Abstract
Objective:
To evaluate the effect of the Assistive Device Selection, Training and Education Program (ADSTEP) on falls and walking and sitting activity in people with multiple sclerosis (PwMS).
Design:
Randomized controlled trial.
Setting:
Veterans affairs medical center.
Participants:
PwMS (N=40) using a walking aid at baseline who had fallen in the previous year.
Interventions:
Participants were randomly assigned to ADSTEP or control. ADSTEP had 6 weekly, 40-minute, 1-on-1 sessions with a physical therapist, starting with walking aid selection and fitting, followed by task-oriented progressive gait training. Control was usual medical care with the option of ADSTEP after the study.
Main Outcome Measures:
The following were assessed at baseline, intervention completion, and 3 months later: falls, timed Up and Go, timed 25-foot walk, 2-minute walk, Four Square Step Test, International Physical Activity Questionnaire, Quebec User Evaluation of Satisfaction with Assistive Technologies, Multiple Sclerosis Walking Scale-12, Activities-Specific Balance Confidence Scale, and Multiple Sclerosis Impact Scale-29. Effect on these outcomes was estimated by a 2-by-2 repeated measures general linear model.
Results:
Fewer ADSTEP than control participants fell (χ2=3.96, P<.05. number needed to treat =3.3). Time spent sitting changed significantly differently with ADSTEP than with control from baseline to intervention completion (F=11.16, P=.002. ADSTEP: reduced 87.00 ±194.89min/d; control: increased 103.50±142.21min/d; d=0.88) and to 3-month follow-up (F=9.25, P=.004. ADSTEP: reduced 75.79 ±171.57min/d; control: increased 84.50±149.23min/d; d=0.79). ADSTEP yielded a moderate effect on time spent walking compared to control at 3-month follow-up (P>.05. ADSTEP 117.53±148.40min/d; control 46.43 ±58.55min/d; d=0.63).
Conclusions:
ADSTEP prevents falls, reduces sitting, and may increase walking in PwMS.
Keywords: Accidental falls, Multiple sclerosis, Physical activity, Randomized controlled trial, Rehabilitation, Walking
Multiple sclerosis (MS) affects approximately 400,000 people in the United States and over 2.5 million people worldwide.1 Impaired walking and frequent falls are among the most ubiquitous symptoms in people with MS (PwMS).1–5 The most consistently reported risk factors for falls in PwMS are having progressive MS or having MS for longer, impaired balance, slower walking, and use of a mobility aid. Around 50% to 60% of PwMS fall over 3 months and 30% to 40% fall twice or more in this time frame.6–9 Falls and impaired walking reduce safety, independence, physical activity, and quality of life in PwMS.
Many PwMS use walking aids (eg, canes, crutches, walkers) to improve their walking safety, ability, and participation.10 Unfortunately, PwMS who use walking aids fall more often than those who do not,8,9 and they attribute many of their falls to the walking aid.11 This suggests that walking aids as currently used are not optimally effective and may even, at times, cause falls rather than prevent them.
Despite the physical and psychological benefits of physical activity,12–14 PwMS, particularly those who use walking aids, are less active than healthy adults15–17 and less active than current guidelines recommend.18 Those with progressive MS are the least active.17 Unfortunately, more physical activity can be associated with more falls, possibly because of increased standing and walking.19 There is a critical need for interventions that improve both safety and physical activity in PwMS who use walking aids.20,21
The associations between walking aid use, falls, and physical activity in PwMS are complex. Improper walking aid selection and fitting, coupled with lack of targeted training, are modifiable risk factors that likely contribute to these associations.8,9 Therefore, the primary investigator for this trial (MHC), a neurologist and physical therapist who treats patients with MS, and the treating physical therapist for this trial (EZ), who specializes in neurological rehabilitation, developed Assistive Device Selection, Training and Education Program (ADSTEP), a standardized multicomponent walking aid selection and training program. We know of no published guidelines or studies on walking aid programs in any patient population, therefore ADSTEP is based on our understanding of effective approaches for motor training and functional restoration in people with central nervous system injury practical within most health care systems in the United States.
ADSTEP consists of 6 weekly, 40-minute, 1-on-1 sessions with a physical therapist, consistent with standard physical therapy referrals and approval in the United States. The program starts with device selection and fitting. People often obtain their walking aids from a store, a friend or relative, based on availability, directto-consumer advertising, or information from untrained personnel, with no or very limited input from health care providers.22–24 Consequently, they are likely to have the wrong device and for the device to fit poorly, potential increasing the risk for falls. ADSTEP then proceeds with task-oriented gait training with the walking aid, adapted from Carr and Shepherd’s motor relearning program for stroke,25 which focuses on improving motor control and relearning daily activities within the context of functional tasks. The training involves repeated guided practice of the task in typical and progressively more challenging circumstances. This takes advantage of the fact that even when people with central nervous system disorders have cognitive and motor impairments, they can still learn motor tasks and improve with training.26–29 Task-oriented training has been shown to improve walking, mobility, and balance in people with various neurological conditions including MS.28,29
ADSTEP differs from usual medical care, in that a PwMS who uses a walking aid may or may not be referred to physical therapy. If they do receive physical therapy, there is little evidence to guide the number or duration of sessions, or whether the sessions should include strengthening, stretching, balance exercises, spasticity management, gait training, and/or other interventions. ADSTEP utilizes skills within the scope and practice of physical therapy but is consistently 6 40-minutes sessions all focused on walking aid selection, fitting, and task-oriented gait training.
