Abstract
Lung cancer is the most common cause of cancer death with high morbidity and mortality, which non-small-cell lung cancer (NSCLC) accounting for the majority. Traditional Chinese Medicine (TCM) is effective in the treatment of complex diseases, especially cancer. However, TCM is still in the conceptual stage. The interaction between different components remains unknown due to its multicomponent and multitarget characteristics. In this study, compound Liuju formula was taken as an example to isolate compounds with synergistic biological activity through systems pharmacology strategy. Through pharmacokinetic evaluation, 37 potentially active compounds were screened out. Meanwhile, 116 targets of these compounds were obtained by combing with the target prediction model. Through network analysis, we found that multicomponent drugs can present a synergistic effect through regulating inflammatory signaling pathway, invasion pathway, proliferation, and apoptosis pathway. Finally, it was confirmed that the bioactive compounds of compound Liuju formula have not only a killing effect on NSCLC tumor cells but also a synergistic effect on inhibiting the secretion of correlative inflammatory mediators, including TNF-α and IL-1β. The systems pharmacology method was applied in this study, which provides a new direction for analyzing the mechanism of TCM.
1. Introduction
With increasing incidence and mortality, cancer has become the leading cause of death and has caused serious public health problems worldwide. Among them, lung cancer is the most common type of cancer [1, 2]. Non-small-cell lung cancer (NSCLC) accounts for 80–85% of all lung cancers [3]. At present, the main effective methods in reducing the mortality of non-small-cell lung cancer include chemotherapy, radiotherapy, targeted therapy, and surgery [4]. Nonetheless, the overall 5-year survival rate of NSCLC remains low and is only 18% [5], while the drug resistance and side effects are getting more serious [2]. Therefore, there is an urgent need for novel methods for treating NSCLC that are effective and safe.
In recent years, Traditional Chinese Medicine (TCM) is widely used all over the world. TCM has been effective to relieve complex diseases for over 4000 years due to multicomponent, multitarget, and multilevel characteristics [6]. For instance, compound Liuju formula is widely used in the treatment of lung diseases in China. Clinical medicines such as clinical compound Liuju tablets and compound Liuju granules contain leaves of Hanliuye (Salix matsudana Koidz., SMK), Yejuhua (Chrysanthemum indicum L., CIL), and Baihuasheshecao (Hedyotis diffusa Willd, HDW). The SMK was used in the Chinese dictionary [7] as a traditional anti-inflammatory and analgesic [7, 8] medicine. Research has shown that CIL has been used to cure inflammation-related diseases and malignant tumors [9, 10]. It is reported that EEHDW has an effective inhibitory activity on human lung cancer cells by inhibiting cell proliferation and reducing cell activity [11]. TCM had fewer side effects, wide availability and better effect, and can availably improve the life quality of NSCLC patients. However, it is very hard to explain the interaction among the collaborative compositions that we confront a huge complex system for TCM formula.
With the development of analytical tools such as biology network [12], network pharmacology [13], and systems biology [14], the complex and comprehensive mechanism of TCM syndrome differentiation is expected to be quickly and efficiently clarified. In previous research, we have successfully constructed a new systems pharmacology method in order to explore the potential mechanism of Traditional Chinese Medicine. This method combines pharmacokinetics (absorption, distribution, metabolism, excretion, and toxicity (ADME/T) characteristics of drugs), molecular evaluation, target prediction, and pathway analysis to explore the effects of drugs [15, 16], which provides a platform for identifying multiple mechanisms of action of drugs. This platform has successfully developed four herbs, including Radix Astragali Mongolici, Radix Puerariae Lobatae, Radix Ophiopogonis Japonici, and Radix Salviae miltiorrhiza [17], that were applied in the comprehensive treatment of cardiovascular disease. systems pharmacology has become a widely used new tool to reveal the mechanism of drug action and drug development.
In our current work, the systems pharmacology method was utilized to study synergic bioactive compounds isolated from the compound Liuju formula treatment of NSCLC. We screened out bioactive ingredients from the constructed compound Liuju formula via ADME by calculating pharmacokinetic properties and evaluating oral bioavailability (OB) and drug-likeness (DL). Then, a comprehensive target prediction method combining biological model and mathematical model was used to predict the homologous target of the selected bioactive ingredients. Next, the obtained target was verified by functional enrichment analysis and target-disease interaction analysis. Finally, the system revealed potential collaborative interactions between bioactive ingredients, active targets, and pathways through systematic pharmacology theory and NSCLC-related signaling pathway evaluation. And, in vitro experiments were conducted to further verify the inhibitory effect of potential bioactive ingredients on tumor cells. These results not only provide new treatments for NSCLC but also promote the elucidation and development of the molecular mechanism of TCM.
2. Materials and Methods
2.1. Construction of Molecular Database and ADME Screening
All compounds of SMK, CIL, and HDW were obtained from our formerly established database named Traditional Chinese Medicine Systems Pharmacology Database (TCMSP, http://lsp.nwu.edu.cn/) [18] and were detected artificially. Because glycosyl molecules are usually hydrolyzed into free glycosides in vivo, which can be easily absorbed by intestinal mucosa, we wrote the molecule without glycosyl viscose as _qt [19]. To gain the bioactive molecules, we employed a comprehensive model comprising predict OB (oral bioavailability) and DL (drug-likeness) to appraise pharmacokinetic and pharmaceutical properties.
2.1.1. Oral Bioavailability
Oral bioavailability (OB) refers to the speed and degree of drug absorption into human circulation, which reflects the proportion of drugs in human circulation and plays a critical role in drug screening. In this work, OB value was calculated by an in-house model OBioavail1.1 [18]. And, the threshold of OB value was positioned as 25% by the following conditions: firstly, get as much information as possible from the herbs studied with the fewest compounds. Secondly, the acquired model is correctly interpreted by the reported pharmacological data [20]. In this work, for further analysis, we limited the OB threshold as 25%.
2.1.2. Drug-Likeness
Drug-likeness (DL) refers to the similarity between compounds and known drugs, which is an important factor in determining the success of final clinical trials of drugs. In this work, we utilized the previously developed internal model (Tanimoto coefficient) [20] to predict drug-like properties of expected molecules. The DL appraisal formula is as follows:
| (1) |
Among them, A represents the molecular descriptor of herbal compounds, and B represents the average molecular properties of all compounds in the database (http://www.drugbank.ca/) [21]. For further study, we defined DL ≥ 0.18 (average of drug library) as the criterion for screening candidate compounds.
In order to obtain the potential bioactive ingredients, the screening standard was defined as OB ≥ 25%, DL ≥ 0.18.
2.2. Drug Targeting
In order to structure a direct link between potential bioactive ingredients and targets, we utilized the in-house developed system drug targeting tool (SysDT) [22] and weighted integration similarity (WES) [23] algorithm to predict the target of the compound and to improve the comprehensiveness and accuracy of the target data bank.
Firstly, the weighted ensemble similarity (WES) and systematic drug targeting tool (SysDT) were applied to explore the target information of active compound. As for SysDT, which includes two mathematical tools, Random Forest (RF) and Support Vector Machine (SVM) can determine the interaction between composite targets more completely [22]. There was another computing model, WES, which combines CDK parameters, Dragon parameters, and CDK-Dragon mixing parameters, to predict the direct target of the actual bioactive ingredients [23]. Secondly, the collected protein targets were mapped to the UniProt database (http://www.uniprot.org) for standardization [24]. Finally, the normalized compound targets were mapped to Therapeutic Target Database (TTD, http://database.idrb.cqu.edu.cn/TTD/) [25], Comparative Toxicogenomics Database (CTD, http://ctdbase.org/) [26], Pharmacogenomics Knowledgebase (PharmGKB, https://www.pharmgkb.org/) [27], and Kyoto Encyclopedia of Genes and Genomes (KEGG, http://www.kegg.jp/) [28] to obtain their corresponding diseases and to screen out a relationship between target and disease network.
2.3. Gene Ontology (GO) Analysis and Pathway Enrichment
In order to further analyze the specific biological processes and approaches of the potential targets we have obtained, Gene Ontology (GO) enrichment analysis was performed by linking the targets to the KEGG. KEGG is a collection of databases for systematic analysis of gene functions, biological pathways, diseases, drugs, and chemicals [29]. Finally, the pathway and process enrichment analyses were carried out by using Metascape (Metascape, http://metascape.org) [30, 31] software.
