Abstract
Menopause has been identified as a high-risk stage for weight gain in a woman's lifecycle. Menopause-related weight gain is a consequence of low circulating estrogen levels due to progressive loss of ovarian function. Moreover, the changes in the hormonal milieu, chronological aging, decline in physical activity coupled with westernized dietary pattern, and recurrent emotional eating episodes associated with psychological distress also contribute to the increase in total body fat and waist circumference. Higher waist circumference is an independent risk factor for cardiovascular and metabolic disease in menopausal women. These obesity-related cardiometabolic risk factors and menopausal symptoms can be effectively managed by achieving clinically significant weight loss through lifestyle modification. Behavioral lifestyle intervention uses behavioral techniques for counseling corrective dietary and physical activity practices in achieving sustainable weight loss outcomes. Majority of menopausal women seek this counseling from gynecologist, especially in primary care settings due to nonavailability of multidisciplinary teams. Thus, the aim of the review is to understand the menopause-obesity link, associated risk factors, and its health-related burden in perimenopausal women to devise a practical women-centric weight management module based on lifestyle modification techniques to address the burden of menopausal obesity in regular gynecological practice.
KEYWORDS: Diet, lifestyle management, menopause, obesity, physical activity, weight loss
INTRODUCTION
Menopause is a crucial event in a woman's life as she witnesses several physical and psychological changes during the transition. One such important change is the increase in body weight and an alteration in fat distribution increasing the risk of menopausal symptoms and metabolic disorders. The severity of menopausal symptoms is higher among obese women as compared to nonobese women, and clinically significant weight loss results in marked improvement of these symptoms, especially hot flashes, mood disorders, and sleep disturbances.[1] However, achieving clinically significant weight loss is far more challenging in perimenopausal women due to several factors. This review aims to understand the association between menopause and obesity and its impact on women in perimenopausal age group. Besides, we have suggested a weight management module for its management.
BURDEN OF OBESITY IN MENOPAUSAL WOMEN
The problem of obesity is rising at an alarming rate, with disproportionately higher prevalence in female than male counterparts. This trend can largely be attributed to differences in age-specific reproductive cycles (pregnancy, lactation, and menopause) in women. A pooled analysis of international studies on menopausal obesity reports that almost 39% women undergoing menopausal transition are either overweight or obese.[2] In the Indian context, the proportion of overweight/obese women increases from 4% at younger age to 34% at middle and older age.[3] This steep increase in the prevalence of obesity in middle-aged women coincides with the initiation of the menopausal transition.
Nearly, 401 million perimenopausal women in our country will be predisposed to the risk of menopausal obesity by 2026.[4] Obese women at this stage are exposed to the dual burden of menopausal symptoms and metabolic complications of obesity for the rest of their life.[5] Weight gain at this stage can be partly attributed to the lack of awareness among middle-aged women toward their health-related issues as they prioritize the wellness of their family members over their own. This neglect impedes the initiation of any weight loss intervention by them, further aggravating the problem of weight gain. The massive proportions of menopausal women and the affected number of life years due to obesity and its consequences make it an issue of public health concern.
PATHOPHYSIOLOGY: MECHANISM OF MENOPAUSAL OBESITY
The mechanism of the development of obesity in menopausal women is outlined in Figure 1. The continuous depletion of the follicular ovarian pool during menopausal transition lowers estrogen production with a relative increase in androgen levels. This hormonal imbalance alters energy homeostasis by regulating hunger and satiety signals.[6] Estrogen inhibits the action of hunger signals, preventing events of excessive calorie consumption. It is postulated that during the menopausal transition because of fluctuating estrogen levels, its effectiveness to modulate hunger hormones is reduced.[7] Menopausal women experience more intense hunger signals encouraging increased food intake which promotes weight gain.
Figure 1.