To date, we are not aware of any published studies primarily evaluating the effects of a walking aid selection and training program on falls and physical activity in PwMS. We therefore performed a pilot, randomized controlled trial to compare the effects of ADSTEP to usual medical care on falls, physical activity (walking and sitting), timed mobility tests, and patient-reported outcomes in PwMS using a walking aid at baseline. We hypothesized that, compared to usual medical care, ADSTEP would prevent falls, increase physical activity, and improve timed mobility tests and patient-reported outcomes.
Methods
Study population
Participants were recruited from the outpatient MS clinic at the Veterans Affairs Portland Health Care System and the surrounding community. Eighty-four people were screened and 40 met inclusion criteria and enrolled. Participants were randomly allocated after baseline measures, in blocks of 4, to the 2 conditions by the study statistician (fig 1). All personnel involved in outcome assessments were blinded to allocation. The Veterans Affairs Portland Health Care System institutional review board approved the study. All participants signed informed consent prior to participation. This trial was registered on clinicaltrials.gov ().
Fig 1.
CONSORT diagram for the clinical investigation. *Inclusion criteria not met: no use of assistive device for walking (n=4), no falls in the past year (n=4), unconfirmed diagnosis of MS (n=1), received gait training within the last 3 years (n=1), making a change to medications (n=1), contraindications to MRI (n=6).
Inclusion criteria were: confirmed MS of any type, self-reported current intermittent or constant use of unilateral or bilateral assistance for walking, over age 18, able to walk at least 25 feet, no relapse in prior 30 days, and self-reported history of 1 or more falls in the previous year. Falling in the previous year was required because this is a strong predictor of future falls.30 Exclusion criteria were: reporting receiving more than 1 hour of walking aid training within the previous 3 years, and serious conditions that would preclude reliable study participation (eg, dementia, deafness, and blindness). Functional magnetic resonance imaging (MRI) was performed in a subset of participants (manuscript in preparation), therefore participants had to be right-handed, weigh under 350 pounds, and not have MRI contraindications.
Interventions
Active condition: ADSTEP
Participants randomized to ADSTEP were scheduled for the 6 sessions with a single physical therapist to begin within 2 weeks of baseline measures. Sessions were scheduled for the same day and time each week, although timing could be adjusted to fit the participant’s needs. ADSTEP took place in a small rehabilitation gym and nearby hallways and outdoor locations.
The first session started with observation and assessment of walking with the current walking aid(s), including safety, comfort, acceptability, and functionality for expected tasks and environments. Then the therapist offered trials with other devices, including canes, crutches, and a front-wheeled walker. The therapist and subject mutually agreed upon the appropriate aid (new or old) and the therapist adjusted this aid according to standard principles, including the elbow being flexed 20 to 30 degrees when holding the aid and, for crutches, the axillary pad being about 3” below the axilla.24,31,32 If the selected aid differed from the participant’s current aid, they were given the new aid to keep.
Task-oriented training with the walking aid followed. Tasks were progressed as specified in the ADSTEP manual and after achieving safe performance of prior tasks beginning with indoor walking on smooth even surfaces, such as vinyl, and progressing to carpet and transitions between surfaces. Turning was then added and progressed, from large open spaces to navigating obstacles such as doors and chairs, to turning in tight spaces. Stair climbing followed and was progressed from holding a handrail with the therapist managing the walking aid to the participant navigating the stairs while holding the walking aid themselves. Outdoor walking was then added and followed similar progression, from sidewalks to grass, gravel and inclines; turning wide then tight; climbing curbs and steps with and then without handrails. Dual-task activities, such as walking with head turns, carrying an object, counting aloud and while conversing, were added as participants mastered single task activities.
Control condition: usual medical care
Participants randomized to the control condition did not participate in ADSTEP during the study. They continued to receive usual medical care and completed the same outcome measures at the same time points as the active intervention group. They were allowed to receive any prescribed therapy and were allowed to change their walking aid and were offered ADSTEP following study participation.
Outcomes
Participant characteristics
Demographics, MS-related disability, and falls in the prior year were self-reported prior to randomization.33
Falls
Falls were counted prospectively during the intervention period and for the following 3 months using self-report calendars, the gold standard for assessing fall frequency.34,35 Each calendar page covered 1 month. The definition of a fall, “A fall is an unexpected event in which you come to rest on the ground, floor, or lower level,”36(p.1619) was explained at enrollment and was on each calendar page. Calendars were mailed back monthly. If a calendar was not received within 1 week of the due date, participants were contacted. Falls were analyzed categorically (no falls, 1 fall, or recurrent [>1] falls) and by total number.
