Abstract
Introduction
Vitamin D deficiency is common in spinal surgery and critical care. Hypovitaminosis D may impact on outcomes in cranial neurosurgical care and play roles in underlying disease processes.
Methods
A prospective observational cohort study was performed. All emergency cranial neurosurgical ward admissions from 1st January to 10th May 2017 were screened for inclusion (n = 406). Patients already receiving vitamin D supplementation, spinal patients and elective admissions were excluded. Admission vitamin D levels were checked for all remaining patients (n = 95). Patients with vitamin D <30 nmol/L were defined as “deficient” and those 30‐50 nmol/L as “inadequate.” All patients with levels <50 nmol/L were replaced, as per local guidelines. Descriptive analyses of the cohorts were undertaken, with multivariate regression used to assess the effect of vitamin D on length of stay, inpatient morbidity and mortality.
Results
The median age of participants was 61 years (n = 95; 57% male, 43% female). The median vitamin D level was 23 nmol/L (deficient). 84% (n = 80) of patients had low vitamin D levels, with 61% (n = 58) classed as deficient (<30 nmol/L). Vitamin D deficiency rates were similar in those aged below 65 years (86%; n = 38/44) and those above 65 years (82%; n = 42/51). Deficient vitamin D level was associated with longer hospital stay (P = .03), and this relationship persisted after adjusting for potential confounders such as age, sex and preadmission Charlson co‐morbidity index. No statistically significant association was seen with vitamin D status and inpatient morbidity or mortality.
Conclusions
Vitamin D deficiency is common in cranial neurosurgical patients, even in predefined low‐risk groups (age <65). Lower vitamin D level was associated with longer length of stay. This study supports the need for: (a) further investigation into the roles of vitamin D in neurosurgical pathologies and management and (b) an appropriately powered, randomised investigation into the impact of vitamin D status upon neurosurgical diagnoses and complications.
Keywords: neuroendocrinology, neurosurgery, surgery, vitamin D
Vitamin D deficiency may have negative impacts upon clinical outcomes of surgical patients. The prevalence of hypovitaminosis D was identified in a cohort of emergency neurosurgical patients (84%; n = 80/95). Low vitamin D was significantly associated with a prolonged inpatient stay. There is a need for a larger investigation into the clinical impact of hypovitaminosis D upon neurosurgical diagnoses and complications.

1. INTRODUCTION
Vitamin D deficiency is common, with low levels thought to be as prevalent as 40%‐60% in patient groups with risk factors for vitamin D deficiency.1 These risk factors include being over 65 years old, frailty, body weight, systemic co‐morbidities, skin pigmentation and reduced sun exposure. These patient groups commonly present to neurosurgical units with cranial pathology. Vitamin D deficiency has also been associated with adverse outcomes in neurocritical care settings1, 2 and spinal surgery.3 Vitamin D deficiency could therefore impact on complications and outcomes in neurosurgical care and may even play roles in underlying disease processes. This is because vitamin D is thought to play key roles in tissue homeostasis, wound healing, neurone function and, potentially, neuroinflammation.4, 5
Studies have identified that supplementation of vitamin D to inpatients with hypovitaminosis D can reduce mortality and morbidity.6 These works have focussed on specific patient populations, such as spinal surgery, medical patients and critical care units.1, 2 However, the prevalence of hypovitaminosis D in cranial neurosurgical patients at a ward‐based level remains unclear. It is also uncertain whether low vitamin D might be an independent risk factor for mortality, morbidity and other poor outcomes in these patients. This study prospectively assessed the prevalence of hypovitaminosis D in cranial neurosurgical ward patients admitted over the winter months to a tertiary neurosurgical unit. This work also studied the association between low vitamin D levels in these patients and clinical outcomes such as mortality, length of stay, inpatient morbidity and patient disability at discharge.