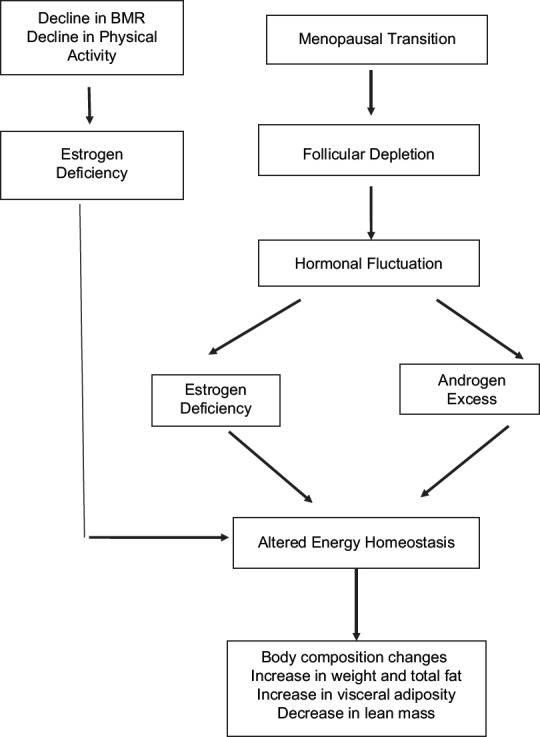
Mechanism for development of obesity during menopausal transition
The hormonal imbalance during menopause also promotes the higher accumulation of fat in the abdominal region. Low estrogen levels along with high androgen levels lead to redistribution of fat present in the gluteal and femoral regions to abdominal regions of the body, favoring abdominal obesity.[8] Besides, higher abdominal obesity is an independent risk factor for future metabolic complications.[9]
Menopausal obesity is primarily driven by hormonal imbalance and its effect on energy balance. Some other crucial factors, such as unhealthy eating behavior, sedentary lifestyle, and secondary causes (hypothyroidism, cushing syndrome, and medication) might also account for the differences in personal weight gain trajectories among these women.
RISK FACTORS OF MENOPAUSAL OBESITY
Obesity in menopausal women is a result of several modifiable and nonmodifiable factors. Nonmodifiable factors comprise of physiological factors, whereas psychosocial and lifestyle-related behaviors are categorized as modifiable risk factors, as depicted in Table 1.[10] Physiological risk factors such as chronological aging, slower basal metabolic rate (BMR), hormonal fluctuations, and the presence of metabolic disorders affect the pace of weight gain. Hormonal fluctuations experienced during the transition are strongly associated with psychological distress.[11] Women generally deal with distress by indulging in unhealthy eating behavior. Excessive caloric intake coupled with an overall sedentary lifestyle is conventionally associated with weight gain in menopausal women. The key factors driving the prevalence of obesity in menopausal women are briefly discussed below:
Table 1.
Etiological factors in menopausal obesity
| Physiological factors | Hormonal factor | Lifestyle-related factors | Psychological distress |
|---|---|---|---|
| Aging Decrease in BMR Decrease in lean mass Secondary causes (hypothyroidism, PCOS etc.) Musculoskeletal disorders |
Hypoestrogenemia Hyperandrogenemia |
Excessive caloric intake Low dietary fiber intake Excessive SSB intake Processed and convenience food (primarily energy-dense) consumption Skipping meal Large portion size Vitamin D deficiency Low physical activity Sedentary behavior Irregular sleep Smoking and alcohol intake |
Depression Anxiety Mood disorder Irritability Emotional eating |
BMR: Basal Metabolic rate, PCOS: Polycystic ovary syndrome, SSB: Sugar-sweetened beverages
Physiological factors
Chronological aging is a competing risk factor for weight gain in middle-aged women. On an average, a weight gain of half kilogram per year is generally observed in this group.[12] Moreover, weight gain coexists with a decline in lean mass. The proportion of lean mass is positively associated with BMR, a component of energy expenditure. Slow metabolic rate in menopausal women decreases their capacity to effectively burn calories promoting a positive calorie balance.[13] Other physiological causes such as hypothyroidism, polycystic ovary syndrome, and musculoskeletal disorders can act as primary reasons for weight gain in menopausal women.
Psychological factors
Menopausal women report a high prevalence of negative emotional state (depression, stress, anxiety, tension, and mood disorder), sleep disturbances, and sexual problems during the period of transition.[14] Psychological distress commonly stems from body image issues. Women presenting with issues related to either body image and/or psychology report more episodes of emotional eating to combat distress.[15] Emotional eating or overeating is strongly associated with weight gain, as well as difficulties in self-regulation during weight loss attempts.[16]
Lifestyle related factors
Positive energy balance and poor quality of the diet are drivers of weight gain in middle-aged women. A “westernised” diet pattern, including HFSS (high fat, sugar, and salt) products and low dietary fiber intake is positively associated with weight gain during the menopausal transition.[17] Higher consumption of processed, fried, or convenience food due to its easy availability is also identified as a prime reason for higher body mass index (BMI).[18]
The higher preference for convenience food is also inversely proportional to time spent in home-cooked meals by these women. The lack of home-cooked meals impacts meal regularity, promoting the intake of large and/or energy-dense portions. The unhealthy eating behavior coupled with physical inactivity, irregular sleep patterns, smoking cessation, and excessive alcohol consumption leads to weight gain in this group of women.
