Abstract
Background
Despite the increasingly recognized role of norovirus in global acute gastroenteritis (AGE), specific estimates of the associated disease burden remain sparse, primarily due to limited availability of sensitive norovirus diagnostics in the clinical setting. We sought to estimate the incidence of norovirus-associated hospitalizations by age group in Taiwan using a previously developed indirect regression method.
Methods
AGE-related hospitalizations in Taiwan were identified using ICD-9-CM codes abstracted from a national database; population data were provided from the Department of Household Registration Affairs. Population and hospitalizations were aggregated by month and year (July 2003 – June 2013) and grouped by age: under 5 years, 5 – 19 years, 20 – 64 years, 65 years and older. Monthly counts of cause-unspecified AGE hospitalizations were modeled as a function of counts of known causes, and the residuals were then analyzed to estimate norovirus-associated hospitalizations.
Results
Over the study period, an annual mean of 101,400 gastroenteritis-associated hospitalizations occurred in Taiwan (44 per 10,000 person-years), most of which (83%) had no specified cause. The overall estimated rate of norovirus-associated hospitalizations was 6.7 per 10,000 person-years, with the highest rates in children aged < 5 years (63.7 / 10,000 person-years). Predicted norovirus peaked in 2006/2007 and 2012/2013.
Conclusions
Our study is one of the first to generate a population-based estimate of severe norovirus disease incidence in Asia, and highlights the large burden of norovirus in Taiwan, particularly in children. Predicted peak norovirus seasons coincided with the emergence of new strains and resulting pandemics, supporting the validity of the estimates.
Keywords: Norovirus, Acute gastroenteritis
SUMMARY
We estimated that norovirus is associated with 15,500 hospitalizations annually in Taiwan, with children <5 years bearing a disproportionately large burden: 6,800 annual norovirus hospitalizations, or 64 per 10,000 person-years (vs. 2.1 / 10,000 person-years in adults 20 – 64 years).
Background
Norovirus is a leading cause of acute gastroenteritis (AGE) globally, estimated to cause nearly 20% of all acute gastroenteritis cases worldwide [1]. Disease occurs across the age spectrum, and while self-limiting illnesses are most common, outcomes can range up to hospitalization (estimated rates of 1 – 7.0 per 10,000 person-years) and even death (estimated rates of 0.02 – 0.4 per 10,000 person-years) [2–6]; while the rates of severe outcomes by vary by country and setting, norovirus causes significant economic impact globally [7].
Despite the increasingly recognized role of norovirus in global AGE, data on the associated disease burden has been historically limited by the lack of availability and use of sensitive norovirus diagnostics in the clinical setting. Population-based incidence estimates remain sparse, particularly outside of the U.S. and Europe, and especially in Asia. In one study from Hong Kong, the incidence of norovirus hospitalization was high in children (147.5 per 10,000 person-years) and the elderly (58.1 per 10,000 person-years), but much lower in adults [8]. In Taiwan, the prevalence of norovirus among hospitalized pediatric AGE cases has been estimated at 8 – 30%, with some data indicating a higher prevalence of norovirus infection following the availability of the rotavirus vaccine (beginning in 2006 as a self-paid immunization), despite coverage < 50% [9–11]. In a 2011 – 2012 study not limiting to hospitalized cases, norovirus prevalence was even higher among children < 10 (53%), but lower when including adults (11%) [12]. Norovirus incidence data has not been previously reported in this population.
As research and development of norovirus vaccines accelerates, the need for up-to-date estimates of norovirus disease burden only increases [13]. Data from diverse regions and across the age spectrum will be important in providing baseline estimates from which to calculate vaccine impact. The objective of the present study was to estimate the incidence of norovirus-associated hospitalizations across the age spectrum in Taiwan, using indirect attribution from regression modeling on national hospitalizations data.