Physical activity
Physical activity was assessed with the International Physical Activity Questionnaire short form (IPAQsf) at baseline, intervention completion, and 3 months later.37 The IPAQsf consists of 7 questions assessing physical activity and inactivity over the prior 7 days, including time spent sitting, time spent walking, and physical activity intensity. The IPAQsf has been used and validated in PwMS.12,38,39
Timed mobility performance
Timed mobility performance was measured at baseline, intervention completion, and 3 months later with the timed Up and Go (TUG),40 the timed 25-foot walk (T25W),41 the 2-minute walk test (2MWT),42 and the Four Square Step Test (FSST).43 These measures are timed with a stopwatch and have good reliability and validity in PwMS.44–47
Patient-reported outcomes
Patient reported outcomes (PROs) were evaluated with questionnaires at baseline, intervention completion, and 3 months later. Specifically, walking aid satisfaction was assessed with the questions related to device satisfaction on the Quebec User Evaluation of Satisfaction With Assistive Technologies (QUEST) 2.0.48 The 4 unused questions relate to device maintenance. The effect of MS on walking was assessed with the Multiple Sclerosis Walking Scale-12 (MSWS-12).49,50 Balance confidence was assessed with the Activities-Specific Balance Confidence Scale (ABC).6,51,52 The effect of MS on day-to-day life was assessed with the Multiple Sclerosis Impact Scale-29 (MSIS-29).53,54 These measures have good reliability and validity in PwMS and the MSWS-12, ABC and MSIS-29 are recommended outcome measures for exercise studies in MS.50
Statistical analyses
All outcome analyses were based on intent to treat. Means and standard deviations were calculated at each time point. Assumption of normality was evaluated using Q-Q plots and equality of variance was analyzed with Levene’s test. Welch’s unequal variance t-test was used for all variables with significant Levene’s test results. A 2-by-2 repeated measures general linear model was used to estimate the effect of ADSTEP. Group and time were the factors. Seven participants in the ADSTEP group and none in the control changed walking aids during this study (t =−3.20, P =.005). Therefore, a categorical variable of device change (YES/NO) was included as a covariate in the general linear models. Alpha was set a priori at P≤.05 for all tests. Post hoc analysis with Bonferroni correction was used to explore significant main effects and interactions. Cohen’s d effect sizes (d ) were calculated to compare outcomes between groups and were interpreted as weak (<0.50), moderate (0.50–0.79), or strong (≥0.80).55 Falls in the groups were compared categorically using chi-square tests and these results were used to derive number needed to treat (NNT). Those who did not fall were categorized as nonfallers. Those who fell once or more were categorized as fallers, and those who fell more than once were categorized as recurrent fallers. Statistical analyses were performed with SPSS version 23.a
Results
Participant characteristics
Forty participants were randomized, 20 to each group. Nineteen of the ADSTEP group completed all 6 ADSTEP sessions and 1 completed 5 sessions. All participants completed all outcome visits and all collected data were included in analyses.
Participants were well matched in their demographics, fall history, and outcome measures at baseline (tables 1, 2, and fig 2).
Table 1.
Baseline participant demographics and number of falls reported retrospectively for the previous year, by group assignment
| Characteristic | ADSTEP (n = 20) | Control (n = 20) |
|---|---|---|
| Age (y), mean ± SD | 56.0±9 | 54.8±1.4 |
| Sex, men/women | 6/1 | 7/1 |
| Race, African American/Caucasian | 1/1 | 3/1 |
| EDSS (self-report), median ± SE | 6.0±0 | 6.0±0 |
| Falls previous year, mean ± SD | 12.4±2.1 | 12.1±14 |
Table 2.
Timed mobility performance and patient-reported outcomes at baseline, intervention completion, and 3 months later
| Measure | Timepoint | Test | ADSTEP (n = 20) | Control (n = 20) | Cohen′s d |
|---|---|---|---|---|---|
| Timed mobility performance | Baseline | TUG (s) | 16.9±10.7 | 17.3±8.5 | 0.05 |
| T25WT (s) | 10.2±6.9 | 10.4±7.6 | 0.03 | ||
| 2MWT (min) | 94.1±35.9 | 95.2±33.8 | 0.01 | ||
| FSST (s) | 31.1±33.0 | 37.4±33.2 | 0.20 | ||
| Intervention completion | TUG (s) | 18.0±13.6 | 17.3±7.5 | 0.06 | |
| T25WT (s) | 10.0±7.9 | 9.2±3.9 | 0.13 | ||
| 2MWT (min) | 100.3±36.1 | 100.4± 35.0 | 0.00 | ||
| FSST (s) | 35.7±43.4 | 28.3±19.3 | 0.22 | ||
| 3 months later | TUG (s) | 19.4±18.6 | 17.0±7.5 | 0.18 | |
| T25WT (s) | 10.2±8.6 | 9.6±4.5 | 0.10 | ||
| 2MWT (min) | 97.5±39.3 | 99.2±35.1 | 0.05 | ||
| FSST (s) | 32.6±39 | 32.2±27.8 | 0.01 | ||
| Patient-reported outcomes | Baseline | QUEST 2.0 | 4.3±0.9 | 4.3±0.6 | 0.05 |
| MSWS-12 | 47.8±8.5 | 47.0±8.8 | 0.10 | ||
| MSIS-29 | 81.6±15.3 | 82.8±23.3 | 0.06 | ||
| ABC | 55.8±15.4 | 51.5±17.4 | 0.27 | ||
| Intervention completion | QUEST 2.0 | 4.7±0.3 | 4.4±0.6 | 0.70 | |
| MSWS-12 | 44.1±8.7 | 49.1±8.5 | 0.60 | ||
| MSIS-29 | 76.9±16.5 | 87.4±23.2 | 0.54 | ||
| ABC | 59.3±15.9 | 47.6±17.3 | 0.72 | ||
| 3 months later | QUEST 2.0 | 4.6±0.5 | 4.4±0.7 | 0.38 | |
| MSWS-12 | 48.5±6.5 | 49.7±7.7 | 0.17 | ||
| MSIS-29 | 79.7±17.3 | 86.9±25.3 | 0.34 | ||
| ABC | 57.6±16.0 | 50.0±15.8 | 0.49 |
NOTE. Values are mean ±SD or as otherwise indicated. None of the changes over time or differences between groups were statistically significant. Lower scores on the MSWS-12 and MSIS-29 are better. Higher scores on the ABC and QUEST 2.0 are better.
