Abstract
Mutations in retina-specific ATP-binding cassette transporter 4 (ABCA4) are responsible for over 95% of cases of Stargardt disease (STGD), as well as a minor proportion of retinitis pigmentosa (RP) and cone-rod dystrophy cases (CRD). Since the knowledge of the genetic causes of inherited retinal diseases (IRDs) in Poland is still scarce, the purpose of this study was to identify pathogenic ABCA4 variants in a subgroup of Polish IRD patients. We recruited 67 families with IRDs as a part of a larger study. The patients were screened with next generation sequencing using a molecular inversion probes (MIPs)-based technique targeting 108 genes involved in the pathogenesis of IRDs. All identified mutations were validated and their familial segregation was tested using Sanger sequencing. In the case of the most frequent complex allele, consisting of two variants in exon 12 and 21, familial segregation was tested using restriction fragment length polymorphism (RFLP). The most prevalent variant, a complex change c.[1622T>C;3113C>T], p.[Leu541Pro;Ala1038Val], was found in this cohort in 54% of all solved ABCA4-associated disorder cases, which is the highest frequency reported thus far. Additionally, we identified nine families displaying a pseudo-dominant mode of inheritance, indicating a high frequency of pathogenic variants within this population.
Keywords: ABCA4, Stargardt disease, cone-rod dystrophy, retinitis pigmentosa, inherited retinal disorders
1. Introduction
Inherited retinal diseases are genetic disorders affecting the retina. A specific subgroup of these disorders is caused by mutations in a gene encoding retina-specific ATP-binding cassette transporter 4 (ABCA4). This enzyme displays flippase activity towards retinoid substrates, enabling influx from the intradiscal membrane or extracellular membrane in rods [1]. ABCA4 is also expressed in the retinal pigment epithelium (RPE) [2]. Mutations disrupting this enzyme result in lipofuscin accumulation [3], which is damaging to photoreceptors and the RPE. Pathogenic alterations in the corresponding gene are responsible for various retinal dystrophies with macular involvement, mostly following an autosomal recessive inheritance pattern.
Stargardt disease 1 (STGD1, Mendelian Inheritance in Man (MIM) #248200), initially described in 1909 by a German ophthalmologist, is a macular dystrophy. In most cases, the inheritance follows an autosomal recessive pattern. In 1997, its inheritance was ascribed by Allikmets et al. to mutations in the ABCA4 gene [4]. Although mutations in ABCA4 cause over 95% of STGD, patients harbouring variants in this gene may also display different phenotypes: cone-rod dystrophy 3 (CRD3, MIM #604116), and retinitis pigmentosa 19 (RP19, MIM #601718) [5]. The model devised by Magueri et al. in 2000 divided ABCA4 mutations into three categories: ‘mild’, ‘moderate’ and ‘severe’, explaining the spectrum of different phenotypes by different variant combinations [6]. There have also been reports of ABCA4 dominant heterozygous mutations causing age-related macular degeneration (AMD, MIM #153800) [7]. However, it is hypothesised now that this entity may indeed be very late-onset Stargardt disease and that very mild and common hypomorphic alleles acting in trans contribute to the pathogenicity [8]. Up until recently, hypomorphic variants, such as p.(Asn1868Ile), were significantly underestimated in respect of the pathogenicity of ABCA4-associated disorders [8,9]. Additionally, deep-intronic changes were discovered earlier to have an impact on the disease when acting in trans with pathogenic alterations [10,11,12]. Over a thousand pathogenic variants have been described so far [13]. Causality and penetrance of some are still the subject of a debate [14,15].
Complex alleles in ABCA4 have been known since the discovery of its connection with retinal diseases. Variants c.[1622T>C;3113C>T], p.[Leu541Pro;Ala1038Val] found in cis were previously described to be present in 33% of Polish patients. Population frequency was estimated to be 0.42% [16]. However, the broader context of ABCA4 mutations in Poland, especially in the case of retinitis pigmentosa patients, has never been tested. Herewith, we performed molecular inversion probes (MIPs) analysis using panel of 108 genes on over two hundred inherited retinal disease (IRD) families to uncover the genetic population characteristics of IRD in Poland.
2. Materials and Methods
This study was approved by the local Bioethics Committee. We enrolled over two hundred families in a larger study designed to uncover the genetic causes of hereditary retinal degeneration in Poland. Informed consent adhering to the tenets of the Declaration of Helsinki was received from all participating affected individuals and unaffected family members. In addition, a Data Processing Agreement with a clause according to the General Data Protection Regulation EU Act was obtained.
A detailed medical history was obtained, and a full ophthalmologic examination was performed for all study participants. Clinical evaluation, when feasible, included best-corrected Snellen visual acuity (BCVA), colour vision, visual field test, dilated ophthalmoscopy, digital fundus photography, autofluorescence imaging, spectral-domain optical coherence tomography (SD-OCT), fluorescein angiography and electrophysiological assessment.