Methods
Data Sources
Data on AGE-related hospitalizations in Taiwan were obtained from the National Health Insurance Research Database (NHIRD) [14]. This database captures claims data from the National Health Insurance (NHI) program, which covers 99.9% of the population of Taiwan and pays for all medically necessary care [15]. Data were abstracted for 2003 – 2013. For this analysis, we defined an AGE-related hospitalization as a hospitalization with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for gastroenteritis in any diagnostic position. Hospitalizations were categorized as cause-specified if any diagnostic code indicating viral, bacterial, or parasitic disease was present; the remaining hospitalizations were categorized as cause-unspecified. Some cause-specified hospitalizations had multiple pathogen-type codes associated with them. Specific ICD-9-CM codes are listed in Table 1.
Table 1:
Pathogen categories and diagnostic codes used to identify and categorize acute gastroenteritis-associated hospitalizations—Taiwan, 2003 – 2013*
| Cause | ICD-9 Code | Annual* Mean Hospitalizations (in 1000) (%) | Hospitalization Rate per 10,000 person-years |
|---|---|---|---|
| Cause unspecified | 009.0–009.3, 558.9, 787.91, 008.8 | 84.4 (83.2) | 36.7 |
| Cause specified** | 17.1 (16.9) | 7.4 | |
| Viral | 008.6 | 8.1 (8.0) | 3.5 |
| Bacterial | 001.0–01.9, 002.0–002.9, 003.0–003.1, 003.3–003.9, 004.0–004.9, 005.0–005.9, 008.0–008.5 | 9.3 (9.2) | 4.0 |
| Parasitic | 006.0–006.2, 006.8–006.9, 007.0–007.9 | 0.1 (0.1) | 0.1 |
| All-cause acute gastroenteritis | 101.4 (100) | 44.1 | |
Abbreviations: ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification.
From July 1 2003 through June 30 2013.
Multiple codes may be assigned to a given admission; thus, the sum of cases for each specific cause exceeds the subtotals for “cause unspecified” and “cause specified.” However, if any cause-specified code was included in the record, the hospitalization was categorized as such.
Population Data and Rate Calculations
Population data were provided from the Department of Household Registration Affairs, Ministry of the Interior, stratified by age, year, and sex [16]. Population and hospitalizations were grouped by age as follows: under 5 years, 5 – 19 years, 20 – 64 years, 65 years and older. Rates for AGE hospitalizations were calculated for each age group and expressed as annual hospitalizations per 10,000 persons. Given the wintertime seasonality of AGE and norovirus in particular, rates are presented by seasonal year (July – June) as opposed to calendar year (January – December).
Statistical Methods for Norovirus Estimation
Norovirus is not often laboratory confirmed, and thus ICD-9-CM codes for norovirus are rarely used. In order to estimate the number and rate of norovirus-associated hospitalizations, we employed a statistical method that has been previously described [3, 5, 17–20]. We first modeled monthly counts of cause-unspecified AGE hospitalizations. We made the following assumptions: 1) the number of cause-unspecified AGE hospitalizations that could be attributed to each pathogen group (bacterial, viral, parasitic) was proportional to the actual number of cause-specified AGE hospitalizations in each group; 2) AGE case numbers may vary seasonally and secularly; 3) patterns may vary by age group. Thus, for each age group, we modeled the number of cause-unspecified AGE hospitalizations as a function of bacterial cases, rotavirus cases, parasitic cases, and study month (to control for month and year and thus seasonal and secular variation). Rotavirus was chosen to represent viral cases because of its known winter seasonality, which may overlap with norovirus seasonality. Due to low case counts of parasitic infection codes, we used parasite counts summed over all age groups in each model (as opposed to using parasite counts within each age group). A small number of cause-specified hospitalizations (2%) had multiple causes associated with them (e.g., viral and parasitic); these contributed to counts for each specified cause (e.g., to viral and parasitic counts). A Poisson distribution was used. The model can be expressed by the following formula:
CU indicates the number of cause-unspecified AGE hospitalizations, Rota indicates the number of rotavirus-coded AGE hospitalizations, Bact indicates the number of bacteria-coded AGE hospitalizations, Para indicates the number of parasite-coded AGE hospitalizations, i indicates the age group, and j indicates the month-year.