A progressive reduction in physical activity is observed with aging, especially in females. The preference for sedentary behavior in middle-aged women might be due to diminished muscle strength that limits their functional ability to perform daily activities.[19] The limited-time spent in daily chores and physical activity is compensated by involvement in sedentary behaviors such as watching television, reading, and talking. More than half (64.7%) of Indian women follow this sedentary lifestyle.[18] Besides, these women rarely adjust their caloric intake according to decreased daily activity, making them gain weight.
The complex interplay of various determinants and associated symptoms enhances the risk of noncommunicable comorbidities, functional disability, and distress in menopausal women impacting the quality of their life.
OBESITY IN MENOPAUSE AND ITS IMPLICATIONS
Overweight and obese menopausal women are at a greater risk of associated metabolic and cardiovascular complications, osteoporosis, and cancers.[20] The risk of metabolic complications is compounded by abdominal fat distribution. Intra-abdominal fat around the viscera acts as metabolically active tissue, producing inflammatory markers (e.g., interleukin [IL]-1, IL-6, leptin, and tumor necrosis factor-α) which regulate the metabolic function.[21] Besides, studies suggest that higher abdominal fat is positively correlated with hypertension, insulin resistance, and pro-atherogenic lipid profile, which are well-established risk factors for cardiovascular diseases.[22]
Majority of women during menopause also complain about bone-related issues such as joint and back pain, knee-related issues, osteoporosis, and fractures. In most of these cases, the degenerative changes in the bone are driven by a marked decrease in circulating estrogen levels. The depletion in the levels of estrogen enhances bone resorption without a corresponding rise in bone deposition rate.[23] The amount of bone resorbed is greater than the amount of bone deposited, leading to a net bone loss, presenting as low bone density and quality. The reduction in bone strength predisposes menopausal women to bone-related issues, especially osteoporosis, exposing them to a high risk of fractures.[24]
At later, premenopausal stage, higher BMI is an independent risk factor for breast, endometrium, and uterine cancers. Obese menopausal women have a long-standing exposure to estrogen due to its continuous production by adipose tissues. The unopposed exposure to estrogen is responsible for high cancer risk in these women.[25] Higher adiposity also poses as an independent risk factor for systemic complications such as chronic kidney failure, chronic liver disease, obstructive sleep apnea, pulmonary distress, and sexual dysfunction than their healthy counterparts.[21]
The harmful effect of obesity at midlife goes beyond body image issues, impacting the overall health of these women. Successful management of obesity is known to help in the management of obesity and its related complications, promoting healthy aging.
CHALLENGES IN THE MANAGEMENT OF MENOPAUSAL OBESITY
The management of obesity in menopausal women is a great challenge. Current weight management interventions result in modest weight loss outcomes, which are poorly sustained in the long term. This can be attributed to a number of barriers that undermine the efficacy of weight-loss strategies producing insignificant weight loss. Some of these factors include specific physiological state, underlying metabolic condition or psychological distress, behavioral issues (low self-esteem, low self-efficacy), obesogenic environment, and lack of social support.[26] Most of these barriers are commonly present at menopausal stage making weight management even more challenging.
Menopausal women encounter more barriers during weight loss attempts than the general adult population. These challenges are specific to their physiological stage. The menopausal stage favors adiposity and might coexist with a number of metabolic comorbidities, functional disability, and body image issues. The presence of menopausal symptoms may also impede successful compliance with weight loss advice. Failure to lose and maintain weight enhances psychological distress, which acts as cues for unhealthy eating behavior and noncompliance to the given weight loss regime favoring further weight gain.
