Abstract.
Imported malaria in Anhui Province, China, remains a significant public health issue with frequent reporting of severe and fatal cases, partly because of globalization and increased international communication. A retrospective evaluation using surveillance data from 2012 to 2018 was conducted to draw lessons on diagnosis of imported malaria. Epidemiological characteristics, together with diagnostic information, were analyzed using descriptive and comparative statistics. Simultaneously, blinded rechecking of malaria blood slides was performed at general hospitals in Anhui Province in 2018. The results showed that, in their first medical visits, 238 (28.2%) of 844 imported cases were not correctly diagnosed. Notably, the proportion of patients who were misdiagnosed at the first clinic visit was 104/120 (86.7%) at private and village clinics, and 41/81 (50.6%) at primary hospitals. The species identification rates for Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, and Plasmodium malariae were 85.2%, 66.7%, 23.2%, and 32.3% (χ2 = 224, P < 0.001), respectively. Nearly 7% of cases lacked laboratory evidence and were classified as presumed cases. Our findings suggest that physicians and health care providers, especially those at the primary level, lacked the awareness of diagnosing imported malaria. The training of physicians in malaria diagnosis needs to be enhanced. In addition, polymerase chain reactions (previously only carried out at the provincial level) should be performed at municipal CDC for rapid species identification, thereby guiding clinical treatment.
INTRODUCTION
Malaria remains a major global public health problem. At the beginning of 2016, 91 countries and territories reported indigenous malaria cases.1 In 2017, there was an estimate of 219 million cases and 435,000 deaths due to malaria worldwide.2 In China, the National Malaria Elimination Action Plan (2010–2020) was launched in 2010, with the objective of eliminating indigenous malaria in non-border regions before the end of 2015.3,4 At its early stage, 1,803 indigenous Plasmodium vivax cases were reported in Anhui Province.5 The local transmission of malaria in Anhui is prevented owing to the introduction of the “1-3-7 model” to deliver and monitor the elimination process. This model involved three steps, namely, the case reporting within 24 hours, the case verification and investigation within 3 days, and the foci investigation and response to inhibit the secondary transmission within 7 days.6 The number of indigenous cases declined rapidly, from 530 cases in 2011 to 32 cases in 2012 and to only four cases in 2013. Besides, no autochthonous cases have been reported since 2014. Nevertheless, with globalization and increased international movement, imported malaria has become a challenge for the province. Severe and fatal cases were frequently reported because of diagnosis delay.7 To identify reasons for delayed diagnosis of imported malaria in Anhui Province, we conducted a retrospective evaluation using surveillance data from 2012 to 2018 (the accurate species identification for each imported case has been made available since 2012 when Anhui Provincial Malaria Diagnosis Reference Laboratory was formally established) and blinded rechecking of malaria blood slides in general hospitals in 2018. The study may come up with suggestions for implementing activities that help improve the capacity for imported malaria diagnosis.
METHODS
Definition of an imported malaria case.
An imported malaria case was defined as a case whose infection was acquired outside the country in which it is diagnosed.8 Plasmodium malariae and Plasmodium ovale are not endemic, and endemic Plasmodium falciparum malaria was successfully eliminated in 1991 in Anhui Province. An individual was determined to be an imported case if he or she was confirmed to carry one of these three malaria parasites and to have lived in an epidemic area outside China. For P. vivax, the procedure for determining an imported case was more complicated. Plasmodium vivax has a dormant hypnozoite stage that can cause multiple relapses after the primary infection, and its relapse periods vary. Therefore, we collected epidemiological and laboratory data (molecular traceability) for all P. vivax cases. These data were then submitted to the technical experts of the National Malaria Elimination advisory committee. These experts reviewed the data and finally determined whether a case was indigenous or imported. In Anhui Province, the diagnosis of all patients was finally confirmed by microscopic examination of Giemsa-stained blood films and fluorescent polymerase chain reaction (PCR) in the Malaria Diagnostic Reference Laboratory of Anhui Province from 2012 to 2018. The epidemiological investigation report of each case was finalized by professionals from the CDC. The report included the onset of malaria, diagnosis, treatment, and the origin of the infection.