2. MATERIALS AND METHODS
Figure 1 describes the methodology of this prospective cohort study. All patients admitted to a single neurosurgical unit at ward‐level were screened for inclusion. Serum 25‐hydroxy vitamin D concentrations were taken from eligible adult patients admitted for cranial neurosurgical pathologies, such as debulking of cranial tumours, cerebrovascular events, traumatic brain injuries, cerebral abscesses and hydrocephalus. Admission vitamin D levels were classified using Institute of Medicine (IOM) international reference ranges.7 Vitamin D levels >50 nmol/L were defined as “sufficient.” Levels 30‐50 nmol/L were defined as “inadequate.” Vitamin D levels <30 nmol/L were defined as “deficient.” Those found to have a level <50 nmol/L (inadequate or deficient) received replacement therapy, as per local public health guidelines, with oral vitamin D supplements (Stexerol (Colecalciferol) 1000 unit tablets; 4000 units daily for 10 weeks then 1000 units daily).8 The data were collected and analysed as described in Figure 1.
Figure 1.
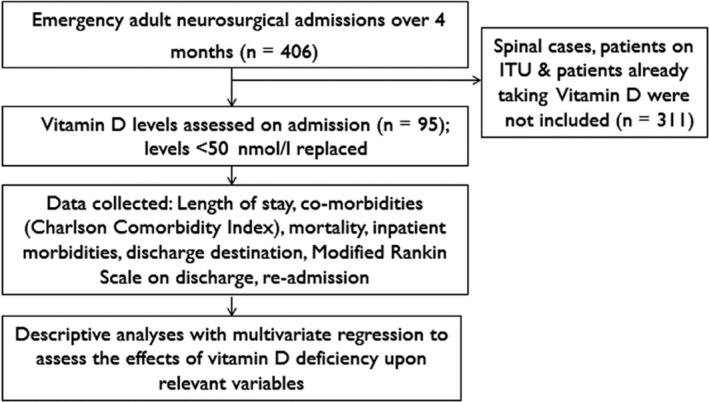
Flowchart outlining the study methodology
Vitamin D levels are known to fluctuate with seasonal variations in sunlight.4 To avoid this variability confounding the study results, the study was conducted over a single season, (winter) such that regional sunlight levels were relatively constant during the time span of the study.
Statistical analyses were completed using descriptive statistics, and multivariate logistical regression analysis using SPPS© software. A normal distribution was approximated using a log transformation, to permit linear regression analysis, which permitted adjusted analyses for suspected confounding variables (eg age, Charlson Co‐morbidity index).
3. RESULTS
Of the 95 patients who met the inclusion criteria, 54 (57%) were male and 41 (43%) were female, with a median age being 61 years (18‐94 years). The median vitamin D level was 23 nmol/L (range 10‐89 nmol/L), which is deficient. 80 patients (84%) had vitamin D <50 nmol/L, necessitating treatment. Vitamin D deficiency rates were similar in those aged below 65 years (86%; n = 38/44) and those above 65 years (82%; n = 42/51), despite older age being a risk factor for vitamin D deficiency. No patients in the study cohort were taking any vitamin D supplements prior to admission to hospital Figure 1.
Table S1 (see Supplementary data) outlines demographic features and clinical outcomes of the study population. Key points include that 61% (n = 58) of patients were identified to be deficient (<30 nmol/L) in vitamin D levels. “Inpatient morbidity” refers to complications such as systemic infection, wound dehiscence or infection, thromboembolism, recollection of the original pathology or other noninfective medical complications. Of the 38 patients in this subcohort who developed at least one of these issues whilst an inpatient, 33 (87%) presented with inadequate or deficient vitamin D levels. Other markers of inpatient outcomes, such as length of stay, return to theatre and disability score at discharge (assessed via the modified Rankin Scale) all identified higher proportions of patients with worse outcomes in the hypovitaminosis D group. There was no statistically significant difference in mortality between vitamin D replete (n = 2/15; 13%) and vitamin D deficient (n = 5/80; 6%) patients.
Figure 2 illustrates that the majority of patients in the study cohort had a suboptimal vitamin D level on admission. Figure 3 outlines the distribution of cranial pathologies amongst patients in the study, and that hypovitaminosis D was more common than adequate vitamin D levels across the entire range of neurosurgical pathologies studied, such as patients with neurovascular conditions (SAH), neurotrauma and intracranial neoplasms or infections.
Figure 2.
