Abstract
Background:
Falls are common and impactful in people with multiple sclerosis (MS) but currently there is no accepted standard of care for fall prevention in MS. Evidence supports that the in-person, group-based, Free from Falls (FFF) program is associated with both immediate and six-month sustained improvements in mobility and balance and a reduction in falls, but program attendance is limited by access to the class at a given time and location and by the cost and availability of trained facilitators. Therefore, we developed and evaluated an online, web-based version of FFF, Free from Falls Online (FFFO).
Methods:
Thirty people with MS who reported falling at least twice in the previous two months were randomized to FFFO or to a control group. FFFO consists of eight weekly sessions, each with an instructional and exercise component. Subjects in the control group were given a brochure on minimizing fall risk, a letter was sent to their treating physician informing them that the subject reported falling, and these subjects were invited to use the FFFO program at study completion. Outcomes included baseline demographics, falls prospectively reported for the eight weeks of intervention and the following three months, and a program satisfaction survey for the active group. Regression models were used to test for associations between treatment group and fall incidence.
Results:
Subjects’ mean age was 55.8 years, 70% were female, 73% had progressive MS, median Expanded Disability Status Scale (EDSS) score was 6.0, and subjects reported a median of two falls in the month prior to study enrollment. Although, in general, regression models demonstrated trends that those in the intervention group were less likely to fall than those in the control group, statistical significance was only achieved (p = 0.0038) with a post hoc model evaluating the relationship between the square of days and the probability of not falling. This model supported that those in the intervention group were slightly less likely to fall than those in the control group. This difference was most prominent in the first month of the study, less prominent in the following month, and not sustained three months following the intervention.
User experience with FFFO was overall positive, with over 75% reporting the web-based program easy to learn and to use, 85% reporting the program was easy to follow, 62% reporting the material to be useful, and 77% finding the exercises to be a useful component of the program.
Conclusion:
This study supports the viability of online delivery of self-management strategies in MS, suggests that FFFO may help prevent falls in people with MS, and provides the preliminary data needed to verify the findings of this pilot study of FFFO with a fully powered randomized controlled trial in people with MS.
Keywords: Accidental falls, Self-management, Internet, Multiple sclerosis, Fall-prevention
1. Introduction
Multiple sclerosis (MS) is a chronic demyelinating disease of the central nervous system that affects over 900,000 people in the United States and 2.5 million people worldwide. MS is the most common non-traumatic cause of disability among young adults (Wallin et al., 2019). The clinical presentation of MS is highly variable and often includes impairments in visual, motor, sensory and cognitive function. Impairments in one, or more commonly several, of these domains are known risk factors for falls (Gianni et al., 2014; Gunn et al., 2013). Studies suggest that around half of people with MS (PwMS) fall at least once in a three-month period and over one-third report multiple falls in a similar time frame (Nilsagard et al., 2009; Nilsagard et al., 2015). Falls in PwMS have a wide range of consequences including physical injury, increased health care utilization and increased fear of falling, which can then result in reduced physical activity, independence, engagement in social activities and quality of life (Matsuda et al., 2011; Gunn et al., 2014).
Currently there is no accepted standard of care for fall prevention in MS. A number of approaches have been used, including exercise, education and multi-component programs, generally with outcomes specific to the intervention (Finlayson et al., 2009; Hugos et al., 2016; Carling et al., 2017; Martini et al., 2018). Studies have shown that, consistent with theories of specificity of learning, programs that incorporate gait and balance exercises and functional training are associated with improved balance outcomes, whereas programs focused on education are associated with improved fall prevention knowledge (Finlayson et al., 2009; Gunn et al., 2015). Based on these findings, the National Multiple Sclerosis Society (NMSS) developed an eight-week, in-person, group-based, comprehensive exercise and education fall prevention program for PwMS called Free from Falls (FFF). An observational study found that FFF attendance was associated with both immediate and 6-month sustained improvements in mobility and balance and a reduction in falls (Hugos et al., 2016). However, access to the FFF program is limited to those who can attend a class at a given time and location and by the cost and availability of trained facilitators
Although older adults may not use the internet as much as younger people (Hunsaker and Hargittai, 2018), the widespread use of the internet by PwMS offers a convenient and potentially sustainable way to address limitations of in-person fall prevention programs for this population. It is estimated that over 90% of PwMS in the United States access the internet at least once a week for topics related to MS, and nearly 60% do so at least twice a week. They use the internet to look for information about MS and associated symptoms, for resources to help cope with the disease, for information regarding the role of physical activity, and they use the internet to access support groups (Lejbkowicz et al., 2010; Marrie et al., 2013). However, younger PwMS use the internet more than older PwMS, possibly because of limited computing and web navigating skills, lack of interest or awareness of heath information on the web, greater disability, including visual, motor and cognitive dysfunction, limiting computer use (Hunsaker and Hargittai, 2018; Altreja et al., 2005; Friemel, 2016). We therefore developed Free from Falls Online (FFFO), a comprehensive web-based fall prevention program based on FFF, with particular attention to barriers for older adults, to provide increased access and availability to self-management strategies to prevent falls in PwMS across all ages.
