Abstract
Objective:
To explore the impact of resiliency factors on the longitudinal trajectory of depressive symptoms in patients admitted to the Neuroscience Intensive Care Unit (Neuro-ICU) and their family caregivers.
Materials and Methods:
Patients (N=102) and family caregivers (N=103) completed self-report assessments of depressive symptoms (depression subscale of the Hospital Anxiety and Depression Scale; HADS-D) and resiliency factors (i.e., mindfulness and coping) during Neuro-ICU hospitalization. The HADS-D was administered again at 3 and 6 months after discharge. The Actor-Partner Interdependence Model (APIM) was used to assess patient-caregiver interdependence.
Results:
Baseline rates of clinically significant depressive symptoms were high among patients (23%) and caregivers (19%), and remained elevated through 6-months. Higher depressive symptoms predicted higher levels of symptoms at the subsequent timepoint (ps<.05). Higher baseline mindfulness and coping were associated with lower levels of depressive symptoms at all timepoints (ps<.001). APIM analysis showed that one’s own higher baseline mindfulness was associated with concurrent levels of depressive symptoms in a partner (p<.05).
Conclusions:
Depressive symptoms in Neuro-ICU patient-caregiver dyads are high through 6 months. Mindfulness is protective against depressive symptoms and interdependent between patients and caregivers. Early, dyadic, mindfulness-based interventions may prevent the development of chronic depression in both patients and caregivers.
Keywords: Neuroscience ICU, depression, resilience, actor-partner interdependence model, informal caregiver
1. Introduction
Admission to the Neuroscience Intensive Care Unit (Neuro-ICU) for an acute neurological injury often occurs without warning and is associated with substantial emotional distress not only for patients but also for their informal caregivers (i.e., family and close friends who provide help with the recovery process) [1], who have little time to adjust to the new demands placed on them. A recent meta-analysis showed that nearly one-third of general ICU patients reported clinically significant depressive symptoms after their hospitalization [2]. A large, longitudinal study of patients admitted to the ICU with acute respiratory distress syndrome shows that 36% experience clinically significant depressive symptoms 6 months after hospitalization [3], and that nearly one-third experience prolonged symptoms up to 5 years later [4]. Reported rates in caregivers of general ICU patients are comparably high (4–36%) 6 months after the patient’s discharge [5]. While two cross-sectional studies reported rates of clinically significant depressive symptoms of 24–69% [6,7] in caregivers and 24% [6] in patients, without prospective longitudinal research the trajectory of depression for patients and caregivers after Neuro-ICU hospitalization remains unknown. With depression affecting not only the patients’ own physical and emotional recovery, but also their caregivers’ abilities to provide quality care for their loved ones [8,9] untreated symptoms can ultimately lead to greater morbidity and mortality in both patients and caregivers [10–12]. Therefore, further characterization of depressive symptoms in Neuro-ICU patients and their informal caregivers has profound long-term health implications.
Resiliency is a biopsychosocial construct defined as the ability to adapt and recover when faced with adversity [13]. Two of the most well studied resiliency factors are mindfulness (the awareness of the present and ability to remain in the given moment nonjudgmentally [14] and coping (the ability to use cognitive and emotional strategies to deal with stressful situations [15]. Both mindfulness [16] and coping [15,17] are associated with a variety of positive physical and mental health outcomes in medical populations, including lower depressive symptoms in patients with motor neuron disease and their caregivers [18,19]. In the Neuro-ICU, cross-sectional studies demonstrated that higher mindfulness and coping were negatively associated with depressive symptoms and global emotional distress [20] and positively associated with quality of life in patients and their caregivers [21]. However, the long-term impact of these modifiable resilience factors on psychological distress in dyads of Neuro-ICU patients and their informal caregivers remains unknown.
There is mounting evidence suggesting that patients’ and their informal caregivers’ psychological functioning is interdependent and that the dyad (i.e. the patient and caregiver together) should be considered as a unit [22–24]. Much of this work has looked at psychological distress and resilience in cancer patients and their partners [24–27], but increasingly, the dyadic framework has been used to characterize psychiatric symptoms in general ICU patients and their caregivers [28,29]. Recently, a cross-sectional study of Neuro-ICU patients and their caregivers found that depressive symptoms are interdependent between dyad members, and that one’s own mindfulness was inversely related to one’s partner’s depressive symptoms [6]. Without prior longitudinal studies, however, the long-term interplay of depressive symptoms and resilience factors in Neuro-ICU survivors and their informal caregivers, as well as the significance of the dyad in the development of chronic depressive symptoms remain unclear.