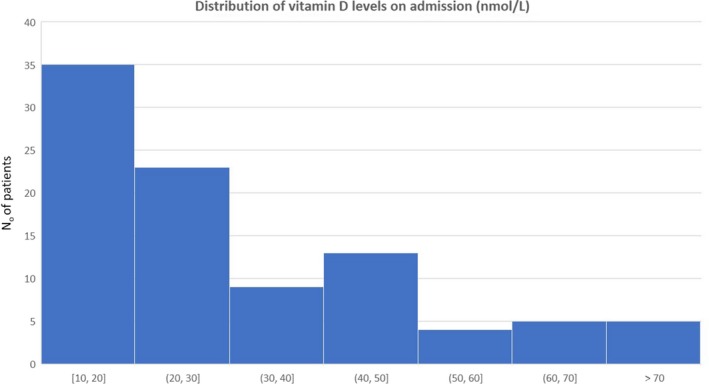
Histogram of vitamin D levels on admission. The majority of patients in the cohort had inadequate (30‐50 nmol/L) or deficient (<30 nmol/L) vitamin D level on admission
Figure 3.

The distribution of vitamin D deficiency amongst varying pathologies in the study cohort. The majority of patients with emergency neurosurgical conditions were identified to have low vitamin D levels. ASDH, Acute subdural haematoma; CSDH, Chronic subdural haematoma; EDH, Extradural haematoma; ICH, intracerebral haemorrhage; SAH, Subarachnoid haemorrhage; SOL, space occupying lesion; TBI, traumatic brain injury
Figure 4 highlights the effect of vitamin D levels on length of inpatient stay in the neurosurgical unit. A median length of stay of 13 days was identified in patients with a normal vitamin D level (range = 3‐22 days). The median length of stay for patients with deficient or inadequate vitamin D levels was 16 days (range = 8‐26). This difference reached statistical significance, even after adjusting analyses for age, sex, ethnicity and admission Charlson co‐morbidity index (P = .03). There was no statistically significant correlation between vitamin D and patient mortality rates, inpatient morbidity or a patient's discharge modified Rankin scale.
Figure 4.

Box plot showing the effect of vitamin D on the median length of stay (LOS). Low (inadequate or deficient) vitamin D was significantly associated with a longer inpatient LOS in the neurosurgical unit compared to vitamin D replete patients (16 days Vs 13 days). Normal vitamin D: serum 25‐hydroxy vitamin D >50 nmol/L. Inadequate or deficient (low) vitamin D: serum 25hydroxy vitamin D ≤50 nmol/L. LOS, length of stay
4. DISCUSSION
To our knowledge, this is the first study to review the prevalence of vitamin D levels in cranial neurosurgical ward patients and assess their clinical outcomes. Hypovitaminosis D was common throughout the cohort, with a prevalence of 84%, with a prevalence in the younger subcohort of 86%. By contrast, the prevalence of hypovitaminosis D in young, healthy populations is approximately 36%9 and 50%‐70% of acutely unwell patients.2, 10 Hypovitaminosis D may therefore be more common in neurosurgical patients compared to healthy adults and patients with other systemic pathologies.
Despite many different risk factors affecting vitamin D levels,1, 3 its statistically significant correlation with length of hospital stay was still observed when statistical adjustments for potential confounders, such as patient age, ethnicity and co‐morbidities, were performed. Thus, the effects of vitamin D deficiency on length of stay identified in this cohort may be a genuine effect, being independent of the analysed potential confounding factors. However, caution is needed in interpretating these results due to possibility of residual confounding.
Whilst previous works have not found significant correlations between hypovitaminosis D and length of ward stay,11 these small studies focussed on general surgical patients, and therefore it remains plausible that vitamin D deficiency may be of key significance in neurosurgical patients. The increased length of hospital stay could have significant economic repercussions, with an average hospital bed in recovery after high risk operation, such as neurosurgery or cardiac surgery, costing between £300 and £700 per day.12, 13, 14
Vitamin D did not have any statistically significant correlation with patient mortality or morbidity. In the neurocritical care setting, associations between hypovitaminosis D and increased mortality and morbidity have been demonstrated.1, 6 These studies involved larger cohorts of intensive care patients, and it is possible that the present study was underpowered to detect significant differences in mortality or morbidity between the vitamin D deficient and nondeficient groups. However, it is also possible that vitamin D takes on a greater role in promoting convalescence and recovery in critically ill patients, who have severe, multisystemic pathologies.15
There is mounting evidence that vitamin D may play important roles in the nervous system, from neurodevelopment in animal models, adult neuronal metabolic activity and potential mediating effects on neurotrophic factors and, hence, neuronal recovery.16 It is also known that vitamin D has a role in systemic and neuroinflammatory responses, both directly and indirectly influencing a variety of immune cells.17 Vitamin D deficiency may therefore have important functions in recovery and repair after brain injury, but also potentially in the pathogenesis of neurosurgical diseases related to neuroinflammation.