To address participants’ need for both knowledge and motor skill acquisition, FFFO consists of eight instructional modules, each with a 15 to 30-min webinar and supplementary, downloadable printed materials, and an hour-long exercise video called Building Better Balance. FFFO participants are instructed to watch one instructional module each week and to perform the exercises three to four times each week. The instructional modules address the following eight topics, which are the same as the original FFF topics: (1) fall prevalence and risk factors and the role of exercise in reducing falls; (2) fear of falling and its impact, the role of center of gravity and multisensory training in fall prevention; (3) assistive devices and the role of flexibility in fall prevention; (4) impact and management of fatigue and cognition for fall prevention; (5) home and community safety and the role of functional fitness; (6) environmental modification; (7) fall recovery and compensatory strategies; and (8) developing a fall prevention plan. The Building Better Balance exercise video demonstrates the same exercises as used in the original FFF program, including sections titled: (1) warming up; (2) firming your muscles; (3) fine tuning your senses; (4) balance basics; and (5) cooling down. These exercises use a systems-based approach to motor learning (Woollacott and Shumway-Cook, 1990). The goal of the exercises is to improve balance and posture, develop core and lower limb muscle strength, and optimize flexibility. The slow, methodical pace of each video allows participants to follow along with the program. The exercises are demonstrated by one individual who is independently ambulatory and another who uses bilateral assistance from a walker while the narrator provides instruction to guide performance and progression. Participants are instructed to follow the program in sequence, performing the recommended sets and repetitions; when the exercises are no longer challenging, participants are instructed to increase repetitions and sets.
We specifically designed the FFFO program to meet the needs of PwMS of all ages by minimizing barriers to internet use such as low contrast, small font, cluttering of content and poor navigational design. Specific features to optimize usability include easy access to home and menu pages, consistent navigation elements, use of bullet points rather than paragraphs, generous use of white space, large font and a high contrast color scheme. We then beta tested the program by asking six PwMS with limited internet experience and varying levels of visual and motor disability to access and navigate the program and provide feedback regarding usability. This feedback was used to modify the program to produce the final version of FFFO.
The purpose of this randomized controlled pilot study was to examine the efficacy of FFFO in reducing the frequency of falls and to measure user satisfaction with FFFO. We hypothesized that participants in FFFO would sustain fewer falls than a control group not participating in FFFO and that they would find the program useful and easy to use.
2. Methods
2.1. Procedures
Participants were recruited from the Oregon Health & Science University (OHSU) Multiple Sclerosis Center and the surrounding community between January and August 2017. Inclusion criteria included physician-confirmed diagnosis of MS of any subtype; no MS relapse in the previous month; self-reported history of two or more falls in the previous two months; age over 18 years; ability to walk at least 100 m with or without intermittent or constant unilateral assistance (Expanded Disability Severity Scale (EDSS) step ≤ 6.0); daily access to a computer and willingness to respond to a daily online fall survey. Exclusion criteria included conditions that would preclude reliable participation or increase risk of injury during the program. Eligible participants gave written informed consent to participate. Upon completion of baseline measures, participants were randomized in a 1:1 ratio to the active intervention group or the waitlist control group. All participants continued to receive their usual medical care during this study, without any specific additions or restrictions. Participants in the intervention group began the FFFO program immediately after completion of baseline measures. Participants in the control group were given access to the program at study completion. The OHSU Institutional Review Board approved this study and the study was registered on clinicaltrials.gov ().