Weight gain has a bidirectional relationship with vasomotor symptoms, metabolic, and functional comorbidities. The clustering of a number of complications might affect the healthy aging and quality of life of these women. These complications can primarily be addressed by successful management of obesity in menopausal women. A comprehensive weight management module addressing women-centric barriers should be devised for achievement of successful weight loss outcomes.
MANAGEMENT OF OBESITY
The management of obesity is a stepwise intensification of pharmacological and nonpharmacological approaches. Grade I obesity is managed by nonpharmacological approaches such as the introduction of a low-calorie diet and increased physical activity. Pharmacological therapy is recommended for patients unable to achieve weight loss goals through these measures. The indications for grade II and grade III obesity include a combination of patient-specific pharmacological and surgical recommendations.[27] These recommendations have to be patient-specific considering the physiology, stage of transition, symptom severity, and the presence of metabolic complications. The weight management advice specific to perimenopausal women is given below:
Dietary recommendations
Dietary management is based on the introduction of caloric deficit while improving the overall quality of diet. A calorie deficit is achieved by reducing 500–750 kcal from current caloric intake taking due account of caloric expenditure, baseline BMI, and the presence of associated comorbidities.[28] In general, an intake of 1200–1000 kcal is suggested in clinical practice. The proportion of protein (20%–25%), fat (<30%), and carbohydrates (40%–50%) with respect to total calories is calculated accordingly.[29] The recommended diet should be high in fiber as the antioxidants, especially from fruits and vegetables decrease the oxidative stress that affects the number and quality of ovarian follicles.[30] Women should have daily intake of at least 2 litres of water. Limitations on salt, sugar, and processed foods should be observed. These women should incorporate corrective eating behavior such as 5–6 small and frequent meals, limited portion size, balanced meals, healthy snacking, and control over emotional eating episodes.[31] Some specific suggestions for menopausal women are as follows:
Incorporate foods rich in calcium such as milk and milk products, nuts and seeds, beans, green leafy vegetables for the maintenance of bone health. The intake of red meat, carbonated beverages, and certain foods high in phytates should be avoided as it hinders calcium absorption.
Iron-rich food (whole cereal and pulses, lean meat, egg, spinach, nuts, and seeds) for heavy menstrual bleeding and magnesium (green leafy vegetables, nuts and seeds, legumes) should be consumed for relieving menopausal symptoms such as hot flushes, insomnia, palpitations, and irritability.
Food rich in phytoestrogen, especially soybean, helps in alleviating menopausal symptoms and promotes musculoskeletal and bone health.
Both peri and postmenopausal women are vulnerable to Vitamin D deficiency. Proper screening and supplementation should be provided.
Spicy food, alcohol, and caffeine should be avoided for relief from hot flashes.
The studies have shown inconsistent results on the effectiveness of incorporating soy products, calcium supplementation, and lifelong fish consumption in relieving menopausal symptoms.[32]
Recommendations for physical activity
Physical activity helps to achieve negative calorie balance and relieves vasomotor symptoms. Menopausal women are generally advised 150 min/week of moderate-intensity physical activity such as aerobic exercise (walking, jogging, swimming, and cycling) coupled with household activities. The incorporation of resistance training exercises (2–3 times/week) helps to maintain bone and muscle mass. A combination of aerobics, resistance training, and balance exercises is the most effective in managing weight, vasomotor symptom severity, and psychological distress in these women.[33] Walking and aerobics have protective effect on vasomotor symptoms. Practicing yoga helps to relieve hot flashes and improves the quality of sleep in menopausal women.[34]
The physical activity regime has to be progressive and individualized according to patient's needs. Steps to a progressive activity regime incorporating recommended activities for menopausal women are given below:
Step I
Aging makes the body less flexible. Start with warm-up exercises such as full body stretches, walking for 10 min on the treadmill, suryanamaskar, etc. Warming up helps to prepare the body for exercise by gradually increasing physical activity, joint mobility, and stretching.
Step II
Aerobic exercises help to burn calories and provide cardiometabolic benefits to older women. Aerobic exercise can be initiated by walking for a short duration at a comfortable pace. A progressive increase in aerobic exercises by incorporating dancing, cycling, jogging, running, and swimming can be done as the regime progresses.
Step III
Short bouts of resistance exercise and strength training can also be incorporated using resistance bands, weight resistance, or utilizing one's own body weight. It is recommended that these exercises can be incorporated on every alternate day focusing on the abdomen, arms, legs, shoulders, and hips.[35] These exercises help to maintain muscle mass and bone density in menopausal women.