The present study has a relatively small sample size. The nature of the variable studied (vitamin D) means there is a high risk of confounding in the identified associations. This limits the power of our study to detect differences in patient length of stay, morbidity and mortality. The relatively ethnically homogenous study group and the single‐centre study design also limit the generalisability of the study findings.4 Furthermore, the study was conducted over winter months in a centre‐based in the Northern hemisphere, when vitamin D levels in the general population are known to reach a nadir.5 However, this design ensured that seasonal variation in baseline vitamin D level was not a confounding factor in the present work; there remains a need to continue this investigation during summer months. This would assess whether the prevalence and impact of hypovitaminosis D varies by season for the study population. Further investigations using pooled data from multiple neurosurgical units, possible from similar latitudes to avoid seasonal confounding of vitamin D levels, would improve the power of a study assessing the effects of hypovitaminosis D on neurosurgery patients.
Another factor to consider is that vitamin D binding protein may act as a negative acute phase reactant in systemic illness and inflammatory states, thereby correlating with low serum vitamin D levels.18 This was mitigated by ensuring all patients in our study had their vitamin D levels drawn prior to any surgery, and none were critically unwell such as to require level 3 intensive care. Measuring levels of VDBP may be advisable in future studies, to identify whether it influences vitamin D levels in neurosurgical patients.
We were duty‐bound to treat patients who had vitamin D deficiency diagnosed on admission to the unit. Whilst this has the potential to bias the study's conclusions, it would tend to do so towards the null hypothesis.6 Therefore, the true effects of hypovitaminosis D on neurosurgery patients may be even more pronounced than that reported in the present study. A comparison of long‐term outcomes in patients with normal and low vitamin D on neurosurgical admission remains to be completed, and there may be value in comparing the prevalence of vitamin D deficiency in our patient population with its prevalence in our local, healthy population. The need for a randomised study to assess the impact of vitamin D supplementation in neurosurgery, which could review factors such as patient length of stay, morbidity and mortality verses a placebo arm, should be considered.
In conclusion, vitamin D deficiency is common in neurosurgical patients, even in predefined “low risk” groups (eg age <65). Lengths of stay for patients who were deficient were prolonged. A key limitation of this study is the high risk of confounding or residual confounding; therefore, it remains to be seen whether immediate supplementation would bring with it clinical benefits. Furthermore, a small number of patients in the study cohort had particularly long stays, which increases the risk of a spurious association being identified. However, given the widespread effects of vitamin D on numerous body systems, the possibility of a true impact of vitamin D deficiency on clinical outcomes seems plausible. Therefore, this data supports further investigation into the role of vitamin D in neurosurgical pathological mechanisms and management, as well as an appropriately powered, randomised investigation into the impact of vitamin D status upon neurosurgical diagnoses, complications and clinical outcomes.
CONFLICT OF INTERESTS
The authors have no conflicts of interests to report. The data that support the findings of this study are available from the corresponding author upon reasonable request.
AUTHOR CONTRIBUTIONS
CH, PT, SD and PS developed the concept and design of the study and developed the manuscript. RV, PS, JF and WFJ completed the data collection and analysis and developed the manuscript. PT and SD also aided in the data collection and analysis for the study.
ETHICAL APPROVAL
This study complied with the principles outlined in the Declaration of Helsinki for medical research involving human participants. This study received ethical approval from the local University Health Board research ethics committee.
Supporting information
ACKNOWLEDGEMENTS
The authors acknowledge the assistance of Dr Dev Datta of The University Hospital of Wales, who aided in the reporting of vitamin D levels for this study.