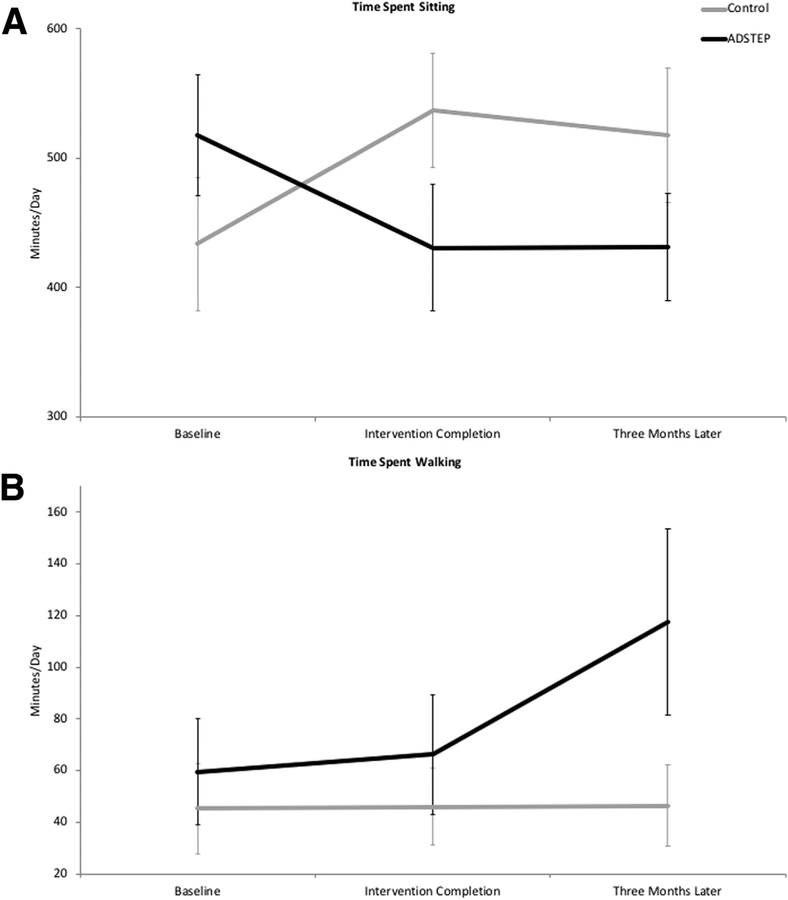
Fig 2.
Average amount of (A) time spent sitting and (B) time spent walking per day at baseline, intervention completion, and 3 months later, based on IPAQsf responses. Error bars represent standard deviation.
Falls
There was a significant association between group (ADSTEP vs control) and falling over the study period (table 3) with significantly fewer fallers in the ADSTEP group than in the control group (χ2=3.96, P<.05, NNT=3.3). There were also fewer recurrent fallers in the ADSTEP group than in the control group but this did not meet statistical significance (χ2=5.24, P=.07, NNT=5). There was no significant difference between groups in the mean total number of falls.
Table 3.
Fall status over the entire reporting period (intervention plus the following 3 months) for the ADSTEP group and the control group
| Characteristic | ADSTEP (n = 2O) | Control (n = 20) | Total |
|---|---|---|---|
| No fall (non-fallers) | 10 | 4 | 14 |
| 1 or more falls (fallers) | 10 | 16 | 26 |
| 2 or more falls (recurrent fallers) | 10 | 14 | 24 |
Physical activity
Based on IPAQsf responses, the ADSTEP group reported a significantly different change in average number of minutes/days spent sitting compared to the control group from baseline to intervention completion (F=11.16, P=.002. ADSTEP: reduced sitting by 87.00 ±194.89min/d; control: increased sitting by 103.50±142.21min/d; d=0.88) (fig 2A) and from baseline to the 3-month follow-up (F=9.25, P=.004. ADSTEP: reduced sitting by 75.79±171.57min/d; control: increased sitting by 84.50±149.23 min/d; d=0.79) (fig 2A). There were no significant differences in vigorous activity, moderate activity, or walking activity as captured by the IPAQsf between groups at any time point or in changes over time between groups (ie, interaction effects). The ADSTEP group also reported more time spent walking than the control group at the 3-month follow-up, with a moderate effect size but this difference did not meet statistical significance (ADSTEP: 117.53±148.40min/d; control: 46.43±58.55min/d; P>.05, d=0.63) (fig 2B).
Timed mobility performance
There were no significant differences between groups at any time point or in changes over time between groups (ie, interaction effects) for any of the timed mobility tests including the TUG, the T25W, the 2MWT, and the FSST, and all effect sizes were weak (see table 3).