Step IV
Practicing yoga and stretches help to maintain flexibility in older age women to perform daily chores. These light intensity exercise do not spike the vasomotor symptoms and help to ease the psychological symptoms.[36]
Step V
Balance exercises help in postural and gait control to prevent falls in menopausal women. Practices such as tai chi, pilates, and some functional exercises Can help to maintain balance[37]
Step VI
The exercise session should conclude with cooling down exercises such as walking a few minutes and muscle relaxing postures and stretches which will ease the pain.
Regular exercise has both short-term and long-term benefits in menopausal women. Short term benefits include the management of menopausal symptoms, psychological distress, weight issues, immobility, and injuries.[35] Long-term physical activity helps in improvement of chronic disorders such as mood disorders, dementia, chronic pain, diabetes, strokes, and cardiovascular episodes reducing mortality and enhancing overall quality of life.[38,39]
Behavioral therapy
Behavioral therapy is a set of strategies, which includes goal setting, problem-solving, emotional eating, stimulus control, and relapse prevention.[40] These strategies aim to improve patient's compliance with the recommended dietary and exercise regimens. The compliance to lifestyle modification advice by menopausal women is influenced by the associated psychological distress. Psychological issues induce unhealthy behaviors and reduce self-regulation during weight loss attempts, which can be better addressed by progressive sessions based on behavioral strategies.
It is imperative to initiate the sessions after assessing the patient's readiness to change their existing dietary and activity behavior and set patient-specific weight loss targets. An initial understanding of woman's knowledge, attitude, and practices regarding obesity can also help in recommending patient-specific advice.[41] Second, the identification of primary behaviors associated with weight gain should be done prior to counseling about the required behavioral modification techniques. This helps to modify, incorporate, and sustain behaviors that would lead to weight loss. For example, a sedentary patient can be advised to complete “10,000 steps per day,” “walking for 30–40 min to and from work or for household chores,” etc. Finally, the patient has to be advised self-monitoring techniques such as to maintain dietary and activity logs to assess the compliance and its associated facilitators and barriers. Patient's compliance can also be assessed with the help of questionnaire, which can highlight the barriers that limits adherence to the given dietary and activity advice.[42] The barriers and facilitators can be addressed in the following sessions for sustenance of positive behaviors to produce clinically significant weight loss.[43]
Pharmacological management
Hormone replacement therapy (HRT) is the administration of estradiol with progesterone to supplement for estrogen deficiency at menopause.[44] The prescription of HRT is an effective strategy for overall management of vasomotor symptoms, bone health, and cognitive functioning, especially at postmenopausal stage.[45] There is contradicting literature on the effect of HRT on the weight status, with studies supporting and refuting its role in weight loss. A number of studies have highlighted the role of HRT in the reduction of abdominal obesity, insulin resistance, and associated cardiovascular risk.[46] The effectiveness of HRT depends on a number of factors such as estrogen dose, combination with progesterone, duration, time of initiation, and route of administration.[47] The discussion regarding the role of HRT on the body fat accumulation and distribution and its role in metabolic risk prevention requires more research and its discussion is beyond the scope of this review.
Table 2 depicts the weight management module for menopausal women. The module consists of pharmacological and nonpharmacological components of obesity management, customized for menopausal women. These components address eating and activity behavior and underlying psychological factors specific for the achievement of desirable weight loss outcomes. This weight management module can be used by obstetricians and gynecologists in their regular clinical practice for an effective management of patients presenting with menopausal obesity.
Table 2.