Data collection.
Malaria is a notifiable disease in China, and each case must be reported within 24 hours of diagnosis.9 The basic information of a malaria case, including date of birth, gender, occupation, usual residence, as well as details related to malaria, such as date of onset of symptoms and diagnosis, was collected from the China Information System for Disease Control and Prevention (CISDCP). Moreover, we obtained clinical and epidemiological data of each case from the Information System for Parasitic Disease Control and Prevention (ISPDCP)—a subsystem of the CISDCP. These data mainly included diagnostic results, complications, antimalarial use, outcome, source of infection, and preventive measures. When a case was reported, the basic information derived from CISDCP was automatically transferred to ISPDCP, and then further details were added by the CDC staff.
Blinded rechecking of malaria blood slides.
In total, 170 general hospitals in Anhui Province were selected to participate in the conduct of blinded rechecking for the detection of malaria parasites by optical microscopy. Specifically, each hospital randomly examined five blood slides, each of which was examined to detect malaria parasites (in case of positive blood slides, species identification was necessary). All test results were then uploaded to http://www.ahccl.org/labmain/ad/detailMeeting-Info.aspx?id=282. The external quality assessment (EQA) designed to examine the ability of malaria diagnosis at general hospitals in Anhui Province was jointly implemented by Anhui Provincial Center for Disease Control and Prevention and Anhui Provincial Center for Clinical Laboratories in 2018.
Data analysis.
Continuous variables with normal distribution were presented as mean (SD), whereas non-normally distributed variables were reported as median (interquartile range [IQR]). In addition, ratios and percentages were used to describe categorical data. Differences in medians of continuous variables were compared using the Kruskal–Wallis H test (multiple independent samples), and the Bonferroni-corrected post hoc test was conducted to adjust the observed significant level for multiple comparisons. Differences in proportions were tested by the chi-square (χ2) test or Fisher’s exact test. A two-sided P < 0.05 was considered statistically significant. All statistical tests were performed using SPSS version 22.0 (SPSS, Chicago, IL).
Ethical considerations.
This study used routine data collected from the CISDCP and the ISPDCP, and no additional ethical approval was required. Data were held anonymously to make sure that no specific patient was identified.
RESULTS
Epidemiological profile.
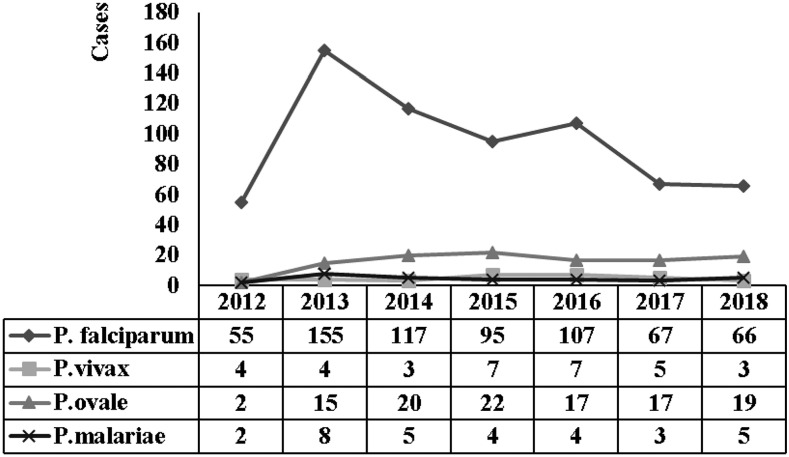
There were 844 cases of malaria reported in Anhui Province between 2012 and 2018. During the 7-year period, there was a general increase in malaria incidence, from 63 cases in 2012 to 95 cases in 2018, with some year-on-year fluctuations. Malaria incidence peaked at 183 cases in 2013 (Figure 1). The mean age of 844 patients was 40.8 ± 9.1 years (range: 16–72 years), and 829 patients (98.2%) were males. Most patients were overseas laborers (i.e., workers and waiters), accounting for 94.7% of all cases; imported cases came from 38 African and Asian countries, with Africa (831; 99.7%) being the most