2.2. Intervention
Participants in the intervention group were instructed to use the FFFO program for eight weeks, completing one module each week. Participants were asked to review that week’s webinar and supplemental reading material from their home computer. They were also instructed to complete the Building Better Balance exercise program at home at least three times per week. To address safety, the video both narrated and showed in writing the following safety instructions before the exercise program: discuss with your healthcare provider before beginning any exercise program; perform the exercise program in a cool, well-ventilated room; use any needed cooling devices; stay hydrated by drinking water before, during and after the workout; plan flexible rest breaks to avoid excessive fatigue or overheating; listen to your body and adjust the frequency, intensity and duration of the exercise accordingly, and; if the activity aggravates an existing symptom, stop, rest or modify the activity. These safety instructions are the same as those given for the in-person FFF program. The control group received an educational brochure developed by the NMSS called Minimizing Your Risk of Falls: A Guide for People with MS; a letter was sent informing their physician that they reported falling; they were instructed to discuss with their physician any subsequent falls over the course of the study; and, at study completion, were emailed an invitation and a link providing access to FFFO.
2.3. Outcome measures
The primary outcome of this study was prospectively counted falls. All participants recorded their falls daily using a web-based survey developed through REDCap, a secure web application for building and managing online surveys and databases specifically geared to support online or offline data capture for research studies and operations. For the 22 weeks of the study, including the eight weeks of intervention and the following three months, participants received a daily email directing them to a survey asking if they fell that day. Participants were required to respond to this survey on a computer and not on a mobile device. Any time a participants reported falling they were then directed to additional questions asking whether they sustained any fall-related injuries and whether they reported their fall to anyone or received any medical care related to their fall(s). Participants were contacted by phone or email if they failed to respond to the fall survey for seven consecutive days.
Satisfaction with the FFFO program was assessed using a 13-item questionnaire that included questions about website appearance, ease of navigation and organization, relevance and likelihood of sharing information, and perceived value of each FFFO component. All items were rated on a five-point likert scale, from strongly agree to strongly disagree (see Table 2). In addition, there were two free text questions, one asking participants to list the most positive aspects of the program and the other asking them to list the most negative aspects of the program. The questionnaire was administered using REDCap survey and was accessed online via a link sent to the active group eight weeks after study enrollment, when they should have completed all FFFO modules.
Table 2.
Participant evaluation of Free from Falls Online.
| Strongly agree (4) | Agree (3) | Neutral (2) | Disagree (1) | Strongly disagree (0) | |
|---|---|---|---|---|---|
| It was easy to learn how to use the program | 6 (46.1) | 6 (46.1) | 1 (7.7) | 0 | 0 |
| It was easy to use this program | 7 (53.8) | 3 (23.1) | 3 (23.1) | 0 | 0 |
| It was easy to navigate the website | 4 (30.8) | 5 (38.5) | 2 (15.4) | 2 (15.4) | 0 |
| The graphics (images and video) used on the website are appealing | 4 (30.8) | 3 (23.1) | 4 (30.8) | 2 (15.4) | 0 |
| The lectures were informative | 6 (46.1) | 2 (15.4) | 5 (38.5) | 0 | 0 |
| The lectures were easy to follow | 7 (53.8) | 4 (30.8) | 2 (15.4) | 0 | 0 |
| The exercise video contributes to the appeal of the material | 5 (38.5) | 5 (38.5) | 2 (15.4) | 1 (7.7) | 0 |
| The exercise video was easy to follow | 7 (53.8) | 4 (30.8) | 2 (15.4) | 0 | 0 |
| The program has all the functions and capabilities that I expect it to have | 4 (30.8) | 7 (53.8) | 2 (15.4) | 0 | 0 |
| The organization of the information is clear | 4 (30.8) | 8 (61.5) | 0 | 1 (7.7) | 0 |
| The website contains all the information I need about fall prevention | 3 (23.1) | 6 (46.1) | 4 (30.8) | 0 | 0 |
| I would use an online self-management program for other MS symptoms | 6 (46.1) | 4 (30.8) | 2 (15.4) | 1 (7.7) | 0 |
| I would recommend this program to others | 6 (46.1) | 5 (38.5) | 2 (15.4) | 0 | 0 |
Demographic information (age, gender, racial/ethnic background and education level) and questions about MS (MS subtype, self-reported EDSS, falls in the month and year prior to the start of the study, and assistive device use) were collected electronically by self-report from the patient using a REDCap survey at the start of the study.