Women centric weight management module
| Women centric weight management module |
|---|
| Step I: Assessment |
| Clinical and lifestyle history: Elicit clinical history of risk factors of obesity and its related comorbidities, psychological distress, and severity of menopausal symptoms. Lifestyle-related factors leading to weight gain should be highlighted |
| Anthropometric measurement: Height, weight, body mass index, waist circumference, and bioelectric impedance (if available) should be measured |
| Biochemical assessment: Biological factors such as lipid profile, HbA1c, kidney function test, liver function test, blood pressure, thyroid-stimulating hormone and fasting blood glucose. Further laboratory test can be initiated for patient-specific indications |
| Dietary and physical activity assessment: Assess current caloric intake and overall physical activity status |
| Step II: Prescription: Medical, dietary, and activity advice |
| Medical prescription: Prescribe the required medication on indication of metabolic or adverse menopausal symptoms |
| HRT is recommended in adverse menopausal symptoms |
| Low-dose HRT - 0.3 mg CEE/1 mg estradiol and MPA 1.5 mg |
| Nonoral route - Patches, gel, vaginal cream, and implants or tibolone |
| Dietary advice |
| Balanced hypocaloric diet (deficit 500 kcal), rich in Fe, Ca, and phytoestrogen |
| Incorporate 5 servings of fruits and vegetables and high fiber (nuts, oilseeds, whole cereal, and pulses) |
| Small and frequent meals with optimum portion size |
| Limit processed foods rich in fat (saturated and cholesterol) food, sugar, and salt intake |
| Physical activity |
| Activity plan of 150 min/week as a combination of aerobics, strength training, balance, and flexibility should be planned |
| Advice to maintain overall active status: Walk-in office, take stairs, commute via public transport, walk the dog, etc. |
| Behavioral advice |
| Use strategies like self-monitoring (food and activity log), goal setting (5%-10% weight loss), eating behavior (EatWell Plate, Food label reading), problem solving (discuss maladaptive eating behavior) and stimulus control (use distraction to avoid excessive eating) |
| Some menopausal symptoms such as hot flashes, mood swings, insomnia and irritability can be managed by lifestyle modification techniques. The incorporation of these advices also helps to maintain heart and bone health |
| Step III: Follow-up |
| Essential to re-enforce advices, track progress, and manage challenges in weight loss process |
MPA: Medroxyprogesterone acetate, CEE: Conjugate equine estrogen, HRT: Hormone replacement therapy, HbA1c: Hemoglobin A1c
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Koo S, Ahn Y, Lim JY, Cho J, Park HY. Obesity associates with vasomotor symptoms in postmenopause but with physical symptoms in perimenopause: A cross-sectional study. BMC Womens Health. 2017;17:126. doi: 10.1186/s12905-017-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu D, Chung HF, Pandeya N, Dobson AJ, Kuh D, Crawford SL, et al. Body mass index and age at natural menopause: An international pooled analysis of 11 prospective studies. Eur J Epidemiol. 2018;33:699–710. doi: 10.1007/s10654-018-0367-y. [DOI] [PubMed] [Google Scholar]
- 3.National Family Health Survey NFHS-4, 2015-2016. Mumbai, India: International Institute for Population Sciences; 2017. International Institute for Population Sciences-IIPS/India and ICF. [Google Scholar]
- 4.Population Projections for India and States 2001-2026. New Delhi: Government of India; 2006. Office of the Registrar General and Census Commissioner. [Google Scholar]
- 5.Rathnayake N, Lenora J, Alwis G, Lekamwasam S. Prevalence and severity of menopausal symptoms and the quality of life in middle-aged women: A study from Sri Lanka. Nurs Res Pract. 2019;2019:1–9. doi: 10.1155/2019/2081507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mauvais-Jarvis F, Clegg DJ, Hevener AL. The role of estrogens in control of energy balance and glucose homeostasis. Endocr Rev. 2013;34:309–38. doi: 10.1210/er.2012-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kozakowski J, Gietka-Czernel M, Leszczyńska D, Majos A. Obesity in menopause – Our negligence or an unfortunate inevitability? Prz Menopauzalny. 2017;16:61–5. doi: 10.5114/pm.2017.68594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lumsden MA, Hor K. Impact of obesity on the health of women in midlife. Obstet Gynaecol. 2015;17:201–8. [Google Scholar]