common region of origin. The top three countries of origin of infection were Angola (223; 26.4%), Equatorial Guinea (137; 16.2%), and Nigeria (106; 12.6%). Plasmodium falciparum was the most dominant species, accounting for 662 cases (78.4%). Of the remainder, there were 112 cases of P. ovale (13.3%), 33 cases of P. vivax (3.9%), 31 cases of P. malariae (3.7%), and six cases (0.7%) of mixed infection. The information on the duration of overseas stay was available in 842 cases (99.8%). In particular, 33 cases (3.9%) stayed for less than 30 days, 162 (19.2%) less than 180 days, 202 (24.0%) less than 365 days, and 445 (52.9%) more than 365 days. Fifty-three patients (6.3%) developed severe malaria (defined by the clinical features stated in “Diagnosis of malaria” and “Management of severe malaria”10,11), including four who died (case fatality rate: 0.5%). The epidemiological characteristics of the individuals with imported malaria are summarized in Table 1.
Figure 1.
Annual number of imported malaria cases in Anhui Province from 2012 to 2018 according to the parasite species.
Table 1.
Epidemiological characteristics of individuals with imported malaria in Anhui Province from 2012 to 2018
| Epidemiological characteristics | Number | % |
|---|---|---|
| Gender | ||
| Male | 829 | 98.2 |
| Female | 15 | 1.8 |
| Country of acquisition | ||
| Angola | 223 | 26.4 |
| Equatorial Guinea | 137 | 16.2 |
| Nigeria | 106 | 12.6 |
| Other countries | 378 | 44.8 |
| Species | ||
| Plasmodium falciparum | 662 | 78.4 |
| Plasmodium ovale | 112 | 13.3 |
| Plasmodium vivax | 33 | 3.9 |
| Plasmodium malariae | 31 | 3.7 |
| Mixed infections | 6 | 0.7 |
| Time out of China (days)* | ||
| ≤ 30 | 33 | 3.9 |
| 31–180 | 162 | 19.2 |
| 181–365 | 202 | 24.0 |
| > 365 | 445 | 52.9 |
* Excluding two cases for which information on time outside the country was unavailable.
Patient situations from onset to diagnosis.
Temporal features.
The median interval between the date of arrival in China and the onset of malaria symptoms was 7 days (IQR 2–15 days), with 673 (79.7%) cases falling ill within 30 days after arrival. Of all cases, 703 (83.4%) sought medical assistance within three days; 492 (58.5%) were diagnosed with malaria within 1 day after medical visits, compared with 693 (82.1%) within 3 days. The median interval from symptom onset to the first medical visit was 1 day (IQR: 0–3 days), that from the first medical visit to diagnosis was 1 day (IQR: 1–3 days), and that from symptom onset to diagnosis was 3 days (IQR: 2–5 days). Differences in median time intervals of four malaria species were compared using the Kruskal–Wallis H test. The results showed statistical differences in the median time intervals from arrival in China to onset, from symptom onset to first medical visit, and from symptom onset to diagnosis. Post hoc multiple comparison tests were carried out to confirm the differences occurring between groups. The median time intervals from return to the country to symptom onset of P. vivax, P. ovale, and P. malariae were longer than that of P. falciparum, and the median time intervals (from onset to the first medical visit and from onset to diagnosis) of P. malariae were longer than those of P. falciparum. The temporal features of the imported malaria cases are summarized in Table 2.
Table 2.