2.4. Network Construction
In order to visualize the action mechanism of active compounds treating NSCLC and further clarify the relationship between active targets and compounds, we constructed two relational networks: Compound-Target network (C-T network) and Target-Pathway network (T-P network). In these networks, compounds, targets, and pathways were represented by nodes, while the relationship between them was represented by line segments. The degree represents the number of edges associated with a node, and the larger the number, the more node relationships it represents. The topological properties of these networks were analyzed using Cytoscape 3.6.0 [32], which is fashionable bioinformatics software.
2.5. Pathway Construction
In terms of pathway, in order to explore the integrative mechanism of action of compound Liuju formula on NSCLC, an integrated pathway related to NSCLC was established based on existing pathological knowledge of NSCLC. Firstly, in order to obtain the basic information of the pathway, we mapped the screened human target proteins to the KEGG database. Secondly, the integrated KEGG pathways of targets with false discovery rated (FDR) less than 0.05 by Fisher's Exact test in the Database for Annotation, Visualization, and Integrated Discovery (DAVID, http://david.abcc.ncifcrf.gov) (evaluated to Fisher's exact test, FDR < 0.05) were inspected [33]. Finally, we manually assembled a relatively complete NSCLC-related pathway to further analyze the molecular action mechanism.
2.6. Experimental Detection
2.6.1. Sample Treatment
Chemicals apigenin (B20981, HPLC ≥ 98%), kaempferol (B21126, HPLC ≥ 98%), and ursolic acid (B21403, HPLC ≥ 98%) were purchased from Shanghai Yuanye BioTechnology Co., Ltd., (Shanghai, China), and the concentration of the original solution prepared with dimethyl sulfoxide (DMSO) (American, Sigma) was 100 mmol/L. In order to ensure that the survival of cells was not affected, the final concentration of DMSO should not exceed 0.1%.
2.6.2. Cell Cultures
The murine macrophage line RAW264.7 cell and human NSCLC cell lines H1975 cells were obtained from Cell Resource Center, Shanghai Institutes for Biological Sciences, and CAS. RAW264.7 and H1975 cells were cultured in DMEM and RPMI 1640 (Gibco, USA) medium, respectively. Supplemented with 10% heat inactivated foetal bovine serum (FBS) and antibiotics (100 units/mL penicillin and 100 μg/mL streptomycin). Cells were survived in the incubator of 5% CO2 at 37°C. Culture medium was changed every other day.
2.6.3. Establishment of Inflammation Model
RAW264.7 cells were used to construct inflammatory models. Firstly, the cells were cultured in 150 mm Petri dish for 24 hours and treated with drugs for 2 hours. Then, 0.1 μg/mL lipopolysaccharide (LPS) was added to culture for 18 hours. Finally, the cells were collected, and the expression level of inflammatory mediators was detected.
2.6.4. Cell Cytotoxicity Analysis
Determination of cell cytotoxicity was conducted by Cell Counting Kit-8 (CCK-8) assay (Best Bio, Shanghai, China). In brief, H1975 cells were cultured in 96-well plates at a density of 1 × 105 cells/well. After 24-hour training, cells were exposed to different concentrations of apigenin, kaempferol, and ursolic acid. After treatment for 48 h, 10 μL of CCK-8 assay was added to each well, and the cells were hatched for 1–4 h at 37°C and 5% CO2. The absorbance value at 550 nm was surveyed using a microplate reader (Molecular Devices, USA). The cell viability was calculated as: OD of treatment/OD of control × 100%.
2.6.5. Expression Levels of TNF-α and IL-1β
Enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, USA) was used to measure the expression of TNF-α and IL-1β. The cell supernatant after drug treatment was collected according to the protocol of the specification, and 50 μL of the sample was used for detection. The sample concentration was calculated according to the standards provided in the kit.
2.7. Statistical Analysis
Variables were analyzed by Student's t-test and one-way ANOVA and post hoc analysis of variance (GraphPad Prism version 7). Results were reported as mean values S.E. ∗p < 0.05; ∗∗p < 0.01, and ∗∗∗p < 0.001.
3. Results
3.1. Active Compound Screening
To screen out the potential bioactive ingredients of SMK, CIL, and HDW, we appraised the ingredients' ADME properties including OB and DL. As shown in Supporting Information , the results showed that among 156 compounds, 37 compounds reached the standard of OB ≥ 25%, DL ≥ 0.18. It was worth noting that 6 shared compounds met the screening conditions of SMK, CIL, or HDW, such as β-sitosterol, apigenin, luteolin, kaempferol, ursolic acid, and sitogluside-qt, indicating that these active compounds may exhibit effective pharmacological effects on NSCLC. Further, in order to verify whether virtual screening results were consistent with NSCLC, we conducted a literature review of the potential components. Many of the 37 active components had been reported of having significant antitumor and anti-inflammatory effects. For example, β-sitosterol (MOL004, OB = 36.91%, DL = 0.75) induced G0/G1 cell cycle arrest and inhibited cell proliferation in A549 cells [34]. Studies have shown that ursolic acid (MOL074, OB = 37.73%, DL = O.75) induces apoptosis via activation of caspases and phosphorylation of glycogen synthase kinase 3 beta in ovarian cancer cells [35]. Apigenin (MOL009, OB = 45.09, DL = 0.21) was affirmed to inhibit the migration/invasion of NSCLC cells harboring different EGFR statuses via suppressing the Snail/Slug-mediated EMT [36]. These potential compounds may be key components in the treatment of NSCLC.
3.2. Medicine Targeting and Analysis
To explore the target of compounds for NSCLC, we enriched the targets of the compounds. Therefore, we identified 116 targets of these active compounds by means of the WES and SysDT algorithms (as shown in Table 1). The results indicated that most compounds act on more than one target and exhibit multiple pharmacological effects of biologically active molecules. For example, target peroxisome proliferator-activated receptor gamma (PPARG) corresponds to 23 compounds accounting for 62% of the total active compound. Studies have shown that activation of PPARG, γ subtype, could cause proliferation inhibition or differentiation of tumor cells [37]. In addition, elevated coexpression of PTGS2 and NOS2 (51% and 48% of the total compounds, respectively) proteins is a strong predictor of poor survival among cancer patients [38]. Hence, these targets involved in the biological processes of NSCLC will be further researched.
Table 1.
The information of disease-related targets.