Genomic DNA was isolated from peripheral blood from patients and their relatives by automated method on a MagNA Pure 24 System, (Roche, Basel, Switzerland) or QIASymphony DSP DNA Mini/Midi kit on a QIASymphony robot or via manual QIAAmp Blood DNA kit (Qiagen, Hilden, Germany). DNA concentration was assessed with a Quant-iT™ dsDNA Assay Kit, broad range, using a NanoDrop 3300 spectrofluorometer (Thermofisher Scientific, Waltham, MA, USA). Subsequently, samples were screened using a molecular inversion probes (MIPs) technique targeting 108 genes involved in the pathogenesis of inherited retinal disorders (IRDs), as described elsewhere [17]. Briefly, over 6000 MIPs covering the regions of interest were designed using an in-house software (Department of Human Genetics, Radboud University Nijmegen Medical Center) and manually verified. The probes were phosphorylated and pooled together. Careful rebalancing experiments were performed to ensure uniform coverage. We prepared the libraries using Ampligase DNA ligase (Thermofisher Scientific, Waltham, MA, USA) and HemoKlenTaq polymerase (New England Biolabs, Ipswich, MA, USA) for gap filling. Polymerase chain reaction (PCR) was performed with high fidelity iProof Master Mix (Biorad, Hercules, CA, USA). We tested the hybridisation efficiency using real-time PCR to empirically determine the optimal number of amplification cycles in each separate pool. Subsequently, PCR products were verified on a 2% agarose gel, pooled and purified using Agencourt AMPure magnetic beads (Beckman-Coulter, Brea, CA, USA). The purity and size of the product was checked on a Fragment Analyzer with High Sensitivity NGS (next-generation sequencing) Fragment Analysis Kit (DNF-474; Agilent Technologies, Santa Clara, CA, USA). Libraries were quantified using a NanoDrop 3300 spectrofluorometer with the Quant-iT™ dsDNA Assay Kit, high sensitivity (Thermofisher Scientific, Waltham, MA, USA). The pools were paired-end sequenced (2× 100 bp) with a Rapid Run Mode on a HiSeq 1500 (Illumina, San Diego, CA, USA) according to the manufacturer’s protocol. For each run, custom sequencing primers were added at a final concentration of 0.5 µM. Raw sequence readouts were analyzed with bcl2fastq software (Illumina) to generate fastq format reads. After the quality control step (including adapter trimming and low quality reads removal), reads were aligned to the hg38 reference genome with Burrows-Wheeler Aligner (BWA; [18]), and processed further by Picard [19] and Genome Analysis Toolkit [20].
We performed secondary analysis of fastq files with the SeqNext module of SeqPilot software. The frequency filter was initially set to minor allele frequency (MAF) <0.5% in public databases, following manual identification of causative variants appearing with higher frequency in global populations. All identified alterations were validated using Sanger sequencing. We recruited family members to perform segregation analysis. Genetic material was self-collected with buccal swabs by family members and DNA was isolated with the QIASymphony Investigator Kit (Qiagen, Hilden, Germany). We have confirmed familial segregation using Sanger sequencing in all amplicons except for the most common variants inherited together as a complex allele: c.1622T > C, p.(Leu541Pro) and c.3113C > T, p.(Ala1038Val), where we used restriction enzymes TspRI and BseYI, respectively (New England Biolabs, Ipswich, MA, USA). We subjected novel splice variants to scrutiny using four in silico prediction programs which are incorporated into AlaMut Visual Splicing Effects module SpliceSiteFinder-like (SSFL), MaxEntScan (MES), NNSPLICE, GeneSplicer (Biosoftware, 2014; Interactive Biosoftware, Rouen, France).
3. Results
3.1. Clinical Testing Results
Out of 67 individuals analysed in this study, 50 probands were diagnosed with STGD, 12 were suffering from RP, three were suffering from CD/CRD and two probands had an unsure diagnosis. Age of onset presented a wide spectrum from 4 to 44 years old (median = 9), and age at diagnosis was 7–62 years old (median = 11) (Table 1). At the time of recruitment, patients ranged in age from 8 to 63 years old (median = 31). There was no difference in median age of onset between RP and STGD1 patients.
Table 1.
Genetic and demographic data of patients suffering from retina-specific ATP-binding cassette transporter 4 (ABCA4)-related disorders. CD = cone dystrophy; CRD = cone-rod dystrophy; RP = retinitis pigmentosa; STGD1 = Stargardt’s dsease type 1
| Sample ID | Family ID | Year of birth | Sex | Diagno-sis | Age of onset | Age at dia-gnosis | Age at exami-nation | Allele 1 | Allele 2 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Nucleotide level | Protein level | Nucleotide level | Protein level | ||||||||
| 225 | F17-003 | 1983 | F | STGD1 | 7.0 | 7.0 | 34 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.634C>T | p.(Arg212Cys) |
| 229 | F17-007 | 1988 | F | STGD1 | 7.0 | 9.0 | 29 | c.4537dup | p.(Gln1513Profs*42) | c.5461-10T>C | p.[Thr1821Valfs*13,Thr1821Aspfs*6] |
