Abstract
Brown tumor is one of the lesions that develop in patients with hyperparathyroidism (HPT) and represents the terminal stages of bone remodeling process. Any of the skeletal bones can be affected including the craniomaxillofacial ones. Many a times, brown tumor was detected after a final diagnosis of HPT is made. However, on occasions, brown tumor can be the first clinical sign of the disease. Primary HPT is an uncommon systemic disease usually caused by hyperplasia or adenoma of the parathyroid glands. It causes overproduction of parathormone, which may affect the entire skeleton, causing bone resorption appear as cyst-like lesions called osteitis fibrosa cystica or brown tumors. Here, we report such a rare case in which multiple radiolucent lesions were noticed in the ramus part of the mandible and premolar region bilaterally, as the initial signs of primary HPT are presented in this report.
Keywords: Brown tumor, giant cell lesions, hyperparathyroidism, parathormone
INTRODUCTION
Overproduction of parathormone (PTH) in cases of hyperparathyroidism (HPT) may affect any part of the skeleton resulting in single/multiple cyst-like lesions of bone called brown tumors. These are caused by rapid osteoclastic activity and peritrabecular fibrosis resulting in erosive bony lesions, form of local destructive phenomenon due to HPT. They represent a reparative cellular process rather than true neoplasia.[1,2] These changes are found in primary or more rarely, secondary HPT. The reported incidence of brown tumor is 4.5% in primary and 1.5%–1.7% in secondary HPT. The prevalence of brown tumor is about 0.1% and is more often in persons older than 50 years.[3]
Although brown tumor of jaws is a rare manifestation of primary HPT, it is important to consider this diagnosis in all unexplained lucent lesions of both the jaws (mandible and maxilla). The case presented here may enlighten the clinicians the importance of complete clinical assessment of patients to be aware of the manifestations of these types of lesions in accurate diagnosis.
CASE REPORT
A 22-year-old female came with a complaint of large swelling in the right back region of lower jaw 1 year back. Initially, it was small in size and expanded to the present size. No treatment was given as the patient was pregnant and in her first trimester. Since the last 2 months, the patient is having intermittent dull pain and slight bleeding from the lesion while eating and swallowing. On extraoral examination, a single, diffuse swelling measuring about 4 cm × 3 cm, on the angle-ramus area of the right mandible [Figure 1] was noted.
Figure 1.

Clinical image showing extraoral swelling on the right mandibular body area
Panoramic radiograph showed a round, well-defined radiolucency on the right side of the lower border of the mandible. Due to the dilemma about the nature of the lesion and the adjacent soft-tissue swelling, surgical exploration of the lesion in local anesthesia was planned. The mandibular lesion was curetted and sent for histopathological examination.
In the meantime, few biochemical tests were also performed to clear the cloud on the lesion. The results of laboratory data were as follows:
PTH → 1828 pg/mL (10–72 ng/L)
Serum alkaline phosphatase (ALP) → 1378 IU/L
Erythrocyte sedimentation rateà30 mm/h
Serum calcium → 12.5 mg/dL.
She underwent a computed tomography (CT) scan as per the opinion of the surgeon, which confirmed a 4 cm × 5 cm expansile, thin-walled radiolucency within the right mandible just lateral to the midline. There was an associated scalloping of adjacent cortex. A similar but smaller radiolucent lesion was also noted on the left side premolar area of the mandible [Figure 2]. Surprisingly, in few slices of CT, a radiolucent lesion at the level of C7 was noted both in lateral as well as coronal sections [Figure 3]. Concurrently for the affirmation of HPT, a 9mTc scan of parathyroid glands was done and showed increased uptake in the left thyroid due to a nodule at the lower pole which confirmed the left “parathyroid adenoma.” Histology of the dissected mass showed hemorrhagic, fibrovascular connective tissue containing spindle-shaped fibroblasts and numerous multinucleated giant cells [Figure 4]. All clinical, histological, radiological and biochemical findings confirmed brown tumor due to primary HPT resulting from parathyroid adenoma. The patient was referred to the physician and endocrinologist for further treatment. The histologic differential diagnosis was either giant cell reparative granuloma or brown tumor of primary HPT. Based on clinical, radiological, histopathological and biochemical assays, a final diagnosis of “Brown tumor of primary hyperparathyroidism” was made.
Figure 2.