| UniProt-ID | Protein names | Gene names | Degree |
|---|---|---|---|
| P03372 | Estrogen receptor | ESR1 | 25 |
| P04150 | Glucocorticoid receptor | NR3C1 | 13 |
| P05067 | Amyloid-beta A4 protein | APP | 15 |
| P06401 | Progesterone receptor | PGR | 4 |
| P06746 | DNA polymerase beta | POLB | 4 |
| P10275 | Androgen receptor | AR | 27 |
| P10636 | Microtubule-associated protein tau | MAPT | 13 |
| P11413 | Glucose-6-phosphate 1-dehydrogenase | G6PD | 13 |
| P11473 | Vitamin D3 receptor | VDR | 13 |
| P37231 | Peroxisome proliferator-activated receptor gamma | PPARG | 23 |
| Q08828 | Adenylate cyclase type 1 | ADCY1 | 12 |
| Q13887 | Krueppel-like factor 5 | KLF5 | 1 |
| Q9NYA1 | Sphingosine kinase 1 | SPHK1 | 3 |
| Q9UBM7 | 7-dehydrocholesterol reductase | DHCR7 | 14 |
| P00915 | Carbonic anhydrase 1 | CA1 | 6 |
| P00918 | Carbonic anhydrase 2 | CA2 | 17 |
| P04798 | Cytochrome P450 1A1 | CYP19A1 | 11 |
| Q07973 | 1,25-dihydroxyvitamin D(3) 24-hydroxylase, mitochondrial | CYP24A1 | 5 |
| Q92731 | Estrogen receptor beta | ESR2 | 18 |
| O15439 | Multidrug resistance-associated protein 4 | ABCC4 | 4 |
| O15118 | NPC intracellular cholesterol transporter 1 | NPC1 | 4 |
| Q96RI1 | Bile acid receptor | NR1H4 | 4 |
| Q12908 | Ileal sodium/bile acid cotransporter | SLC10A2 | 6 |
| P51449 | Nuclear receptor ROR-gamma | RORC | 4 |
| O75751 | Solute carrier family 22 member 3 | SLC22A3 | 5 |
| P04278 | Sex hormone-binding globulin | SHBG | 5 |
| Q12772 | Sterol regulatory element-binding protein 2 | SREBF2 | 4 |
| P02774 | Vitamin D-binding protein | GC | 2 |
| O95622 | Adenylate cyclase type 5 | ADCY5 | 13 |
| P04798 | Cytochrome P450 1A1 | CYP1A1 | 12 |
| P05091 | Aldehyde dehydrogenase, mitochondrial | ALDH2 | 11 |
| P05177 | Cytochrome P450 1A2 | CYP1A2 | 10 |
| P07900 | Heat shock protein HSP 90-alpha | HSP90AA1 | 16 |
| P09917 | Arachidonate 5-lipoxygenase | ALOX5 | 13 |
| P11309 | Serine/threonine-protein kinase pim-1 | PIM1 | 15 |
| P18031 | Tyrosine-protein phosphatase non-receptor type 1 | PTPN1 | 18 |
| P19438 | Tumor necrosis factor receptor superfamily member 1A | TNFRSF1A | 9 |
| P23219 | Prostaglandin G/H synthase 1 | PTGS1 | 14 |
| P24941 | Cyclin-dependent kinase 2 | CDK2 | 14 |
| P33527 | Multidrug resistance-associated protein 1 | ABCC1 | 14 |
| P35228 | Nitric oxide synthase, inducible | NOS2 | 18 |
| P35354 | Prostaglandin G/H synthase 2 | PTGS2 | 19 |
| P36888 | Receptor-type tyrosine-protein kinase FLT3 | FLT3 | 7 |
| P47989 | Xanthine dehydrogenase/oxidase (includes xanthine dehydrogenase) | XDH | 12 |
| P48736 | Phosphatidylinositol 4,5-bisphosphate 3-kinase catalytic subunit gamma isoform | PIK3CG | 9 |
| P49841 | Glycogen synthase kinase-3 beta | GSK3B | 15 |
| P68400 | Casein kinase II subunit alpha | CSNK2A1 | 4 |
| Q00534 | Cyclin-dependent kinase 6 | CDK6 | 12 |
| Q12791 | Calcium-activated potassium channel subunit alpha-1 | KCNMA1 | 4 |
| Q12882 | Dihydropyrimidine dehydrogenase [NADP(+)] | DPYD | 4 |
| Q16539 | Mitogen-activated protein kinase 14 | MAPK14 | 15 |
| Q16678 | Cytochrome P450 1B1 | CYP1B1 | 14 |
| Q9BVA1 | Tubulin beta-2B chain | TUBB2B | 15 |
| Q9UNQ0 | ATP-binding cassette subfamily G member 2 | ABCG2 | 13 |
| Q9Y263 | Phospholipase A-2-activating protein | PLAA | 12 |
| P00519 | Tyrosine-protein kinase ABL1 | ABL1 | 7 |
| P35869 | Aryl hydrocarbon receptor | AHR | 8 |
| O43570 | Carbonic anhydrase 12 | CA12 | 18 |
| P51679 | C-C chemokine receptor type 4 | CCR4 | 10 |
| P13569 | Cystic fibrosis transmembrane conductance regulator | CFTR | 2 |
| P16220 | Cyclic AMP-responsive element-binding protein 1 | CREB1 | 12 |
| P53355 | Death-associated protein kinase 1 | DAPK1 | 11 |
| P60568 | Interleukin-2 | IL2 | 18 |
| P51812 | Ribosomal protein S6 kinase alpha-3 | RPS6KA3 | 11 |
| P43405 | Tyrosine-protein kinase SYK | SYK | 4 |
| Q04760 | Lactoylglutathione lyase | GLO1 | 15 |
| P08183 | Multidrug resistance protein 1 | ABCB1 | 12 |
| P14174 | Macrophage migration inhibitory factor | MIF | 3 |
| P15559 | NAD(P)H dehydrogenase [quinone] 1 | NQO1 | 6 |
| O14746 | Telomerase reverse transcriptase | TERT | 11 |
| P02766 | Transthyretin | TTR | 12 |
| P15692 | Vascular endothelial growth factor A | VEGFA | 17 |
| P00734 | Prothrombin | F2 | 9 |
| P08514 | Integrin alpha-IIb | ITGA2B | 2 |
| P08842 | Steryl-sulfatase | STS | 3 |
| P15090 | Fatty acid-binding protein, adipocyte | FABP4 | 2 |
| P28223 | 5-hydroxytryptamine receptor 2A | HTR2A | 8 |
| Q16790 | Carbonic anhydrase 9 | CA9 | 8 |
| P05230 | Fibroblast growth factor 1 | FGF1 | 7 |
| P09038 | Fibroblast growth factor 2 | FGF2 | 7 |
| P10145 | Interleukin-8 | CXCL8 | 1 |
| P09382 | Galectin-1 | LGALS1 | 2 |
| P17931 | Galectin-3 | LGALS3 | 4 |
| P01112 | GTPase HRas | HRAS | 1 |
| P14679 | Tyrosinase | TYR | 9 |
| P08253 | 72 kDa type IV collagenase | MMP2 | 4 |
| P08254 | Stromelysin-1 | MMP3 | 4 |
| P09874 | Poly [ADP-ribose] polymerase 1 | PARP1 | 2 |
| P14780 | Matrix metalloproteinase-9 | MMP9 | 4 |
| P24864 | G1/S-specific cyclin-E1 | CCNE1 | 4 |
| P39900 | Macrophage metalloelastase | MMP12 | 4 |
| O60285 | NUAK family SNF1-like kinase 1 | NUAK1 | 6 |
| P37840 | Alpha-synuclein | SNCA | 5 |
| P11712 | Cytochrome P450 2C9 | CYP2C9 | 3 |
| P51684 | C-C chemokine receptor type 6 | CCR6 | 2 |
| P27695 | DNA-(apurinic or apyrimidinic site) lyase | APEX1 | 4 |
| P11388 | DNA topoisomerase 2-alpha | TOP2A | 5 |
| O60218 | Aldo-keto reductase family 1 member B10 | AKR1B10 | 9 |
| P25116 | Proteinase-activated receptor 1 | F2R | 5 |
| P43681 | Neuronal acetylcholine receptor subunit alpha-4 | CHRNA4 | 4 |
| P63151 | Serine/threonine-protein phosphatase 2A 55 kDa regulatory subunit B alpha isoform | PPP2R2A | 3 |
| Q04206 | Transcription factor p65 | RELA | 3 |
| P14867 | Gamma-aminobutyric acid receptor subunit alpha-1 | GABRA1 | 3 |
| P06881 | Calcitonin gene-related peptide 1 | CALCA | 1 |
| P13501 | C-C motif chemokine 5 | CCL5 | 1 |
| P32245 | Melanocortin receptor 4 | MC4R | 1 |
| P68104 | Elongation factor 1-alpha 1 | EEF1A1 | 3 |
| Q13822 | Ectonucleotide pyrophosphatase/phosphodiesterase family member 2 | ENPP2 | 3 |
| Q9Y251 | Heparanase | HPSE | 3 |
| P53985 | Monocarboxylate transporter 1 | SLC16A1 | 2 |
| P11509 | Cytochrome P450 2A6 | CYP2A6 | 3 |
| Q15788 | Nuclear receptor coactivator 1 | NCOA1 | 1 |
| Q99814 | Endothelial PAS domain-containing protein 1 | EPAS1 | 3 |
| P00533 | Epidermal growth factor receptor | EGFR | 4 |
| Q16665 | Hypoxia-inducible factor 1-alpha | HIF1A | 2 |
| P40926 | Malate dehydrogenase, mitochondrial | MDH2 | 2 |
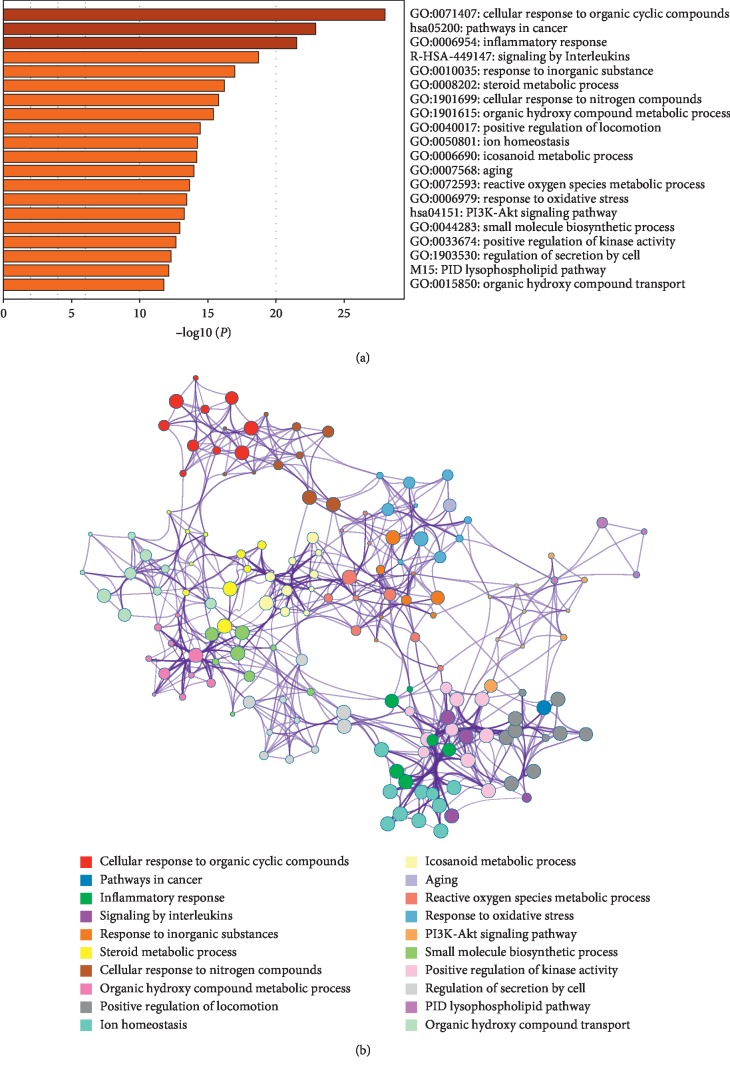
3.3. Pathway and Process Enrichment Analyses
Next, we used Metacape software to enrich and analyze the gene ontology (GO) of proteins targeting potential bioactive components to verify whether these proteins are related to NSCLC and to set threshold of P value ≤0.05. As shown in Figure 1, we discovered that they all participate in the biological processes such as “cellular response to organic cyclic compound,” “inflammatory response,” “response to inorganic substance,” and “cellular response to nitrogen compound”. Thus, the targets of active molecules we filter from the compound Liuju formula could be regarded as the NSCLC therapeutic targets.