2.4. Data analysis
All participants who completed at least one post-baseline assessment were included in the analyses, using a modified intent to treat approach. The analyses divided the 22 weeks of calendar-captured fall data into five four-week periods and a sixth period interval of two weeks. We treated days with nothing recorded as days with no falls because, even amongst a population at high risk for falls, there is a high probability that any given day will be free of falls. In addition, a fall is generally a memorable event, and more likely to be recorded by the participant, while not falling is not memorable and is less likely to be recorded.
Analyses of treatment effects were performed using Glimmix on SAS 9.4. In the model we assumed a random intercept effect to account for baseline differences between participants. A repeated measures mixed model, with participants as a random effect, was used to compare change in the number of falls over time across treatment groups, incorporating data from all six time periods.
3. Results
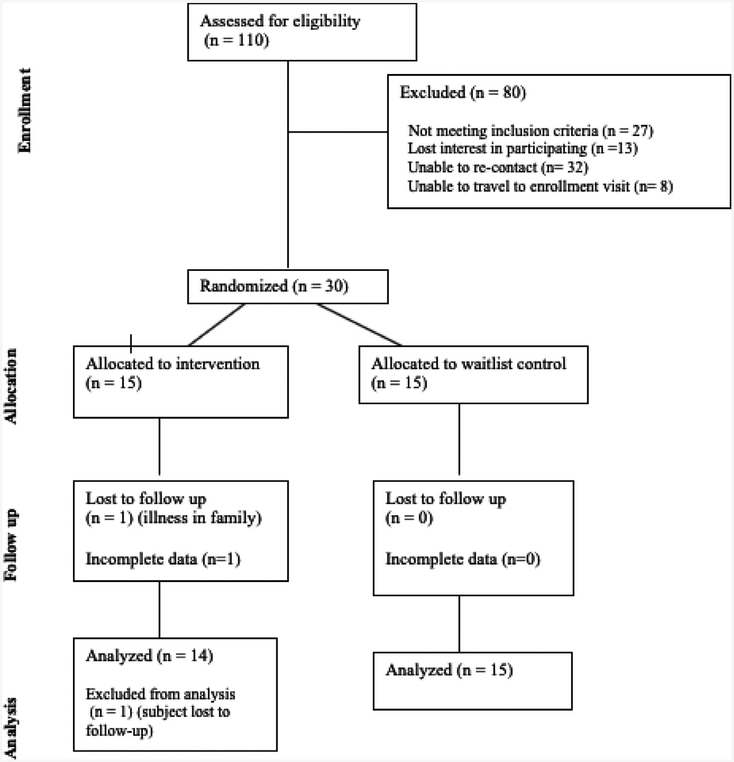
110 people expressed interest in participating in this study and were assessed for eligibility. Of these, 27 did not meet inclusion criteria; eight had transportation issues preventing them from participating in the enrollment visit; 13 lost interest in participating prior to the enrollment visit, and we were unable to re-contact 32 individuals. Thus, 30 participants completed the enrollment visit and were randomized to the active or control group. One participant in the active group was lost to follow-up due to an illness in the family prior to any post baseline measures. Therefore, 14 out of 15 participants from the active group and all 15 participants in the control group were included in the analyses (Fig. 1).
Fig. 1.
Consort diagram for enrollment and group allocation.
3.1. Demographics
The participants’ age range was 32 to 78 years, with a mean of 56 years. Seventy percent were female and 97% were Caucasian. All but one had at least some college education. Most (73%) had either primary-progressive or secondary-progressive MS and most required unilateral assistance for walking (57% had an EDSS score of 6). The number of falls in the month prior to starting the study ranged from zero to seven, with a median of two, and the number of falls in the year prior to starting the study ranged from two to 75, with a median of seven. The active FFFO group was slightly younger than the control group (53 vs 58 years) and had a higher proportion with relapsing versus progressive disease (40% relapsing and 60% progressive: in the active group vs 13% relapsing and 87% progressive in the control group), but none of the differences in demographics between groups were statistically significant (Table 1).
Table 1.