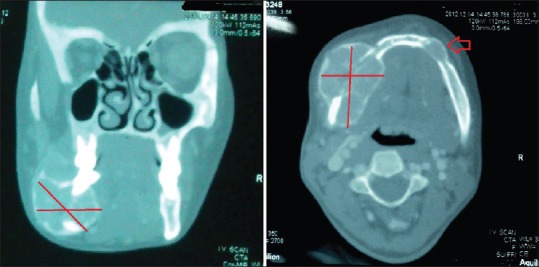
Computed tomography scan of the mandible showing a large swelling on the right side and a smaller lesion on the left premolar area (show by arrow)
Figure 3.
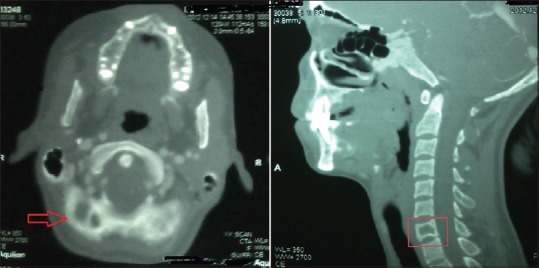
Photograph of computed tomography image of neck area showing a radiolucent lesion at C7 level both in coronal (show by arrow) and lateral (indicated in the box) views
Figure 4.
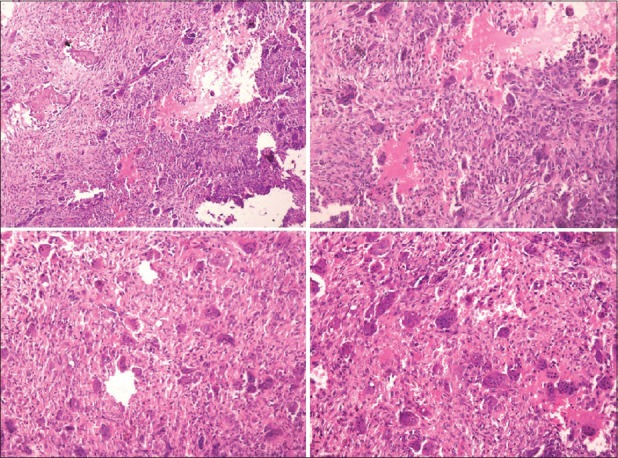
Photomicrograph showing multiple giant cells with fibroblasts, blood vessels and areas of hemorrhage in the stroma (H and E stain)
The patient is on pharmacotherapy with periodic checkup and evaluation of blood calcium and Vitamin D3 levels. After 6 months of follow-up, the patient underwent for surgical excision of “parathyroid adenoma.” Later on, the patient was lost for further follow-up and consultation.
DISCUSSION
HPT is a disease in which there may be a complex of biochemical, anatomic and clinical abnormalities resulting from increased secretion of parathormone (PTH). It may occur in primary, secondary and tertiary forms.[3] Brown tumors represent the terminal stages of bone remodeling process in HPT.[2]
The term “brown tumor” was first coined by Jaffe for bony lesions occurring in HPT owing to reddish brown color due to the high vascularity and hemosiderin pigment. The term tumor is a misnomer, and osteoclastoma is also used often. These lesions are basically nonneoplastic and result from reparative process; histologically, contain multiple giant cells admixed with stromal fibroblasts and CT matrix.[4,5]
Brown tumor is a rare presentation of primary HPT, and only 5% of cases are associated with brown tumors.[2] Primary HPT is usually caused by solitary adenoma (80%), also hyperplasia (15%), multiple adenomas (4%) and primary neoplasia (1.5%) and is seen predominantly in women.[3] It can occur as solitary or multiple lesions in any bone; most common sites of involvement are pelvis, ribs, clavicle, femora and the extremities.[6,7] The facial bones are affected in about 2% of cases. It may be the first clinical manifestation of HPT seldom as in the present case.