Figure 1.
Pathway and process enrichment analyses of the potential targets. (a) Heatmap of enriched terms across input gene lists, colored by p values. (b) Network of enriched terms: colored by cluster ID, where nodes that share the same cluster ID are typically close to each other.
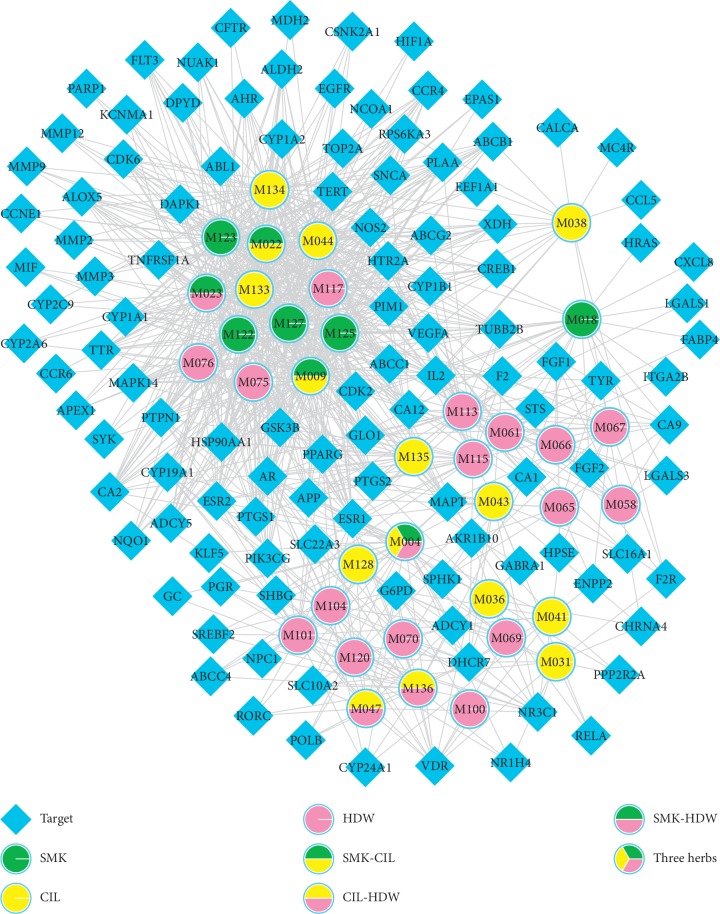
3.4. Compound-Target Network Analysis
In this section, we used Cytoscape 3.6.0 to generate the C-T relation network diagram (Figure 2) which contains 950 interactions between 37 molecules and 116 targets to reveal the relationship between the target and the compound more directly. Subsequently, the C-T network topology analysis showed that the average degree of the compound was 31 and the average target degree was 8, respectively. This may mean that each active compound is associated with multiple targets and all play key roles in disease mechanisms.
Figure 2.
Compound-target network. A compound node and a protein node are linked if the protein is targeted by the corresponding compound. Node size is proportional to its degree.
Notably, apigenin (MOL009, Degree = 51) effectively suppressed lung cancer progression by targeting the CD26-Akt-Snail/Slug signaling pathway [36]. And, the research indicated that kaempferol (MOL023, degree = 48) increased tumor cell killing effect through inhibition of the AKT/PI3K and ERK pathways [39]. Also, ursolic acid (MOL047, Degree = 14) was one of the action components that was present in extracts of CIL and HDW. In recent years, anticancer, anti-inflammation, and regulating immune cell effects of ursolic acid have been discovered [40–42]. Therefore, these three ingredients with a high degree play crucial roles in NSCLC treatment. Significantly, prostaglandin-endoperoxide synthase 2 (PTGS2, Degree = 19) has been found to be highly expressed in many cancer types, and it contributes to tumorigenesis via the inhibition of apoptosis, increased angiogenesis, and invasiveness [43]. All these suggest that compounds probably treat NSCLC by inhibition of tumor cell cycle, anti-inflammation, and inhibiting tumor angiogenesis.
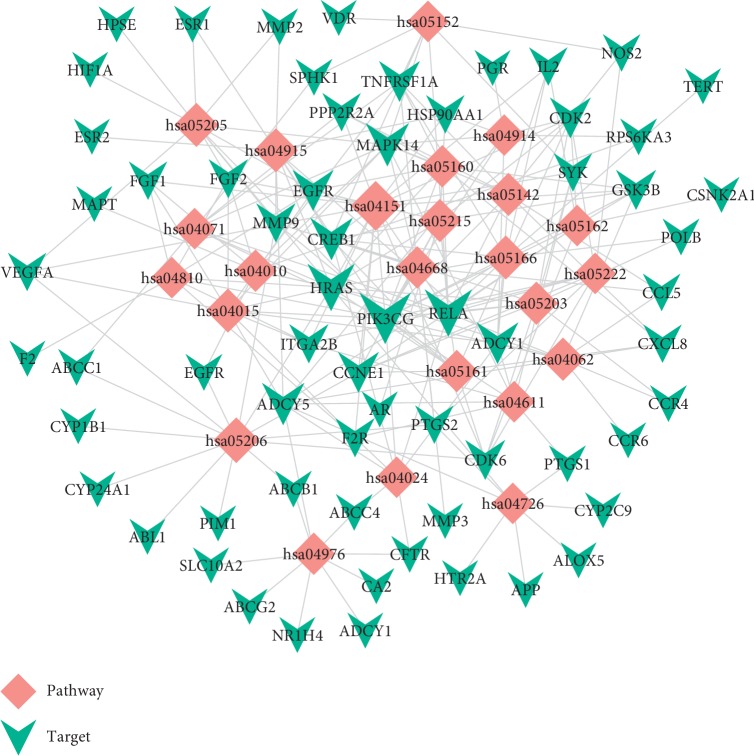
3.5. Target-Pathway Network Analysis
The results are shown in Table 2; the 24 dramatically enriched pathways (p value ≤0.05, multiple targets ≥8) may be the main pathway of action and play a key role in NSCLC disease. As shown in Figure 3, the T-P network includes 88 nodes (64 targets and 24 pathways) and 232 edges. Meanwhile, numerous pathways are regulated by multiple target proteins, which might be the main factor contributing to the anti-NSCLC effect of the herbal formula for NSCLC. pathways in cancer (p value = 7.7 ∗ 10(−12), hsa05200, degree = 28), PI3K-Akt signaling pathway (p value = 1.0 ∗ 10(−5), hsa04151, degree = 18), MicroRNAs in cancer (p value = 1.0 ∗ 10(−3), hsa05206, degree = 13), Proteoglycans in cancer (p value = 7.2 ∗ 10(−4), hsa05205, degree = 11), and TNF signaling pathway (p value = 1.7 ∗ 10(−4), hsa04668, degree = 9) may be crucial pathways. For instance, the PI3K-AKT pathway may be a key pathway regulating the proliferation and apoptosis of NSCLC cells [44]. Meanwhile, the activation of TNF signaling by inflammatory signaling plays an important role in the development of tumors [45]. Also, heparin sulfate proteoglycans (HSPGs) in the proteoglycans in cancer pathway are key components of the extracellular matrix that mediate cell proliferation, invasion, and cell signaling [46, 47]. Therefore, tumor invasion is an important process of tumor growth and metastasis. So, we infer that the compound activates multiple signaling pathways to inhibit inflammation, enhance immune response, and delay invasion of NSCLC. It is noteworthy that the multitarget enrichment of these pathways provides further theoretical support for the treatment of NSCLC.