| 230 | F17-008 | 1954 | M | STGD1 | 44.0 | 62.0 | 63 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5603A>T | p.(Asn1868Ile) |
| 231 | F17-009 | 1972 | F | STGD1 | 14.0 | 16.0 | 45 | c.4234C>T | p.(Gln1412*) | c.5882G>A | p.(Gly1961Glu) |
| 235 | F17-010 | 1989 | F | STGD1 | 7.0 | 11.0 | 28 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5714+5G>A | p.[=,Glu1863Leufs*33] |
| 239 | F17-014 | 1984 | M | STGD1 | 30.0 | 31.0 | 33 | c.194G>A | p.(Gly65Glu) | c.2588G>C | p.[Gly863Ala,Gly863del] |
| 240 | F17-015 | 1980 | M | STGD1 | 8.0 | 10.0 | 37 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] |
| 247 | F17-022 | 1990 | F | STGD1 | 13.0 | 23.0 | 27 | c.194G>A | p.(Gly65Glu) | c.5882G>A | p.(Gly1961Glu) |
| 252 | F17-025 | 2009 | M | STGD1 | 7.0 | 8.0 | 8 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.1622T>C | p.(Leu541Pro) |
| 253 | F17-026 | 2006 | M | STGD1 | 8.5 | 9.0 | 11 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.2041C>T | p.(Arg681*) |
| 255 | F17-028 | 2001 | F | STGD1 | 7.0 | 7.5 | 16 | c.5684_5685delTG | p.(Leu1895Argfs*16) | c.5882G>A | p.(Gly1961Glu) |
| 264 | F17-036 | 1999 | M | STGD1 | 14.0 | 16.0 | 18 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.4462T>C | p.(Cys1488Arg) |
| 266 | F17-038 | 2006 | M | STGD1 | 9.0 | 9.5 | 11 | c.2894A>G | p.(Asn965Ser) | c.6319_6325del | p.(Arg2107Cysfs*6) |
| 277 | F17-045 | 2004 | M | STGD1 | 11.0 | 12.0 | 13 | c.1211C>A | p.(Ser404*) | c.5882G>A | p.(Gly1961Glu) |
| 284 | F17-052 | 2001 | M | STGD1 | 10.0 | 16.0 | 16 | c.454C>T | p.(Arg152*) | c.2588G>C | p.[Gly863Ala,Gly863del] |
| 286 | F17-054 | 1981 | F | RP | 8.0 | 11.0 | 36 | c.2626C>T | p.(Gln876*) | c.5196+1G>A | p.(?) |
| 289 | F17-057 | 2006 | M | STGD1 | 8.0 | 9.0 | 11 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.3056C>T | p.(Thr1019Met) |
| 298 | F17-062 | 2005 | M | STGD1 | 8.0 | 9.0 | 12 | c.710T>C | p.(Leu237Pro) | c.4234C>T | p.(Gln1412*) |
| 302 | F17-065 | 2004 | F | STGD1 | 9.0 | 11.0 | 13 | c.[2588G>C;5603A>T] | p.[Gly863Ala,Gly863del;Asn1868Ile] | c.(2653+1_2654-1)_(*1_?)del | p.(Gly885Valfs*71) |
| 305 | F17-068 | 2005 | M | STGD1 | 11.0 | 11.0 | 12 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.4139C>T | p.(Pro1380Leu) |
| 309 | F17-072 | 1987 | F | STGD1 | 8.0 | 8.5 | 30 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.4234C>T | p.(Gln1412*) |
| 314 | F17-077 | 2003 | F | STGD1 | 12.0 | 14.0 | 14 | c.61C>T | p.(Gln21*) | c.3413T>A | p.(Leu1138His) |
| 316 | F17-079 | 2007 | F | CD | 8.0 | 9.5 | 10 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] |
| 318 | F17-081 | 2009 | F | STGD1 | 7.5 | 8.0 | 8 | c.3364G>T | p.(Glu1122*) | c.4234C>T | p.(Gln1412*) |
| 321 | F17-083 | 2004 | M | STGD1 | 11.5 | 12.0 | 13 | c.4234C>T | p.(Gln1412*) | c.5882G>A | p.(Gly1961Glu) |
| 325 | F17-086 | 2004 | F | STGD1 | 11.0 | 12.0 | 13 | c.454C>T | p.(Arg152*) | c.66G>A | p.[=,?] |
| 327 | F17-088 | 2008 | F | STGD1 | 7.5 | 8.0 | 9 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.4234C>T | p.(Gln1412*) |
| 333 | F17-095 | 1994 | M | RP | 10.0 | 11.0 | 23 | c.5196+1G>A | p.(?) | c.5196+1G>A | p.(?) |
| 338 | F17-100 | 1976 | F | STGD1 | 10.0 | 12 | 41 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] |
| 344 | F17-106 | 1990 | F | STGD1 | 7.0 | 19.0 | 27 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5882G>A | p.(Gly1961Glu) |
| 345 | F17-107 | 1989 | F | STGD1 | 18.0 | 20.0 | 28 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5882G>A | p.(Gly1961Glu) |
| 347 | F17-109 | 1990 | F | STGD1 | 16.0 | 20.0 | 27 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5714+5G>A | p.[=,Glu1863Leufs*33] |
| 348 | F17-110 | 1975 | F | STGD1 | 19.0 | 20.0 | 42 | c.4234C>T | p.(Gln1412*) | c.2588G>C | p.[Gly863Ala,Gly863del] |
| 349 | F17-111 | 1992 | M | STGD1 | 22.0 | 24.0 | 25 | c.4234C>T | p.(Gln1412*) | c.1654G>A | p.(Val552Ile) |
| 351 | F17-113 | 1994 | M | STGD1 | 9.0 | 9.0 | 23 | c.2588G>C | p.(Gly863Ala) | c.5461-10T>C | p.[Thr1821Valfs*13,Thr1821Aspfs*6] |
| 356 | F17-118 | 1990 | F | STGD1 | 21.0 | 27.0 | 27 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5882G>A | p.(Gly1961Glu) |
| 363 | F18-002 | 1968 | F | RP | 7.0 | 11.0 | 50 | c.4234C>T | p.(Gln1412*) | c.1622T>C | p.(Leu541Pro) |
| 364 | F18-003 | 1987 | F | STGD1 | 4.0 | 15.0 | 31 | c.3413T>A | p.(Leu1138His) | c.4919G>A | p.(Arg1640Gln) |
| 370 | F18-009 | 1975 | M | RP | 7.0 | 9.0 | 43 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.1622T>C | p.(Leu541Pro) |
| 373 | F18-012 | 1982 | F | STGD1 | 28.0 | 33.0 | 36 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5882G>A | p.(Gly1961Glu) |
| 377 | F18-016 | 1991 | M | STGD1 | 8.0 | 21.0 | 27 | c.3259G>A | p.(Glu1087Lys) | c.5714+5G>A | p.[=,Glu1863Leufs*33] |
| 379 | F18-018 | 1996 | F | STGD1 | ? | 21 | 22 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] |
| 385 | F18-024 | 1995 | F | CRD | 12.0 | 19.0 | 23 | c.3261G>A | p.(Glu1087Asp) | ||
| 389 | F18-028 | 1962 | F | RP | 7.0 | 7 | 56 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.4234C>T | p.(Gln1412*) |