Other manifestations of HPT are generally apparent although a brown tumor is occasionally the only presenting finding in the disease.[6] Clinically, these lesions are slow growing and generally asymptomatic. However, they can be locally destructive by weakening bone structure and leading to pathological fractures.[8] Moreover, when a brown tumor involves the face and having aggressive growth, it may cause severe deformities, discomfort, alteration of the masticatory apparatus and difficulty to breathe through the nose or to eat.[6,9]
Brown tumors have no pathognomonic histologic changes and are histologically indistinguishable from the other giant cell lesions such as fibrous dysplasia, giant cell tumor and reparative granuloma. Therefore, a definitive diagnosis should be made by clinical history and confirmed by biochemical tests.[10]
In primary HPT, there is a need for biopsy as the brown tumor could be the first clinical manifestation of the disease.[11,12] Conversely, biopsy is not needed in secondary HPT since the clinical findings usually help in establishing the diagnosis.[13] Microscopically, brown tumors represent localized accumulations of fibrous tissue and giant cells, which can replace bone and may produce osseous expansion. All lesions of the jaws showing giant cells microscopically should raise suspicion of HPT. The differential diagnosis is based on the clinical and radiographic findings. Serum calcium and phosphorus level disturbances and increased levels of serum ALP and PTH are helpful to diagnose a brown tumor.[14] In the present case, serum PTH and ALP levels were much higher than normal but no/little alteration was noted in calcium level.
Brown tumors are nonneoplastic lesions resulting from abnormal bone metabolism in HPT resulting in local destructive phenomenon of single or multiple bones. On clinical examination and using only routine panoramic radiography, the lesions may resemble osteosarcoma, bone metastases of a carcinoma, multiple myeloma, Langerhans cell histiocytosis, Paget's disease and osteomyelitis. Histologically and radiographically, it is very similar to the other giant cell lesions such as true giant cell tumor, reparative giant cell granuloma, cherubism and aneurysmal bone cyst.[15]
Early diagnosis is to prevent further late bony complications of the disease include generalized osteoporosis and multiple focal areas of demineralization.[16,17] Normalization of PTH levels will often cause the brown tumors to regress or sometimes even resolve spontaneously.[18]
The first line of treatment for primary HPT is parathyroidectomy. However, the choice of treatment is still controversial for brown tumors.[19] A general and most accepted treatment of brown tumor is treating the underlying cause of HPT, and if lesion still persists after the primary treatment, enucleation and curettage should be added. Some clinicians believe that excision of brown tumors before or concurrent with parathyroid anomalies is better.[11,20,21] Few authors have treated with systemic corticosteroids initially, and after reduction its size, surgical excision is done.[12] The authors believe that the treatment protocol for brown tumor depends on the clinical symptoms. However, in case of no functional limitations a medical therapy is preferred hoping for probable regression and later surgical excision, if required.
The case presented here draws the attention and interest of the general dental practitioners, oral and maxillofacial surgeons, endocrinologists and radiologists who play a vital role for patients with HPT since the disease may result in nearly serious consequences if neglected.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fineman I, Johnson JP, Di-Patre PL, Sandhu H. Chronic renal failure causing brown tumors and myelopathy. Case report and review of pathophysiology and treatment. J Neurosurg. 1999;90:242–6. doi: 10.3171/spi.1999.90.2.0242. [DOI] [PubMed] [Google Scholar]
- 2.Wyngaarden JB, Smith LH, Cecil RL. 19th ed. Philadelphia: W.B. Saunders; 1992. Cecil Textbook of Medicine; pp. 1409–26. [Google Scholar]
- 3.Keyser JS, Postma GN. Brown tumor of the mandible. Am J Otolaryngol. 1996;17:407–10. doi: 10.1016/s0196-0709(96)90075-7. [DOI] [PubMed] [Google Scholar]