The estimated coefficients from the model above were then multiplied by the monthly counts of each cause-specified pathogen group (i.e., bacterial, rotaviral, or parasitic AGE hospitalizations) to generate estimates of the number of cause-unspecified AGE cases that could be attributed to specific causes. The remaining cause-unspecified AGE (the residual) were then used to generate estimates of norovirus AGE hospitalizations: the minimum residual for each seasonal year was subtracted from the residual for each month-year to generate the estimated number of norovirus cases for that month-year. This assumes that there is one month each year with no norovirus-associated visits, and that any excess seasonality not explained by the month-year term in the model is attributable to norovirus. Norovirus-coded hospitalizations were extremely rare, as norovirus testing was only available at two medical centers during the study period. Norovirus-specific counts were added to the model-generated estimates to yield totals referred to herein as predicted norovirus. The uncertainty of the model predictions (95% confidence intervals [CI]) was applied to the predicted norovirus counts to generate 95% CI for predicted norovirus.
Data were analyzed using SAS, version 9.4 (Cary, NC) and the R Environment for Statistical Computing.
Results
Over the course of the study period, 2003 – 2013, there was a mean of 101,400 gastroenteritis-associated hospitalizations in Taiwan annually, with the vast majority (83%) of these having no specified cause (Table 1). This amounted to a rate of 44 gastroenteritis-associated hospitalizations per 10,000 person-years. Among hospitalizations with specified causes, bacterial codes were slightly more common than viral causes, while parasitic causes were rarely coded. Norovirus-specific codes were extremely rare: only 482 norovirus-specified hospitalizations were reported during the entire study period, accounting for 0.05% of all AGE hospitalizations and 0.6% of cause-unspecified hospitalizations.
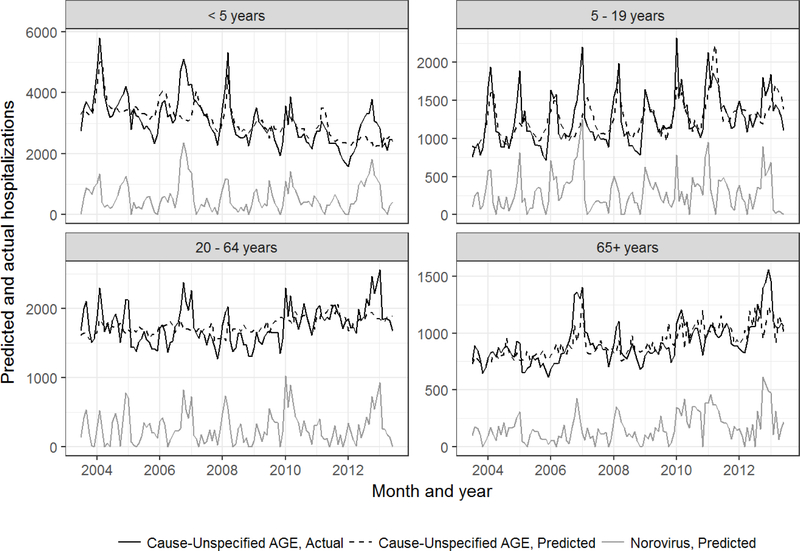
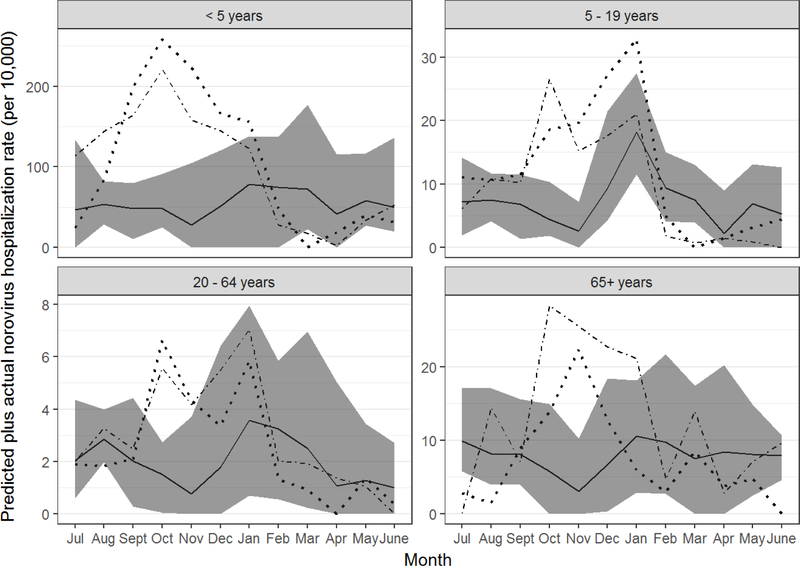
When cause-unspecified hospitalizations were modeled as a function of cause-specified hospitalizations and time, a winter-peaking seasonal pattern was evident in the predicted norovirus values (Figure 1). The clearest and highest peaks were during the 2006/2007 and 2012/2013 winters, with the differences most notable for children < 20 years of age in 2006/2007, and for children < 5 years in 2012/2013. For the oldest age group, higher-than-normal activity was noted in the 2012/2013 winter. In these epidemic years, peak predicted norovirus activity occurred earlier (October – January) as compared to non-epidemic years (December – March) (Figure 2).