| 391 | F18-030 | 1979 | M | STGD1 | 24.0 | 26.0 | 39 | c.4234C>T | p.(Gln1412*) | c.5714+5G>A | p.[=,Glu1863Leufs*33] |
| 397 | F18-036 | 1963 | F | RP | 8.5 | 9.5 | 55 | c.4793C>A | p.(Ala1598Asp) | c.5196+1G>A | p.(?) |
| 403 | F18-040 | 2000 | F | STGD1 | 10.0 | 13.0 | 18 | c.3413T>A | p.(Leu1138His) | c.4070C>T | p.(Ala1357Val) |
| 407 | F18-044 | 1957 | F | RP | 4.0 | 14 | 61 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] |
| 410 | F18-047 | 1972 | F | RP | 7.0 | 8.0 | 46 | c.1937+1G>A | p.(?) | c.4918C>T | p.(Arg1640Trp) |
| 413 | F18-050 | 1977 | M | STGD1 | 8.0 | 8.5 | 41 | c.4234C>T | p.(Gln1412*) | c.4234C>T | p.(Gln1412*) |
| 417 | F18-054 | 1983 | M | STGD1/CRD | 8.0 | 8.5 | 35 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5461-10T>C | p.[Thr1821Valfs*13,Thr1821Aspfs*6] |
| 418 | F18-055 | 1955 | F | STGD1/CRD | 27.0 | 60.0 | 63 | c.5887C>T | p.(Arg1963Cys) | ||
| 419 | F18-056 | 1981 | F | RP | 5.0 | 18.0 | 37 | c.5882G>A | p.(Gly1961Glu) | c.1411G>A | p.(Glu471Lys) |
| 420 | F18-057 | 1959 | M | RP | 26.0 | 26 | 59 | c.587C>T | p.(Pro196Leu) | ||
| 424 | F18-061 | 1980 | M | RP | 10.0 | 23.0 | 38 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5899-3T>G | p.(?) |
| 427 | F18-064 | 2000 | F | STGD1 | 5.0 | 10.0 | 18 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.1022A>G | p.(Glu341Gly) |
| 428 | F18-065 | 1972 | F | RP | 8.0 | 10.0 | 46 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5461-10T>C | p.[Thr1821Valfs*13,Thr1821Aspfs*6] |
| 478 | F18-069 | 2005 | F | STGD1 | 9.0 | 12.0 | 13 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.2588G>C | p.[Gly863Ala,Gly863del] |
| 479 | F18-070 | 2000 | F | STGD1 | 7.5 | 8.0 | 18 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.634C>T | p.(Arg212Cys) |
| 480 | F18-071 | 2009 | F | CRD | 7.0 | 8.0 | 9 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] |
| 485 | F18-075 | 2007 | M | STGD1 | 9.0 | 9.5 | 11 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.634C>T | p.(Arg212Cys) |
| 486 | F18-076 | 2007 | M | STGD1 | 9.0 | 10.0 | 11 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.5714+5G>A | p.[=,Glu1863Leufs*33] |
| 490 | F18-080 | 2008 | M | STGD1 | 9.0 | 9.0 | 10 | c.[1622T>C;3113C>T] | p.[Leu541Pro;Ala1038Val] | c.4352+1G>A | p.(?) |
The most common clinical presentation of STGD1 patients was RPE atrophy and pigment clumping in the macula. Characteristic fundus flecks were noted in 28% of patients. The dark choroid sign on fluorescein angiography was present in 46% of cases. Fundus autofluorescence showed central areas of hyperautofluorescence in all tested subjects. Multifocal electroretinography (mfERG) proved to be the most useful electrophysiological test with reduced response from the central 10 degrees confirming the diagnosis. mfERG pattern varied greatly in STGD1 subjects, ranging from a normal response to rod and/or cone abnormalities, which correlated poorly with clinical presentation. The best corrected distance visual acuity (BCVA) was 0.1 in the majority of patients and they mostly retained reading ability. All 12 of the patients diagnosed with RP experienced visual deterioration and nyctalopia before the age of 10. They mostly presented with the classic triad of arteriolar attenuation, optic nerve pallor and bone spicules in the peripheral retina. The disease led to severe visual impairment and legal blindness in the majority of cases—BCVA was limited to light perception in one third of cases and hand movement in another one third of cases. Ten out of 12 patients lost reading ability.
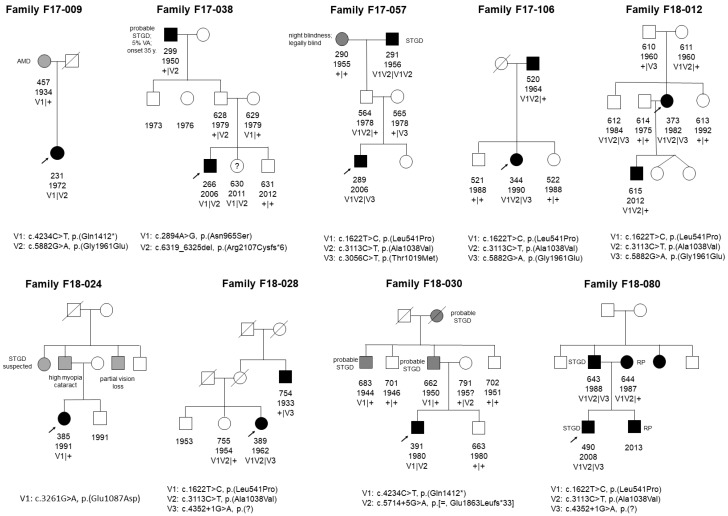
Additionally, we detected nine families displaying a pseudo-dominant mode of inheritance in this group. Their corresponding pedigrees with family members available for co-segregation are depicted in Figure 1. Segregation analysis was not possible in three cases, since we lost contact with the families.
Figure 1.
Pedigrees of nine families with pseudo-dominant inheritance pattern. Various phenotypes are present within families. Only variants detected in probands were sequenced in family members. Patient 385 remains unsolved. AMD = age-related macular dystrophy; STGD = Stargardt disease; RP = retinitis pigmentosa; VA = visual acuity; V = variant.
3.2. Genetic Testing Results
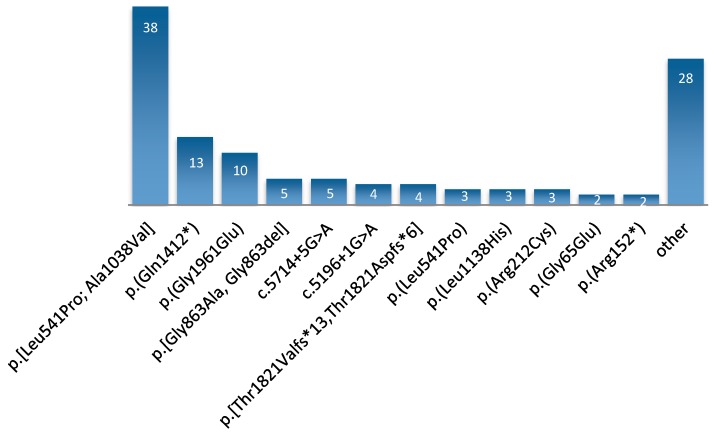
After secondary in silico analysis, we found ABCA4 variants in 63 probands. Four additional STGD patients received no genetic diagnosis. Two of them underwent whole exome sequencing (WES) with no results. The complex allele c.[1622T>C;3113C>T], p.[Leu541Pro;Ala1038Val] was present in 32 individuals suffering from ABCA4-associated disorders (six of them homozygous), which makes it the most prevalent allele in the Polish population (50.7% of all cases in subgroup with ABCA4 variants; 38/123 pathogenic alleles; MAF = 0.31) (Figure 2, Table 1, Table S2). Additionally, we found a second variant from the complex allele independently in three cases. All cases taken together represented the whole spectrum of ABCA4-related diagnoses. All identified mutations are shown in Table S2.
