To the Editor:
Effective as of September 23, 2010, a national policy change allowed young adults less than age 26 years to remain on their parents’ private health insurance plans with dependent coverage (“dependent coverage extension” [DCE]).1 Subsequently, private health insurance coverage among young adults aged 19 to 25 years increased.1 Research has begun to examine the impact of DCE on health care use among this population1–3; asthma-related effects of DCE remain unknown. We investigated access to care among young adults with current asthma aged 19–25 years before and after DCE implementation, using data from a nationally representative survey.
We analyzed Behavioral Risk Factor Surveillance System (BRFSS) data from 2006–2009 and 2011–2016 (before and after DCE implementation, respectively); BRFSS is a state-based, random-digit-dialed, cross-sectional telephone survey of non-institutionalized U.S. adults. We treated the year 2010 as a phase-in period by excluding 2010 data, similar to prior literature.2,4
Our study population was adults with current asthma aged 19–32 years; those aged 19–25 years were eligible by age to be affected by DCE, whereas those aged 26–32 years served as our comparison group. We define current asthma in Table E1 of the Online Repository.
We investigated health insurance-related barriers using responses to two BRFSS questions: (1) “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare?” and (2) “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?” Regarding the latter question, we conducted two subanalyses: one restricted to insured adults with current asthma, and another restricted to uninsured adults with current asthma.
We used SUDAAN to calculate single-year point estimates and standard errors for each variable by age group, weighted to be representative of all 50 states. We compared the two groups using t-tests (α=0.05) within each dataset (2006–2009; 2011–2016). We could not compare responses across datasets because of changes to BRFSS methods implemented in 2011 (i.e., improved weighting methods [using iterative proportional fitting weighting]5 and inclusion of cellular telephone interviews).6 Jurisdiction-specific Institutional Review Board (IRB) requirements apply to each participating state; informed consent was obtained. Analyses of BRFSS data are exempt from review by the Centers for Disease Control and Prevention IRB.
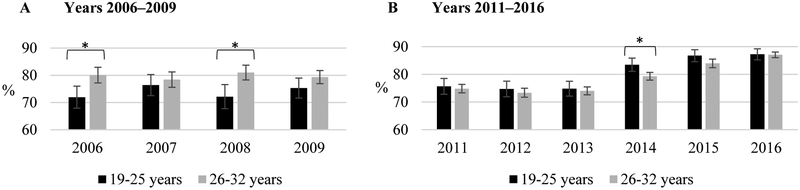
Our results were based on 48,194 survey responses from unique individuals, representative of 50,924,595 U.S. adults with current asthma aged 19–32 years (details in Table E2). In 2006–2009, fewer adults aged 19–25 years with current asthma reported health insurance coverage compared to those aged 26–32 years (Figure 1A). In contrast, in 2011–2016 more adults aged 19–25 years with current asthma reported health insurance coverage compared to those aged 26–32 years (Figure 1B).
Figure 1.
Prevalence of Health Insurance Coverage among Young Adults with Current Asthma, by Age Group: Behavioral Risk Factor Surveillance System, 2006–2009 and 2011–2016. A, Years 2006–2009. B, Years 2011–2016. *p<0.05.
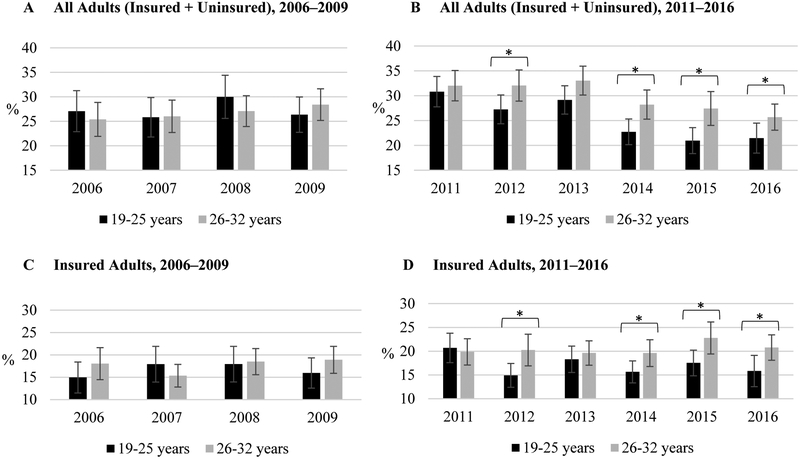
Regarding whether respondents could not see a doctor because of cost, we observed no consistent difference across age groups in 2006–2009 (Figure 2A). However, in 2011–2016 cost barriers to medical care were reported less frequently among adults aged 19–25 years with current asthma than the comparison group (Figure 2B). A similar pattern was present in a subanalysis of cost barriers to medical care restricted only to insured adults with current asthma from these age groups (Figure 2C and 2D). Significant differences were less consistent among uninsured adults with current asthma from these age groups (Figure E1).
Figure 2.