Table 2.
The information of disease-related pathways.
| Term | Pathways | Degree |
|---|---|---|
| hsa05200 | Pathways in cancer | 28 |
| hsa04151 | PI3K-AKT signaling pathway | 18 |
| hsa05206 | MicroRNAs in cancer | 13 |
| hsa04915 | Estrogen signaling pathway | 11 |
| hsa05205 | Proteoglycans in cancer | 11 |
| hsa04015 | Rap1 signaling pathway | 11 |
| hsa05166 | HTLV-I infection | 11 |
| hsa05215 | Prostate cancer | 10 |
| hsa05142 | Chagas disease (American trypanosomiasis) | 10 |
| hsa04062 | Chemokine signaling pathway | 10 |
| hsa05203 | Viral carcinogenesis | 10 |
| hsa04976 | Bile secretion | 9 |
| hsa04668 | TNF signaling pathway | 9 |
| hsa05160 | Hepatitis C | 9 |
| hsa05161 | Hepatitis B | 9 |
| hsa04010 | MAPK signaling pathway | 9 |
| hsa05222 | Small-cell lung cancer | 8 |
| hsa04914 | Progesterone-mediated oocyte maturation | 8 |
| hsa04726 | Serotonergic synapse | 8 |
| hsa04071 | Sphingolipid signaling pathway | 8 |
| hsa04611 | Platelet activation | 8 |
| hsa05162 | Measles | 8 |
| hsa05152 | Tuberculosis | 8 |
| hsa04024 | cAMP signaling pathway | 8 |
| hsa04810 | Regulation of actin cytoskeleton | 8 |
Figure 3.
Target-pathway network. The T-P network is built by a target and a pathway if the pathway is lighted at the target. Node size is proportional to its degree.
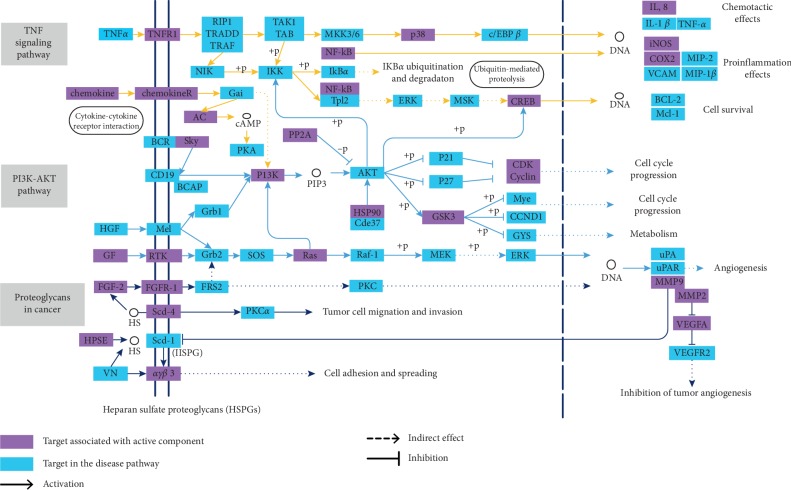
3.6. NSCLC Disease Pathway Analysis
To explain the therapeutic mechanism of the active ingredients at the pathway level, based on the target pathway information obtained in the KEGG database, the key pathways obtained from the T-P network analysis were integrated to construct a complete “NSCLC pathway.” As shown in Figure 4, the “NSCLC pathway” includes three signaling pathways, hsa04151: PI3K-Akt signaling pathway, hsa05205: polysaccharide in cancer, and hsa04668: TNF signaling pathway. The integrated pathway reflects multiple modules such as cell proliferation, apoptosis, angiogenesis, and migration.
Figure 4.
The integrated NSCLC pathway for compound Liuju formula.
3.6.1. Cell Cycle Progression Module
PI3K-AKT pathway and TNF signaling pathway are involved in regulating the cell cycle progress. As we mentioned in Figure 4, apigenin (MOL009) was observed to affect cyclin-dependent kinase 2 (CDK2). It plays a key role in cell cycle progression which could accelerate the transition from G1 to S phase, and the dysregulation of CDK2 is closely related to many cancers [48]. Besides, luteolin (MOL022) was predicted to impact the heat shock protein 90 (HSP90), which regulates DNA methyltransferase transcription and silences tumor suppressor and DNA repair gene methylation in tumor development, growth, and therapeutic response plays an important role [49]. Above results indicate that the compound can effectively regulate the expression of PI3K, CDK/cyclin, GSK3, and other genes, thereby activating the pathway and regulating the cell cycle progression.
3.6.2. Inflammation Effects Module
Inflammatory mediators and inflammatory cells are important components of tumor microenvironment and play an important role in the occurrence, development, and metastasis of tumor [50]. Hence, anti-inflammatory is an integral strategy for the compound treatment. As an important indicator of inflammation, the transcription factor p65 (NF-κB) reduces the expression of the downstream protein prostaglandin G/H synthase 2 (COX-2) and nitric oxide synthase (iNOS) by activated luteolin (MOL022) [51]. Studies have shown that COX2 may be affected by systemic inflammation, and the prognostic impact of COX2 expression depends on tumor characteristics [52]. Also, iNOS is the main mediator of inflammation, and iNOS can enhance inflammation and plays an important role in apoptosis [53]. Therefore, the analysis showed that the compound alleviated the symptoms of inflammatory disorders in patients with NSCLC by regulating the anti-inflammatory activities of NF-κB, cox-2, and iNOS.
3.6.3. Invasion Module
Invasion and metastasis of tumor cells are critical to the development of tumors and exacerbate the progression of tumors. In the “NSCLC pathway” shown in Figure 4, the polysaccharide in cancer pathway was involved in regulating the invasion and metastasis progress. Research have shown that tumor cells migration was associated with an increase of αγβ3 (MOL022, luteolin) integrin proteasome degradation [54, 55]. Meanwhile, FGF2, also known as basic fibroblast growth factor (bFGF) and FGF-β, is a growth factor and signaling protein encoded by the FGF2 gene. It was involved in a variety of biological processes, including cell growth, tissue repair, angiogenesis, tumor growth, and invasion [56, 57]. In addition, VEGFA was modulated by apigenin (MOL009) and luteolin (MOL022). It has been reported in literature that VEGFA has many functions such as increasing vascular permeability, inducing angiogenesis, angiogenesis and endothelial cell growth, promoting cell migration, and inhibiting apoptosis [58–60]. Thus, these above analyses show that compound may treat NSCLC by regulating the angiogenesis, migration, and invasion.