PROs
There were no significant differences between groups at any time point or in changes over time between groups (ie, interaction effects) for the QUEST, the MSWS-12, the ABC, or the MSIS-29. However, all of these outcomes showed moderate effect sizes for improvements in the ADSTEP group compared to the control at intervention completion, with the strongest effect for walking aid satisfaction (QUEST) and balance confidence (ABC) (d for QUEST=0.70, ABC=0.72, MSWS-12=0.60, MSIS-29=0.54). The effect size for the ABC also approached moderate at the 3-month follow-up (d=0.49) (see table 2).
Discussion
This pilot study is the first to provide evidence that the multicomponent walking aid program, ADSTEP (consisting of walking aid selection, fitting, and task-oriented training) prevents falls and improves physical activity behavior, including less sitting time and possibly more walking time, compared to usual medical care. Statistically significantly fewer people in the training group fell and, based on statistically significant interactions with moderate to strong effect sizes, the ADSTEP group reduced the amount of time they spent sitting while the control group increased the amount of time they spent sitting. In addition, although not statistically significant, based on a moderate effect size, the ADSTEP group also likely spent more time walking.
Previous studies of fall prevention interventions in MS have primarily examined the effects of exercise and/or education.21,56–62 Exercise generally improves strength and balance, and education increases fall prevention knowledge but neither consistently reduces fall risk or, more importantly, prevents falls.6,21,56–58,60,61 A 2015 systematic review of studies of interventions to reduce falls and improve balance in adults with MS surprisingly found that few studies specifically examined the effect on future falls and, that the strength and balance improvements may not be sufficient to affect falls.58 In contrast to earlier studies, ADSTEP focuses on improving walking with a walking aid, a single strong modifiable risk factor for falls in PwMS.8,63 Specifically and exclusively addressing walking with a walking aid likely helped achieve the task-specific outcomes of safer walking and less sitting, seen in this trial.
Although the effect of ADSTEP on other physical activity outcomes did not meet statistical significance, this study was not powered to detect significant effects on these outcomes. Based on the observed effect sizes, post hoc power calculations indicate a study with 120 PwMS would yield statistically significant effects on falls as well as time spent walking and sitting. In addition, physical activity measurement was limited to self-report when objective measurement of free-living physical activity that could be obtained with body-worn accelerometers would be more accurate and thus more likely to yield statistically significant findings.64 It is also important that in this trial, falling and sitting were reduced and walking possibly increased while in other studies, more physical activity, with more exposure to fall hazards, has been associated with more falls.19
In contrast to the effect of ADSTEP on falls and sitting time, ADSTEP did not appear to affect timed mobility or PROs. We believe that mobility was not accelerated because, although being able to walk faster is associated with improved functional outcomes, faster walking can also come at the cost of decreased safety.65–67 Therefore, ADSTEP emphasized walking safety and ability but not speed, yielding effects consistent with this emphasis. Studies of people receiving the medication dalfampridine, an intervention that increases gait speed, actually reported more falls in the intervention group, which again, has been attributed to increased exposure.68 Our study did not include a timed dual task measure, such as the dual task TUG.69 This may have been more likely to show acceleration because ADSTEP includes dual task training and because fall risk is strongly correlated with dual task speed in PwMS and in other populations.70,71 The lack of significant effects on the PROs may also be attributed to the specificity of the effect of ADSTEP, and the small sample size.
This study has a number of strengths. It was a randomized controlled trial with objective outcome assessments performed by assessors blinded to allocation with excellent adherence and minimal missing data. Falls were prospectively assessed, the current gold standard, rather than retrospectively recalled or a fall proxy of balance or fall risk.58,59 The clinical effect of this outcome alone could be substantial, with a NNT of 3.3 to prevent one person falling and 5 to prevent recurrent falls, and the possibility that ADSTEP may also increase physical activity.
Study limitations
This study also has several limitations. The sample was small, limiting power to draw definitive conclusions about many outcomes. Potential participants were excluded if they reported receiving more than 1 hour of walking aid training within the previous 3 years but were not excluded for having received other forms of physical therapy, which may have confounded our results. Physical activity was assessed with a self-report measure, the IPAQsf, rather than an objective measure such as a body-worn accelerometer.64,72 Furthermore, we did not capture the effect of this program on functional activities as could be captured with the functional mobility assessment questionnaire.73 In addition, although a multicomponent multisession program can address a range of important issues, combining components in 1 program prevents evaluation of the individual or incremental contributions of components or sessions. The control condition did not control for 1-on-1 contact, and this study was carried out at a single site with a single physical therapist providing the intervention, limiting generalizability.
Conclusions
This pilot study suggests that, compared to usual medical care, a multicomponent walking aid program, ADSTEP (consisting of walking aid selection, fitting, and task-oriented training), is associated with preventing falls, reducing sitting time, and possibly increasing walking time in PwMS. This study supports the need for a fully powered, multisite trial to definitively determine the effect of ADSTEP on falls and physical activity in PwMS.
Acknowledgments
This work was supported by a Small Projects in Rehabilitation award no. 5I21RX001918–02 from the United States Department of Veterans Affairs Rehabilitation Research and Development Service. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States government.
List of abbreviations:
- 2MWT
2-minute walk test
- ABC
Activities-Specific Balance Confidence Scale
- ADSTEP
Assistive Device Selection, Training and Education Program
- FSST
Four Square Step Test
- IPAQsf
International Physical Activity Questionnaire, short form
- MRI
magnetic resonance imaging
- MS
multiple sclerosis
- MSIS-29
Multiple Sclerosis Impact Scale-29
- MSWS-12
Multiple Sclerosis Walking Scale-12
- NNT
number needed to treat
- PRO
patient-reported outcome
- PwMS
people with multiple sclerosis
- QUEST
Quebec User Evaluation of Satisfaction With Assistive Technologies
- T25W
timed 25-foot walk
- TUG
timed Up and Go
Footnotes
SPSS, version 23; IBM.