Figure 1:
Predicted, coded, and residual acute gastroenteritis hospitalizations by month and age group, July 1, 2003 – June 30, 2013. The solid black line represents the actual number of cause-unspecified acute gastroenteritis hospitalizations. The dotted line represents the predicted value based on the time series regression. The gray line represents the predicted monthly norovirus hospitalizations, calculated as the monthly residual less the minimum residual for that seasonal year, plus any norovirus-coded hospitalizations for that month.
Figure 2:
Estimated norovirus-associated discharges per 10,000 persons from seasonal years 2003/2004 through 2012/2013. Gray regions represent the estimated monthly (July–June) minimum and maximum discharges per 10,000 persons for all years except 2003/2004 and 2012/2013. The epidemic seasons of 2006/2007 and 2012/2013 are represented by separate dotted and dashed lines, respectively. The mean norovirus-associated discharge rates are represented by a solid black line.
Examination of calculated gastroenteritis rates and predicted norovirus rates by seasonal year (July – June) showed year-to-year variability (Table 2). Predicted norovirus peaked in 2006/2007 (9.7 hospitalizations per 10,000 person-years, 95% CI: 9.5 – 10.0) and 2012/2013 (9.4 [9.0 – 9.7] hospitalizations per 10,000 person-years).
Table 2:
Calculated Rates (per 10,000 Person-Years) of Acute Gastroenteritis (AGE) by Seasonal Year—Taiwan, 2003 – 2013*
| Total AGE | Cause-Unspecified AGE | Predicted Norovirus AGE | |
|---|---|---|---|
| 2003/2004 | 49.9 | 40.5 | 6.2 (5.8–6.6) |
| 2004/2005 | 44.1 | 37.9 | 6.3 (6.0–6.6) |
| 2005/2006 | 41.6 | 33.7 | 5.6 (5.3–5.9) |
| 2006/2007 | 50.8 | 43.2 | 9.7 (9.5–10.0) |
| 2007/2008 | 44.3 | 36.2 | 5.7 (5.3–6.0) |
| 2008/2009 | 38.9 | 32.5 | 4.6 (4.4–4.9) |
| 2009/2010 | 43.7 | 36.0 | 8.3 (8.0–8.6) |
| 2010/2011 | 44.1 | 35.9 | 6.7 (6.4–7.0) |
| 2011/2012 | 37.9 | 32.1 | 5.0 (4.7–5.3) |
| 2012/2013 | 45.7 | 38.9 | 9.4 (9.0–9.7) |
From July 1 2003 through June 30, 2013.
Stratification of gastroenteritis hospitalization rates by age showed that children under 5 years bore the greatest burden, by a factor of 10 (Table 3). Among children under 5 years, there were 453 gastroenteritis-associated hospitalizations per 10,000 person-years, including 64 predicted norovirus-associated hospitalizations per 10,000 person-years, amounting to almost 7000 cases per year. The lowest burden in terms of incidence was found in adults 20 – 64 years of age, while the remaining two age groups (older children and older adults) had similar predicted rates of norovirus-associated hospitalizations.
