Abstract
Leiomyomas are classified as benign mesenchymal neoplasms and consist of smooth muscle cells with variable amounts of fibrous stroma. The tumors occur most frequently in the uterus, affecting 20%–30% of women of reproductive age, but vaginal leiomyomas are rare with only around 300 cases reported since the first case was described in 1733. These tumors are thought to arise from Müllerian smooth muscle cells in the subepithelium of the vagina. Here, we present a case of vaginal leiomyoma who presented as left vaginal wall mass.
KEYWORDS: Enucleation, leiomyoma, mass
INTRODUCTION
Fibroid tumors (leiomyoma) of the female genital tract are common benign tumors in the uterus and to some extent, in the cervix, followed occurrences in the round ligament, the uterosacral ligament, ovaries, and inguinal canal. Moreover, its presentation in the vagina is the rarest of all.
Though Young et al.[1] observed two cases of vaginal tumors are rare and include papilloma, hemangioma, mucus polyp, and rarely leiomyoma. Vaginal leiomyomas remain an uncommon entity with only about 300 reported cases since the first detected case back in 1733 by Denys de Leyden Bennett and Erlich.[2] Vaginal wall tumors are most commonly seen in anterior wall of the vagina elsewhere presentation is still unusual. Here, we report the case of medial vaginal wall leiomyoma.
CASE REPORT
A 45-year-old female gravid 3, parity 3 adopted with terminal sterilization method reported first to the casualty with constipation for 3 days. She underwent ultrasonography of the abdomen and pelvis to find the cause of constipation. Ultrasonography abdo-pelvis did not reveal any pathology in the abdomen and pelvis. On further probing, she presented complaints of mass in vaginal opening for 1½ years. Mass was slow-growing associated with pain on and off along with discharge.
On examination, her vital were stable. On per abdominal examination, the abdomen was soft, nontender, and no mass was felt. On per speculum examination, small mass was seen arising from left vaginal wall in the lower third of the area. On palpation, it had cystic to firm consistency. Pap smear was taken which reported bacterial vaginosis.
A transvaginal ultrasonography was performed. A well-defined heterogeneous predominantly hypoechoic lesion of size 1.9 × 1.9 arising from the left lower one-third vaginal wall was noted. There was no other abnormality on ultrasonography. The tumor was surgically removed by the vaginal route. A Foleys catheter was introduced in the urethra for protecting the latter. The tumor was then sent for histopathological examination. Gross examination revealed a 3 cm × 2 cm × 1.5 cm irregular, firm grayish-white tissue mass. Microscopically, well-circumscribed mass composed of intersecting and interlacing fascicles of smooth muscle fibers arranged in whorled pattern. Moreover, intervening scanty stroma composed of fibroconnective tissue along with focal hyaline changes [Figure 1]. These findings were consistent with diagnosis of vaginal leiomyoma (fibroid).
Figure 1.
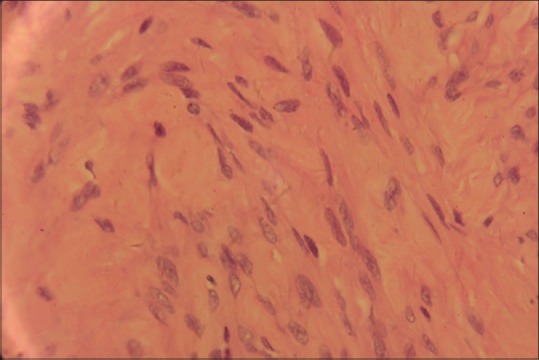
Slide showing the aggregation of spindle cells confirming leiomyoma
DISCUSSION
Extrauterine fibroids are rare benign neoplasm, which may cause diagnostic difficulties. Leiomyomas in the female genital tract are common in the uterus and to some extent in the cervix followed by the round ligament, uterosacral ligament, ovary, and inguinal canal.