Ved R, Taylor P, Stewart P, et al. Vitamin D deficiency is endemic in neurosurgical patients and is associated with a longer length of inpatient stay. Endocrinol Diab Metab. 2020;3:e00097 10.1002/edm2.97
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Ardehali SH, Dehghan S, Baghestani AR, Velayati A, Shariatpanahi ZV. Association of admission serum levels of vitamin D, calcium, Phosphate, magnesium and parathormone with clinical outcomes in neurosurgical ICU patients. Sci Rep. 2018;8(1):2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Higgins DM, Wischmeyer PE, Queensland KM, Sillau SH, Sufit AJ, Heyland DK. Relationship of vitamin D deficiency to clinical outcomes in critically ill patients. J Parenter Enter Nutr. 2012;36(6):713‐720. [DOI] [PubMed] [Google Scholar]
- 3. Mabey T, Singhatanadgige W, Yingsakmongkol W, Limthongkul W, Honsawek S. Vitamin D and spine surgery. World J Ortho. 2016;7(11):726‐730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grace C, Vincent R, Aylwin SJ. High prevalence of vitamin D insufficiency in a United Kingdom urban morbidly obese population: implications for testing and treatment. Surg Obes Relat Dis. 2014;10(2):355‐360. [DOI] [PubMed] [Google Scholar]
- 5. Zgaga L, Theodoratou E, Farrington SM, et al. Diet, environmental factors, and lifestyle underlie the high prevalence of vitamin D deficiency in healthy adults in Scotland, and supplementation reduces the proportion that are severely deficient. J Nutr. 2011;141(8):1535‐1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guan J, Karsy M, Brock AA, et al. A prospective analysis of hypovitmainosis D and mortality in 400 patient in the neurocritical care setting. J Neurosurg. 2016;127(1):1‐7. [DOI] [PubMed] [Google Scholar]
- 7. Vieth R, Holick M. The IOM—Endocrine Society Controversy on recommended vitamin D targets. In support of the endocrine society position In: Feldman D, ed. Vitamin D: Biochemistry, Physiology and Diagnostics, Vol. 4 London:Elsevier;2018:1091‐1107. [Google Scholar]
- 8. Datta D, Turk A, Stephens E, Stone M, Warner J, Body G. Guidelines on the Diagnosis and Management of Vitamin D Deficiency in Children and Adults. New York: Cardiff and Vale University Health Board Medicines Management Group Guidelines; 2016:1–19. [Google Scholar]
- 9. Tangpricha V, Pearce EN, Chen TC, Holick MF. Vitamin D insufficiency among free‐living healthy young adults. Am J Med. 2002;112(8):659‐662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Biliniski K, Boyages S. The rise and rise of vitamin D testing. BMJ. 2012;345:e4743. [DOI] [PubMed] [Google Scholar]
- 11. Flynn L, Zimmerman LH, McNorton K, et al. Effects of vitamin D deficiency in critically ill surgical patients. Am J Surg. 2012;203(3):379‐382. [DOI] [PubMed] [Google Scholar]
- 12. Beauregard CL, Friedman WA. Routine use of postoperative ICU care for elective craniotomy: a cost‐benefit analysis. Surg Neurol. 2003;60:483‐489. [DOI] [PubMed] [Google Scholar]
- 13. National Institiute for Health and Care Excellence (NICE) Costing statement . Implementing the NICE guideline on Transition between inpatient hospital settings and community or care home settings for adults with social care needs In: Ausman J, ed. Putting NICE Guidance into Practice, Vol. 1 London:Elsevier;2015:1‐14. [Google Scholar]
- 14. Cardiff and Vale University Health Board . Freedom of Information act Request – Cardiac Beds Day Costs, Vol. 1 California:Cardiff and Vale University Health Board; 2000:1‐2. [Google Scholar]
- 15. Norman AW. From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health. Am J Clin Nutr. 2008;88(2):491s‐s499. [DOI] [PubMed] [Google Scholar]
- 16. Harms LR, Burne T, Eyles DW, McGrath JJ. Vitamin D and the brain. Best Pract Res Clin Endocrinol Metab. 2011;25(4):657‐669. [DOI] [PubMed] [Google Scholar]
- 17. Guillot X, Semerano L, Saidenberg‐Kermanac'h N, Falgarone G, Boissier MC. Vitamin D and inflammation. Joint Bone Spine. 2010;77(6):552‐557. [DOI] [PubMed] [Google Scholar]
- 18. Waldron J, Ashby H, Cornes M, et al. Vitamin D: a negative acute phase reactant. Journal of Clinical Pathology. 2013;66:7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


