Abstract
An excessive posterior tibial slope has been identified as a potential risk factor for anterior cruciate ligament tears. Anterior closing-wedge osteotomy decreases the posterior slope and can eliminate this risk factor in patients with recurrent instability and greater than 12° posterior slope. We will describe an anterior closing-wedge osteotomy technique performed at the tibial tubercle (TT), in which the TT is not detached to preserve the extensor mechanism attachment. A vertical cut is performed in the sagittal plane just posterior to the TT, leaving a distal cortical hinge. Two proximal parallel K-wires and 2 distal parallel K-wires convergent to the proximal ones are inserted from the anterior cortex on both sides of the tubercle toward the tibial posterior cortex at the posterior cruciate ligament's tibial insertion. Proximal and distal cuts are performed to remove the bone wedge. Reduction is achieved by gentle knee extension. Fixation is completed with 2 staples placed medially and laterally to the TT.
Introduction
An excessive posterior tibial slope (PTS) has been associated with increased anterior translation, potentially leading to greater strains in the anterior cruciate ligament (ACL) and greater risk of ACL injury.1, 2 Biomechanical and imaging studies have confirmed that the greater the slope, the greater the in situ forces in the ACL, thereby increasing 5-fold the odds of further ACL injury in patients with a PTS greater than 12°.3, 4, 5
This article presents an osteotomy for tibial slope correction in which the anterior wedge is removed at the level of the tibial tubercle (TT), without fully detaching the tubercle from the anterior tibial cortex; 2 staples are used for fixation (Video 1). This technique can be used during ACL re-revision for slope correction, solely addressing the increased lateral tibial slope and preserving the varus/valgus alignment of the tibia.
Surgical Technique
Indications
Anterior closing-wedge osteotomy should be considered in patients with a PTS greater than 12° who have recurrent instability after 2 or more failed ACL reconstructions.6, 7 Contraindications include severe leg misalignment, e.g., varus or valgus >10° or knee hyperextension (>10°) and grade IV osteoarthritis according to Kellgren and Lawrence.
Preoperative Planning
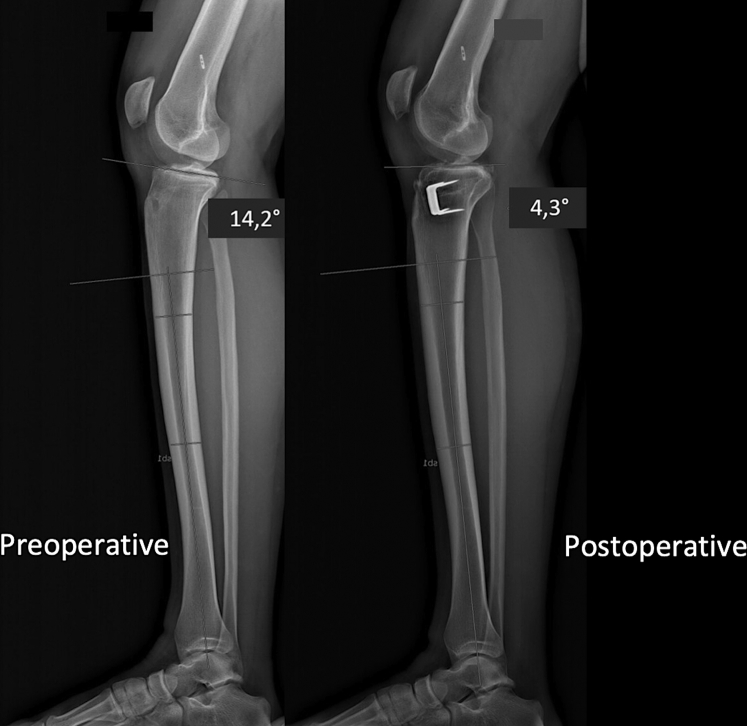
Patients should have anteroposterior and lateral weight-bearing views and Schuss views taken of their knee. The tibial slope is determined using a lateral view of the knee under fluoroscopy. It is calculated as the angle between the tangent to the medial tibial plateau and the lateral mechanical axis of the leg. The correction aims to reduce the PTS to <10° (Fig 1). The anterior bony segment is resected to obtain the desired surgical correction, considering that 1 mm of anterior resection leads to 1° of tibial slope correction. A slope correction of 6° to 10° is generally planned for.
Fig 1.
Preoperative and postoperative radiographic lateral views of the right knee. The 14.2° preoperative posterior tibial slope has been corrected to 4.3° postoperatively.
Patient Setup
The procedure can be performed with general, spinal, or regional anesthesia. The patient is placed supine on the operating table with a tourniquet placed high on the thigh. A lateral post at the level of the tourniquet maintains the leg position in the frontal plane. A distal support placed on the table keeps the knee in 90° flexion, while allowing full range of motion when needed. The fluoroscopy unit is tested, and the knee is positioned to ensure it is stable when taking a true lateral intraoperative image.