- 4.Ashrafi SK, Suhail Z, Khambaty Y. Brown tumor of maxilla – A rare occurrence. Pak J Otolaryngol. 2010:26:61–2. [Google Scholar]
- 5.Jebasingh F, Jacob JJ, Shah A, Paul TV, Seshadri MS. Bilateral maxillary brown tumours as the first presentation of primary hyperparathyroidism. Oral Maxillofac Surg. 2008;12:97–100. doi: 10.1007/s10006-008-0105-9. [DOI] [PubMed] [Google Scholar]
- 6.Pinar Sumer A, Arik N, Sumer M, Karagoz F. A rare complication of secondary hyperparathyroidism. Brown tumor of the maxilla and mandible. Saudi Med J. 2004;25:2010–2. [PubMed] [Google Scholar]
- 7.Daniels JS. Primary hyperparathyroidism presenting as a palatal brown tumor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:409–13. doi: 10.1016/j.tripleo.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Al-Gahtany M, Cusimano M, Singer W, Bilbao J, Kovacs K, Marotta T, et al. Brown tumors of the skull base. Case report and review of the literature. J Neurosurg. 2003;98:417–20. doi: 10.3171/jns.2003.98.2.0417. [DOI] [PubMed] [Google Scholar]
- 9.Morrone LF, Ettorre GC, Passavanti G, Tampoia M, Schiavone P, Coratelli P, et al. Maxillary brown tumor in secondary hyperparathyroidism requiring urgent parathyroidectomy. J Nephrol. 2001;14:415–9. [PubMed] [Google Scholar]
- 10.Lessa MM, Sakae FA, Tsuji RK, Filho BC, Voegels RL, Butugan O, et al. Brown tumor of the facial bones: Case report and literature review. Ear Nose Throat J. 2005;84:432–4. [PubMed] [Google Scholar]
- 11.Yamazaki H, Ota Y, Aoki T, Karakida K. Brown tumor of the maxilla and mandible: Progressive mandibular brown tumor after removal of parathyroid adenoma. J Oral Maxillofac Surg. 2003;61:719–22. doi: 10.1053/joms.2003.50142. [DOI] [PubMed] [Google Scholar]
- 12.Guimaraes AL, Marques-Silva L, Gomes CC, Castro WH, Mesquita RA, Gomez RS. Peripheral brown tumour of hyperparathyroidism in the oral cavity. Oral Oncol Extra. 2006;42:91–3. [Google Scholar]
- 13.Triantafillidou K, Zouloumis L, Karakinaris G, Kalimeras E, Iordanidis F. Brown tumors of the jaws associated with primary or secondary hyperparathyroidism. A clinical study and review of the literature. Am J Otolaryngol. 2006;27:281–6. doi: 10.1016/j.amjoto.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Wood NK, Goaz PW. 5th ed. St. Louis: Mosby; 1997. Differential Diagnosis of Oral and Maxillofacial Lesions; pp. 393–6. [Google Scholar]
- 15.Shang ZJ, Li ZB, Chen XM, Li JR, McCoy JM. Expansile lesion of the mandible in a 45-year-old woman. J Oral Maxillofac Surg. 2003;61:621–5. doi: 10.1053/joms.2003.50073. [DOI] [PubMed] [Google Scholar]
- 16.Suarez-Cunqueiro MM, Schoen R, Kersten A, Klisch J, Schmelzeisen R. Brown tumor of the mandible as first manifestation of atypical parathyroid adenoma. J Oral Maxillofac Surg. 2004;62:1024–8. doi: 10.1016/j.joms.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 17.Leal CT, Lacativa PG, Gomes EM, Nunes RC, Costa FL, Gandelmann IH, et al. Surgical approach and clinical outcome of a deforming brown tumor at the maxilla in a patient with secondary hyperparathyroidism due to chronic renal failure. Arq Bras Endocrinol Metabol. 2006;50:963–7. doi: 10.1590/s0004-27302006000500021. [DOI] [PubMed] [Google Scholar]
- 18.Alvarado F, Waguespack SG, Campbell JH, Williams TP. Expansile intraosseus lesion of the mandible. J Oral Maxillofac Surg. 2003;61:1318–23. doi: 10.1016/s0278-2391(03)00734-1. [DOI] [PubMed] [Google Scholar]
- 19.Scott SN, Graham SM, Sato Y, Robinson RA. Brown tumor of the palate in a patient with primary hyperparathyroidism. Ann Otol Rhinol Laryngol. 1999;108:91–4. doi: 10.1177/000348949910800114. [DOI] [PubMed] [Google Scholar]
- 20.Cebesoy O, Karakok M, Arpacioglu O, Baltaci ET. Brown tumor with atypical localization in a normocalcemic patient. Arch Orthop Trauma Surg. 2007;127:577–80. doi: 10.1007/s00402-007-0302-2. [DOI] [PubMed] [Google Scholar]
- 21.Emin AH, Süoǧlu Y, Demir D, Karatay MC. Normocalcemic hyperparathyroidism presented with mandibular brown tumor: Report of a case. Auris Nasus Larynx. 2004;31:299–304. doi: 10.1016/j.anl.2004.03.014. [DOI] [PubMed] [Google Scholar]