- 9.Lizcano F, Guzmán G. Estrogen deficiency and the origin of obesity during menopause. Biomed Res Int. 2014;2014:757461. doi: 10.1155/2014/757461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jung SY, Vitolins MZ, Fenton J, Frazier-Wood AC, Hursting SD, Chang S. Risk profiles for weight gain among postmenopausal women: A classification and regression tree analysis approach. PLoS One. 2015;10:e0121430. doi: 10.1371/journal.pone.0121430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vivian-Taylor J, Hickey M. Menopause and depression: Is there a link? Maturitas. 2014;79:142–6. doi: 10.1016/j.maturitas.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Davis SR, Castelo-Branco C, Chedraui P, Lumsden MA, Nappi RE, Shah D, et al. Understanding weight gain at menopause. Climacteric. 2012;15:419–29. doi: 10.3109/13697137.2012.707385. [DOI] [PubMed] [Google Scholar]
- 13.Kapoor E, Collazo-Clavell ML, Faubion SS. Weight gain in women at midlife: A concise review of the pathophysiology and strategies for management. Mayo Clin Proc. 2017;92:1552–8. doi: 10.1016/j.mayocp.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Prairie BA, Wisniewski SR, Luther J, Hess R, Thurston RC, Wisner KL, et al. Symptoms of depressed mood, disturbed sleep, and sexual problems in midlife women: Cross-sectional data from the study of women's health across the nation. J Womens Health (Larchmt) 2015;24:119–26. doi: 10.1089/jwh.2014.4798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pimenta F, Maroco J, Ramos C, Leal I. Predictors of weight variation and weight gain in peri – And post-menopausal women. J Health Psychol. 2014;19:993–1002. doi: 10.1177/1359105313483153. [DOI] [PubMed] [Google Scholar]
- 16.Frayn M, Livshits S, Knäuper B. Emotional eating and weight regulation: A qualitative study of compensatory behaviors and concerns. J Eat Disord. 2018;6:23. doi: 10.1186/s40337-018-0210-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ventura Dde A, Fonseca Vde M, Ramos EG, Marinheiro LP, Souza RA, Chaves CR, et al. Association between quality of the diet and cardiometabolic risk factors in postmenopausal women. Nutr J. 2014;13:121. doi: 10.1186/1475-2891-13-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagarkar AM, Kulkarni SS. Obesity and its effects on health in middle-aged women from slums of Pune. J Midlife Health. 2018;9:79–84. doi: 10.4103/jmh.JMH_8_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bondarev D, Laakkonen EK, Finni T, Kokko K, Kujala UM, Aukee P, et al. Physical performance in relation to menopause status and physical activity. Menopause. 2018;25:1432–41. doi: 10.1097/GME.0000000000001137. [DOI] [PubMed] [Google Scholar]
- 20.Patni R, Mahajan A. The metabolic syndrome and menopause. J Life Health. 2018;9:111. doi: 10.4103/0976-7800.241951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atapattu P. Obesity at menopause: An expanding problem. J Pat Care. 2015;1:2–7. [Google Scholar]
- 22.Sen P, Das S, Hore S, Bhattacharjee S, Choudhuri D. Obesity and associated cardiometabolic risk among women from Tripura – A Northeastern state of India. J Midlife Health. 2017;8:110–7. doi: 10.4103/jmh.JMH_116_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sornay-Rendu E, Boutroy S, Vilayphiou N, Claustrat B, Chapurlat RD. In obese postmenopausal women, bone microarchitecture and strength are not commensurate to greater body weight: the Os des Femmes de Lyon (OFELY) study. J Bone Miner Res. 2013;28:1679–87. doi: 10.1002/jbmr.1880. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan SD, Lehman A, Nathan NK, Thomson CA, Howard BV. Age of menopause and fracture risk in postmenopausal women randomized to calcium + Vitamin D, hormone therapy, or the combination: Results from the Women's Health Initiative Clinical Trials. Menopause. 2017;24:371–8. doi: 10.1097/GME.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Key TJ, Appleby PN, Reeves GK, Roddam A, Dorgan JF, Longcope C, et al. Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. J Natl Cancer Inst. 2003;95:1218–26. doi: 10.1093/jnci/djg022. [DOI] [PubMed] [Google Scholar]
- 26.Sharifi N, Mahdavi R, Ebrahimi-Mameghani M. Perceived barriers to weight loss programs for overweight or obese women. Health Promot Perspect. 2013;3:11–22. doi: 10.5681/hpp.2013.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:254–66. doi: 10.1056/NEJMra1514009. [DOI] [PubMed] [Google Scholar]