Surgical Technique
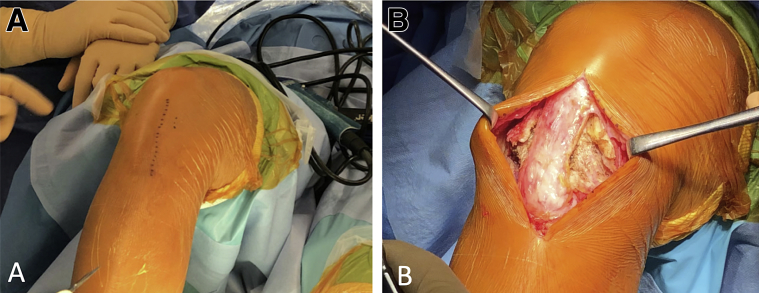
An anterior longitudinal incision centered on the TT is made, exposing the patellar tendon insertion. Medial dissection is performed, and the deep medial collateral ligament is detached up to its posterior portion. Dissection is then performed on the lateral side of the TT, and the lateral extensor muscles are detached from the intended lateral osteotomy site (Fig 2).
Fig 2.
Right knee. (A) Skin landmarks for the anterior longitudinal incision centered on the tibial tubercle. (B) Medial and lateral dissection is performed along the patellar tendon's medial and lateral borders.
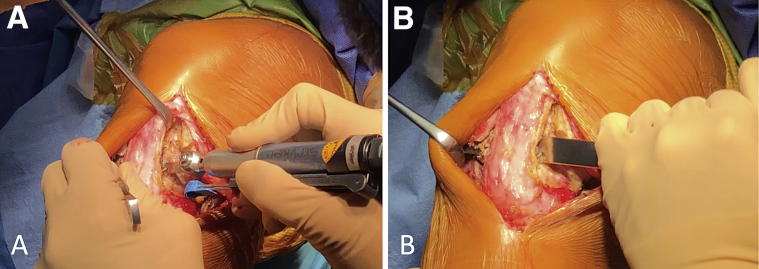
Hohmann retractors on both sides of the tibia are used to maintain the exposure. The osteotomy starts 1 cm below the patellar tendon insertion. The first vertical cut is made just posterior to the TT in the sagittal plane, preserving the TT's distal insertion (Fig 3). This allows the osteotomy to be carried out without detaching the extensor mechanism.
Fig 3.
Right knee. The vertical cut of the tibial tubercle is performed in the sagittal plane from proximal to distal. (A) The vertical cut is started with an oscillating saw and (B) carefully completed with an osteotome to preserve the distal cortical hinge.
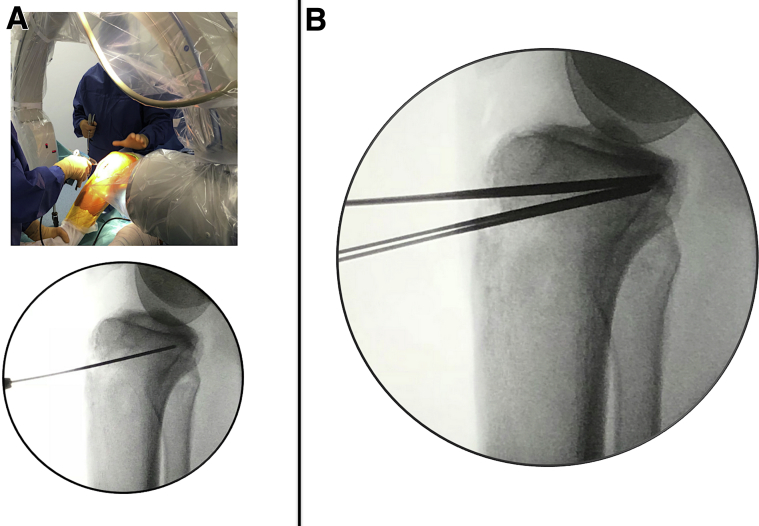
Two parallel K-wires are inserted under fluoroscopy control from either side of the patellar tendon at the TT level toward the posterior tibial cortex, aiming for the insertion site of the posterior cruciate ligament. Then, 2 other parallel K-wires are inserted distal to the first ones at a distance corresponding to the desired correction and in a convergent direction toward the posterior cruciate ligament's tibial insertion (Fig 4).
Fig 4.
Right knee. (A) Parallel K-wires are inserted under fluoroscopy control toward the posterior cortex. (B) Two proximal K-wires and 2 distal ones are inserted from either side of the patellar tendon in a convergent direction toward the posterior cruciate ligament's tibial insertion.