Table 3:
Calculated Rates (per 10,000 Person-Years) and Mean Annual Cases (in 1000s) of Acute Gastroenteritis (AGE) by Age Group—Taiwan, 2003 – 2013*
| Rates per 10,000 Person-Years |
Mean Annual Cases (in 1000s) |
|||||
|---|---|---|---|---|---|---|
| Total AGE | Cause-Unspecified AGE | Predicted Norovirus | Total AGE | Cause-Unspecified AGE | Predicted Norovirus | |
| < 5 years | 453.4 | 348.3 | 63.7 (61.5–66.1) | 48.1 | 37.0 | 6.8 (6.5–7.0) |
| 5 – 19 years | 39.9 | 34.3 | 7.9 (7.6–8.3) | 17.7 | 15.2 | 3.5 (3.4–3.7) |
| 20 – 64 years | 15.2 | 14.0 | 2.1 (2.0–2.3) | 23.1 | 21.1 | 3.2 (3.1–3.4) |
| 65+ years | 52.5 | 46.3 | 8.4 (7.9–9.0) | 12.5 | 11.0 | 2.0 (1.9–2.2) |
| Total | 44.1 | 36.7 | 6.7 (6.4–7.1) | 101.4 | 84.4 | 15.5 (14.8–16.3) |
From July 1 2003 through December 31 2013.
Discussion
This study adds to the limited literature on the incidence of norovirus-associated hospitalization and highlights the high burden of severe norovirus among children in Taiwan. We estimated that norovirus is associated with 15,500 hospitalizations annually across the island, with over one third of these occurring in children under 5 years of age. These estimated norovirus hospitalizations exhibited winter seasonality, peaking December – March. Relative peaks also tended to be higher and earlier during seasons with known increased norovirus activity in Taiwan associated with the emergence of new strains, such as the 2006/2007 and 2012/2013 seasons, as captured in Taiwan’s outbreak reporting system; differences in incidence and peak incidence by age may also be related to the phenomenon of genotype replacement [21–26].
Our estimate of 6.7 (6.4 – 7.1) norovirus hospitalizations per 10,000 person-years is within the range of those reported in other studies (1.2 – 7.0 per 10,000 person-years), including two studies (Lopman et al. and Verstraeten et al.) which used comparable methods [2, 4–6]. Our estimate in the pediatric population (63.7 [61.5 – 66.1] norovirus hospitalizations per 10,000 person-years) is somewhat higher than estimates in other studies conducted in the US, England, and Israel (7.2 – 33.0 hospitalizations per 10,000 person-years) [5, 6, 27, 28], though much lower than an estimate from a study conducted in Hong Kong (147.5 hospitalizations per 10,000 person-years) [8]. However, it is worth noting that samples in Chan et al.’s Hong Kong study were tested only upon clinical suspicion of norovirus, which may have inflated estimates, since the prevalence of norovirus among suspect norovirus cases is likely higher than among all-cause gastroenteritis cases. Our estimate in older adults of 8.4 hospitalizations per 10,000 person-years is very similar to the 8 per 10,000 person-years reported by Grytdal et al. in a Veterans’ Affairs hospital population [29], though slightly lower than the 18.5 per 10,000 person-years reported by Lopman et al. in a slightly older population [5], and again far lower than the estimate of 58.1 per 10,000 person-years from Chan’s study [8].
Our methods are subject to several limitations. The key underlying assumption to these estimates is that residual seasonality in cause-unspecified gastroenteritis hospitalizations (i.e., those not accounted for by the other pathogens in the model) is attributable to norovirus. This may lead to an overestimation of the role of norovirus if other pathogens also have overlapping winter seasonality; however, it is reassuring that astrovirus has not been shown to have strong seasonality in pediatric infections in Taiwan [9, 11]. The fact that our peak predicted norovirus seasonal years correspond to known peak norovirus seasons in Taiwan also lends credibility to the estimates. It is also possible that our methods may have led to an underestimate of the norovirus burden. For example, since rotavirus and norovirus seasonality overlap in Taiwan [30], and rotavirus testing is not always performed, it may be that some rotavirus infections were mistakenly attributed to norovirus. However, rotavirus testing was commonly performed in the inpatient setting in Taiwan during the study period. Further, including rotavirus as a predictor in our model should have mitigated this possibility. Another assumption of the model is that there is one month of the year when there are no norovirus-associated hospitalizations. Since norovirus does in fact circulate year-round, this assumption will cause an underestimate [21].
