (18–20). In contrast to laparoscopy, in which switching the primary operator is quite laborious and complex, dual consoles allow for operator controls to be easily swapped between the trainer and trainee (21). In addition, the trainer can choose to keep control of the third arm, which was cited by residents as a “crutch” in which trainers can provide assistance to the trainee while still allowing the latter to operate with two instruments. Another commonly used tool is the screen annotation, which allows the trainer to visually direct the trainee intraoperatively. Lastly, the dual console gives the trainer the ability to perform an emergency stop, which is a rarely-used but comforting safety feature (22). Other features that were not mentioned by interviewees include the use of video review for surgeon education (23, 24) and the possibility of remote proctoring in the future (25, 26). However, to take advantage of these educational tools, residents must be on the console, which has been relatively rare (27, 28). This is also true at our institution and will be the basis for a future related study.
Simulation and Simulators
At our institution, trainees can practice on the consoles using the dVSSS, the effectiveness of which has been validated through multiple studies (29–35). The dVSSS contains multiple simulation exercises designed to familiarize the trainee with skills and techniques required to operate on the robotic console. Both residents and attendings agree that the dVSSS can effectively familiarize the trainee to the console, noting that skills learned on the dVSSS can be directly applied in the OR. However, an effective RAS curriculum requires thoughtful consideration on which specific simulator exercises should be required for trainees to complete (36, 37). The possibility of procedure-specific simulations in the future will likely increase the value of simulation-based training in robotic education.
The simulation lab has an important role in RAS education. It can be divided into “dry” labs, which often consists of low-fidelity inanimate objects (29, 38), and “wet” labs, which often consist of high-fidelity live animals or human cadavers (39). Our interviewees indicated a preference for wet labs over dry labs. However, wet labs are often more expensive than dry labs. An alternative may be heavier reliance on simulators, as they are essentially dry labs, and studies have shown that simulator-based curricula may be cost effective compared to wet labs (40).
The simulation lab can be used to familiarize residents to the role of the bedside assistant as well (41, 42). This is especially important for interns and junior residents, who are more likely to be bedside assistants in the OR. Attendings, and most residents, believed that trainees should begin their robotic training in the simulation lab. This ensures a baseline set of skills in all residents and can give attendings confidence in the residents’skills in the OR. However, efforts must be made to ensure that residents are able to access these simulation resources. Many residents opined that access to the simulators and the simulation lab is limited, presenting a barrier for many in completing the curriculum. A possible solution may be to set aside dedicated “simulator time” for residents, instead of expecting residents to complete the requirements “on their own time.” In addition, some residents were frustrated that the feedback received from the dVSSS was vague and not helpful. More guidance from trainers on specific techniques and “directed” instruction (as opposed to “free-play”) may be warranted.
Role of the Bedside Assistant
The relegation of the resident to the bedside assistant role is often cited as an example of the detrimental effect of RAS to resident education. While the educational benefit plateaus very quickly, the bedside assist does have some educational value (41, 43). This is a sentiment that is shared by most attendings and, perhaps begrudgingly, residents as well. It is important to note that bedside assist is not purely exchanging instrument, but may involve patient positioning, trocar positioning and insertion, robot docking, and providing surgical assistance via the laparoscopic assistant port (44). Attendings point out that the bedside assistant can both learn from watching the case and practicing their laparoscopic skills. In addition, the bedside assistant can play a pivotal role in emergency situations given their proximity to the patient (42). While most curricula in literature require residents to complete bedside assistant requirements prior to starting on the console, one attending believed that both can be done concurrently. Lastly, residents’ opinions regarding the role of the bedside assistant may be affected by the fact that they are often relegated to that role due to a shortage of qualified bedside assistants. This limits their time on the console, making bedside assisting seem like an obstacle in their surgical training.
Maximum Resident Exposure
Most residents advocated for earlier exposure to robotic surgery, either in the simulation lab or in the OR. Many residents believed that their simulation lab experience helped them in the OR, which has been suggested in literature (41). Recognizing that their role is likely limited to the bedside, interns were in favor of having bedside assistant simulation sessions prior to the OR. Junior and senior residents yearned for more console time but felt that robotic surgery is reserved for either attending surgeons or fellows only. However, almost every RAS case has a portion that is trainee-appropriate. The modular training approach, in which procedures are broken up into discrete parts, has been shown to be an effective training tool (45–47). Examples of “simple” parts of procedures, brought up by residents and attendings, included dissecting the white line of Toldt in a robotic colectomy or sewing the peritoneum in a robotic inguinal hernia repair. The use of “simple” cases (e.g. robotic cholecystectomy, robotic appendectomy) was more divisive among residents and attendings, though some studies have advocated for their use in training novice robotic surgeons (48–50).