The present study aims to fill this knowledge gap by characterizing the trajectory of depression from hospitalization to 6 months post-discharge for both Neuro-ICU patients and caregivers, as well as understand the relationship among psychosocial resiliency factors (mindfulness and coping) and symptoms of depression among dyads. Specifically, we first estimate rates of clinically significant depression in patient-caregiver dyads during initial hospitalization (i.e., baseline), as well as at 3-and 6-months post-discharge from the Neuro-ICU. Second, we explore the associations between patients’ and caregivers’ own baseline resiliency (i.e., mindfulness and coping) on both their own depressive symptoms and their partners’ depressive symptoms. We hypothesize that (1) for both patients and caregivers, one’s own baseline depressive symptoms will predict higher levels of own depressive symptoms at future time points, while resiliency factors will be associated with lower own depressive symptoms.
2. Methods
2.1. Participants and Procedures
Patients admitted to the Neuro-ICU at a major academic medical center in Boston, MA, and their informal caregivers were recruited as part of a prospective, longitudinal study between March 2015 and August 2016. All study procedures were approved by the local Institutional Review Board and consent was provided by all participants. Patients and caregivers were approached in their hospital room and screened based on the inclusion criteria: 1) at least 18 years of age, 2) English literacy and fluency, 3) Neuro-ICU hospitalization within the past 2 weeks, and 4) caregiver determined to be the primary source of informal care following hospitalization. Patients were cleared for research participation by their medical staff. Dyads who consented to participate in the study completed baseline self-report demographics and psychosocial measures during inpatient enrollment. Follow-up questionnaires sent at 3-and 6-monts after hospital discharge were administered through the secure electronic data collection platform REDCap [30].
2.2. Measures
2.2.1. Sociodemographics.
Dyads self-reported age, gender, race and ethnicity, marital status, highest level of education, primary employment status, and relationship (family member vs. romantic partner).
2.2.2. Depression.
The Hospital Anxiety and Depression Scale depression subscale (HADS-D) [31] includes 7 items that assess depression symptoms over the last week. Responses choices range from 0 (“not at all” or “rarely”) to 3 (“all of the time” or “very often”). Items are summed to generate a total score (range 0–21), with higher scores indicating greater depression symptoms. Scores ≥8 were considered indicative of clinically significant depression.
2.2.3. Mindfulness.
The Cognitive Affective Mindfulness Scale – Revised (CAMS-R) [32] is a 12-item measure that assesses four domains of mindfulness: observing, describing, awareness, and non-judgment. Response choices ranged from 1 (“rarely”/“not at all”) to 4 (“almost always”). Items are summed to generate a total score (range 12–48), with higher scores representing greater mindfulness.
2.2.4. Coping.
The Measure of Current Status-A (MOCS-A) [33] is a 13-item questionnaire that assesses perceived ability to utilize adaptive coping strategies – relaxation, recognizing stress, restructuring thoughts, assertiveness, and choosing appropriate responses. Items are scored on a 5-point Likert scale of 0 (“I cannot do this at all”) to 4 (“I can do this extremely well”), with higher scores indicating higher self-perceived coping status. The sum of all items represents the total score (range 0–52), with higher scores indicating greater perceived coping ability.
2.3. Statistical Analyses
All analyses were completed using SPSS version 24 (IBM Corp, 2016). First, patient and caregiver characteristics were assessed using measures of central tendency. We then examined univariate relationships between patient and caregiver variables using Pearson’s correlation, chisquare analyses, and paired sample t tests, as was determined appropriate. An alpha level of .05 and two-tailed tests were used to determine statistical significance. Effect size was categorized as small, medium, or large based on Pearson r values of 0.10, 0.30, and 0.50 [34].
We tested our hypotheses with the Actor-Partner Interdependence Model (APIM) [35,36]. APIM is an analytic design that simultaneously models the effects of one individual’s predictor values on their own outcomes (actor effects) and one’s partner’s outcomes (partner effects), while accounting for the fact that one’s own and one’s partner’s variables are interrelated. APIM has been used to understand the interdependence of psychological distress longitudinally in non-ICU [37] and ICU [28] populations, and cross-sectionally in the Neuro-ICU [6]. In the current study, APIM is used to determine the longitudinal effects of a patient or caregiver’s depression (continuous HADS-D score) and resiliency (continuous MOCS-A and CAMS-R scores) on their own psychological outcomes (actor effect), or on a partner’s psychological outcomes (partner effect) at all timepoints (i.e. baseline, 3, and 6 months). We used contrast tests to determine whether there was a significant difference in patient and caregiver actor effects. We repeated this process for partner effects. If the contrast test resulted p<.05, the actor effect or partner effect was deemed significantly different for patients and caregivers, so effects were reported and analyzed separately. If p>.05, the actor effect or partner effect was deemed to be not significantly different between patients and caregivers, so pooled effects are reported and analyzed.