Baseline participant demographic characteristics.
| Characteristic | Active | Control | Total |
|---|---|---|---|
| (n = 15)* | (n = 15) | (n = 30) | |
| Gender, n females (%) | 11 (73.3) | 10 (66.7) | 21 (70.0) |
| Age, n (%) | |||
| Mean | 53.8 (SD | 57.7 (SD | 55.8 (SD |
| 30–39 years | 11.1) | 9.7) | 10.5) |
| 40–49 years | 2 (13.3) | 0 (0) | 2 (6.7) |
| 50–59 years | 3 (20.0) | 4 (26.7) | 7 (23.3) |
| 60–69 years | 4 (26.7) | 3 (20.0) | 7 (23.3) |
| 70–79 years | 6 (40.0) | 7 (46.7) | 13 43.3) |
| 0 (0) | 1 (6.7) | 1 (3.3) | |
| Ethnicity, n Caucasian (%) | 14 (93.3) | 15 (100.0) | 29 (96.7) |
| Education, years (%) | |||
| Completed high | 1 (6.7) | 0 (0.0) | 1 (3.3) |
| school | 4 (26.7) | 6 (40.0) | 10 (33.3) |
| Some college | 2 (13.3) | 7 (46.7) | 9 (30.0) |
| Completed college | 8 (53.3) | 2 (13.3) | 10 (33.3) |
| Graduate school | |||
| MS Subtype n (%) | |||
| Relapsing | 6 (40.0) | 2 (13.3) | 8 (26.7) |
| Secondary | 4 (26.7) | 9 (60.0) | 13 (43.3) |
| Progressive | 5 (33.3) | 4 (26.7) | 9 (30.0) |
| Primary Progressive | |||
| EDSS, n (%) | |||
| Median | 5.5 | 6.0 | 6.0 |
| 3–3.5 | 2 (13.3) | 2 (13.3) | 4 (13.3) |
| 4–4.5 | 4 (26.7) | 2 (13.3) | 6 (20.0) |
| 5–5.5 | 2 (13.3) | 1 (6.7) | 3 (10.0) |
| 6 | 7 (46.7) | 10 (66.7) | 17 (56.7) |
| Falls in past month (median, range) | 2 (0–7) | 2 (0–6) | 2 (0–7) |
| Falls in past year (median, range) | 8 (2–55) | 7 (3–75) | 7 (2–75) |
One subject lost to follow-up after providing baseline data.
3.2. Falls
The fall calendars were completed on 76% of all possible reporting study days and thus 24% of the days were imputed as having no falls. Adherence to calendar completion was similar between the active and the control group. Sensitivity analyses done on the 76% of days with completed calendars yielded similar results to the analyses with imputation and thus only the analyses with imputation are reported in this paper.
Over the course of this five-month study, 28 of the 29 (96.6%) participants reported falling at least once and 26 (89.7%) fell twice or more. The participant who did not fall and the two who fell only once were both in the active intervention group (p < 0.01). There was a total of 270 falls, for an average of 9.3 falls/participant over the course of the study.
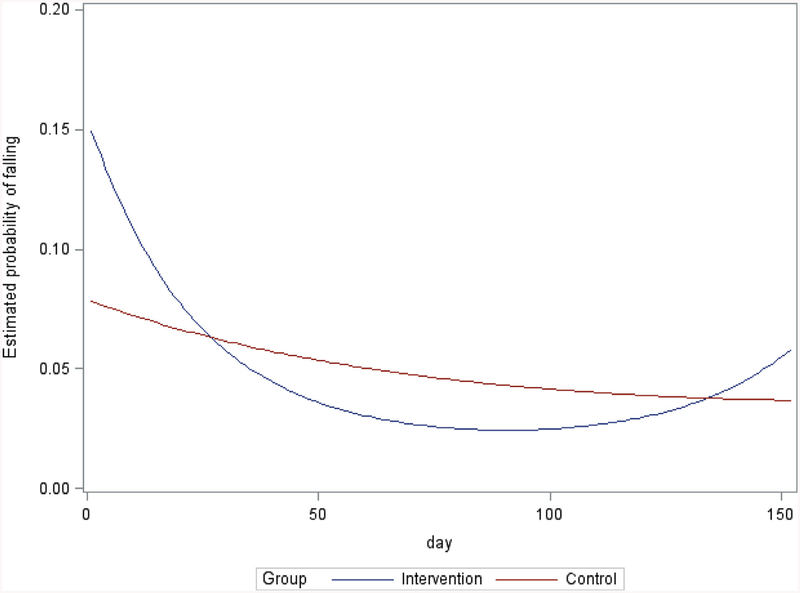
The repeated measures logistic model found that the interaction between group (active or control) and falling over time was not significant (F = 1.32, p = 0.251), although the difference between groups was in the hypothesized direction. The pattern of fall frequency over time also appeared to be slightly different for the two groups on visual inspection, with some delay in impact followed by waning of the effects over time in the active FFFO group (Fig. 2). To assess this visualization, a quadratic term was added to evaluate the relationship between time (days and square of days) and probability of falling. Despite the small sample size, we did demonstrate a statistically significant difference in probability of falling between groups with this post-hoc model (p = 0.0038). This quadratic effect showed a slight decrease in the probability of falling by the intervention group that was most prominent in the first month, less prominent in the last month and not sustained three months following the intervention.