At our institution, only minimally invasive surgery and colorectal surgery consistently perform RAS. Therefore, residents often rotate off a robotics-heavy rotation for months, resulting in skill atrophy. One possible solution, in addition to increasing the RAS case volume, is to supplement the robotic experience with regular and frequent simulation. As discussed above, this requires programs to ensure easy accessibility of these simulation resources.
Implications for Our Curriculum
The results of this study have led us to reevaluate our own robotic surgery curriculum. While residents have witnessed attendings use the majority of the educational features, some believed that the educational tools are still under-utilized. To maximize use of all the educational tools available, a tutorial will be developed for all attending surgeons who perform robotic procedures and may potentially be incorporated as part of the credentialing procedure for all robotic surgeons at our institution. Incorporating video review to surgical education will also be evaluated, though a specific protocol will need to be implemented to be maximize effectiveness (24, 51). Through our interviews, we found that many residents were not aware of the requirements of the curriculum. More work will be done to disseminate this information more effectively. In addition, we will place high-visibility placards on consoles that have the dVSSS “backpack”, making them easier to identify. However, extending access to the simulation lab remains challenging due to security concerns. Lastly, while some residents enjoyed the “free-play” simulation lab experience, most preferred more “directed” labs. Therefore, efforts to formalize the robotic simulation curriculum with faculty support has been made.
Limitations
Our study has limitations that are inherent to qualitative research. We employed a combination of convenient and purposeful sampling of a specific study population at an institution with a robust robotic surgery program, which may limit generalizability (52). The majority of the RAS exposure for residents took place within the training program of a large tertiary referral center. While residents do rotate at a community hospital that also utilizes robotic surgery, it is unclear how this experience affected residents’ opinions regarding RAS. All attendings in this study only perform RAS in an academic setting. Future studies on the role of RAS education in general surgery training will include surgeons in the community setting. Our sampling technique may also introduce bias, in that interviewees with strong opinions may be more likely to agree to participate. For example, 8 (25%) residents are interested in completing a minimally-invasive or colorectal fellowship, which may indicate an inherent interest in robotic surgery. However, the same number of residents are also interested in surgical sub-specialties with low robotic penetration (e.g. trauma, breast, and pediatric surgery). Variability in data interpretation is another limitation inherent to qualitative research. To combat this, our protocol employed coding by consensus for resident interviews, which has been recommended to improve validity (53). Unfortunately, to maintain interviewee anonymity, this could not be employed for attending interviews.
As RAS becomes more ubiquitous, it is increasingly important to effectively train future surgeons on this emerging technology. It is clear that RAS offers unique educational tools and efforts should be made to utilize these tools. The importance of simulation and simulators in RAS training cannot be understated. Lastly, while the value of the bedside assistant experience to resident education is clear, efforts should be made to maximize resident exposure to the console early and often. Based on this study, we have instituted changes to our RAS education curriculum. It is our hope that insights gained from this study can be used to help develop and/or refine robotic surgery education curricula for general surgery residencies nationwide. In addition, future longitudinal studies exploring how residents acquire robotic skills throughout their surgical residency, and what effects robotic education tools have on skill acquisition, would be highly beneficial.
ACKNOWLEDGEMENT
DISCLOSURES
Dr. Zhao was supported by the National Library of Medicine Training Grant [NIH Grant: T15LM011271]. The funding source had no role in the design and/or general conduct of this study; had no access to the data or role in data collection, management, analysis, or interpretation; had no role in the preparation, review, or approval of the manuscript; and had no role in the decision to submit the manuscript for publication.
Funding Source:
Dr. Beiqun Zhao is supported by the National Library of Medicine Training Grant [NIH Grant: T15LM011271]
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Dr. Lam has no conflicts of interest to disclose.
Dr. Hollandsworth has no conflicts of interest to disclose.
Dr. Lee has no conflicts of interest to disclose.
Dr. Lopez has no conflicts of interest to disclose.
Dr. Abbadessa has no conflicts of interest to disclose.
Dr. Eisenstein has no conflicts of interest to disclose.
Dr. Cosman has no conflicts of interest to disclose.
Dr. Ramamoorthy has no conflicts of interest to disclose.
Dr. Parry has no conflicts of interest to disclose.
REFERENCES
- 1.Surgical Intuitive. Intuitive Surgical, Inc. 2016 Annual Report. [Internet]. 2016. Available at: www.intuitivesurgical.com.