3. Results
3.1. Characteristics of Patients and Caregivers
For this prospective study, 114 patient-caregiver dyads were enrolled (patients n=102, 89%; caregivers n=103; 90%) (Table 1). 102 patients and 103 caregivers from 108 different dyads (96 were complete patient-caregiver dyads, 6 patients were without caregivers, and 6 caregivers were without patients) completed measures and were included in this analysis. Measurement completion rates were 94% at baseline, 77% at 3-month follow up, and 71% at 6-month follow up. Most patients were enrolled within 1–2 days of Neuro-ICU admission. Caregivers were most commonly the patient’s partner. Cerebrovascular diseases, including ischemic and hemorrhagic stroke (35%), intracranial tumors (30%) or other structural lesions (8%), were the most common neurological diagnoses for this sample.
Table 1.
Demographic and medical characteristics of Neuroscience ICU patients (n=102) and their informal caregivers (n=103).
| Patients | Caregivers | |||
|---|---|---|---|---|
| Demographic/Medical Characteristic | n (%) | n (%) | t or X2 | df |
| Age (M[SD]) | 52 (17) | 53 (14) | −0.471 | 92 |
| Gender (female) | 48 (47) | 65 (63) | 5.011a | 1 |
| Race/ethnicity (non-Hispanic white) | 83 (81) | 92 (89) | 2.744 | 1 |
| Education (some college or more) | 76 (75) | 82 (80) | 0.556 | 1 |
| Marital status (married/cohabitating) | 70 (69) | 86 (83) | 6.423a | 1 |
| Employment (full-time) | 52 (51) | 60 (58) | 1.105 | 1 |
| Diagnosis, n (%) | ||||
| Cerebrovascular | ||||
| Stroke/Hemorrhage | 38 (35) | |||
| Brain aneurysm (unruptured) | 3 (3) | |||
| Other vascular | 2 (2) | |||
| Structural | ||||
| Tumor | 32 (30) | |||
| Lesion/brain mass | 9 (8) | |||
| Other | ||||
| Traumatic brain injury | 5 (5) | |||
| Seizure | 4 (4) | |||
| Other />1 diagnosis | 11 (10) | |||
| Not reported | 4 (4) | |||
| Discharge status, n (%) | ||||
| Discharge to home | 69 (64) | |||
| Discharge to rehabilitation facility | 31 (29) | |||
| Deceased at discharge | 1 (1) | |||
| Not reported | 7 (6) | |||
| Relationship to patient, n (%) | ||||
| Spouse/partner | 71 (66) | |||
| Parent | 14 (13) | |||
| Child | 14 (13) | |||
| Sibling | 5 (5) | |||
| Not reported | 4 (4) |
p<0.05
3.2. Patients and caregivers’ psychological factors
Coping and mindfulness scores did not significantly differ between patients and caregivers (Table 2). At baseline, rates of clinically significant depressive symptoms were high and were not significantly different between patients and caregivers (23% and 19%, respectively). Rates of clinically significant depressive symptoms remained high patients (24% and 26% at 3 and 6 months, respectively) and caregivers (19% and 20% at 3 and 6 months, respectively). Patients were more likely to report a clinically significant degree of symptoms at 3 months than caregivers (p=0.005). Individuals who were married/cohabitating had lower baseline depressive symptoms (p=0.038). Those without college education had higher levels of depressive symptoms at 3 and 6 months than their respective counterparts (p=0.012 and p= 0.006, respectively). Last, patients’ degree of depressive symptoms differed by diagnosis, with those having a cerebrovascular diagnosis exhibiting higher levels of depressive symptoms (3mo M = 5.19), than those with structural (3mo M = 3.36) or other diagnoses (3mo M = 3.72; F(2)=4.14, p = .015).
Table 2.
Psychological characteristics of Neuroscience ICU patients and their family caregivers.
| Patients | Caregivers | Comparison | ||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Mean | SD | Range | Mean | SD | Range | t | df |
| Mindfulness | 36.09 | 7.37 | 18–48 | 36.81 | 7.43 | 20–48 | −0.79 | 1377 |
| Coping | 31.90 | 11.77 | 2–52 | 32.42 | 11.21 | 0–51 | −0.27 | 653 |
| HADS depression score | ||||||||
| Baseline | 4.97 | 4.66 | 0–21 | 4.03 | 4.03 | 0–18 | 1.74 | 758 |
| 3 months | 4.59 | 4.87 | 0–21 | 3.8 | 3.97 | 0–15 | 1.33 | 235 |
| 6 months | 4.8 | 5.42 | 0–21 | 3.57 | 4.35 | 0–15 | 1.61 | 165 |
| % with clinically significant depressive symptoms | n (%) | n (%) | X2 | df | ||||
| Baseline | 23 (23) | 20 (19) | 3.60 | 1 | ||||
| 3 months | 24 (24) | 20 (19) | 8.05* | 1 | ||||
| 6 months | 27 (26) | 21 (20) | 4.27 | 1 | ||||
p<0.05
p<0.001
3.2.1. Effects of Own Psychological Factors on Own Depressive Symptoms (Actor Effects)
Bivariate analysis.