Figure 2.
Number of alleles for the most common variants. The most prevalent, complex allele was found on 38 chromosomes. Its component, c.1622T > C, p.(Leu541Pro), was identified independently on three additional alleles. Unique causative alterations present on one chromosome in a single patient are combined within “other”.
Three mutations found in this cohort were thus far unreported. We identified c.5899-3T>G, p.?; c.66G>A, p.[=,?] and a copy number variant (CNV) encompassing exons 18–50, whose breakpoint could not be determined due to ending downstream of the ABCA4 gene (c.(2653+1_2654-1)_(*1_?)del, p.(Gly885Valfs*71); [21]). All detected mutations are shown in Table 1 and Table S1. The corresponding MAFs and classifications are shown in Table S2.
4. Discussion
We have hereby proven our hypothesis that the spectrum of ABCA4 alterations in Poland differs from Western populations. Three novel changes were identified—one was a CNV and two represented splice site variants (the latter two lately published in the Human Genome Mutation Database). Interestingly, one of them was a silent type, affecting the last nucleotide in exon 1 (p.Lys22=). All splice prediction algorithms showed almost completely abolished donor splice sites (SSFL: −100%, MES: −79%, NNSPLICE: −100%, GeneSplicer: −100%). In case of c.5899-3T > G the acceptor splice site estimates were also severely diminished in all except one predictor (SSFL: −6%, MES: −100%, NNSPLICE: −100%, GeneSplicer: −100%). Both patients had a ‘severe’ variant on the other allele inherited from their fathers (p.(Arg152*) and p.[Leu541Pro;Ala1038Val]). Individual 424, suffering from RP, has inherited c.5899-3T > G from the mother and 325, who has STGD1, received the (p.Lys22=) allele. Therefore, according to previous classifications, we may assume that the first one represents a null mutation and the latter results in a moderate effect. However, midigene splice site assays, such as the ones performed by Sangermano et al. [22], are necessary to determine their actual effects.
CNVs in the ABCA4 gene are not common events [11,23,24]. Patient 302, who harboured a large deletion on one allele, had classic Stargardt disease with juvenile age of onset (nine years old). The presence of a CNV was strongly suggested by the fact that a single heterozygous mutation, c.2588G > C, p.[Gly863Ala, Gly863del], was accompanied by the seemingly homozygous c.5603A > T, p.(Asn1868Ile) and upon segregation, the father appeared to harbour both changes heterozygously, and the mother had none. This suggested a local loss of heterozygosity. A CNV analysis using the SeqNext CNV module revealed a deletion of exons 18–50, which was subsequently confirmed in a smMIPs(single-molecule molecular inversion probes)-based whole ABCA4 gene sequencing study [21]). Most probably the mother is a carrier of this variant. Unfortunately, since the deletion stretches further downstream of the ABCA4 gene, its breakpoints could not be determined and thus segregation testing of this variant was not performed.
Only eight patients in our group were homozygous: six for the aforementioned complex allele, one for p.(Gln1412*)—the second most common allele in this cohort, present on 13 chromosomes—and one for c.5196 + 1G > A. This is in line with the general outbred profile of the Polish population. Notably, individual 333 carrying c.5196 + 1G > A on both alleles was born of a consanguineous union of second degree cousins, which is a practice uncommon within this society. Additionally, one of patient’s 289 affected grandparents was homozygous for the p.[Leu541Pro;Ala1038Val] complex variant (consanguinity not known). In family F18-002, where two pairs of siblings intermarried, second degree cousins displayed the same combination of p.(Gln1412*) and p.(Leu541Pro) variants, which resulted in the RP phenotype.
RP patients almost invariably displayed only alleles deemed “severe”, whereas the STGD1 phenotype could be ascribed to a broader spectrum of alterations, suggesting genetic modifiers. The only RP patients who were not solved with severe mutations (419 and 420) harboured a mild change and variants of unknown significance (VUS). Individual 419 had p.(Gly1961Glu) and p.(Glu471Lys) VUS, which segregated within the family. The p.(Glu471Lys) variant has been described in the literature before, both as a VUS and a likely pathogenic variant. Initially, Allikmets et al. reported it as an AMD-associated variant [7], which may indicate that it exerts a very mild effect on protein activity. Lately, it was reported in a phenotype called bull’s-eye maculopathy [25]; however, in both cases, no deep intronic variants or CNV screening was performed, indicating that it may be a ‘passenger’ mutation linked with an unknown pathogenic variant. It is a matter of debate whether patient 419 could be considered as solved, despite having two segregating ABCA4 variants and no other variant within the 108 genes studied. Further studies involving broader analysis including deep intronic variants in cis, possibly to identify a third, severe mutation, are required. Similarly, individual 420 had only single-allelic VUS, p.(Pro196Leu), which is most likely not a causative mutation. In this RP patient, the genetic cause most likely lies within another gene. Four additional STGD patients had no candidate ABCA4 variants. Two of them underwent WES, but the results were negative. These individuals may carry deep intronic variants or CNVs in ABCA4, which should be elucidated in the next step.
Classical Stargardt disease was also displayed by patient 385, who was a carrier of the heterozygous c.3261G > A, p.(Glu1087Asp) variant. Patient 418 was another single allele carrier who first noticed disease symptoms at the age of 27. A heterozygous VUS, c.5887C > T p.(Arg1963Cys), was identified with no counterpart on the other chromosome. Despite her rather advanced age (63), this individual showed mild symptoms and still retained some vision in her left eye. Both of these patients have not yet been tested for deep intronic variants.