Temporal features of the 844 malaria cases imported during 2012 to 2018
| Days from return to the onset, median (IQR) | H | P-value | Days from the onset to the first medical visit, median (IQR) | H | P-value | Days from the first medical visit to diagnosis, median (IQR) | H | P-value | Days from the onset to treatment, median (IQR) | H | P-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P. falciparum | 5 (1, 10) | 228.9 | < 0.01* | 1 (0, 2) | 8.8 | 0.032* | 1 (1, 2) | 3.643 | 0.30* | 3 (2, 5) | 19.7 | < 0.01* |
| P. vivax | 26 (6, 99.5) | – | – | 1 (0, 3.5) | – | – | 2 (1, 4) | – | – | 4 (2, 7.5) | – | – |
| P. ovale | 62.5 (18, 182.5) | – | – | 1 (0, 3) | – | – | 1 (1, 3) | – | – | 4 (2, 7) | – | – |
| P. malariae | 22 (8, 43) | – | – | 3 (0, 9) | – | – | 1 (1, 3) | – | – | 6 (3, 11) | – | – |
| P. falciparum vs. P. vivax | – | −216.9 | < 0.01† | – | −26.8 | 1.00† | – | – | – | – | −56.3 | 0.13† |
| P. ovale | – | −228.0 | < 0.01† | – | −27.5 | 1.00† | – | – | – | – | −89.9 | 0.21† |
| P. malariae | – | −345.7 | < 0.01† | – | −120.4 | 0.032† | – | – | – | – | −155 | 0.003† |
IQR = interquartile range; P. = Plasmodium.
* Differences in medians were compared using the Kruskal–Wallis H test (multiple independent samples).
† The Bonferroni-corrected post hoc test was conducted to adjust the observed significant level for multiple comparisons.
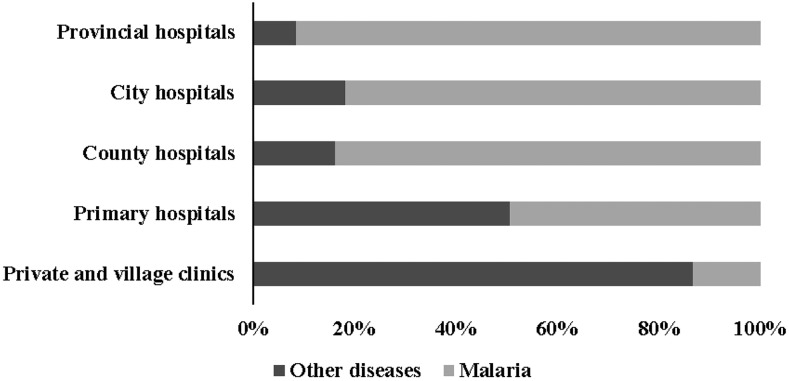
Initial medical visit rate and misdiagnosis rate, by health care facility.
At their first medical visits, 255 patients sought medical care at the county-level hospitals, accounting for the highest percentage of 30.2%, compared with 120 patients (14.2%) at private clinics or village clinics, 81 (9.6%) at primary hospitals, 166 (19.7%) at city-level hospitals, 215 (25.5%) at provincial-level hospitals, and seven (0.8%) at other health care facilities (e.g., overseas medical assistance teams and overseas hospitals). Of all 844 imported cases, 238 patients (28.2%) were incorrectly diagnosed in their first medical visits. Notably, the misdiagnosis rate in the first medical visits was up to 86.7% (104/120) at private clinics and village clinics, and 50.6% (41/81) at primary hospitals. Overall, the diagnosis was more accurate at higher level health care facilities (Figure 2).
Figure 2.
Diagnostic results in the first medical visits, by level of health care facility.
The diagnostic results of the case-reporting unit.