Table 3 presents bivariate correlations between depressive symptoms and resilience variables. For patients and caregivers, baseline depressive symptoms were significantly correlated with depressive symptoms at follow up (ps<0.05). Depressive symptoms were negatively correlated with mindfulness and coping variables at baseline and 3 months in patients (ps<0.001) and at all time three timepoints in caregivers (ps<0.001). The observed effect sizes for both patients and caregivers were medium to large (r>0.30).
Table 3.
Bivariate correlations of psychological resilience factors and depressive symptoms for Neuroscience ICU patients and their family caregivers.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Patient baseline depressive symptoms | 1 | |||||||||
| 2. Patient 3-month depressive symptoms | 0.315* | 1 | ||||||||
| 3. Patient 6-month depressive symptoms | 0.380** | 0.636** | 1 | |||||||
| 4. Patient coping | −0.491** | −0.335** | −0.194 | 1 | ||||||
| 5. Patient mindfulness | −0.457** | −0.429** | −0.368** | 0.625** | 1 | |||||
| 6. Caregiver baseline depressive symptoms | 0.244 | 0.233* | 0.241 | −0.122 | −0.257* | 1 | ||||
| 7. Caregiver 3-month depressive symptoms | 0.121 | 0.333* | 0.260* | −0.060 | −0.221 | 0.545** | 1 | |||
| 8. Caregiver 6-month depressive symptoms | 0.130 | 0.241 | 0.253 | −0.044 | −0.113 | 0.541** | 0.734** | 1 | ||
| 9. Caregiver coping | −0.107 | −0.076 | −0.088 | 0.100 | 0.135 | −0.605** | −0.399** | −0.355** | 1 | |
| 10. Caregiver mindfulness | −0.132 | −0.096 | −0.099 | 0.091 | 0.106 | −0.559** | −0.363** | −0.355** | 0.796** | 1 |
p<0.05
P<0.001
Dyadic analysis.
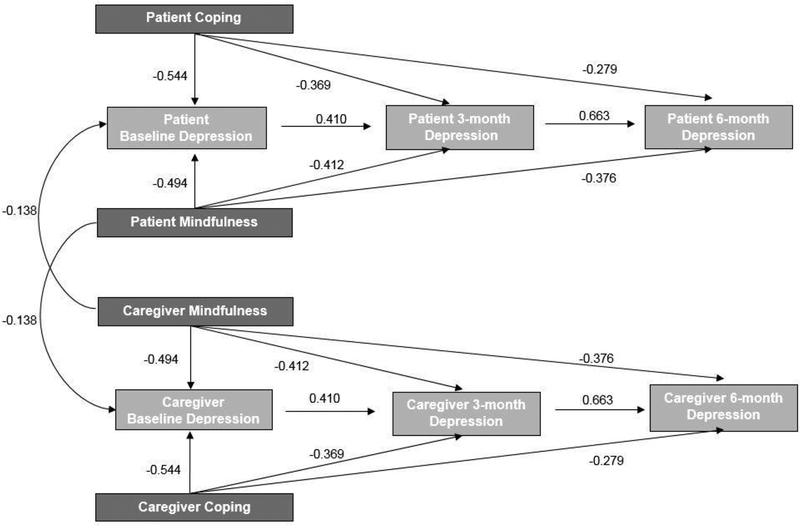
Table 4 summarizes actor effects from APIM analyses for this sample. Baseline mindfulness and coping scores for both patients and caregivers significantly predicted one’s own degree of depressive symptoms measured as the HADS-D continuous score at all three timepoints (baseline, 3-, and 6-month follow-up; ps<0.001). Baseline depressive symptoms also significantly predicted continued presence at follow-up time points (ps<0.001). Actor effects were equivalent for patients and caregivers.
Table 4.