Percent of Young Adults with Current Asthma Who Could Not See a Doctor Because of Cost, by Insurance Status and Age: Behavioral Risk Factor Surveillance System, 2006–2009 and 2011–2016. A, All adults (insured + uninsured), 2006–2009. B, All adults (insured + uninsured), 2011–2016. C, Insured adults, 2006–2009. D, Insured adults, 2011–2016. *p<0.05.
In this nationally representative analysis, we observed improved health insurance coverage among adults with current asthma in the age group covered by DCE (ages 19–25 years) after 2010 (the year of DCE implementation), relative to a comparison group. Also, cost barriers to medical care were less frequent after 2010 among this population. Differences in cost barriers to medical care persisted after accounting for insurance coverage through a subanalysis restricted to insured adults. These patterns were not present before 2010.
This analysis is the first investigation of the asthma-related impact of DCE. To further strengthen this study, we conducted weighted statistical analyses so results were representative of all 50 states. Also, we included 10 years of data, a comparison group, and a subanalysis restricted to insured adults.
Our findings support and extend prior DCE-related literature not specific to asthma. After DCE implementation, health insurance coverage increased among U.S. adults aged 19–25 years in general.1 Delaying care or not receiving care because of cost also decreased in this population.1 Other publications have found overall reductions in emergency department use and increases in routine health checkups; asthma-specific visits were not examined.4,7 Existing literature on DCE includes studies on obstetrics-gynecology, mental health, and dental care.2,3,8,9
Our analysis had several limitations. Because of survey design, we could not differentiate between insurance coverage types (e.g., private, Medicaid, etc.), pinpoint cost barriers to asthma-specific care, or assess asthma-related health outcomes. These data were not longitudinal; rather, they represented serial cross-sectional surveys. Causality cannot be inferred from cross-sectional surveys. Non-response bias was possible; sampling and weighting procedures helped reduce this likelihood. Weighting can introduce estimate variability, so we provided standard errors with our estimates. Also, we were unable to directly compare pre- and post-DCE periods, because survey method changes implemented in 2011 precluded accurate comparisons. Lastly, we did not account for potential changes in the U.S. economy that could have affected health insurance coverage or cost barriers to medical care over this period.
In summary, we conducted a nationally representative analysis that shows increased health insurance coverage among adults with current asthma in the age group covered by DCE (ages 19–25 years) after DCE was implemented, relative to a comparison group. Also, we observed fewer cost barriers to medical care in this population after DCE implementation. This investigation is a first step in understanding the potential effects of this national policy change on people with asthma; exploration of asthma-specific treatments and health outcomes (e.g., emergency department visits) could advance knowledge on this topic. Also, this study could be used to inform future analyses of asthma-related impacts from other Affordable Care Act provisions.
Supplementary Material
Clinical Implications:
Effective 2010, young adults could remain on parental health plans until age 26 years. Afterwards, insurance coverage expanded and cost barriers to care decreased among 19–25-year-old adults with current asthma, versus a comparison group.
ACKNOWLEDGMENTS
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of interest: No conflicts of interest were reported by the authors of this paper.
REFERENCES
- 1.Sommers BD, Buchmueller T, Decker SL, Carey C, Kronick R. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff (Millwood). 2013;32(1):165–174. [DOI] [PubMed] [Google Scholar]
- 2.Robbins AS, Han X, Ward EM, Simard EP, Zheng Z, Jemal A. Association Between the Affordable Care Act Dependent Coverage Expansion and Cervical Cancer Stage and Treatment in Young Women. JAMA. 2015;314(20):2189–2191. [DOI] [PubMed] [Google Scholar]
- 3.McClellan CB. The Affordable Care Act’s Dependent Care Coverage Expansion and Behavioral Health Care. J Ment Health Policy Econ. 2017;20(3):111–130. [PubMed] [Google Scholar]
- 4.Lau JS, Adams SH, Park MJ, Boscardin WJ, Irwin CE, Jr. Improvement in preventive care of young adults after the Affordable Care Act: the Affordable Care Act is helping. JAMA Pediatr. 2014;168(12):1101–1106. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. The BRFSS Data User Guide. Available at: https://www.cdc.gov/brfss/data_documentation/pdf/UserguideJune2013.pdf. Accessed July 23, 2018.
- 6.Centers for Disease Control and Prevention. Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR Morb Mortal Wkly Rep. 2012;61(22):410–413. [PubMed] [Google Scholar]
- 7.Akosa Antwi Y, Moriya AS, Simon K, Sommers BD. Changes in Emergency Department Use Among Young Adults After the Patient Protection and Affordable Care Act’s Dependent Coverage Provision. Ann Emerg Med. 2015;65(6):664–672 e662. [DOI] [PubMed] [Google Scholar]
- 8.Cheng ER, Carroll AE. The Dependent Coverage Provision Is Good for Mothers, Good for Children, and Good for Taxpayers. JAMA Pediatr. 2018;172(5):487–488. [DOI] [PubMed] [Google Scholar]
- 9.Shane DM, Ayyagari P. Spillover Effects of the Affordable Care Act? Exploring the Impact on Young Adult Dental Insurance Coverage. Health Serv Res. 2015;50(4):1109–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.