In China, malaria is a notifiable disease, and it is mandatory that each malaria case be reported within 24 hours of diagnosis. The diagnostic information of the cases at reporting units that made the final diagnosis and finished infectious disease report card was recorded and collected. Among the 844 cases, the parasite detection rates (calculated according to whether or not a parasite was detected) for P. falciparum, P. vivax, P. ovale, and P. malariae were 92.9%, 93.9%, 92.9%, and 93.6%, respectively. The remaining 59 patients (7.0%) who lacked laboratory evidence were classified as suspected cases at the case-reporting unit. These suspected cases were eventually confirmed with malaria infection in the Malaria Diagnostic Reference Laboratory of Anhui Province. The species identification rates for P. falciparum, P. vivax, P. ovale, and P. malariae were 85.2%, 66.7%, 23.2%, and 32.3% (χ2 = 224, P < 0.000), respectively. Besides, 29.5% (33/112) of P. ovale cases and 41.9% (13/31) of P. malariae cases were misdiagnosed as P. vivax cases. The diagnostic results of the case-reporting unit are shown in the Supplemental Appendix 1.
Blinded rechecking of malaria blood slides.
One hundred seventy general hospitals participated in the EQA. The overall parasite detection rate at 170 hospitals was 90.9% (773/850), and the species identification rates for P. falciparum, P. vivax, P. ovale, and P. malariae were 60.9%, 53.5%, 53.5%, and 63.5%, respectively. The detailed results of blinded rechecking are presented in (Table 3).
Table 3.
Results of blinded rechecking of malaria blood slides in Anhui Province in 2018
| Correct number | Parasite detection* | Species identification† | ||
|---|---|---|---|---|
| N‡ | % | N‡ | % | |
| 5 | 113 | 66.5 | 38 | 22.4 |
| 4 | 44 | 25.9 | 40 | 23.5 |
| 3 | 11 | 6.5 | 42 | 24.7 |
| 2 | 2 | 1.2 | 31 | 18.2 |
| 1 | 0 | 0 | 13 | 7.6 |
| 0 | 0 | 0 | 6 | 3.5 |
| Total | 170 | 100 | 170 | 100 |
* Parasite detection: calculated according to whether or not a parasite was detected.
† Species identification: calculated based on the number of correctly identified species.
‡ The number of hospitals.
DISCUSSION
Imported malaria remains a significant public health threat in China because of globalization and increased international communication. Specially, since the establishment of the Forum on China–Africa Cooperation in 2000, the number of exported laborers from China to Africa has been on a rise. This tendency is closely related to the increasing number of imported malaria cases.13,14 The pattern of imported malaria in Anhui Province resembles the national one. Among 844 imported malaria cases, 94.7% of patients were overseas laborers. Plasmodium falciparum, the predominant species, was found in 662 cases (78.4%), and it was most commonly associated with severe malaria and deaths. Therefore, prompt diagnosis and appropriate treatment of malaria cases are of vital importance.11
During the study period, severe and fatal cases were frequently reported in Anhui Province.5 Fifty-three patients (6.3%) developed severe malaria, including four cases that died during this period, leading to a case fatality rate of 0.5%. This rate was lower than the national figure and those of other high-income countries.15–18 Obviously, the prompt diagnosis of imported malaria still needs further improvement. In this study, we analyzed surveillance data in Anhui Province with the aim to draw lessons on the diagnosis of imported malaria. These lessons would then contribute to the implementation of activities for improving diagnostic capacity.