Actor-Partner Interdependence Models on effect of own psychological resilience factors and depressive symptoms on own and partner’s symptoms.
| Actor effects | Partner effects | |||||||
|---|---|---|---|---|---|---|---|---|
| B | Unstandardized 95% CI | p | Standardized β | B | Unstandardized 95% CI | p | Standardized β | |
| Prior Depression Symptoms | ||||||||
| Baseline → 3-month | 0.419 | 0.292 – 0.546 | <0.001 | 0.410 | 0.088 | −0.045 – 0.220 | 0.182 | 0.087 |
| 3-month → 6-month | 0.736 | 0.618 – 0.854 | <0.001 | 0.663 | 0.066 | −0.062 – 0.194 | 0.430 | 0.059 |
| Mindfulness | ||||||||
| Baseline depressive symptoms | −0.293 | −0.367 - −0.218 | <0.001 | −0.494 | −0.082 | −0.156 - −0.008 | 0.031 | −0.138 |
| 3-month depressive symptoms | −0.249 | −0.326 - −0.173 | <0.001 | −0.412 | −0.064 | −0.140 – 0.012 | 0.096 | 0.106 |
| 6-month depressive symptoms | −0.253 | −0.339 - −0.116 | <0.001 | −0.376 | −0.041 | −0.127 – 0.045 | 0.349 | −0.061 |
| Coping | ||||||||
| Baseline depressive symptoms | −0.209 | −0.255 - −0.162 | <0.001 | −0.544 | −0.023 | −0.069 – 0.024 | 0.379 | −0.059 |
| 3-month depressive symptoms | −0.144 | −0.195 - −0.093 | <0.001 | −0.369 | −0.012 | −0.063 – 0.039 | 0.585 | −0.030 |
| 6-month depressive symptoms | −0.121 | −0.179 - −0.063 | <0.001 | −0.279 | −0.016 | −0.074 – 0.043 | 0.557 | −0.036 |
Bold = significant effect with p<0.05
3.2.2. Effects of Partner’s Psychological Factors on Depressive Symptoms (Partner Effects)
Bivariate analysis.
Table 3 presents bivariate correlations between patient and caregiver factors. Caregiver depressive symptoms at 3 months were significantly correlated with patient depressive symptoms at 3 and 6 months with a small to medium effect size (r<=0.30; ps<0.04). There were no other significant correlations between patient and caregiver symptoms. Patients’ mindfulness was negatively correlated with caregivers’ baseline depressive symptoms (p=0.04). However, one’s own coping was not associated with partner’s depressive symptoms at any timepoint.
3.2.3. Dyadic analysis.
Table 4 presents partner effects from APIM analyses for this sample. For both patients and caregivers, baseline mindfulness predicted partner’s degree of depressive symptoms (HADS-D continuous score) at baseline (p=0.03), but not at 3-, and 6-month follow-up (ps>0.09). This partner effect was equivalent from patients’ mindfulness to caregivers’ depressive symptoms, and from caregiver’s mindfulness to patients’ depressive symptoms. No other partner effects were significant.
4. Discussion
We found that during ICU hospitalization, 23% of patients and 19% of caregivers reported clinically significant levels of depressive symptoms. Rates of clinically significant symptoms remained high over time in patients and caregivers. The increase risk in depression observed in patients can be explained in 2 major ways. First, permanent deficits in cognitions and function are often unknown at hospitalization but may become clear in the months after discharge when acute rehabilitation is generally completed. Among stroke patients, degree of functional and cognitive impairment has consistently been found to be a predictor of depression [38,39], so distress over persistent deficits may contribute the observed increase in rates of clinically significant symptoms over time and overall higher rates in patients than in caregivers. Second, depression among neuro-critical care patients is complicated by biological confounds associated with the actual brain injury and may drive post-stroke depression [39], adding to the discrepancy between patient and caregiver rates. Our finding that patients with admission diagnoses of cerebrovascular disease showed a higher rate of clinically significant depressive symptoms lends support to this hypothesis. Third, as a similar increase in depression symptom incidence at 3 months has been shown in general ICU populations [40], it may be that this is the natural progression of emotional distress in patients recovering from a severe critical illness.
In line with our hypothesis, we found that higher levels of depressive symptoms predicted higher levels of depressive symptoms at subsequent timepoints in both patients and caregivers. This is supported by previous work that affirmed existing depression was a strong predictor for continued symptoms over time [41]. For patients and caregivers, own baseline mindfulness and coping skills were associated with lower levels of depressive symptoms at all time points, which is consistent with previous studies in ICU patients and families [20]. Mindfulness, specifically, may be protective as it helps stop rumination on negative thoughts [42], which can contribute to the development of depressive symptoms.
APIM is a crucial tool that facilitates the analysis of patients and their caregivers as a dyad unit, rather than as separate entities. In this study, the APIM dyadic approach allows us to detect both cross-sectional and longitudinal effects that one dyad member’s symptoms and skills has on the other member. We observed that one’s own baseline mindfulness predicts concurrent level of baseline depressive symptoms in one’s partner. As more mindful individuals tend to me more skilled at tuning into their own psychological states and emotional needs [16], they might similarly be attuned to their partner, and therefore more able facilitate positive interpersonal interactions and adaptive coping to protect against depressive symptoms during the early adaptation to illness. Later, as negative thought processes become more fixed and chronic, a mindful partner’s support may be less helpful in augmenting symptoms. This may represent an early critical period in which mindfulness-based dyad interventions may be most potent in preventing depressive symptoms.