The superior and inferior cuts are then started with an oscillating saw guided by the proximal and distal K-wires. The osteotomy is finished with an osteotome. Both cuts should preserve the posterior cortex, as the bony bridge is critical to protecting the popliteal structures and limits the risk of secondary displacement or non-union. During this last step, we recommend marking the length of the osteotomy on the osteotome and verifying it using fluoroscopy to preserve a posterior bony hinge.
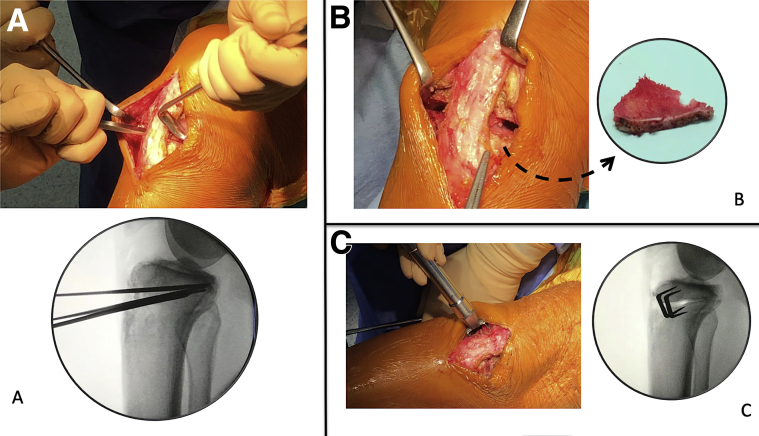
The anterior bony wedge is resected to obtain the desired surgical correction and achieve a PTS between 4° and 10°. After the bone wedge is removed, the resected surfaces are reduced by gentle knee extension. Fixation is completed with 2 staples positioned medially and laterally to the TT (Fig 5).
Fig 5.
Right knee. (A) The osteotomy is carefully completed with an osteotome under fluoroscopy control to preserve a posterior bony hinge. (B) Fixation is performed in full extension with staples positioned medially and laterally. (C) After staple fixation, the staple placement and posterior bony hinge are checked with fluoroscopy.
Rehabilitation
After surgery, progressive weight bearing is allowed, and passive and active extension exercises are done as tolerated by the patient. The main goals are to reduce knee swelling, regain control over the quadriceps muscles, and recover the range of motion. A gradual return to sports activities is allowed at 5 months for nonpivoting sports; at 9 months for pivoting, noncontact sports; and at 1 year for pivoting, contact sports.
Discussion
We have described a technique for anterior closing-wedge tibial slope correction for re-revision ACL surgery that preserves the TT and allows subsequent ACL reconstruction. The success of second revision ACL reconstruction requires careful analysis of the causes of the previous failures. The role of intrinsic factors (PTS and intercondylar notch) should not be underestimated. PTS greater than 12° increases the risk for ACL reconstruction failure and for contralateral ACL rupture. Correction of excessive PTS (>12°) should be considered during ACL reconstruction revision, especially in cases with previous reconstruction failures.6, 7 Techniques for slope correction involve closing-wedge osteotomy, either proximal or distal to the TT,5, 8 but there is no consensus regarding its indications and outcomes.
Our technique provides a safe and reproducible method for tibial slope correction. In contrast to other techniques, we performed a vertical cut behind the TT to allow us to perform the osteotomy in the tibial epiphysis at the level of the tubercle, while preserving the extensor mechanism. The osteotomy preserves the overall coronal alignment of the knee, as the proximal cut is parallel to the joint line in the coronal plane. As ACL reconstruction could be performed simultaneously, the fixation with 2 metal staples on either side of the TT leaves the central tibial epiphysis free of any metal devices, thereby allowing standard ACL tibial tunnel placement.
There are only 2 recently published studies6, 7 reporting the outcomes of anterior closing-wedge osteotomy. Both studies are retrospective and included only 5 and 9 patients, respectively. Both describe the results of osteotomy with concomitant ACL reconstruction. The threshold for slope correction was 12° in re-revision ACL surgery and the mean correction was 5°. Clinical improvement was apparent based on the Lysholm and International Knee Documentation Committee scores. Large patient samples and longer follow-up are needed to validate these early results.
Proximal anterior tibial closing-wedge osteotomy is a technically demanding procedure, associated with significant risks and potential complications. The most worrisome is damage to the neurovascular popliteal bundle, which can be avoided by careful placement of the guidewires and osteotomes under fluoroscopy control. In summary, this technique is used to perform an osteotomy at the level of the TT and generates a low-angle osteotomy line without needing to detach the tubercle. Contraindications, pearls, advantages, disadvantages, and potential risks are listed in Table 1.
Table 1.