3.7. In Vitro Experimental Detection
3.7.1. Cell Cytotoxicity Assay
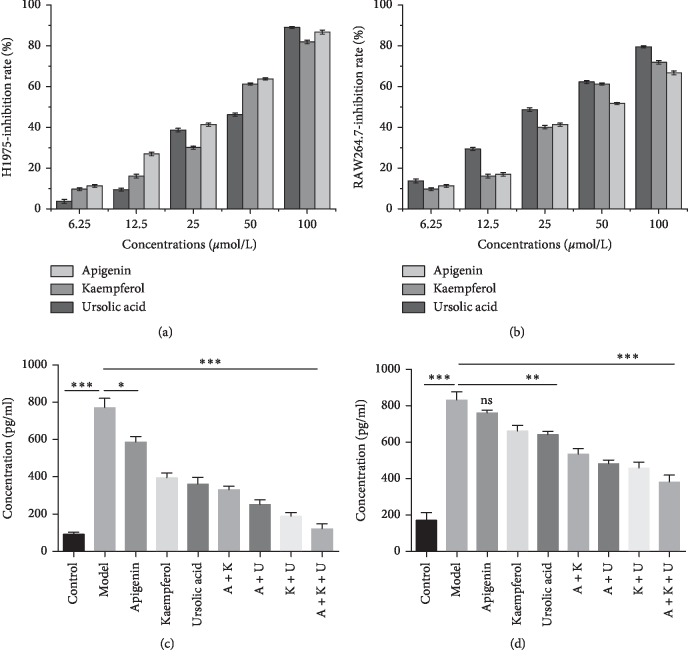
In this section, we used H1975 cell line to verify the compound efficacy. We selected three highly active multitarget components apigenin (MOL009), kaempferol (MOL023) and ursolic acid (MOL047) common to three plants described above for further verification. We used different concentrations of medicine concentration to detect the cytotoxicity of apigenin, kaempferol, and ursolic acid on H1975 and RAW264.7 cell and explored its inhibition rate. The results of cellular cytotoxicity assay (Figures 5(a) and 5(b)) showed that different concentrations of active ingredients significantly inhibited the growth of H1975 and RAW264.7 cells. These results demonstrated that apigenin, kaempferol, and ursolic acid had obvious proliferation inhibition activity on cancer cells.
Figure 5.
Effect of compound Liuju formula active component at the cellular level. (a, b) Cellular cytotoxicity assay. The x-axis shows the drugs concentrations. The y-axis shows the inhibition rate of drugs on cells. (c, d) Effect of apigenin, kaempferol, and ursolic acid on LPS-induced production of inflammatory mediators. Expression levels TNF-α and IL-1β in RAW264.7 cells: experience group cells treated with different dose medicines and analyzed by ELISA. A + K: apigenin and kaempferol; A + U: apigenin and ursolic acid; K + U: kaempferol and ursolic acid; A + K + U: apigenin, kaempferol, and ursolic acid. Data are presented as the mean ± SD (n = 3). ∗p < 0.05, ∗∗p < 0.01, and ∗∗∗p < 0.001.
3.7.2. Expression Levels of TNF-α and IL-1β
To further confirm the anti-inflammatory activity of apigenin, kaempferol, and ursolic acid, we used RAW264.7 macrophages which were treated by LPS, with or without apigenin, kaempferol, and ursolic acid. Based on previous toxicity results, we chose a dose of 20 μM for further test. Therefore, we examined TNF-α and IL-1β by ELISA, whose results demonstrated that the apigenin, kaempferol, and ursolic acid can downregulate the levels of TNF-α. The combination of drugs is more effective, especially in the three coadministered groups (Figures 5(c) and 5(d)). It is worth noting that the expression of IL-1β was not as obvious as TNF-α, and the apigenin group was not different from the model group. However, compared with the model group, the expression level of the combined group was significantly reduced. In summary, the results of two groups showed that the combined group was better than the single drug group, and the combination of three drugs was the most obvious one with significant differences.
4. Discussion
With increasing incidence and mortality, lung cancer has become the most common cancer and the leading cause of cancer death [61]. In addition, high metastatic rate of lung cancer and its poor prognosis leading to the search for antilung cancer drugs has become an important issue to be solved.
Hence, in this study, we chose compound Liuju formula, a clinically used Chinese medicine compound, as an example to interpret the combination effect of Traditional Chinese Medicine treatment. In order to further reveal the potential action mechanism of active compounds in Traditional Chinese Medicine formulas, we proposed a systematic pharmacological approach to gain a deeper understanding of the synergistic pharmacological mechanisms of compound Liuju formula. Firstly, based on the evaluation method, 37 active ingredients were obtained, and 116 potential disease-related targets were predicted. The results showed that the compound Liuju formula has the characteristics of multicomponent and multitarget synergistic treatment. Then, active compounds and C-T analysis showed that several active compounds in the compound Liuju formula are essential for the treatment of NSCLC, including apigenin, kaempferol, and ursolic acid. Moreover, some targets such as CDK2, COX2, iNOS, and VEGF have anti-inflammatory, antimigration, and antiproliferation effects on NSCLC. In addition, the result of pathway and process enrichment analyses, T-P analyses, and the integrated “NSCLC pathway” suggest that compound Liuju formula mainly treats NSCLC by regulating cellular process, inflammatory response, migration, and invasion. Finally, we have shown that apigenin, kaempferol, ursolic acid has obvious anti-proliferative effect on lung cancer cells by in vitro cytotoxicity test results. Furthermore, we determined by ELISA kit that apigenin, kaempferol, and ursolic acid have significant anti-inflammatory effects, especially in the combination treatment group, confirming the synergistic effect between apigenin, kaempferol, and ursolic acid. The formula has a promoting effect on the regulation of tumor inflammatory microenvironment and has a potential research value in the treatment of NSCLC.
In summary, the systems pharmacology method reveals the characteristics of compound Liuju formula with multicomponent Chinese medicine treatment and multitarget effective treatment. And, this strategy provides a potential method for the rational discovery of new medicines.
However, the current methods of systems pharmacology are still in the early stage of development, and the content of the platform needs to be further enriched. Some models, such as ADME screening, need to be optimized, and some database bases should be expanded and updated. And, developing new algorithms, adding more drug-like properties, and improving screening accuracy could enrich the content of the platform. Moreover, the inhibitory effect on the lung cancer of compound Liuju formula was investigated by us in the study, and then we can carry out systems pharmacology prediction on other diseases and other malignant cancers in in-depth exploration. A more comprehensive therapeutic effect of compound Liuju formula would be developed and may contribute new strategies to cancer therapy.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (nos. U1603285 and 81803960).
Contributor Information
Wei Xiao, Email: xw_kanion@163.com.
Yonghua Wang, Email: yh_wang@nwsuaf.edu.cn.
Yan Li, Email: yanli@dlut.edu.cn.
Data Availability
The data such as active constituent ADME parameters, disease-related targets, and disease-related pathways to support the findings of this study are included within the article. The data such as compound structure, pathway and process enrichment analyses, compound-target network, Target-Pathway network, and the integrated NSCLC pathway used to support the findings of this study are included within the supplementary information file. The cellular level effect data used to support the findings of this study are available from the corresponding author upon request because part of the data for this result is included in the mentor's fund project, and it is temporarily not suitable for disclosure.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Y. L. conceived and designed the study. X. S., M. J., and X. T. C. carried out target prediction and analysis. Y. P. L. and J. L. Z. performed network building and analysis. X. S. and M. J. carried out experiments and acquisition of data. X. S., C. L. Z., and J. Z. analyzed and interpreted the data. W. X. provided financial support. Y. L. and Y. H. W. approved the final version of the manuscript.
Supplementary Materials
Supplementary Figure 1: Graphical Abstract. Table 1: Active constituents and their corresponding ADME parameters.