According to our results, there were four main findings in this study. First, imported malaria cases mostly included exported laborers, those with longer stays in China, and those engaged in outdoor occupations (e.g., construction and mining). Such jobs exposed them to a higher risk of contracting malaria. This population was generally poorly educated and lacked awareness of the risk of malaria; thus, they often failed to seek timely medical assistance.19 In this study, nearly 17% of all the 844 imported cases sought medical assistance after more than three days of symptom onset. Obviously, more attention should be paid to patient delay in seeking medical help. Second, most physicians and health care providers in Anhui Province, especially those working at private clinics and primary health care facilities, lacked the awareness of and skills in diagnosing imported malaria. Indeed, the diagnosis rates within one day and three days after the first medical visit were low (58.5% versus 82.1%, correspondingly), whereas the misdiagnosis rates in the first medical visits remained relatively high at private and village clinics (86.7%), as well as at primary hospitals (50.6%). All these evidences indicate that the awareness to diagnose imported malaria of physicians still needs further improvement. Third, the lack of laboratory evidence in nearly 7% of cases, which were first classified as clinical cases at the case-reporting unit and later confirmed with malaria at the Malaria Diagnostic Reference Laboratory of Anhui Province, may result from the sensitivity of detection methods. For example, microscopy, the traditional diagnostic method, has a limit of detection of about 50 parasites/μL of whole blood,20,21 and rapid diagnostic tests (RDTs) perform variably below 200 parasites/μL.22,23 Various factors might lead to negative results, for example, slide preparation techniques, the quality of essential laboratory supplies, condition of the microscope, workload, lack of training, and skills maintenance.24 Finally, according to our surveillance data, the species identification rates for P. falciparum, P. vivax, P. ovale, and P. malariae were 85.2%, 66.7%, 23.2%, and 32.3%, respectively (χ2 = 224, P < 0.000). These low rates had adverse impacts on treatment, depending on treatment protocols specific for different species.25 Blinded rechecking of malaria blood slides was conducted in 2018, and the results showed that the species identification rates for P. falciparum, P. vivax, P. ovale, and P. malariae were 60.9%, 53.5%, 53.5%, and 63.5%, respectively. The results were still at a low level. Interestingly, compared with the surveillance data, the species identification rate for P. falciparum decreased by nearly 25 percentage points, whereas the rates for P. ovale and P. malariae both experienced an increase of > 30% points. This difference was derived from two reasons. First, two RDTs with higher sensitivity in detecting P. falciparum and P. vivax, which were procured from two manufacturers (Pf/pan; Wondfo, Guangzhou Wondfo Biotech Co., Ltd., Guangzhou, China, and ACCESSBIO Access Bio, Inc., Somerset, NJ), have been used to provide parasite-based diagnosis in Anhui Province since 2013. However, they are insensitive for P. malariae and P. ovale (although there has been some improvement since 2018). Second, the laboratory technicians at the Anhui Provincial Malaria Diagnosis Reference Laboratory carefully prepared and provided the malaria blood slides of selected samples with typical morphology for blinded rechecking. Obviously, the high quality of blood slides facilitated species identification.
Our study has several limitations. First, it was a retrospective evaluation, and so recall bias is a major limitation. Second, treatment protocols were species specific, so to avoid medical disagreement, inspectors sometimes reported cases as “unclassified” if parasites were detected, but the species was not correctly identified. This is likely to have had an adverse impact on species identification and subsequent treatment. However, we did not evaluate this problem in our study. Last, we measured diagnostic delays in terms of days. The temporal features could be evaluated in greater depth if hours were used instead of days.
In conclusion, we conducted a retrospective evaluation to draw lessons on diagnosis of imported malaria using surveillance data from 2012 to 2018. Based on our findings, we provide certain recommendations to strengthening the malaria diagnosis capacity of hospitals as follows: 1) A more effective mechanism of multi-sectoral cooperation, between the CDC and customs, labor, and business departments, should be developed to better the management of imported cases and to provide more effective health education for target populations. Presently, new interventions are being piloted with departmental collaboration in Anhui Province. For example, to increase the number of patients seeking timely medical treatment, health tips on vaccination certificates were provided to people going overseas.7 2) Private clinics and village clinics should be advised not to deal with any suspected malaria cases but to forward them to proper health care facilities for diagnosis. 3) The training of local physicians in diagnosis of malaria cases should be enhanced. 4) PCR methods should be used in parasite detection because they have high sensitivity and specificity, as well as supreme advantages in species identification.26–28 Polymerase chain reaction detection should also be carried out at municipal CDCs (previously only at the provincial level) for the sake of rapid species identification, thereby guiding clinical treatment.