Fig. 2.
Relationship between time in the study and probability of falling for the active FFFO group and the control group, demonstrating that fall rate is stable over time for the control group and slightly decreases in the active group at about four weeks, then stabilizes, and then increases again by the three-month follow-up.
3.3. FFFO program satisfaction
User experience with FFFO was overall positive (Table 2). Based on a response of agree or strongly agree, a majority found the program easy to learn (92%) and easy to use (77%). Regarding the educational component, 85% found the lectures easy to follow and 62% found the material informative. Regarding the exercise component, 85% found the video easy to follow and 77% found it to contribute to the appeal of the material. In addition, 54% found the graphics appealing, 69% found the program easy to navigate and 82% found the organization of the information clear. Overall, 85% of the respondents agreed that the program had all the components they had expected while 69% agreed that the program had all the information regarding fall prevention they needed. 85% would recommend this program to others and 77% would use an online self-management program for other MS symptoms. Many respondents commented that the positive aspects of the program were its comprehensiveness, ease of use and convenience. Many were also pleased that this program provides readily accessible fall prevention information should they have difficulty traveling to participate in physical therapy exercise. The most common suggestions for improvement included increasing the pace and variety of exercises and incorporating more interactive activities and animated narration in the educational sessions to accommodate higher functioning individuals.
3.4. Safety
No adverse events, other than falls, which were expected, were reported in either group during the course of this study. None of the falls resulted in any reported hospitalization.
4. Discussion
The need for evidence-based fall prevention interventions for people with MS is well-recognized. Participation in-person programs is often limited by transportation or program availability. To our knowledge, this is the first study to evaluate a comprehensive web-based fall prevention program, FFFO, in people with MS. This pilot study suggests that the FFFO program is highly acceptable to the target audience and that participation in FFFO may reduce falls.
Participation in FFFO was not associated with a lower probability of falling compared to the control group. However, when a post-hoc analysis was performed summarizing the pattern of response over time, we detected an association between participation in FFFO and lower probability of falling early in the observation period. However, this impact was small and was not sustained three months after the end of the program. None the less, this effect may be clinically important and should be evaluated further with a larger population of high-risk participants. A larger study with greater power might be able to detect effects of this intervention. Also, the pattern of waning over time suggests that various changes to the program, such as including regular supervision, feedback or input by health professionals, may be needed to enhance its impact and thus produce a more clear and sustained benefit. In addition, increasing the pace and variety of the exercises and providing more interactive activities would address the major shortcomings in FFFO noted by study participants and may also increase the size and duration of effect. Repeated or longer participation, alone or in combination with the live FFF program, could also improve, reinforce and maintain efficacy, particularly as web-based delivery allows FFFO to be viewed as often and for as long as desired, supporting self-management among patients with a chronic progressive condition such as MS.
Fall prevention is complex and challenging, particularly in a patient population with limitations in mobility and in accessing effective, evidence-based strategies. Overall, the findings of this pilot study support the feasibility and acceptability of the FFFO program and provide a signal of efficacy of this web-based fall prevention program for PwMS. FFFO is now available free of charge online at the National MS Society website, https://www.nationalmssociety.org/Resources-Support/Library-Education-Programs/Free-From-Falls. FFFO use may also be adapted by and for the individual. It could be used in concert with the in-person FFF program to preview and review program materials before and/or after in-person sessions. This could be particularly useful for people with MS, a disorder associated with fatigue and cognitive dysfunction (Chiaravalloti and DeLuca, 2008). In addition, since it can be difficult to attend in-person group sessions at a given fixed scheduled time, FFFO could be used to cover materials independently in the event of a missed class. However, compared to an in-person group program, FFFO does not have the guidance of the leader or the benefits of peer interaction, and compared to one-on-one interventions, the FFFO program is not personalized based on individual professional assessment and guidance.