References
- 1.Han M.-l., Zhao Y.-f., Tan C.-h., et al. Cathepsin L upregulation-induced EMT phenotype is associated with the acquisition of cisplatin or paclitaxel resistance in A549 cells. Acta Pharmacologica Sinica. 2016;37(12):1606–1622. doi: 10.1038/aps.2016.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou S.-F., Pan S.-T., Zhou Z.-W., et al. Proteomic response to 5,6-dimethylxanthenone 4-acetic acid (DMXAA, vadimezan) in human non-small cell lung cancer A549 cells determined by the stable-isotope labeling by amino acids in cell culture (SILAC) approach. Drug Design, Development and Therapy. 2015;2015:937–968. doi: 10.2147/DDDT.S76021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu L., Wei S. Research progress of KRAS mutation in non-small cell lung cancer. Chinese Journal of Lung Cancer. 2018;21(5):419–424. doi: 10.3779/j.issn.1009-3419.2018.05.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keith R. L., Miller Y. E. Lung cancer chemoprevention: current status and future prospects. Nature Reviews Clinical Oncology. 2013;10(6):334–343. doi: 10.1038/nrclinonc.2013.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siegel R. L., Miller K. D., Jemal A. Cancer statistics, 2015. CA: A Cancer Journal for Clinicians. 2015;65(1):5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 6.Chen S. L., Jiang J.-G. Application of gene differential expression technology in the mechanism studies of nature product-derived drugs. Expert Opinion on Biological Therapy. 2012;12(7):823–839. doi: 10.1517/14712598.2012.683858. [DOI] [PubMed] [Google Scholar]
- 7.Morita N., Shimizu M., Arisawa M., Kitanaka S. Studies on medicinal resources. XXXV. The components of salix plants (salicaceae) in Japan. (2) the components of the leaves of salix matsudana KOIDZ. f.tortuosa REHD., and S.gilgiana SEEMEN. Yakugaku Zasshi. 1974;94(7):875–877. doi: 10.1248/yakushi1947.94.7_875. [DOI] [PubMed] [Google Scholar]
- 8.Zhang J., Zhang J. N., Han L. K. Studies on chemical constituents of leaves of Salix matsudana Koidz and their influence on lipolysis. Zhongguo Zhong Yao Za Zhi = Zhongguo Zhongyao Zazhi = China Journal of Chinese Materia Medica. 2000;25(9):538–541. [PubMed] [Google Scholar]
- 9.Kim C., Kim M.-C., Kim S.-M., et al. Chrysanthemum indicum L. extract induces apoptosis through suppression of constitutive STAT3 activation in human prostate cancer DU145 cells. Phytotherapy Research. 2013;27(1):30–38. doi: 10.1002/ptr.4689. [DOI] [PubMed] [Google Scholar]
- 10.Lee H. J., Seo H. S., Ryu J., Yoon Y. P., Park S. H., Lee C. J. Luteolin inhibited the gene expression, production and secretion of MUC5AC mucin via regulation of nuclear factor kappa B signaling pathway in human airway epithelial cells. Pulmonary Pharmacology & Therapeutics. 2015;31:117–122. doi: 10.1016/j.pupt.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 11.Kuo Y.-J., Yang J.-S., Lu C.-C., Chiang S.-y., Lin J.-G., Chung J.-G. Ethanol extract of hedyotis diffusawilld upregulates G0/G1 phase arrest and induces apoptosis in human leukemia cells by modulating caspase cascade signaling and altering associated genes expression was assayed by cDNA microarray. Environmental Toxicology. 2015;30(10):1162–1177. doi: 10.1002/tox.21989. [DOI] [PubMed] [Google Scholar]
- 12.Ideker T., Krogan N. J. Differential network biology. Molecular Systems Biology. 2014;8(1):p. 565. doi: 10.1038/msb.2011.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hopkins A. L. Network pharmacology. Nature Biotechnology. 2007;25(10):1110–1111. doi: 10.1038/nbt1007-1110. [DOI] [PubMed] [Google Scholar]
- 14.Nicholson J. K., Lindon J. C. Metabonomics. Nature. 2008;455(7216):1054–1056. doi: 10.1038/4551054a. [DOI] [PubMed] [Google Scholar]
- 15.Huang C., Zheng C., Li Y., Wang Y., Lu A., Yang L. Systems pharmacology in drug discovery and therapeutic insight for herbal medicines. Briefings in Bioinformatics. 2013;15(5):710–733. doi: 10.1093/bib/bbt035. [DOI] [PubMed] [Google Scholar]
- 16.Zheng C., Pei T., Huang C., et al. A novel systems pharmacology platform to dissect action mechanisms of traditional Chinese medicines for bovine viral diarrhea disease. European Journal of Pharmaceutical Sciences. 2016;94:33–45. doi: 10.1016/j.ejps.2016.05.018. [DOI] [PubMed] [Google Scholar]
- 17.Wang X., Xu X., Tao W., Li Y., Wang Y., Yang L. A systems biology approach to uncovering pharmacological synergy in herbal medicines with applications to cardiovascular disease. Evidence-Based Complementray and Alternative Medicine. 2012;2012:15. doi: 10.1155/2012/519031.519031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ru J., Peng L., Wang J., et al. TCMSP: a database of systems pharmacology for drug discovery from herbal medicines. Journal of Cheminformatics. 2014;6(1):p. 13. doi: 10.1186/1758-2946-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang Y., Huang C., Su X., et al. Deciphering the multicomponent synergy mechanism from a systems pharmacology perspective: application to Gualou Xiebai Decoction for coronary heart disease. Journal of Functional Foods. 2018;47:143–155. doi: 10.1016/j.jff.2018.02.030. [DOI] [Google Scholar]
- 20.Wang X., Xu X., Li Y., et al. Systems pharmacology uncovers Janus functions of botanical drugs: activation of host defense system and inhibition of influenza virus replication. Integrative Biology. 2013;5(2):351–371. doi: 10.1039/c2ib20204b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wishart D. S., Feunang Y. D., Guo A. C., et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Research. 2017;46(1):D1074–D1082. doi: 10.1093/nar/gkx1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hua Y., Chen J., Xue X., et al. A systematic prediction of multiple drug-target interactions from chemical, genomic, and pharmacological data. PLoS One. 2012;7(5) doi: 10.1371/journal.pone.0037608.e37608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zheng C., Guo Z., Huang C., et al. Large-scale direct targeting for drug repositioning and discovery. Scientific Reports. 2015;5(1):p. 11970. doi: 10.1038/srep11970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu C. H., Rolf A., Amos B., et al. The universal protein resource (UniProt): an expanding universe of protein information. Nucleic Acids Research. 2006;34:187–191. doi: 10.1093/nar/gkj161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feng Z., Zhe S., Chu Q., et al. Therapeutic target database update 2012: a resource for facilitating target-oriented drug discovery. Nucleic Acids Research. 2012;40(1):1128–1136. doi: 10.1093/nar/gkr797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis A. P., Grondin C. J., Johnson R. J., et al. The comparative toxicogenomics database: update 2017. Nucleic Acids Research. 2019;45(1):D972–D978. doi: 10.1093/nar/gky868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorn C. F., Klein T. E., Altman R. B. Methods in Molecular Biology. Vol. 1015. Totowa, NJ, USA: Humana Press; 2013. PharmGKB: the Pharmacogenomics knowledge base; pp. 311–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kanehisa M., Furumichi M., Tanabe M., Sato Y., Morishima K. KEGG: new perspectives on genomes, pathways, diseases and drugs. Nucleic Acids Research. 2017;45(D1):D353–D361. doi: 10.1093/nar/gkw1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lobert S., Graichen M. E., Hamilton R. D., et al. Prognostic biomarkers for HNSCC using quantitative real-time PCR and microarray analysis: β-tubulin isotypes and the p53 interactome. Cytoskeleton. 2014;71(11):628–637. doi: 10.1002/cm.21195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bindea G., Mlecnik B., Hackl H., et al. ClueGO: a cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics. 2009;25(8):1091–1093. doi: 10.1093/bioinformatics/btp101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu S., Wang G. Bioinformatic analysis reveals CYP2C9 as a potential prognostic marker for HCC and liver cancer cell lines suitable for its mechanism study. Cellular and Molecular Biology. 2018;64(7):70–74. doi: 10.14715/cmb/2018.64.7.12. [DOI] [PubMed] [Google Scholar]
- 32.Liu J., Pei T., Mu J., et al. Systems pharmacology uncovers the multiple mechanisms of xijiao dihuang decoction for the treatment of viral hemorrhagic fever. Evidence-Based Complementary and Alternative Medicine. 2016;2016:17. doi: 10.1155/2016/9025036.9025036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang D. W., Sherman B. T., Lempicki R. A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nature Protocols. 2009;4(1):44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 34.Wang X., Li M., Hu M., Wei P., Zhu W. BAMBI overexpression together with β-sitosterol ameliorates NSCLC via inhibiting autophagy and inactivating TGF-β/Smad2/3 pathway. Oncology Reports. 2017;37(5):3046–3054. doi: 10.3892/or.2017.5508. [DOI] [PubMed] [Google Scholar]
