Stroke remains one of the most feared complications of atrial fibrillation (AF) with an overall risk of 5% per year [1]. AF-related strokes have a more fatal and disabling impact than those with other etiologies [2]. In non-rheumatic AF, the great majority of intra-atrial thrombi occur in the left atrial appendage (LAA) [3]. To reduce stroke risk, patients are prescribed oral anticoagulants (OAC), but this treatment has well-known side effects. Implementation of direct OAC (DOAC) as first line treatment provides a better risk-benefit profile compared to vitamin-K antagonists, but DOAC induced bleeding and drug interactions still leave some patients intolerant to its use. As an alternative to (D)OAC, endo- and epicardial LAA-closure devices have been developed. While percutaneous closure devices are increasingly being used, insufficient closure, need for endothelialization and incompatibility with certain LAA-anatomies remain an issue [4]. Moreover, intracardiac thrombi, and especially if located in the LAA, are a major contraindication for such an approach.
In patients with atrial fibrillation intolerant to the use of oral anticoagulation, a thrombus in the left atrial appendage (LAA) carries not only a high risk for stroke but also makes mechanical LAA-occlusion challenging. Here, we report a successful and uncomplicated beating-heart thoracoscopic epicardial closure of a LAA with adherent thrombus using a new steerable open-ended clipping device. The AtriClip Pro-V is a thoracoscopic port-compatible, v-shaped titanium clip using a three-spring mechanism to close first at the open end and to apply equal force across the entire length of the device to seal the LAA orifice at its base (Fig. 1A).
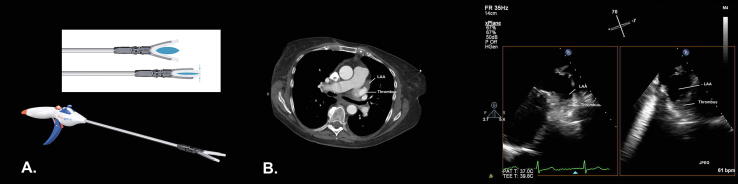
Fig. 1.
Atriclip pro-V device and illustration of the gradual closure mechanism. (A) Preoperative imaging of the thrombus distal in the left atrial appendage on cardiac CT and TOE (C).
The procedure was performed in a 70-year old female patient with alcoholic hepatic cirrhosis, chronic kidney disease and well rate-controlled permanent AF for 10 years. In 2016, she suffered a transient ischemic attack (CHA2DS2-VASc 5, HAS-BLED 6). DOAC-therapy was eventually discontinued after major gastrointestinal bleeds and frequent epistaxis. In the work-up for a LAA occlusion procedure, pre-operative CT-scan and transesophageal echocardiography (TOE) revealed a thrombus in the LAA (Fig. 1B + C, video 1). This finding precluded the use of a percutaneous closure device, but also raised safety concerns for application of the closed-ended version of the Atriclip device. To minimize the risk of periprocedural thrombus dislocation, the use of the open-ended AtriClip Pro-V was considered to give the best risk-benefit ratio. A thoracoscopic approach was preferred over an open procedure given the patient’s morbidity, the expected faster postoperative recovery and the much lower risk of peri-operative bleeding since such a thoracoscopic procedure does not require any form of heparinization. As the device has no CE-mark, a compassionate use allowance was obtained from the Dutch Ministry of Health, Welfare and Sport. Extensive informed consent was obtained.