We revealed phenotype discordance in four families. Discordant siblings, carrying the same set of mutations but showing no phenotype, were invariably male. In one case, an eight-year-old individual with c.[1622T>C;3113C>T], p.[Leu541Pro;Ala1038Val] and c.2588G > C, p.[Gly863Ala, Gly863del] may not have yet developed the symptoms (his sister started noticing visual problems at the age of nine). Patient 235 had two brothers with the same pathogenic variants: c.[1622T>C;3113C>T], p.[Leu541Pro; p.Ala1038Val] and c.5714+5G > A, p.[=, Glu1863Leufs *33]. Her age of onset was seven, and the affected younger brother was 13 years old. The other brother was already 26 years old and displayed no phenotype. The same situation was seen in the pseudo-dominant family of patient 373; however, here the difference between the ages of onset was smaller. The proband, carrying c.[1622T>C;3113C>T], p.[Leu541Pro;Ala1038Val] and c.5882G > A, p.(Gly1961Glu) mutations first had symptoms at 28. Her brother was still asymptomatic at 35. The last family harboured the c.4234C > T, p.(Gln1412*) c.1654G > A, p.(Val552Ile) combination. In this case, no intronic variants or CNVs were found in a parallel study [21]). Age of onset of the proband was 22, whereas his brother showed no symptoms at 34. These inconsistencies may indicate the presence of a genetic modifier within these families. Further studies are required to uncover possible variants influencing the penetrance and expressivity of the disease.
It is striking how extremely common the p.[Leu541Pro;Ala1038Val] allele is in the populations of Mid-Eastern Europe. It was first found in 1997 by Allikmets et al. upon the identification of ABCA4 variants as a cause of Stargardt disease. Subsequently, this combination was detected in many other families. The first suggestion of a German origin founder effect of the p.[Leu541Pro;Ala1038Val] allele was made by Rivera in 2000 [26], when it was found among STGD1 and AMD patients with a frequency of 12.7%. However, more recent publications indicate that the high frequency in Germany was rather due to migrations from Eastern Europe, where this allele is more common. The Hungarian population was found to display a frequency of 28% among STGD patients [27]. Finally, Scieżyńska et al. tested 93 unrelated Polish STGD and CRD patients and detected this allele in 33 individuals [16]. The population frequency was estimated as 0.42%. In the current in-house database, which now contains data from 5007 samples, this allele appears 33 times (0.63%), and p.(Ala1038Val) alone appears twice. This means that crossing-over does indeed occur between these two linked loci, albeit it is not a frequent event.
In a recent publication, the three-dimensional (3D) structure of ABCA4 was devised and structural in silico tools were used to link the functional effects of mutations to the related phenotypes [28]. The pathogenic effect of p.(Leu541Pro), residing in extracellular domain 1, was reported to result from misfolding. Garces et al. described this variant earlier as having a negative impact on the ATP-binding capacity and abolishing of retinal-stimulated ATP hydrolysis [29]. The second variant of the complex allele, p.(Ala1038Val), located in nucleotide binding domain 1, seemed to be a milder alteration. Nevertheless, it still contributed to the severe outcome [13,29,30].
Out of the 67 patients in this group, nine came from families showing a clear pseudo-dominant pattern, either with full or incomplete penetrance (Figure 1). Pseudo-dominance in this gene has been reported many times [6,31,32]. This plays a crucial role, especially in cases where clinical phenotype cannot be easily determined. For instance, cone-rod dystrophy is a disease that can be inherited in both autosomal recessive and dominant mode. Wrong conclusions about risks for family members can be drawn if misinterpreted in the absence of genetic diagnosis.
Four patients with STGD could not be genetically solved. Despite performing additional WES in two cases, no causative mutations could be found in these individuals. However, neither MIP analysis nor WES is able to reliably detect large deletions, duplications, inversions or other changes of this kind. Although rare, CNVs and large rearrangements in ABCA4 could be responsible for the lack of genetic diagnosis.
The frequency of pathogenic ABCA4 variants in the Polish population is relatively high (Table S2). According to Magueri’s hypothesis, compound heterozygous combinations of a mild and a severe variant would cause STGD1, moderate and severe variants would cause CRD, and severe variants on both chromosomes would result in RP [6]. Lately, a third category of very mild variants has been discovered. With the recent emergence of proof of pathogenicity in hypomorphic and deep intronic variants, a doctor has to be very careful in establishing the risks for future offspring and grandchildren of the affected individuals. For example, children of a patient with RP, due to the presence of two severe alleles in the parent, would have a different lifetime risk of developing retinal degeneration than in case of ‘regular’ recessive Mendelian disorders. A 100% chance of inheriting a severe allele from an affected parent by such a child would meet a possibility of getting one of the very mild common alleles from the unaffected parent. Combined together, these variants may appear in the population with a frequency even higher than 10%. Even though there is some non-penetrance, this risk would still be higher than in other rare diseases. This has a great impact on genetic counselling. Therefore, clinical geneticists should be thoroughly informed before giving reproductive advice to the patients and their family members.
Taken together, our results show that 39 individuals (58% of our cohort) could be genetically solved with just 11 of the most frequent variants depicted in Figure 2. Since next-generation sequencing is still not popular in Poland due to its costs, it may be an indication to screen for these mutations in the first instance. Especially with emerging new therapy prospects, patients have the right to a proper genetic diagnosis.
Acknowledgments
We would like to thank Mubeen Khan and Stéphanie S. Cornelis for their cooperation and assessment of intronic variants in four single-allelic ABCA4-related cases.
Supplementary Materials
The following are available online at https://www.mdpi.com/2073-4425/10/12/959/s1, Figure S1: Family pedigrees, Table S2: Clinical and genetic characteristics of all probands.
Author Contributions
Conceptualization, A.M.T., R.P. and K.H.C.; methodology, M.I.K., F.P.M.C.; software, A.H. (Arjen Henkes), A.H. (Alexander Hoischen), C.G., M.v.d.V.; investigation, K.H.C., E.C., A.R., J.M., B.K.-K., J.J.-J., M.R.; data curation, P.S.; writing—original draft preparation, A.M.T., A.R.; writing—review and editing, F.P.M.C., B.K.-K, M.R.; E.C.; project administration and funding acquisition, A.M.T.