Bivariate analysis showed that caregiver depressive symptoms at 3 months correlated with patient depressive symptoms at both 3 and 6 months. It may be that following an ICU hospitalization, patients and caregivers acclimate to their post-discharge environment in parallel [22]. However, these findings did not bear out in APIM analysis. So, while mindfulness may be interdependent, the more internally-oriented nature of depressive symptoms may not impact an individual’s partner as strongly.
Our findings, along with the growing body of knowledge about Neuro-ICU patient and caregiver psychological factors, have several important clinical implications. First, since the incidence of depressive symptoms in both patient and caregivers is high and remain high through 6 months, our findings of the protective nature and mindfulness and coping suggest that an intervention targeted at bolstering these resilience factors may help prevent chronic depression in patients and caregivers. Second, since a patient or caregiver’s mindfulness skills is also protective against depression in their partner, these interventions should be dyadic, and focus on the patient and caregiver as a unit. Finally, the interdependence of mindfulness and baseline depression symptoms points to a window for dyadic intervention early in the recovery process. Qualitatively, patients and caregivers have endorsed interest in such an intervention [43].
A primary strength of this study is the prospective, longitudinal design. Longitudinal data can inform how to better provide preventative care and tailored recovery programs to Neuro-ICU survivors, even after discharge from the hospital. Our study also contributes to the growing evidence about patient and caregiver interdependence through our use of APIM analysis.
There are several limitations to this study. First, we required patients to be cognitively intact, a criterion which excluded the most critically ill patients in the Neuro-ICU. Second, the use of self-report measures may introduce biased, but was important in the Neuro-ICU for feasibility. Finally, this study was conducted at a single, urban medical center and the sample was homogenous in demographics such as race, ethnicity, and education. These procedures should be replicated in a more diverse population.
Despite limitations, strong indication that dyadic interventions starting early in the Neuro-ICU can improve psychosocial functioning among patients and families. Overall, these results convey important clinical findings. First, the presence of depressive symptoms predicts sustained symptoms at the subsequent time point in both patients and caregivers. As mindfulness and coping are both associated with lower inpatient symptoms of depression, early psychosocial interventions teaching resiliency skills in the Neuro-ICU could address and prevent the onset of chronic depression in patients and caregivers. In addition, patient and caregiver resiliency factors were found to be interdependent, which lends support to the development of dyadic resiliency interventions. Taken together, targeting resiliency and mindfulness in the Neuro-ICU has the potential of alleviating or preventing the onset of depressive symptoms and prevent chronic depression in both members of the dyadic unit.
Figure 1.
Actor-Partner Interdependence modeling (APIM) for resilience factors and depression symptoms at baseline, 3, and 6 months. Values represent standardized beta coefficients. Only significant paths shown.
Acknowledgements
We thank Tara Tehan, Mary Guanci, Danielle Salgueiro, and the dedicated team of Neuro-ICU nurses for their help with recruitment.
Funding
This study was supported by a grant from the National Institute of Nursing Research awarded to Ana-Maria Vranceanu [grant number 1R21NR017979]; a Grant in Aid from the American Heart Association awarded to Ana-Maria Vranceanu [grant number 228671]; an American Heart Association Founders Affiliate Fellowship awarded to Ann Lin; and the Henry and Allison McCance Center for Brain Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
Dr. Rosand reports serving as a consultant for Boehringer Ingelheim, Pfizer and New Beta Innovation. No other authors report conflicts.