- 35.Song Y.-H., Jeong S.-J., Kwon H.-Y., Kim B., Kim S.-H., Yoo D.-Y. Ursolic acid from oldenlandia diffusa induces apoptosis via activation of caspases and phosphorylation of glycogen synthase kinase 3 beta in SK-OV-3 ovarian cancer cells. Biological & Pharmaceutical Bulletin. 2012;35(7):1022–1028. doi: 10.1248/bpb.b110660. [DOI] [PubMed] [Google Scholar]
- 36.Chang J.-H., Cheng C.-W., Yang Y.-C., et al. Downregulating CD26/DPPIV by apigenin modulates the interplay between Akt and Snail/Slug signaling to restrain metastasis of lung cancer with multiple EGFR statuses. Journal of Experimental & Clinical Cancer Research. 2018;37(1):p. 199. doi: 10.1186/s13046-018-0869-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Langle Y., Lodillinsky C., Belgorosky D., Sandes E. O., Eiján A. M. Role of peroxisome proliferator activated receptor-gamma in bacillus Calmette-Guérin bladder cancer therapy. The Journal of Urology. 2012;188(6):2384–2390. doi: 10.1016/j.juro.2012.07.109. [DOI] [PubMed] [Google Scholar]
- 38.Basudhar D., Glynn S. A., Greer M., et al. Coexpression of NOS2 and COX2 accelerates tumor growth and reduces survival in estrogen receptor-negative breast cancer. Proceedings of the National Academy of Sciences of the United States of America. 2017;114(49):13030–13035. doi: 10.1073/pnas.1709119114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuo W.-T., Tsai Y.-C., Wu H.-C., et al. Radiosensitization of non-small cell lung cancer by kaempferol. Oncology Reports. 2015;34(5):2351–2356. doi: 10.3892/or.2015.4204. [DOI] [PubMed] [Google Scholar]
- 40.Lopes S. C. d. A., Novais M. V. M., Teixeira C. S., et al. Preparation, physicochemical characterization, and cell viability evaluation of long-circulating and pH-sensitive liposomes containing ursolic acid. BioMed Research International. 2013;2013:7. doi: 10.1155/2013/467147.467147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ruan J. S., Zhou H., Yang L., et al. Ursolic acid attenuates TGF-β1 induced epithelial-ymesenchymal transition in NSCLC by targeting integrin αvβ5/MMPs signaling. Oncology Research Featuring Preclinical and Clinical Cancer Therapeutics. 2019;27(5):593–600. doi: 10.3727/096504017x15051723858706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jang S.-E., Jeong J.-J., Hyam S. R., Han M. J., Kim D.-H. Ursolic acid isolated from the seed of cornus officinalis ameliorates colitis in mice by inhibiting the binding of lipopolysaccharide to toll-like receptor 4 on macrophages. Journal of Agricultural and Food Chemistry. 2014;62(40):9711–9721. doi: 10.1021/jf501487v. [DOI] [PubMed] [Google Scholar]
- 43.Bertrand J., Liagre B., Ghezali L., Beneytout J.-L., Leger D. Y. Cyclooxygenase-2 positively regulates Akt signalling and enhances survival of erythroleukemia cells exposed to anticancer agents. Apoptosis: An International Journal on Programmed Cell Death. 2013;18(7):836–850. doi: 10.1007/s10495-013-0825-7. [DOI] [PubMed] [Google Scholar]
- 44.Zhou B., Wang D., Sun G., Mei F., Cui Y., Xu H. Effect of miR-21 on apoptosis in lung cancer cell through inhibiting the PI3K/akt/NF-κB signaling pathway in vitro and in vivo. Cellular Physiology and Biochemistry. 2018;46(3):999–1008. doi: 10.1159/000488831. [DOI] [PubMed] [Google Scholar]
- 45.Hildebrandt M. A. T., Roth J. A., Vaporciyan A. A., et al. Genetic variation in the TNF/TRAF2/ASK1/p38 kinase signaling pathway as markers for postoperative pulmonary complications in lung cancer patients. Scientific Reports. 2015;5(1) doi: 10.1038/srep12068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hull E., Montgomery M., Leyva K. Epigenetic regulation of the biosynthesis & enzymatic modification of heparan sulfate proteoglycans: implications for tumorigenesis and cancer biomarkers. International Journal of Molecular Sciences. 2017;18(7):p. 1361. doi: 10.3390/ijms18071361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Okolicsanyi R. K., van Wijnen A. J., Cool S. M., Stein G. S., Griffiths L. R., Haupt L. M. Heparan sulfate proteoglycans and human breast cancer epithelial cell tumorigenicity. Journal of Cellular Biochemistry. 2014;115(5):967–976. doi: 10.1002/jcb.24746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Y., Chen Y., Cheng X., et al. Design, synthesis and biological evaluation of pyrimidine derivatives as novel CDK2 inhibitors that induce apoptosis and cell cycle arrest in breast cancer cells. Bioorganic & Medicinal Chemistry. 2018;26(12):3491–3501. doi: 10.1016/j.bmc.2018.05.024. [DOI] [PubMed] [Google Scholar]
- 49.Nagaraju G. P., Wu C., Merchant N., Chen Z., Lesinski G. B., El-Rayes B. F. Epigenetic effects of inhibition of heat shock protein 90 (HSP90) in human pancreatic and colon cancer. Cancer Letters. 2017;402:110–116. doi: 10.1016/j.canlet.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 50.Guo L., Zhang Y., Zhang L., Huang F., Li J., Wang S. MicroRNAs, TGF-β signaling, and the inflammatory microenvironment in cancer. Tumour Biology. 2016;37(1):115–125. doi: 10.1007/s13277-015-4374-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Natarajan K., Abraham P., Kota R., Isaac B. NF-κB-iNOS-COX2-TNF α inflammatory signaling pathway plays an important role in methotrexate induced small intestinal injury in rats. Food and Chemical Toxicology. 2018;118:766–783. doi: 10.1016/j.fct.2018.06.040. [DOI] [PubMed] [Google Scholar]
- 52.Sano Y., Kogashiwa Y., Araki R., et al. Correlation of inflammatory markers, survival, and COX2 expression in oral cancer and implications for prognosis. Otolaryngology—Head and Neck Surgery. 2018;158(4):667–676. doi: 10.1177/0194599817745284. [DOI] [PubMed] [Google Scholar]
- 53.Nakazawa H., Chang K., Shinozaki S., et al. iNOS as a driver of inflammation and apoptosis in mouse skeletal muscle after burn injury: possible involvement of sirt1 S-nitrosylation-mediated acetylation of p65 NF-κB and p53. PLoS One. 2017;12(1) doi: 10.1371/journal.pone.0170391.e0170391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hsu Y.-L., Wu L.-Y., Hou M.-F., et al. Glabridin, an isoflavan from licorice root, inhibits migration, invasion and angiogenesis of MDA-MB-231 human breast adenocarcinoma cells by inhibiting focal adhesion kinase/Rho signaling pathway. Molecular Nutrition & Food Research. 2011;55(2):318–327. doi: 10.1002/mnfr.201000148. [DOI] [PubMed] [Google Scholar]
- 55.Jing Z., Qiong Z., Yonggang W., Yanping L. Rat bone marrow mesenchymal stem cells improve regeneration of thin endometrium in rat. Fertility and Sterility. 2014;101(2):587–594. doi: 10.1016/j.fertnstert.2013.10.053. [DOI] [PubMed] [Google Scholar]
- 56.Dionne C. A., Crumley G., Bellot F., et al. Cloning and expression of two distinct high-affinity receptors cross-reacting with acidic and basic fibroblast growth factors. The EMBO Journal. 1990;9(9):2685–2692. doi: 10.1002/j.1460-2075.1990.tb07454.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lafage-Pochitaloff M., Galland F., Simonetti J., Prats H., Mattei M. G., Birnbaum D. The human basic fibroblast growth factor gene is located on the long arm of chromosome 4 at bands q26-q27. Oncogene Research. 1990;5(3):241–244. [PubMed] [Google Scholar]
- 58.Jiang H., Toscano J. F., Schiraldi M., et al. Differential expression of vascular endothelial growth factor-A isoforms between intracranial atherosclerosis and moyamoya disease. Journal of Stroke and Cerebrovascular Diseases. 2019;28(2):360–368. doi: 10.1016/j.jstrokecerebrovasdis.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Karaman S., Leppänen V.-M., Alitalo K. Vascular endothelial growth factor signaling in development and disease. Development. 2018;145(14) doi: 10.1242/dev.151019. [DOI] [PubMed] [Google Scholar]
- 60.Song Y., Hu J., Chen Q., et al. Association between vascular endothelial growth factor rs699947 polymorphism and the risk of three major urologic neoplasms (bladder cancer, prostate cancer, and renal cell carcinoma): a meta-analysis involving 11,204 subjects. Gene. 2018;679:241–252. doi: 10.1016/j.gene.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 61.Siegel R. L., Miller K. D., Jemal A. Cancer statistics, 2017. CA: A Cancer Journal for Clinicians. 2017;67(1):7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: Graphical Abstract. Table 1: Active constituents and their corresponding ADME parameters.
Data Availability Statement
The data such as active constituent ADME parameters, disease-related targets, and disease-related pathways to support the findings of this study are included within the article. The data such as compound structure, pathway and process enrichment analyses, compound-target network, Target-Pathway network, and the integrated NSCLC pathway used to support the findings of this study are included within the supplementary information file. The cellular level effect data used to support the findings of this study are available from the corresponding author upon request because part of the data for this result is included in the mentor's fund project, and it is temporarily not suitable for disclosure.