- 2.Lanfranco AR, Catellanos AE, Desai JP, Meyers WC. Robotic Surgery: A Current Perspective. Ann. Surg; 2004;239:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawson EH, Curet MJ, Sanchez BR, et al. Postural ergonomics during robotic and laparoscopic gastric bypass surgery : a pilot project. J. Robot. Surg; 2007;1:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szold A, Bergamaschi R, Broeders I, et al. European association of endoscopic surgeons (EAES) consensus statement on the use of robotics in general surgery. Surg. Endosc; 2015;29:253–288. [DOI] [PubMed] [Google Scholar]
- 5.Zelhart M, Kaiser AM. Robotic versus laparoscopic versus open colorectal surgery : towards defining criteria to the right choice. Surg. Endosc Springer US; 2018;32:24–38. [DOI] [PubMed] [Google Scholar]
- 6.Higgins RM, Frelich MJ, Bosler ME, Gould JC. Cost analysis of robotic versus laparoscopic general surgery procedures. [Internet]. Surg. Endosc [Internet]. Springer US; 2017;31:185–192. Available at: http://link.springer.com/10.1007/s00464-016-4954-2. [DOI] [PubMed] [Google Scholar]
- 7.Barbash GI, Glied SA. New technology and health care costs - the case of robot-assisted surgery. N. Engl. J. Med; 2010;363:701–704. [DOI] [PubMed] [Google Scholar]
- 8.Tom CM, Maciel JD, Korn A, et al. A survey of robotic surgery training curricula in general surgery residency programs: How close are we to a standardized curriculum?. Am. J. Surg Elsevier Ltd; 2019;217:256–260. [DOI] [PubMed] [Google Scholar]
- 9.George LC, O’Neill R, Merchant AM. Residency Training in Robotic General Surgery: A Survey of Program Directors. Minim. Invasive Surg. Hindawi; 2018;2018:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dulan G, Rege RV, Hogg DC, Gilberg-fisher KM. Developing a comprehensive, proficiency-based training program for robotic surgery. [Internet].Surgery [Internet]. Mosby, Inc.; 2012;152:477–488. Available at: 10.1016/j.surg.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 11.Chitwood WR, Nifong LW, Chapman WHH, et al. Robotic Surgical Training in an Academic Institution. Ann. Surg; 2001;234:475–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vetter MH, Green I, Martino M, et al. Time to consider integration of a formal robotic-assisted surgical training program into obstetrics/gynecology residency curricula. J. Robot. Surg; 2017. [DOI] [PubMed] [Google Scholar]
- 13.Martin R, Hsu J, Soliman M, et al. Incorporating a Detailed Case Log System to Standardize Robotic Colon and Rectal Surgery Resident Training and Performance Evaluation. [Internet].J. Surg. Educ [Internet]. Elsevier Inc.; 2019:1–8. Available at: 10.1016/j.jsurg.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Winder JS, Juza RM, Sasaki J, et al. Implementing a robotics curriculum at an academic general surgery training program : our initial experience. J. Robot. Surg Springer London; 2016;10:209–213. [DOI] [PubMed] [Google Scholar]
- 15.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. In: AldineTransaction, 1967. [Google Scholar]
- 16.Kaplowitz MD, Hoehn JP. Do focus groups and individual interviews reveal the same information for natural resource valuation ?. Ecol. Econ; 2001;36:237–247. [Google Scholar]
- 17.Shenton AK. Strategies for Ensuring Trustworthiness in Qualitative Research Projects Strategies for ensuring trustworthiness in qualitative research projects. Educ. Inf; 2004;22:63–75. [Google Scholar]