References
- [1].Caregiving in the U.S. 2015. | National Alliance for Caregiving. National Alliance for Caregiving; n.d. [Google Scholar]
- [2].Rabiee A, Nikayin S, Hashem MD, Huang M, Dinglas VD, Bienvenu OJ, et al. Depressive Symptoms After Critical Illness: A Systematic Review and Meta-Analysis. Crit Care Med 2016;44:1744–53. doi: 10.1097/CCM.0000000000001811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Huang M, Parker AM, Bienvenu OJ, Dinglas VD, Colantuoni E, Hopkins RO, et al. Psychiatric Symptoms in Acute Respiratory Distress Syndrome Survivors: A One-Year National Multi-Center Study. Crit Care Med 2016;44:954–65. doi: 10.1097/CCM.0000000000001621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bienvenu OJ, Friedman LA, Colantuoni E, Dinglas VD, Sepulveda KA, Mendez-Tellez P, et al. Psychiatric symptoms after acute respiratory distress syndrome: a 5-year longitudinal study. Intensive Care Med 2018;44:38–47. doi: 10.1007/s00134-017-5009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].van Beusekom I, Bakhshi-Raiez F, de Keizer NF, Dongelmans DA, van der Schaaf M. Reported burden on informal caregivers of ICU survivors: a literature review. Crit Care 2016;20:16. doi: 10.1186/s13054-016-1185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Shaffer KM, Riklin E, Jacobs JM, Rosand J, Vranceanu A-M. Mindfulness and Coping Are Inversely Related to Psychiatric Symptoms in Patients and Informal Caregivers in the Neuroscience ICU: Implications for Clinical Care. Crit Care Med 2016;44:2028–36. doi: 10.1097/CCM.0000000000001855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Norup A, Welling K-L, Qvist J, Siert L, Mortensen EL. Depression, anxiety and qualityof-life among relatives of patients with severe brain injury: the acute phase. Brain Inj 2012;26:1192–200. doi: 10.3109/02699052.2012.672790. [DOI] [PubMed] [Google Scholar]
- [8].Warren AM, Rainey EE, Weddle RJ, Bennett M, Roden-Foreman K, Foreman ML. The intensive care unit experience: Psychological impact on family members of patients with and without traumatic brain injury. Rehabil Psychol 2016;61:179–85. doi: 10.1037/rep0000080. [DOI] [PubMed] [Google Scholar]
- [9].Choi J, Tate JA, Hoffman LA, Schulz R, Ren D, Donahoe MP, et al. Fatigue in family caregivers of adult intensive care unit survivors. J Pain Symptom Manage 2014;48:353–63. doi: 10.1016/j.jpainsymman.2013.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: spouse caregivers. J Clin Oncol Off J Am Soc Clin Oncol 2007;25:4829–34. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- [11].Mausbach BT, Patterson TL, Rabinowitz YG, Grant I, Schulz R. Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychol Off J Div Health Psychol Am Psychol Assoc 2007;26:539–44. doi: 10.1037/0278-6133.26.5.539. [DOI] [PubMed] [Google Scholar]
- [12].Bartoli F, Lillia N, Lax A, Crocamo C, Mantero V, Carrà G, et al. Depression after stroke and risk of mortality: a systematic review and meta-analysis. Stroke Res Treat 2013;2013:862978. doi: 10.1155/2013/862978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rutter M Psychosocial resilience and protective mechanisms. Am J Orthopsychiatry 1987;57:316–31. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- [14].Kabat-Zinn J Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin Psychol Sci Pract 2003;10: 144–56. doi: 10.1093/clipsy.bpg016. [DOI] [Google Scholar]
- [15].Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: a meta-analytic review. J Behav Med 2002;25:551–603. [DOI] [PubMed] [Google Scholar]
- [16].Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol 2003;84:822–48. [DOI] [PubMed] [Google Scholar]
- [17].Austenfeld JL, Stanton AL. Coping through emotional approach: a new look at emotion, coping, and health-related outcomes. J Pers 2004; 72: 1335–63.doi: 10.1111/j.1467-6494.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- [18].Pagnini F, Phillips D, Bosma CM, Reece A, Langer E. Mindfulness as a Protective Factor for the Burden of Caregivers of Amyotrophic Lateral Sclerosis Patients. J Clin Psychol 2016;72:101–11. doi: 10.1002/jclp.22235. [DOI] [PubMed] [Google Scholar]
- [19].Pagnini F, Phillips D, Bosma CM, Bosma MC, Reece A, Langer E. Mindfulness, physical impairment and psychological well-being in people with amyotrophic lateral sclerosis. Psychol Health 2015;30:503–17. doi: 10.1080/08870446.2014.982652. [DOI] [PubMed] [Google Scholar]
- [20].Shaffer KM, Riklin E, Jacobs JM, Rosand J, Vranceanu A-M. Psychosocial resiliency is associated with lower emotional distress among dyads of patients and their informal caregivers in the neuroscience intensive care unit. J Crit Care 2016;36:154–9. doi: 10.1016/j.jcrc.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zale EL, Heinhuis TJ, Tehan T, Salgueiro D, Rosand J, Vranceanu A-M. Resiliency is independently associated with greater quality of life among informal caregivers to neuroscience intensive care unit patients. Gen Hosp Psychiatry 2018;52:27–33. doi: 10.1016/j.genhosppsych.2018.02.012. [DOI] [PubMed] [Google Scholar]