Supplemental appendix
Acknowledgments:
We thank staff members of the municipal and county Centers for Disease Control and Prevention for their contribution to data collection.
Note: Supplemental appendix appears at www.ajtmh.org.
REFERENCES
- 1.World Health Organization , 2016. World Malaria Report 2016. Geneva, Switzerland: WHO; Available at: https://apps.who.int/iris/bitstream/handle/10665/252038/97892415 11711-eng.pdf. Accessed June 24, 2019. [Google Scholar]
- 2.World Health Organization , 2018. World Malaria Report 2018. Geneva, Switzerland: WHO; Available at: https://apps.who.int/iris/bitstream/handle/10665/275867/9789241 565653-eng.pdf. Accessed June 24, 2019. [Google Scholar]
- 3.Ministry of Health of the People’s Republic of China , 2010. Action Plan of China Malaria Elimination (2010–2020). Beijing, China: Available at: http://www.moh.gov.cn/mohbgt/s10788//201005/47529.shtml.webcite. Accessed June 24, 2019. [Google Scholar]
- 4.Feng J, Zhang L, Huang F, Yin JH, Tu H, Xia ZG, Zhou SS, Xiao N, Zhou XN, 2018. Ready for malaria elimination: zero indigenous case reported in the People’s Republic of China. Malar J 17: 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu X, Li WD, Jiang JJ, Zhang T, Wang JJ, 2015. Analysis of malaria epidemic characteristics in Anhui province during 1999–2013. Chin J Parasitol Parasit Dis 33: 1–6. [PubMed] [Google Scholar]
- 6.Cao J, Sturrock HJ, Cotter C, Zhou S, Zhou H, Liu Y, Tang L, Gosling RD, Feachem RG, Gao Q, 2014. Communicating and monitoring surveillance and response activities for malaria elimination: China’s “1-3-7” strategy. PLoS Med 11: e1001642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang T, Xu X, Jiang J, Yu C, Tian C, Xie Q, Li W, 2019. Risk factors of severe imported malaria in Anhui province, China. Acta Trop 197: 104934. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization , 2016. WHO Malaria Terminology. Geneva, Switzerland: WHO; Available at: https://apps.who.int/iris/bitstream/handle/10665/208815/WHO_HTM_GMP_2016.6_eng.pdf. Accessed June 24, 2019. [Google Scholar]
- 9.Wang LD, Wang Y, Jin SG, Wu ZY, Chin DP, Koplan JP, Wilson ME, 2008. Emergence and control of infectious diseases in China. Lancet 372: 1598–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Health and Family Planning Commission of the People’s Republic of China , 2015. Diagnosis of Malaria (in Chinese). Available at: http://www.nhfpc.gov.cn/ewebeditor/uploadfile/2015/11/20151125105511210.pdf. Accessed June 24, 2019. [Google Scholar]
- 11.World Health Organization , 2012. Management of Severe Malaria. Geneva, Switzerland: WHO; Available at: https://apps.who.int/iris/bitstream/handle/10665/79317/9789241548 526_eng.pdf. Accessed June 24, 2019. [Google Scholar]
- 12.World Health Organization , 2016. Malaria Microscopy Quality Assurance Manual Version 2. Geneva, Switzerland: WHO; Available at: https://apps.who.int/iris/bitstream/hand le/10665/204266/9789241549394_eng.pdf. Accessed June 24, 2019. [Google Scholar]
- 13.Zhou S, Li Z, Cotter C, Zheng C, Zhang Q, Li H, Zhou S, Zhou X, Yu H, Yang W, 2016. Trends of imported malaria in China 2010–2014: analysis of surveillance data. Malar J 15: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y, Hsiang MS, Zhou H, Wang W, Cao Y, Gosling RD, Cao J, Gao Q, 2014. Malaria in overseas labourers returning to China: an analysis of imported malaria in Jiangsu province, 2001–2011. Malar J 13: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang L, Feng J, Zhang SS, Xia ZG, Zhou SS, 2018. The progress of national malaria elimination and epidemiological characteristics of malaria in China in 2017. Chin J Parasitol Parasit Dis 36: 201–209. [Google Scholar]