The occurrence of vaginal leiomyomas is very rare. They are usually seen in the age group of 35–50 years old[3] and are reported to be more common among Caucasian women, while uterine leiomyomas are more common among non-Caucasian groups.[4,5,6] Vaginal leiomyomas are usually situated in the midline anterior vaginal wall as a single, well-circumscribed mass. In this instance, it was left vaginal wall mass located in the lower one-third of the vagina.
Vaginal leiomyoma has varied presentation may include vaginal bleeding, lower abdominal pain, frequency of micturition, dyspareunia, dysuria, or other features of urinary obstruction. The present case reported with constipation and abdominal pain.[3,7]
Usually, these tumors are single, benign, and slow-growing, but sarcomatous transformation has been reported.[8] Preoperatively, diagnosis by ultrasonography may be difficult, but magnetic resonance imaging usually clinches the diagnosis. In magnetic resonance imaging, they appear as well-demarcated solid masses of low signal intensity in T1- and T2-weighted images, with homogeneous contrast enhancement, while leiomyosarcomas and other vaginal malignancies show characteristic high T2 signal intensity with irregular and heterogeneous areas of necrosis or hemorrhage.[9,10] However, histopathological confirmation is the gold standard of diagnosis and also beneficial to rule out any possible focus of malignancy.
The most effective approach to surgery depends on the size and location of the fibroid. This is either by abdominal or vaginal route. There are instances where abdominoperineal approach has been employed.
The tumor must be removed en masse to avoid its recurrence and propensity to malignant transformation.[8] In the present scenario, we underwent en masse enucleation (myomectomy) to prevent further recurrence.
CONCLUSION
Although vaginal tumors are rare, care must be given in identifying the tumor at an early stage in view of its potential to get malignant transformation. Vaginal leiomyoma may present with various presentations; hence, probing is necessary while taking medical history. It has been advisable to execute en masse enucleation to prevent its recurrence and malignant transformation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Young SB, Rose PG, Reuter KL. Vaginal fibromyomata: Two cases with preoperative assessment, resection, and reconstruction. Obstet Gynecol. 1991;78:972–4. [PubMed] [Google Scholar]
- 2.Bennett HG, Jr, Erlich MM. Myoma of the vagina. Am J Obstet Gynecol. 1941;42:314–20. [Google Scholar]
- 3.Chakrabarti I, De A, Pati S. Vaginal leiomyoma. J Midlife Health. 2011;2:42–3. doi: 10.4103/0976-7800.83274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Östör AG. Tumours of the vagina: Mesenchymal tumours. In: Tavassoli FA, Devilee P, editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Breast and Female Genital Organs. Ch. 6. Lyon: IARC Press; 2003. [Google Scholar]
- 5.Nel CP, Tiltman AJ. Leiomyoma of the vagina. S Afr Med J. 1978;54:816–7. [PubMed] [Google Scholar]
- 6.Pulfus E, Newcomer J. Vaginal wall mass. Obstet Gynecol Surv. 1999;54:149–50. doi: 10.1097/00006254-199903000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Sim CH, Lee JH, Kwak JS, Song SH. Necrotizing ruptured vaginal leiomyoma mimicking a malignant neoplasm. Obstet Gynecol Sci. 2014;57:560–3. doi: 10.5468/ogs.2014.57.6.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cobanoǧlu O, Gürkan Zorlu C, Ergun Y, Kutluay L. Leiomyosarcoma of the vagina. Eur J Obstet Gynecol Reprod Biol. 1996;70:205–7. doi: 10.1016/s0301-2115(95)02554-5. [DOI] [PubMed] [Google Scholar]
- 9.Bae JH, Choi SK, Kim JW. Vaginal leiomyoma: A case report and review of the literature. J Women's Med. 2008;1:92–4. [Google Scholar]
- 10.Shadbolt CL, Coakley FV, Qayyum A, Donat SM. MRI of vaginal leiomyomas. J Comput Assist Tomogr. 2001;25:355–7. doi: 10.1097/00004728-200105000-00005. [DOI] [PubMed] [Google Scholar]