Clinical Trial Registration No.: .
Disclosures: none.
References
- 1.Zwibel HL. Contribution of impaired mobility and general symptoms to the burden of multiple sclerosis. Adv Ther 2009;26:1043–57. [DOI] [PubMed] [Google Scholar]
- 2.Sutliff MH. Contribution of impaired mobility to patient burden in multiple sclerosis. Curr Med Res Opin 2010;26:109–19. [DOI] [PubMed] [Google Scholar]
- 3.Larocca NG. Impact of walking impairment in multiple sclerosis: perspectives of patients and care partners. Patient 2011;4:189–201. [DOI] [PubMed] [Google Scholar]
- 4.Cameron MH, Poel AJ, Haselkorn JK, Linke A, Bourdette D. Falls requiring medical attention among veterans with multiple sclerosis: a cohort study. J Rehabil Res Dev 2011;48:13–20. [DOI] [PubMed] [Google Scholar]
- 5.Matsuda PN, Shumway-Cook A, Bamer AM, Johnson SL, Amtmann D, Kraft GH. Falls in multiple sclerosis. PM R 2011;3: 624–32. [DOI] [PubMed] [Google Scholar]
- 6.Nilsagard Y, Gunn H, Freeman J, et al. Falls in people with MS–an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Mult Scler 2015;21:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cameron MH, Asano M, Bourdette D, Finlayson ML. People with multiple sclerosis use many fall prevention strategies but still fall frequently. Arch Phys Med Rehabil 2013;94:1562–6. [DOI] [PubMed] [Google Scholar]
- 8.Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys Ther 2013;93:504–13. [DOI] [PubMed] [Google Scholar]
- 9.Gianni C, Prosperini L, Jonsdottir J, Cattaneo D. A systematic review of factors associated with accidental falls in people with multiple sclerosis: a meta-analytic approach. Clin Rehabil 2014;28:704–16. [DOI] [PubMed] [Google Scholar]
- 10.Finlayson M, Guglielmello L, Liefer K. Describing and predicting the possession of assistive devices among persons with multiple sclerosis. Am J Occup Ther 2001;55:545–51. [DOI] [PubMed] [Google Scholar]
- 11.Peterson EW, Ben Ari E, Asano M, Finlayson ML. Fall attributions among middle-aged and older adults with multiple sclerosis. Arch Phys Med Rehabil 2013;94:890–5. [DOI] [PubMed] [Google Scholar]
- 12.Motl RW, McAuley E, Wynn D, Sandroff B, Suh Y. Physical activity, self-efficacy, and health-related quality of life in persons with multiple sclerosis: analysis of associations between individual-level changes over one year. Qual Life Res 2013;22:253–61. [DOI] [PubMed] [Google Scholar]
- 13.Motl RW, McAuley E, Wynn D, Vollmer T. Lifestyle physical activity and walking impairment over time in relapsing-remitting multiple sclerosis: results from a panel study. Am J Phys Med Rehabil 2011;90:372–9. [DOI] [PubMed] [Google Scholar]
- 14.Stroud NM, Minahan CL. The impact of regular physical activity on fatigue, depression and quality of life in persons with multiple sclerosis. Health Qual Life Outcomes 2009;7:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kinnett-Hopkins D, Adamson B, Rougeau K, Motl RW. People with MS are less physically active than healthy controls but as active as those with other chronic diseases: an updated meta-analysis. Mult Scler Relat Disord 2017;13:38–43. [DOI] [PubMed] [Google Scholar]
- 16.Klaren RE, Motl RW, Dlugonski D, Sandroff BM, Pilutti LA. Objectively quantified physical activity in persons with multiple sclerosis. Arch Phys Med Rehabil 2013;94:2342–8. [DOI] [PubMed] [Google Scholar]
- 17.Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Mult Scler 2005;11:459–63. [DOI] [PubMed] [Google Scholar]
- 18.Latimer-Cheung AE, Martin Ginis KA, Hicks AL, et al. Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Arch Phys Med Rehabil 2013;94:1829–36. [DOI] [PubMed] [Google Scholar]
- 19.Graafmans WC, Lips P, Wijlhuizen GJ, Pluijm SM, Bouter LM. Daily physical activity and the use of a walking aid in relation to falls in elderly people in a residential care setting. Z Gerontol Geriatr 2003;36:23–8. [DOI] [PubMed] [Google Scholar]
- 20.Plow MA, Resnik L, Allen SM. Exploring physical activity behaviour of persons with multiple sclerosis: a qualitative pilot study. Disabil Rehabil 2009;31:1652–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coote S, Hogan N, Franklin S. Falls in people with multiple sclerosis who use a walking aid: prevalence, factors, and effect of strength and balance interventions. Arch Phys Med Rehabil 2013;94:616–21. [DOI] [PubMed] [Google Scholar]
- 22.Scherer MJ, Sax C, Vanbiervliet A, Cushman LA, Scherer JV. Predictors of assistive technology use: the importance of personal and psychosocial factors. Disabil Rehabil 2005;27:1321–31. [DOI] [PubMed] [Google Scholar]
- 23.Scherer MJ, Craddock G, Mackeogh T. The relationship of personal factors and subjective well-being to the use of assistive technology devices. Disabil Rehabil 2011;33:811–7. [DOI] [PubMed] [Google Scholar]
- 24.Sadowski CA, Jones CA. Ambulatory assistive devices: how to appropriately measure and safely use canes, crutches and walkers. Pharmacy Practice 2014;1:24–31. [Google Scholar]