- 18.Smith AL, Krivak TC, Scott EM, et al. Dual-console robotic surgery compared to laparoscopic surgery with respect to surgical outcomes in a gynecologic oncology fellowship program. [Internet].Gynecol. Oncol [Internet]. Elsevier Inc.; 2012;126:432–436. Available at: 10.1016/j.ygyno.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 19.Smith AL, Scott EM, Krivak TC, et al. Dual-console robotic surgery: a new teaching paradigm. J. Robot. Surg; 2012;7:113–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mikhail E, Salemi JL, Hart S, Imudia AN. Comparing Single and Dual Console Systems in the Robotic Surgical Training of Graduating OB/GYN Residents in the United States. Minim. Invasive Surg Hindawi Publishing Corporation; 2016;2016:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernandes E, Elli E, Giulianotti P. The role of the dual console in robotic surgical training. [Internet].Surgery [Internet]. Mosby, Inc.; 2014;155:1–4. Available at: 10.1016/j.surg.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 22.Crawford DL, Dwyer AM. Evolution and literature review of robotic general surgery resident training 2002–2018. [Internet].Updates Surg. [Internet]. Springer International Publishing; 2018;70:363–368. Available at: 10.1007/s13304-018-0573-x. [DOI] [PubMed] [Google Scholar]
- 23.Carter SC, Chiang A, Shah G, et al. Video-based Peer Feedback Through Social Networking for Robotic Surgery Simulation: A Multicenter Randomized Controlled Trial. Ann. Surg; 2015;261:870–875. [DOI] [PubMed] [Google Scholar]
- 24.Ahmet A, Gamze K, Rustem M, Sezen KA. Is Video-Based Education an Effective Method in Surgical Education? A Systematic Review. J. Surg. Educ Elsevier; 2018;75:1150–1158. [DOI] [PubMed] [Google Scholar]
- 25.Agarwal R, Levinson AW, Allaf M, et al. The RoboConsultant: Telementoring and Remote Presence in the Operating Room During Minimally Invasive Urologic Surgeries Using a Novel Mobile Robotic Interface. Urology.; 2007;70:970–974. [DOI] [PubMed] [Google Scholar]
- 26.Ali MR, Loggins JP, Fuller WD, et al. 3-D Telestration: A Teaching Tool for Robotic Surgery. J. Laparoendosc. Adv. Surg. Tech; 2008;18:107–112. [DOI] [PubMed] [Google Scholar]
- 27.Farivar BS, Flannagan M, Leitman IM, et al. General Surgery Residents ‘Perception of Robot-Assisted Procedures During Surgical Training. [Internet].J. Surg. Educ [Internet]. Elsevier; 2014;72:235–242. Available at: 10.1016/j.jsurg.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 28.Mehaffey JH, Michaels AD, Mullen MG, et al. Adoption of robotics in a general surgery residency program: at what cost? [Internet].J. Surg. Res [Internet]. Elsevier Inc; 2017;213:269–273. Available at: 10.1016/j.jss.2017.02.052. [DOI] [PubMed] [Google Scholar]
- 29.Ramos P, Montez J, Tripp A, et al. Face, content, construct and concurrent validity of dry laboratory exercises for robotic training using a global assessment tool. BJU Int.; 2014;113:836–842. [DOI] [PubMed] [Google Scholar]
- 30.Hung AJ, Patil MB, Zehnder P, et al. Concurrent and Predictive Validation of a Novel Robotic Surgery Simulator: A Prospective, Randomized Study. J. Urol; 2011;187:630–637. [DOI] [PubMed] [Google Scholar]
- 31.Hung AJ, Jayaratna IS, Teruya K, et al. Comparative assessment of three standardized robotic surgery training methods. BJU Int.; 2013;112:864–871. [DOI] [PubMed] [Google Scholar]
- 32.Finnegan KT, Meraney AM, Staff I, Shichman SJ. Da vinci skills simulator construct validation study: Correlation of prior robotic experience with overall score and time score simulator performance. [Internet].Urology [Internet]. Elsevier Inc.; 2012;80:330–336. Available at: 10.1016/j.urology.2012.02.059. [DOI] [PubMed] [Google Scholar]
- 33.Lyons C, Goldfarb D, Jones SL, et al. Which skills really matter? proving face, content, and construct validity for a commercial robotic simulator. Surg. Endosc; 2013;27:2020–2030. [DOI] [PubMed] [Google Scholar]
- 34.Connolly M, Seligman J, Kastenmeier A, et al. Validation of a virtual reality-based robotic surgical skills curriculum. Surg. Endosc; 2013;28:1691–1694. [DOI] [PubMed] [Google Scholar]
- 35.Kelly DC, Margules AC, Kundavaram CR, et al. Face, content, and construct validation of the da Vinci Skills Simulator. [Internet].Urology [Internet]. Elsevier Inc.; 2012;79:1068–1072. Available at: 10.1016/j.urology.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 36.Stegemann AP, Ahmed K, Syed JR, et al. Fundamental Skills of Robotic Surgery: A Multi-institutional Randomized Controlled Trial for Validation of a Simulation-based Curriculum. [Internet].Urology [Internet]. Elsevier Inc.; 2013;81:767–774. Available at: 10.1016/j.urology.2012.12.033. [DOI] [PubMed] [Google Scholar]