Our study is one of the first to generate a population-based estimate of severe norovirus disease incidence in Asia, and provides important data on the burden of norovirus in Taiwan, particularly in children and the elderly. These results support the increased use of diagnostic testing for norovirus, as a confirmed norovirus diagnosis may affect decisions around infection prevention, thus helping to prevent spread in the healthcare setting or after discharge. Preventing such subsequent transmission may be particularly relevant for children and the elderly, given that schools and long-term care facilities are the most common outbreak locations in Taiwan [23]. Our findings also support the continued development of norovirus vaccines, which could benefit individuals across the age range. Additional studies, particularly multi-year studies, are needed to quantify the burden of norovirus across the spectrum of severity from outpatient visits to mortality, especially in Asia, where such studies of norovirus are scarce.
Acknowledgments
FUNDING
This work was supported by grant support provided by the Taiwan Centers for Disease Control [grant number MOHW105-CDC-C-114-123302].
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the US Centers for Disease Control and Prevention (CDC).
REFERENCES
- 1.Ahmed SM, Hall AJ, Robinson AE, et al. Global prevalence of norovirus in cases of gastroenteritis: a systematic review and meta-analysis. Lancet Infect Dis 2014; 14:725–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States--major pathogens. Emerg Infect Dis 2011; 17:7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hall AJ, Curns AT, McDonald LC, Parashar UD, Lopman BA. The roles of Clostridium difficile and norovirus among gastroenteritis-associated deaths in the United States, 1999–2007. Clin Infect Dis 2012; 55:216–23. [DOI] [PubMed] [Google Scholar]
- 4.Verhoef L, Koopmans M, W VANP, et al. The estimated disease burden of norovirus in The Netherlands. Epidemiol Infect 2013; 141:496–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lopman BA, Hall AJ, Curns AT, Parashar UD. Increasing rates of gastroenteritis hospital discharges in US adults and the contribution of norovirus, 1996–2007. Clin Infect Dis 2011; 52:466–74. [DOI] [PubMed] [Google Scholar]
- 6.Verstraeten T, Cattaert T, Harris J, Lopman B, Tam CC, Ferreira G. Estimating the Burden of Medically Attended Norovirus Gastroenteritis: Modeling Linked Primary Care and Hospitalization Datasets. J Infect Dis 2017; 216:957–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bartsch SM, Lopman BA, Ozawa S, Hall AJ, Lee BY. Global Economic Burden of Norovirus Gastroenteritis. PLoS One 2016; 11:e0151219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan MC, Leung TF, Chung TW, et al. Virus Genotype Distribution and Virus Burden in Children and Adults Hospitalized for Norovirus Gastroenteritis, 2012–2014, Hong Kong. Sci Rep 2015; 5:11507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen CJ, Wu FT, Huang YC, et al. Clinical and Epidemiologic Features of Severe Viral Gastroenteritis in Children: A 3-Year Surveillance, Multicentered Study in Taiwan With Partial Rotavirus Immunization. Medicine (Baltimore) 2015; 94:e1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen SY, Tsai CN, Chen CL, et al. Severe viral gastroenteritis in children after suboptimal rotavirus immunization in Taiwan. Pediatr Infect Dis J 2013; 32:1335–9. [DOI] [PubMed] [Google Scholar]
- 11.Chen SY, Chang YC, Lee YS, et al. Molecular epidemiology and clinical manifestations of viral gastroenteritis in hospitalized pediatric patients in Northern Taiwan. J Clin Microbiol 2007; 45:2054–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang MB, Chen CH, Chen SC, Chou YC, Yu CP. Epidemiological and molecular analysis of human norovirus infections in Taiwan during 2011 and 2012. BMC Infect Dis 2013; 13:338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopman BA, Steele D, Kirkwood CD, Parashar UD. The Vast and Varied Global Burden of Norovirus: Prospects for Prevention and Control. PLoS Med 2016; 13:e1001999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Health Research Institutes of Taiwan. National Health Insurance Research Database: Background Available at: http://nhird.nhri.org.tw/en/index.html. Accessed August 1 2017.