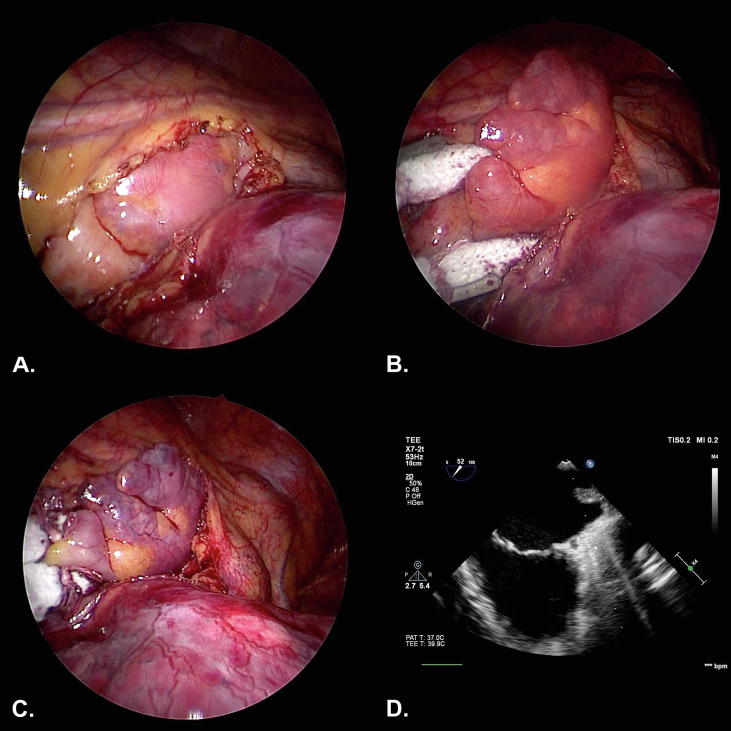
After anesthesia induction and double-lumen endotracheal tube intubation, single-lung, right-sided ventilation was established. Intraoperative TOE confirmed the presence of a thrombus distal to the base of the LAA. A 5 mm-camera port was introduced in the 4th left intercostal space. Two 5 mm-working ports were placed in the 2nd and 6th intercostal space at the midaxillary line. The pericardium was opened below the phrenic nerve and the LAA was inspected (Fig. 2A, video 2). To obtain full closure at the level of the LAA-base, a 50 mm AtriClip Pro-V was selected. The lower working port was exchanged for a 12 mm port to introduce the device. The clip was carefully positioned by sliding the open end from caudal to cranial along the course of the LAA-base without manipulating the distal portion of the LAA to avoid potential thrombus dislocation (Fig. 2B). After clip application, complete occlusion of the LAA at its base was confirmed on TOE (Fig. 2C+D, video 1). The patient was extubated in the OR. The patient was discharged 2 days after the operation without any complications. A follow-up visit, 6 months after the procedure, confirmed a uneventful post-operative course.
Fig. 2.
Periprocedural steps showing (A) exposure of the left atrial appendage (LAA), (B) during and (C) after LAA clipping. (D) Final result on TOE.
Although there are no randomized controlled trials confirming stroke risk reduction after surgical LAA exclusion, a multi-center registry evaluating 222 consecutive patients that underwent thoracoscopic AF surgery and LAA exclusion with a closed-ended AtriClip device demonstrated an observed cerebrovascular event rate as low as 0.5 per 100 patient-years, with 57% of patients off OAC [5]. Moreover, a high LAA closure rate (95.0%) and the absence of clip-related complications were reported, indicating that thoracoscopic LAA clipping is an effective and safe procedure. However, treating patients with a thrombus in the LAA and intolerant to (D)OAC use remains challenging. Our report shows that beating-heart thoracoscopic epicardial closure of a thrombus-containing LAA using an open-ended clipping device is feasible and seems safe. The excellent closure rates of the closed-ended AtriClip device need to be confirmed for the open-ended AtriClip Pro-V in clinical trials.
CRediT authorship contribution statement
Mindy Vroomen: Writing - original draft. Justin G.L.M. Luermans: Writing - review & editing.
Declaration of Competing Interest
MLM and BM are consultant for Atricure.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2019.100460.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Roger V.L., Go A.S., Lloyd-Jones D.M., Benjamin E.J., Berry J.D., Borden W.B. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barra S., Fynn S. Untreated atrial fibrillation in the United Kingdom: Understanding the barriers and treatment options. J. Saudi Heart Assoc. 2015;27:31–43. doi: 10.1016/j.jsha.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blackshear J.L., Odell J.A. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann. Thorac. Surg. 1996;61:755–759. doi: 10.1016/0003-4975(95)00887-X. [DOI] [PubMed] [Google Scholar]
- 4.Tan N.Y., Yasin O.Z., Sugrue A., El Sabbagh A., Foley T.A., Asirvatham S.J. Anatomy and physiologic roles of the left atrial appendage: implications for endocardial and epicardial device closure. Interv. Cardiol. Clin. 2018;7:185–199. doi: 10.1016/j.iccl.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 5.van Laar C., Verberkmoes N.J., van Es H.W., Lewalter T., Dunnington G., Stark S. Thoracoscopic left atrial appendage clipping: a multicenter cohort analysis. JACC Clin. Electrophysiol. 2018;4:893–901. doi: 10.1016/j.jacep.2018.03.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.