- 37.Raza SJ, Froghi S, Chowriappa A, et al. Construct Validation of the Key Components of Fundamental Skills of Robotic Surgery (FSRS) Curriculum — A Multi-Institution Prospective Study. [Internet].J. Surg. Educ [Internet]. Elsevier; 2014;71:316–324. Available at: 10.1016/j.jsurg.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 38.Siddiqui NY, Galloway ML, Geller EJ, et al. Validity and reliability of the robotic objective structured assessment of technical skills. Obstet. Gynecol; 2014;123:1193–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bur AM, Gomez ED, Newman JG, et al. Evaluation of high-fidelity simulation as a training tool in transoral robotic surgery. Laryngoscope.; 2017;127:2790–2795. [DOI] [PubMed] [Google Scholar]
- 40.Rehman S, Raza SJ, Stegemann AP, et al. Simulation-based robot-assisted surgical training: A health economic evaluation. [Internet].Int. J. Surg [Internet]. Elsevier Ltd; 2013;11:841–846. Available at: 10.1016/j.ijsu.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 41.Thiel DD, Lannen A, Richie E, et al. Simulation-Based Training for Bedside Assistants Can Benefit Experienced Robotic Prostatectomy Teams. J. Endourol; 2012;27:230–237. [DOI] [PubMed] [Google Scholar]
- 42.Sgarbura O, Vasilescu C. The decisive role of the patient-side surgeon in robotic surgery. Surg. Endosc; 2010;24:3149–3155. [DOI] [PubMed] [Google Scholar]
- 43.Sur RL, Wagner AA, Albala DM, Su L-M. Critical Role of the Assistant in Laparoscopic and Robot-Assisted Radical Prostatectomy. J. Endourol; 2008;22:587–590. [DOI] [PubMed] [Google Scholar]
- 44.Kumar R, Hemal AK. The “scrubbed surgeon” in robotic surgery. World J. Urol; 2006;24:144–147. [DOI] [PubMed] [Google Scholar]
- 45.Hashimoto DA, Gomez ED, Danzer E, et al. Intraoperative Resident Education for Robotic Laparoscopic Gastric Banding Surgery : A Pilot Study on the Safety of Stepwise Education. [Internet].J. Am. Coll. Surg [Internet]. Elsevier Inc.; 2012;214:990–996. Available at: 10.1016/j.jamcollsurg.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 46.Lovegrove C, Novara G, Mottrie A, et al. Structured and Modular Training Pathway for Robot-assisted Radical Prostatectomy (RARP): Validation of the RARP Assessment Score and Learning Curve Assessment. [Internet].Eur. Urol [Internet]. European Association of Urology; 2016;69:526–535. Available at: 10.1016/j.eururo.2015.10.048. [DOI] [PubMed] [Google Scholar]
- 47.Lovegrove C, Ahmed K, Novara G, et al. Modular Training for Robot-Assisted Radical Prostatectomy: Where to Begin?. J. Surg. Educ Elsevier; 2017;74:486–494. [DOI] [PubMed] [Google Scholar]
- 48.Nelson EC, Gottlieb AH, Müller H, et al. Robotic cholecystectomy and resident education : the UC Davis experience. Int. J. Med. Robot. Comput. Assist. Surg; 2014;10:218–222. [DOI] [PubMed] [Google Scholar]
- 49.Huang Y, Chua TC, Ed M. Robotic cholecystectomy versus conventional laparoscopic cholecystectomy : A meta-analysis. [Internet].Surgery [Internet]. Elsevier Inc.; 2015;161:628–636. Available at: 10.1016/j.surg.2016.08.061. [DOI] [PubMed] [Google Scholar]
- 50.Jayaraman S, Davies W, Schlachta CM. Getting started with robotics in general surgery with cholecystectomy: The Canadian experience. Can. J. Surg; 2009;52:374–378. [PMC free article] [PubMed] [Google Scholar]
- 51.Green JL, Suresh V, Bittar P, et al. The Utilization of Video Technology in Surgical Education: A Systematic Review. J. Surg. Res Elsevier Inc; 2019;235:171–180. [DOI] [PubMed] [Google Scholar]
- 52.Marshall C, Rossman GB. Designing Qualitative Research. [Internet].Issues Appl. Linguist [Internet].; 1989;1:268–275. Available at: http://escholarship.org/content/qt3m25g8j8/qt3m25g8j8.pdf. [Google Scholar]
- 53.Richards KAR, Hemphill MA. A Practical Guide to Collaborative Qualitative Data Analysis. J. Teach. Phys. Educ; 2017:1–7. [Google Scholar]