- 16.Li Z, et al. 2016. Epidemiologic features of overseas imported malaria in the People’s Republic of China. Malar J 15: 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newman RD, Parise ME, Barber AM, Steketee RW, 2004. Malaria-related deaths among U.S. travelers, 1963–2001. Ann Intern Med 141: 547–555. [DOI] [PubMed] [Google Scholar]
- 18.Seringe E, et al. French National Reference Center for Imported Malaria Study Group , 2011. Severe imported Plasmodium falciparum malaria, France, 1996–2003. Emerg Infect Dis 17: 807–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang M, Liu Z, He H, Luo L, Wang S, Bu H, Zhou X, 2011. Knowledge, attitudes, and practices on malaria prevention among Chinese international travelers. J Travel Med 18: 173–177. [DOI] [PubMed] [Google Scholar]
- 20.Kilian AH, Metzger WG, Mutschelknauss EJ, Kabagambe G, Langi P, Korte R, von Sonnenburg F, 2010. Reliability of malaria microscopy in epidemiological studies: results of quality control. Trop Med Int Health 5: 3–8. [DOI] [PubMed] [Google Scholar]
- 21.Mwingira F, Genton B, Kabanywanyi AN, Felger I, 2014. Comparison of detection methods to estimate asexual Plasmodium falciparum parasite prevalence and gametocyte carriage in a community survey in Tanzania. Malar J 13: 433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization , 2017. Results of WHO Product Testing of Malaria RDTs Round 7 (2015–2016). Geneva, Switzerland: WHO; Available at: https://apps.who.int/iris/bitstream/handle/10665/255836/9789241512688-eng.pdf. Accessed June 24, 2019. [Google Scholar]
- 23.World Health Organization , 2018. Results of WHO Product Testing of Malaria RDTs Round 8 (2016–2018). Geneva, Switzerland: WHO; Available at: https://apps.who.int/iris/bitstream/handle/10665/276190/9789241514965-eng.pdf. Accessed June 24, 2019. [Google Scholar]
- 24.Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH, 2007. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). Am J Trop Med Hyg 77 (Suppl 6): 119–127. [PubMed] [Google Scholar]
- 25.National Health and Family Planning Commission of the People’s Republic of China , 2016. Technical regulations for application of antimalarials (in Chinese). Available at: http://www.moh.gov.cn/ewebeditor/uploadfile/2016/05/201605301434293-28.pdf. Accessed June 24, 2019. [Google Scholar]
- 26.Wu L, van den Hoogen LL, Slater H, Walker PG, Ghani AC, Drakeley CJ, Okell LC, 2015. Comparison of diagnostics for the detection of asymptomatic Plasmodium falciparum infections to inform control and elimination strategies. Nature 528: S86–S93. [DOI] [PubMed] [Google Scholar]
- 27.Andrews L, et al. 2005. Quantitative real-time polymerase chain reaction for malaria diagnosis and its use in malaria vaccine clinical trials. Am J Trop Med Hyg 73: 191–198. [PubMed] [Google Scholar]
- 28.Rockett RJ, Tozer SJ, Peatey C, Bialasiewicz S, Whiley DM, Nissen MD, Trenholme K, Mc Carthy JS, Sloots TP, 2011. A real-time, quantitative PCR method using hydrolysis probes for the monitoring of Plasmodium falciparum load in experimentally infected human volunteers. Malar J 10: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.