- 15.Universal Health Coverage in Taiwan. Available at: http://www.nhi.gov.tw/English/Content_List.aspx?n=8FC0974BBFEFA56D&topn=ED4A30E51A609E49. Accessed August 1 2017.
- 16.Statistical Yearbook of the Interior. Taiwan 2015. Available at: http://sowf.moi.gov.tw/stat/year/elist.htm. Accessed August 1 2017.
- 17.Harris JP, Edmunds WJ, Pebody R, Brown DW, Lopman BA. Deaths from norovirus among the elderly, England and Wales. Emerg Infect Dis 2008; 14:1546–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haustein T, Harris JP, Pebody R, Lopman BA. Hospital admissions due to norovirus in adult and elderly patients in England. Clin Infect Dis 2009; 49:1890–2. [DOI] [PubMed] [Google Scholar]
- 19.Markov PV, Crowcroft NS. Modelling the unidentified mortality burden from thirteen infectious pathogenic microorganisms in infants. Epidemiol Infect 2007; 135:17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gastanaduy PA, Hall AJ, Curns AT, Parashar UD, Lopman BA. Burden of norovirus gastroenteritis in the ambulatory setting--United States, 2001–2009. J Infect Dis 2013; 207:1058–65. [DOI] [PubMed] [Google Scholar]
- 21.Chen SY, Feng Y, Chao HC, et al. Emergence in Taiwan of novel norovirus GII.4 variants causing acute gastroenteritis and intestinal haemorrhage in children. J Med Microbiol 2015; 64:544–50. [DOI] [PubMed] [Google Scholar]
- 22.Chen SY, Tsai CN, Lai MW, et al. Norovirus infection as a cause of diarrhea-associated benign infantile seizures. Clin Infect Dis 2009; 48:849–55. [DOI] [PubMed] [Google Scholar]
- 23.Wu FT, Chen HC, Yen C, et al. Epidemiology and molecular characteristics of norovirus GII.4 Sydney outbreaks in Taiwan, January 2012-December 2013. J Med Virol 2015; 87:1462–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tzu-Chi Liu L KT, Wu CY, Liao WT, Hall AJ, Wu FT. Recombinant GII.P16-GII.2 norovirus, Taiwan, 2016. Emerg Infect Dis 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tsai CN, Lin CY, Lin CW, Shih KC, Chiu CH, Chen SY. Clinical relevance and genotypes of circulating noroviruses in northern Taiwan, 2006–2011. J Med Virol 2014; 86:335–46. [DOI] [PubMed] [Google Scholar]
- 26.Wu FT, Oka T, Katayama K, et al. Genetic diversity of noroviruses in Taiwan between November 2004 and March 2005. Arch Virol 2006; 151:1319–27. [DOI] [PubMed] [Google Scholar]
- 27.Payne DC, Vinje J, Szilagyi PG, et al. Norovirus and medically attended gastroenteritis in U.S. children. N Engl J Med 2013; 368:1121–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leshem E, Givon-Lavi N, Vinje J, Gregoricus N, Parashar U, Dagan R. Differences in Norovirus-Associated Hospital Visits Between Jewish and Bedouin Children in Southern Israel. Pediatr Infect Dis J 2015; 34:1036–8. [DOI] [PubMed] [Google Scholar]
- 29.Grytdal SP, Rimland D, Shirley SH, et al. Incidence of Medically-Attended Norovirus-Associated Acute Gastroenteritis in Four Veteran’s Affairs Medical Center Populations in the United States, 2011–2012. PLoS One 2015; 10:e0126733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang SY, Hwang KP, Wu FT, et al. Epidemiology and clinical peculiarities of norovirus and rotavirus infection in hospitalized young children with acute diarrhea in Taiwan, 2009. J Microbiol Immunol Infect 2010; 43:506–14. [DOI] [PubMed] [Google Scholar]