Funding
This research was funded by the National Science Center (Poland), grant number UMO-2015/19/D/NZ2/03193.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Sullivan J.M. Focus on molecules: ABCA4 (ABCR)—An import-directed photoreceptor retinoid flipase. Exp. Eye Res. 2009;89:602–603. doi: 10.1016/j.exer.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lenis T.L., Hu J., Ng S.Y., Jiang Z., Sarfare S., Lloyd M.B., Esposito N.J., Samuel W., Jaworski C., Bok D., et al. Expression of ABCA4 in the retinal pigment epithelium and its implications for Stargardt macular degeneration. Proc. Natl. Acad. Sci. USA. 2018;115:E11120–E11127. doi: 10.1073/pnas.1802519115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cideciyan A.V., Aleman T.S., Swider M., Schwartz S.B., Steinberg J.D., Brucker A.J., Maguire A.M., Bennett J., Stone E.M., Jacobson S.G. Mutations in ABCA4 result in accumulation of lipofuscin before slowing of the retinoid cycle: A reappraisal of the human disease sequence. Hum. Mol. Genet. 2004;13:525–534. doi: 10.1093/hmg/ddh048. [DOI] [PubMed] [Google Scholar]
- 4.Allikmets R., Singh N., Sun H., Shroyer N.F., Hutchinson A., Chidambaram A., Gerrard B., Baird L., Stauffer D., Peiffer A., et al. A photoreceptor cell-specific ATP-binding transporter gene (ABCR) is mutated in recessive Stargardt macular dystrophy. Nat. Genet. 1997;15:236–246. doi: 10.1038/ng0397-236. [DOI] [PubMed] [Google Scholar]
- 5.Cremers F.P.M., van de Pol D.J., van Driel M.A., den Hollander A.I., van Haren F.J., Knoers N.V., Tijmes N., Bergen A.A.B., Rohrschneider K., Blankenagel A., et al. Autosomal recessive retinitis pigmentosa and cone-rod dystrophy caused by splice site mutations in the Stargardt’s disease gene ABCR. Hum. Mol. Genet. 1998;7:355–362. doi: 10.1093/hmg/7.3.355. [DOI] [PubMed] [Google Scholar]
- 6.Maugeri A., Klevering B.J., Rohrschneider K., Blankenagel A., Brunner H.G., Deutman A.F., Hoyng C.B., Cremers F.P. Mutations in the ABCA4 (ABCR) gene are the major cause of autosomal recessive cone-rod dystrophy. Am. J. Hum. Genet. 2000;67:960–966. doi: 10.1086/303079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allikmets R., Shroyer N.F., Singh N., Seddon J.M., Lewis R.A., Bernstein P.S., Peiffer A., Zabriskie N.A., Li Y., Hutchinson A., et al. Mutation of the Stargardt disease gene (ABCR) in age-related macular degeneration. Science. 1997;277:1805–1807. doi: 10.1126/science.277.5333.1805. [DOI] [PubMed] [Google Scholar]
- 8.Zernant J., Lee W., Collison F.T., Fishman G.A., Sergeev Y.V., Schuerch K., Sparrow J.R., Tsang S.H., Allikmets R. Frequent hypomorphic alleles account for a significant fraction of ABCA4 disease and distinguish it from age-related macular degeneration. J. Med. Genet. 2017;54:404–412. doi: 10.1136/jmedgenet-2017-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Runhart E.H., Sangermano R., Cornelis S.S., Verheij J.B.G.M., Plomp A.S., Boon C.J.F., Lugtenberg D., Roosing S., Bax N.M., Blokland E.A.W., et al. The common ABCA4 variant p.Asn1868Ile shows nonpenetrance and variable expression of Stargardt disease when present in trans with severe variants. Investig. Ophth. Vis. Sci. 2018;59:3220–3231. doi: 10.1167/iovs.18-23881. [DOI] [PubMed] [Google Scholar]
- 10.Zernant J., Lee W., Nagasaki T., Collison F.T., Fishman G.A., Bertelsen M., Rosenberg T., Gouras P., Tsang S.H., Allikmets R. Extremely hypomorphic and severe deep intronic variants in the ABCA4 locus result in varying Stargardt disease phenotypes. Cold Spring Harb. Mol. Case Stud. 2018;4:a002733. doi: 10.1101/mcs.a002733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bauwens M., Garanto A., Sangermano R., Naessens S., Weisschuh N., De Zaeytijd J., Khan M., Sadler F., Balikova I., Van Cauwenbergh C. ABCA4-associated disease as a model for missing heritability in autosomal recessive disorders: Novel noncoding splice, cis-regulatory, structural, and recurrent hypomorphic variants. Genet. Med. J. Am. Coll. Med. Genet. 2019;21:1761–1771. doi: 10.1038/s41436-018-0420-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sangermano R., Garanto A., Khan M., Runhart E.H., Bauwens M., Bax N.M., van den Born L.I., Khan M.I., Cornelis S.S., Verheij J. Deep-intronic ABCA4 variants explain missing heritability in Stargardt disease and allow correction of splice defects by antisense oligonucleotides. Genet. Med. Off. J. Am. Coll. Med. Genet. 2019;21:1751–1760. doi: 10.1038/s41436-018-0414-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cornelis S.S., Bax N.M., Zernant J., Allikmets R., Fritsche L.G., den Dunnen J.T., Ajmal M., Hoyng C.C.B., Cremers F.P.M. In silico functional meta-analysis of 5962 ABCA4 variants in 3,928 Stargardt disease and cone-rod dystrophy cases. Investig. Ophth. Vis. Sci. 2017;58:400–408. doi: 10.1002/humu.23165. [DOI] [PubMed] [Google Scholar]
- 14.Cremers F.P.M., Cornelis S.S., Runhart E.H., Astuti G.D.N. Author response: Penetrance of the ABCA4 p.Asn1868Ile allele in Stargardt Disease. Investig. Ophthalmol. Vis. Sci. 2018;59:5566–5568. doi: 10.1167/iovs.18-25944. [DOI] [PubMed] [Google Scholar]