- 25.Carr JH, Shepherd RB. A motor relearning programme for stroke. London: Heinemann Medical; 1982. [Google Scholar]
- 26.Tomassini V, Matthews PM, Thompson AJ, et al. Neuroplasticity and functional recovery in multiple sclerosis. Nat Rev Neurol 2012;8: 635–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tomassini V, Johansen-Berg H, Leonardi L, et al. Preservation of motor skill learning in patients with multiple sclerosis. Mult Scler 2011;17:103–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lord SE, Wade DT, Halligan PW. A comparison of two physiotherapy treatment approaches to improve walking in multiple sclerosis: a pilot randomized controlled study. Clin Rehabil 1998; 12:477–86. [DOI] [PubMed] [Google Scholar]
- 29.Paltamaa J, Sjogren T, Peurala SH, Heinonen A. Effects of physiotherapy interventions on balance in multiple sclerosis: a systematic review and meta-analysis of randomized controlled trials. J Rehabil Med 2012;44:811–23. [DOI] [PubMed] [Google Scholar]
- 30.Cameron MH, Thielman E, Mazumder R, Bourdette D. Predicting falls in people with multiple sclerosis: fall history is as accurate as more complex measures. Mult Scler Int 2013;2013:496325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson PH. Physical therapist’s clinical companion. Springhouse, PA: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 32.Bradley SM, Hernandez CR. Geriatric assistive devices. Am Fam Physician 2011;84:405–11. [PubMed] [Google Scholar]
- 33.Bowen J, Gibbons L, Gianas A, Kraft GH. Self-administered expanded disability status scale with functional system scores correlates well with a physician-administered test. Mult Scler 2001;7: 201–6. [DOI] [PubMed] [Google Scholar]
- 34.Hauer K, Becker C, Lindemann U, Beyer N. Effectiveness of physical training on motor performance and fall prevention in cognitively impaired older persons: a systematic review. Am J Phys Med Rehabil 2006;85:847–57. [DOI] [PubMed] [Google Scholar]
- 35.Coote S, Sosnoff JJ, Gunn H. Fall incidence as the primary outcome in multiple sclerosis falls-prevention trials: recommendation from the international MS falls prevention research network. Int J MS Care 2014;16:178–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C; Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc 2005; 53:1618–22. [DOI] [PubMed] [Google Scholar]
- 37.Bassett DR. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1396. [DOI] [PubMed] [Google Scholar]
- 38.Gosney JL, Scott JA, Snook EM, Motl RW. Physical activity and multiple sclerosis: validity of self-report and objective measures. Fam Community Health 2007;30:144–50. [DOI] [PubMed] [Google Scholar]
- 39.Snook EM, Motl RW, Gliottoni RC. The effect of walking mobility on the measurement of physical activity using accelerometry in multiple sclerosis. Clin Rehabil 2009;23:248–58. [DOI] [PubMed] [Google Scholar]
- 40.Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “getup and go” test. Arch Phys Med Rehabil 1986;67:387–9. [PubMed] [Google Scholar]
- 41.Cutter GR, Baier ML, Rudick RA, et al. Development of a multiple sclerosis functional composite as a clinical trial outcome measure. Brain 1999;122:871–82. [DOI] [PubMed] [Google Scholar]
- 42.Gijbels D, Eijnde BO, Feys P. Comparison of the 2- and 6-minute walk test in multiple sclerosis. Mult Scler 2011;17:1269–72. [DOI] [PubMed] [Google Scholar]
- 43.Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 2002;83:1566–71. [DOI] [PubMed] [Google Scholar]
- 44.Sebastiao E, Sandroff BM, Learmonth YC, Motl RW. Validity of the timed Up and Go test as a measure of functional mobility in persons with multiple sclerosis. Arch Phys Med Rehabil 2016;97:1072–7. [DOI] [PubMed] [Google Scholar]
- 45.Goldman MD, Motl RW, Scagnelli J, Pula JH, Sosnoff JJ, Cadavid D. Clinically meaningful performance benchmarks in MS: timed 25-foot walk and the real world. Neurology 2013;81:1856–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wagner JM, Norris RA, Van Dillen LR, Thomas FP, Naismith RT. Four Square Step Test in ambulant persons with multiple sclerosis: validity, reliability, and responsiveness. Int J Rehabil Res 2013;36: 253–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scalzitti DA, Harwood KJ, Maring JR, Leach SJ, Ruckert EA, Costello E. Validation of the 2-minute walk test with the 6-minute walk test and other functional measures in persons with multiple sclerosis. Int J MS Care; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Demers L, Monette M, Lapierre Y, Arnold DL, Wolfson C. Reliability, validity, and applicability of the Quebec User Evaluation of Satisfaction With Assistive Technology (QUEST 2.0) for adults with multiple sclerosis. Disabil Rehabil 2002;24:21–30. [DOI] [PubMed] [Google Scholar]
- 49.Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ. Measuring the impact of MS on walking ability: the 12-Item MS Walking Scale (MSWS-12). Neurology 2003;60:31–6. [DOI] [PubMed] [Google Scholar]