- [22].Hodges LJ, Humphris GM, Macfarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med 1982. 2005;60:1–12. doi: 10.1016/j.socscimed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- [23].Savini S, Buck HG, Dickson VV, Simeone S, Pucciarelli G, Fida R, et al. Quality of life in stroke survivor-caregiver dyads: a new conceptual framework and longitudinal study protocol. J Adv Nurs 2015;71:676–87. doi: 10.1111/jan.12524. [DOI] [PubMed] [Google Scholar]
- [24].Bakas T, Clark PC, Kelly-Hayes M, King RB, Lutz BJ, Miller EL. Evidence for Stroke Family Caregiver and Dyad Interventions: A Statement for Healthcare Professionals From the American Heart Association and American Stroke Association. Stroke 2014:STR.0000000000000033. doi: 10.1161/STR.0000000000000033. [DOI] [PubMed] [Google Scholar]
- [25].Lim J-W, Shon E-J, Paek M, Daly B. The dyadic effects of coping and resilience on psychological distress for cancer survivor couples. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 2014;22:3209–17. doi: 10.1007/s00520-014-2334-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shaffer KM, Kim Y, Carver CS. Physical and mental health trajectories of cancer patients and caregivers across the year post-diagnosis: a dyadic investigation. Psychol Health 2016;31:655–74. doi: 10.1080/08870446.2015.1131826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Jacobs JM, Shaffer KM, Nipp RD, Fishbein JN, MacDonald J, El-Jawahri A, et al. Distress is Interdependent in Patients and Caregivers with Newly Diagnosed Incurable Cancers. Ann Behav Med Publ Soc Behav Med 2017;51:519–31. doi: 10.1007/s12160-017-9875-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Rosendahl J, Brunkhorst FM, Jaenichen D, Strauss B. Physical and mental health in patients and spouses after intensive care of severe sepsis: a dyadic perspective on long-term sequelae testing the Actor-Partner Interdependence Model. Crit Care Med 2013;41:69–75. doi: 10.1097/CCM.0b013e31826766b0. [DOI] [PubMed] [Google Scholar]
- [29].Wintermann G-B, Petrowski K, Weidner K, Strauß B, Rosendahl J. Impact of posttraumatic stress symptoms on the health-related quality of life in a cohort study with chronically critically ill patients and their partners: age matters. Crit Care Lond Engl 2019;23:39. doi: 10.1186/s13054-019-2321-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- [32].Feldman G, Hayes A, Kumar S, Greeson J, Laurenceau J-P. Mindfulness and Emotion Regulation: The Development and Initial Validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). J Psychopathol Behav Assess 2007;29:177. doi: 10.1007/s10862-006-9035-8. [DOI] [Google Scholar]
- [33].Carver C Measure of Current Status 2006. http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html (accessed September 25, 2017).
- [34].Cohen J A power primer. Psychol Bull 1992;112:155–9. [DOI] [PubMed] [Google Scholar]
- [35].Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. New York, NY: Guilford Press; 2006. [Google Scholar]
- [36].Kenny DA, Cook W. Partner effects in relationship research: Conceptual issues, analytic difficulties, and illustrations. Pers Relatsh 1999;6:433–48. doi: 10.1111/j.1475-6811.1999.tb00202.x. [DOI] [Google Scholar]
- [37].Segrin C, Badger T, Dorros SM, Meek P, Lopez AM. Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psychooncology 2007;16:634–43. doi: 10.1002/pon.1111. [DOI] [PubMed] [Google Scholar]
- [38].Ayerbe L, Ayis S, Wolfe CDA, Rudd AG. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry J Ment Sci 2013;202:14–21. doi: 10.1192/bjp.bp.111.107664. [DOI] [PubMed] [Google Scholar]
- [39].Robinson RG, Jorge RE. Post-Stroke Depression: A Review. Am J Psychiatry 2016;173:221–31. doi: 10.1176/appi.ajp.2015.15030363. [DOI] [PubMed] [Google Scholar]
- [40].Bienvenu OJ, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Shanholtz C, Husain N, et al. Depressive symptoms and impaired physical function after acute lung injury: a 2-year longitudinal study. Am J Respir Crit Care Med 2012;185:517–24. doi: 10.1164/rccm.201103-0503OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med 2009;35:796–809. doi: 10.1007/s00134-009-1396-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Broderick PC. Mindfulness and Coping with Dysphoric Mood: Contrasts with Rumination and Distraction. Cogn Ther Res 2005;29:501–10. doi: 10.1007/s10608-005-3888-0. [DOI] [Google Scholar]
- [43].McCurley JL, Funes CJ, Zale EL, Lin A, Jacobo M, Jacobs JM, et al. Preventing Chronic Emotional Distress in Stroke Survivors and Their Informal Caregivers. Neurocrit Care 2018. doi: 10.1007/s12028-018-0641-6. [DOI] [PMC free article] [PubMed] [Google Scholar]