- 15.Allikmets R., Zernant J., Lee W. Penetrance of the ABCA4 p.Asn1868Ile Allele in Stargardt Disease. Investig. Ophthalmol. Vis. Sci. 2018;59:5564–5565. doi: 10.1167/iovs.18-25579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sciezynska A., Ozieblo D., Ambroziak A.M., Korwin M., Szulborski K., Krawczynski M., Stawinski P., Szaflik J., Szaflik J.P., Ploski R., et al. Next-generation sequencing of ABCA4: High frequency of complex alleles and novel mutations in patients with retinal dystrophies from Central Europe. Exp. Eye Res. 2015;145:93–99. doi: 10.1016/j.exer.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 17.Weisschuh N., Feldhaus B., Khan M.I., Cremers F.P.M., Kohl S., Wissinger B., Zobor D. Molecular and clinical analysis of 27 German patients with Leber congenital amaurosis. PLoS ONE. 2018;13:e0205380. doi: 10.1371/journal.pone.0205380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li H., Durbin R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics. 2010;26:589–595. doi: 10.1093/bioinformatics/btp698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Picard A set of command line tools (in Java) for manipulating high-throughput sequencing (HTS) data and formats such as SAM/BAM/CRAM and VCF. [(accessed on 21 November 2019)]; Available online: http://broadinstitute.github.io/picard/
- 20.Poplin R., Ruano-Rubio V., DePristo M.A., Fennell T.J., Carneiro M.O., Van der Auwera G.A., Kling D.E., Gauthier L.D., Levy-Moonshine A., Roazen D., et al. Scaling accurate genetic variant discovery to tens of thousands of samples. bioRxiv. 2018:201178. doi: 10.1101/201178. [DOI] [Google Scholar]
- 21.Khan M., Cornelis S.S., del Pozo-Valero M., Whelan L., Runhart E.H., Mishra K., Bults F., AlSwaiti Y., AlTabishi A., De Baere E., et al. Resolving the dark matter of ABCA4 for 1054 Stargardt disease probands through integrated genomics and transcriptomics. bioRxiv. 2019:817767. doi: 10.1101/817767. [DOI] [PubMed] [Google Scholar]
- 22.Sangermano R., Khan M., Cornelis S.S., Richelle V., Albert S., Garanto A., Elmelik D., Qamar R., Lugtenberg D., van den Born L.I., et al. ABCA4 midigenes reveal the full splice spectrum of all reported noncanonical splice site variants in Stargardt disease. Genome Res. 2018;28:100–110. doi: 10.1101/gr.226621.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yatsenko A.N., Shroyer N.F., Lewis R.A., Lupski J.R. An ABCA4 genomic deletion in patients with Stargardt disease. Hum. Mutat. 2003;21:636–644. doi: 10.1002/humu.10219. [DOI] [PubMed] [Google Scholar]
- 24.Zernant J., Xie Y.A., Ayuso C., Riveiro-Alvarez R., Lopez-Martinez M.A., Simonelli F., Testa F., Gorin M.B., Strom S.P., Bertelsen M., et al. Analysis of the ABCA4 genomic locus in Stargardt disease. Hum. Mol. Genet. 2014;23:6797–6806. doi: 10.1093/hmg/ddu396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nasser F., Kurtenbach A., Kohl S., Obermaier C., Stingl K., Zrenner E. Retinal dystrophies with bull’s-eye maculopathy along with negative ERGs. Doc. Ophthalmol. 2019;139:45–57. doi: 10.1007/s10633-019-09694-7. [DOI] [PubMed] [Google Scholar]
- 26.Rivera A., White K., Stohr H., Steiner K., Hemmrich N., Grimm T., Jurklies B., Lorenz B., Scholl H.P., Apfelstedt-Sylla E., et al. A comprehensive survey of sequence variation in the ABCA4 (ABCR) gene in Stargardt disease and age-related macular degeneration. Am. J. Hum. Genet. 2000;67:800–813. doi: 10.1086/303090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hargitai J., Zernant J., Somfai G.M., Vamos R., Farkas A., Salacz G., Allikmets R. Correlation of clinical and genetic findings in Hungarian patients with Stargardt disease. Investig. Ophthalmol. Vis. Sci. 2005;46:4402–4408. doi: 10.1167/iovs.05-0504. [DOI] [PubMed] [Google Scholar]
- 28.Trezza A., Bernini A., Langella A., Ascher D.B., Pires D.E.V., Sodi A., Passerini I., Pelo E., Rizzo S., Niccolai N., et al. computational approach from gene to structure analysis of the human ABCA4 transporter involved in genetic retinal diseases. Investig. Ophthalmol. Vis. Sci. 2017;58:5320–5328. doi: 10.1167/iovs.17-22158. [DOI] [PubMed] [Google Scholar]
- 29.Garces F., Jiang K., Molday L.L., Stohr H., Weber B.H., Lyons C.J., Maberley D., Molday R.S. Correlating the expression and functional activity of ABCA4 disease variants with the phenotype of patients with stargardt disease. Investig. Ophthalmol. Vis. Sci. 2018;59:2305–2315. doi: 10.1167/iovs.17-23364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang N., Tsybovsky Y., Kolesnikov A.V., Rozanowska M., Swider M., Schwartz S.B., Stone E.M., Palczewska G., Maeda A., Kefalov V.J., et al. Protein misfolding and the pathogenesis of ABCA4-associated retinal degenerations. Hum. Mol. Genet. 2015;24:3220–3237. doi: 10.1093/hmg/ddv073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee W., Xie Y., Zernant J., Yuan B., Bearelly S., Tsang S.H., Lupski J.R., Allikmets R. Complex inheritance of ABCA4 disease: Four mutations in a family with multiple macular phenotypes. Hum. Genet. 2016;135:9–19. doi: 10.1007/s00439-015-1605-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huckfeldt R.M., East J.S., Stone E.M., Sohn E.H. Phenotypic Variation in a Family With Pseudodominant Stargardt Disease. JAMA Ophthalmol. 2016;134:580–583. doi: 10.1001/jamaophthalmol.2015.5471. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.