- 50.Paul L, Coote S, Crosbie J, et al. Core outcome measures for exercise studies in people with multiple sclerosis: recommendations from a multidisciplinary consensus meeting. Mult Scler 2014;20:1641–50. [DOI] [PubMed] [Google Scholar]
- 51.Powell LE, Myers AM. The Activities-Specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci 1995;50A:M28–34. [DOI] [PubMed] [Google Scholar]
- 52.Nilsagard Y, Carling A, Forsberg A. Activities-specific balance confidence in people with multiple sclerosis. Mult Scler Int 2012; 2012:613925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hobart J, Lamping D, Fitzpatrick R, Riazi A, Thompson A. The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain 2001;124:962–73. [DOI] [PubMed] [Google Scholar]
- 54.Hoogervorst EL, Zwemmer JN, Jelles B, Polman CH, Uitdehaag BM. Multiple Sclerosis Impact Scale (MSIS-29): relation to established measures of impairment and disability. Mult Scler 2004;10:569–74. [DOI] [PubMed] [Google Scholar]
- 55.Cohen J Statistical power analysis for the behavioral sciences, rev. ed. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1977. [Google Scholar]
- 56.Hugos CL, Frankel D, Tompkins SA, Cameron M. Community delivery of a comprehensive fall-prevention program in people with multiple sclerosis: a retrospective observational study. Int J MS Care 2016;18:42–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Miake-Lye IM, Hempel S, Ganz DA, Shekelle PG. Inpatient fall prevention programs as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:390–6. [DOI] [PubMed] [Google Scholar]
- 58.Gunn H, Markevics S, Haas B, Marsden J, Freeman J. Systematic review: the effectiveness of interventions to reduce falls and improve balance in adults with multiple sclerosis. Arch Phys Med Rehabil 2015;96:1898–912. [DOI] [PubMed] [Google Scholar]
- 59.Sosnoff JJ, Sung J. Reducing falls and improving mobility in multiple sclerosis. Expert Rev Neurother 2015;15:655–66. [DOI] [PubMed] [Google Scholar]
- 60.Nilsagard YE, von Koch LK, Nilsson M, Forsberg AS. Balance exercise program reduced falls in people with multiple sclerosis: a single-group, pretest-posttest trial. Arch Phys Med Rehabil 2014;95: 2428–34. [DOI] [PubMed] [Google Scholar]
- 61.Sosnoff JJ, Finlayson M, McAuley E, Morrison S, Motl RW. Homebased exercise program and fall-risk reduction in older adults with multiple sclerosis: phase 1 randomized controlled trial. Clin Rehabil 2014;28:254–63. [DOI] [PubMed] [Google Scholar]
- 62.Kalron A, Fonkatz I, Frid L, Baransi H, Achiron A. The effect of balance training on postural control in people with multiple sclerosis using the CAREN virtual reality system: a pilot randomized controlled trial. J Neuroeng Rehabil 2016;13:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Finlayson ML, Peterson EW, Asano M. A cross-sectional study examining multiple mobility device use and fall status among middle-aged and older adults with multiple sclerosis. Disabil Rehabil Assist Technol 2014;9:12–6. [DOI] [PubMed] [Google Scholar]
- 64.Motl RW, Sandroff BM. Objective monitoring of physical activity behavior in multiple sclerosis. Phys Ther Rev 2010;15:204–11. [Google Scholar]
- 65.Callisaya ML, Blizzard L, McGinley JL, Srikanth VK. Risk of falls in older people during fast-walking—the TASCOG study. Gait Posture 2012;36:510–5. [DOI] [PubMed] [Google Scholar]
- 66.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc 1997;45:313–20. [DOI] [PubMed] [Google Scholar]
- 67.Sosnoff JJ, Socie MJ, Boes MK, et al. Mobility, balance and falls in persons with multiple sclerosis. PLoS One 2011;6:e28021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Goodman AD, Brown TR, Cohen JA, et al. Dose comparison trial of sustained-release fampridine in multiple sclerosis. Neurology 2008; 71:1134–41. [DOI] [PubMed] [Google Scholar]
- 69.Wajda DA, Sosnoff JJ. Cognitive-motor interference in multiple sclerosis: a systematic review of evidence, correlates, and consequences. Biomed Res Int 2015;2015:720856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wajda DA, Motl RW, Sosnoff JJ. Dual task cost of walking is related to fall risk in persons with multiple sclerosis. J Neurol Sci 2013;335:160–3. [DOI] [PubMed] [Google Scholar]
- 71.Hofheinz M, Mibs M. The prognostic validity of the timed up and go test with a dual task for predicting the risk of falls in the elderly. Gerontol Geriatr Med 2016;2 2333721416637798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Block VJ, Lizee A, Crabtree-Hartman E, et al. Continuous daily assessment of multiple sclerosis disability using remote step count monitoring. J Neurol 2017;264:316–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kumar A, Schmeler MR, Karmarkar AM, et al. Test-retest reliability of the functional mobility assessment (FMA): a pilot study. Disabil Rehabil Assist Technol 2013;8:213–9. [DOI] [PubMed] [Google Scholar]