- 28.Ard JD, Miller G, Kahan S. Nutrition Interventions for Obesity. Med Clin North Am. 2016;100:1341–56. doi: 10.1016/j.mcna.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 29.Dwyer JT, Melanson KJ, Sriprachy-anunt U, Cross P, Wilson M. Dietary treatment of obesity. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc; 2000. [Last accessed on 2019 Nov 02]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK278991/ [Google Scholar]
- 30.Wang S, He G, Chen M, Zuo T, Xu W, Liu X. The role of antioxidant enzymes in the ovaries. Oxid Med Cell Longev. 2017;2017:2–7. doi: 10.1155/2017/4371714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smethers AD, Rolls BJ. Dietary management of obesity: Cornerstones of healthy eating patterns. Med Clin North Am. 2018;102:107–24. doi: 10.1016/j.mcna.2017.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kroenke CH, Caan BJ, Stefanick ML, Anderson G, Brzyski R, Johnson KC, et al. Effects of a dietary intervention and weight change on vasomotor symptoms in the Women's Health Initiative. Menopause. 2012;19:980–8. doi: 10.1097/gme.0b013e31824f606e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Misra A, Nigam P, Hills AP, Chadha DS, Sharma V, Deepak KK, et al. Consensus physical activity guidelines for Asian Indians. Diabetes Technol Ther. 2012;14:83–98. doi: 10.1089/dia.2011.0111. [DOI] [PubMed] [Google Scholar]
- 34.Joshi S, Vaze N. Yoga and menopausal transition. J Life Health. 2010;1:56–8. doi: 10.4103/0976-7800.76212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grindler NM, Santoro NF. Menopause and exercise. Menopause. 2015;22:1351–8. doi: 10.1097/GME.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 36.Daley AJ, Stokes-Lampard HJ, Macarthur C. Exercise to reduce vasomotor and other menopausal symptoms: A review. Maturitas. 2009;63:176–80. doi: 10.1016/j.maturitas.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Mishra N, Devanshi, Mishra V. Exercise beyond menopause: Dos and don′ts. J Life Health. 2011;2:51–6. doi: 10.4103/0976-7800.92524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Swift DL, Johannsen NM, Tudor-Locke C, Earnest CP, Johnson WD, Blair SN, et al. Exercise training and habitual physical activity: A randomized controlled trial. Am J Prev Med. 2012;43:629–35. doi: 10.1016/j.amepre.2012.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–45. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 40.Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am. 2011;34:841–59. doi: 10.1016/j.psc.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reethesh SR, Ranjan P, Arora C, Kaloiya GS, Vikram NK, Dwivedi SN, et al. Development and validation of a questionnaire assessing knowledge, attitude, and practices about obesity among obese individuals. Indian J Endocrinol Metab. 2019;23:102–10. doi: 10.4103/ijem.IJEM_487_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dubasi SK, Ranjan P, Arora C, Vikram NK, Dwivedi SN, Singh N, et al. Questionnaire to assess adherence to diet and exercise advices for weight management in lifestyle-related diseases. J Family Med Prim Care. 2019;8:689–94. doi: 10.4103/jfmpc.jfmpc_338_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: A systematic review of the literature. J Am Diet Assoc. 2011;111:92–102. doi: 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bakour SH, Williamson J. Latest evidence on using hormone replacement therapy in the menopause. Obstet Gynaecol. 2015;17:20–8. [Google Scholar]
- 45.The NAMS 2017 Hormone Therapy Position Statement Advisory Panel. The 2017 hormone therapy position statement of the North American Menopause Society. Menopause. 2017;24:728–53. doi: 10.1097/GME.0000000000000921. [DOI] [PubMed] [Google Scholar]
- 46.Sites CK, L'Hommedieu GD, Toth MJ, Brochu M, Cooper BC, Fairhurst PA. The effect of hormone replacement therapy on body composition, body fat distribution, and insulin sensitivity in menopausal women: A randomized, double-blind, placebo-controlled trial. J Clin Endocrinol Metab. 2005;90:2701–7. doi: 10.1210/jc.2004-1479. [DOI] [PubMed] [Google Scholar]
- 47.El Khoudary SR, Zhao Q, Venugopal V, Manson JE, Brooks MM, Santoro N, et al. Effects of hormone therapy on heart fat and coronary artery calcification progression: secondary analysis from The KEEPS trial. [Last accessed on 2019 Nov 02];J Am Heart Assoc. 2009 8:e012763. doi: 10.1161/JAHA.119.012763. Available from: https://www.ahajournals.org/doi/10.1161/JAHA.119.012763 . [DOI] [PMC free article] [PubMed] [Google Scholar]