Contraindications, Pearls, Advantages, Disadvantages, and Potential Risks
| Contraindications |
| Severe misalignment of the limb (i.e., >10° varus valgus) |
| Hyperextension of the knee (>10°) |
| Grade IV osteoarthritis according to Kellgren and Lawrence classification |
| Pearls |
| Medial and lateral dissection allows good soft-tissue closure around osteotomy site. |
| Vertical cut on TT oriented distally along the tibia leaves a cortical distal hinge. |
| Marking the osteotomy length on the osteotome and verifying it with fluoroscopy helps to preserve a posterior bony hinge. |
| Complete the bone resection before attempting to reduce the osteotomy. |
| Close the osteotomy by gentle knee extension to avoid fracturing the posterior cortex. |
| Advantages |
| Safe and reproducible method for tibial slope correction |
| Vertical cut in the TT preserves the extensor mechanism without distal detachment and allows accurate positioning of the osteotomy at the appropriate level. |
| Osteotomy is located in the epiphysis with a low angle for better healing and lower risk of non-union. |
| Using staples keeps the central tibial epiphysis free of hardware, allowing for standard tibial tunnel placement during ACL reconstruction. |
| Potential risks and disadvantages |
| Damage to the popliteal vessels and nerves |
| Modification of patellar height |
| Non-union |
| TT fracture |
| Does not allow varus or valgus correction |
| Potential for overcorrection or undercorrection |
ACL, anterior cruciate ligament; TT, tibial tubercle.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.S-C. is a paid consultant and receive royalties from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Technique for anterior closing-wedge osteotomy for slope correction. The patient is placed in a supine position with a lateral post just proximal to the right knee, at the level of the padded tourniquet; a foot roll is used to maintain 90° of knee flexion. The osteotomy is performed at the level of the tibial tubercle (TT), without detaching the extensor mechanism. A vertical cut is performed in the sagittal plane just posterior to the TT. Two proximal parallel K-wires and 2 distal parallel K-wires convergent to the proximal ones are inserted from the anterior cortex at the TT level toward the tibial posterior cortex at the level of the posterior cruciate ligament’s tibial insertion. Proximal and distal convergent cuts are made to remove the bone wedge; reduction is achieved by gentle knee extension. Fixation is completed with 2 staples positioned medially and laterally to the TT.
References
- 1.Feucht M.J., Mauro C.S., Brucker P.U., Imhoff A.B., Hinterwimmer S. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21:134–145. doi: 10.1007/s00167-012-1941-6. [DOI] [PubMed] [Google Scholar]
- 2.Brandon M.L., Haynes P.T., Bonamo J.R., Flynn M.I., Barrett G.R., Sherman M.F. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22:894–899. doi: 10.1016/j.arthro.2006.04.098. [DOI] [PubMed] [Google Scholar]
- 3.Lee C.C., Youm Y.S., Cho S.D. Does posterior tibial slope affect graft rupture following ACL reconstruction? Arthroscopy. 2018;34:2152–2155. doi: 10.1016/j.arthro.2018.01.058. [DOI] [PubMed] [Google Scholar]
- 4.Giffin J.R., Vogrin T.M., Zantop T., Woo S.L., Harner C.D. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 5.Sonnery-Cottet B., Archbold P., Cucurulo T. The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. J Bone Joint Surg Br. 2011;93:1475–1478. doi: 10.1302/0301-620X.93B11.26905. [DOI] [PubMed] [Google Scholar]
- 6.Dejour D., Saffarini M., Demey G., Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:2846–2852. doi: 10.1007/s00167-015-3758-6. [DOI] [PubMed] [Google Scholar]
- 7.Sonnery-Cottet B., Mogos S., Thaunat M. Proximal Tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:1873–1880. doi: 10.1177/0363546514534938. [DOI] [PubMed] [Google Scholar]
- 8.Hees T., Petersen W. Anterior closing-wedge osteotomy for posterior slope correction. Arthrosc Tech. 2018;7:e1079–e1087. doi: 10.1016/j.eats.2018.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for anterior closing-wedge osteotomy for slope correction. The patient is placed in a supine position with a lateral post just proximal to the right knee, at the level of the padded tourniquet; a foot roll is used to maintain 90° of knee flexion. The osteotomy is performed at the level of the tibial tubercle (TT), without detaching the extensor mechanism. A vertical cut is performed in the sagittal plane just posterior to the TT. Two proximal parallel K-wires and 2 distal parallel K-wires convergent to the proximal ones are inserted from the anterior cortex at the TT level toward the tibial posterior cortex at the level of the posterior cruciate ligament’s tibial insertion. Proximal and distal convergent cuts are made to remove the bone wedge; reduction is achieved by gentle knee extension. Fixation is completed with 2 staples positioned medially and laterally to the TT.