This study had a number of strengths. Full enrollment was reached in just over six months, and only one subject was lost to follow-up after enrollment; this ease of recruitment and low attrition suggest high interest in web-based delivery of fall prevention programs and support the feasibility of a future larger, fully powered randomized controlled study. Participants, including older adults, rated the FFFO program as highly usable and were highly satisfied with the content, supporting the feasibility and acceptability of using FFFO as a tool to minimize the risk of falls among both younger and older adults with MS. The falls data were collected on a daily basis using a prompt from a central system, avoiding completion at the end of a month, and thus recall bias, that can occur when paper diaries are collected monthly.
This study also had a number of limitations. The small sample size only allowed limited interpretation and insight into study results. However, the total number of falls and number of falls/participant during the study was high, increasing the probability of finding a difference between groups. The overall high fall rate in this study compared to other studies likely reflects our successful recruitment of people at high fall risk (Gianni et al., 2014; Gunn et al., 2013). Subjects in this trial were also largely older and more well-educated and disabled than an average group of people with MS. Although these demographic features were similar in both groups, maintaining the internal validity of our findings, this may limit the generalizability of the findings. There may also have been selection bias since PwMS who volunteer to participate in a study of patient education programs may be more motivated than most to participate in health promoting behaviors. A further limitation to this study was the lack of analytics to monitor program use and adherence, limiting assessment of utilization of the program or its specific components and evaluation of any dose-response relationship between program or component use and outcomes (O’Connor et al., 2016).
Overall, this study supports the viability of online delivery of self-management strategies, including fall prevention strategies, in PwMS, and will help inform the design of future web-based self-management programs and clinical trials investigating their efficacy in PwMS. Further research is needed to verify the findings of this pilot study of FFFO in PwMS. These findings provide the preliminary data needed for designing a fully powered randomized controlled trial to definitively evaluate the impact of FFFO on falls and other outcomes. If found to be effective, FFFO could easily be used throughout the world to prevent falls and potentially reduce fall related injuries, improve confidence and independence, reduce health care costs, and improve quality of life for PwMS. Beyond its impact in MS, FFFO could also be adapted for other populations at increased risk for falls, including people with spinal cord injury, diabetes, Parkinson’s disease and traumatic brain injury, thereby improving the lives and prolonging the independence of many.
Acknowledgments
This work was supported by the REACT Center Pilot Studies Program (Grant #1P2CHD086851). Study data were collected and managed using REDCap electronic data capture tools hosted at OHSU. REDCap (Research Electronic Data Capture), a secure, web-based application designed to support data capture for research studies, is supported at OHSU by (1 UL RR024140 01). Free From Falls program materials and website hosting of the online program were provided by the National MS Society.
Abbreviations:
- EDSS
Expanded Disability Severity Scale
- FFF
Free From Falls
- FFFO
Free From Falls Online
- MS
multiple sclerosis
- OHSU
Oregon Health & Science University
- PwMS
people with MS
Footnotes
Conflict of interest
All authors report no conflicts of interest relevant to this research study.
References
- Altreja A, Mehta N, Miller D, et al. , 2005. One size does not fit all: using qualitative methods to inform the development of an internet portal for multiple sclerosis patients. AMIA Annu. Symp. Proc 16–20. [PMC free article] [PubMed] [Google Scholar]
- Carling A, Forsberg A, Gunnarsson M, Nilsagard Y, 2017. CoDuSe group exercise programme improves balance and reduces falls in people with multiple sclerosis: a multi-centre, randomized, controlled pilot study. Mult Scler. 23 (10), 1394–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiaravalloti ND, DeLuca J, 2008. Cognitive impairment in multiple sclerosis. LancetNeurol. 7 (12), 1139–1151. [DOI] [PubMed] [Google Scholar]
- Finlayson M, Peterson EW, Cho C, 2009. Pilot study of a fall risk management program for middle aged and older adults with MS. NeuroRehabilitation. 25 (2), 107–115. [DOI] [PubMed] [Google Scholar]
- Friemel TN, 2016. The digital divide has grown old: determinants of a digital divide among seniors. New Media Soc. 18 (2), 313–331. [Google Scholar]
- Gianni C, Prosperini L, Jonsdottir J, Cattaneo D, 2014. A systematic review of factors associated with accidental falls in people with multiple sclerosis: a meta-analytic approach. Clin. Rehabil 28 (7), 704–716. [DOI] [PubMed] [Google Scholar]
- Gunn H, Creanor S, Haas B, Marsden J, Freeman J, 2014. Frequency, characteristics, and consequences of falls in multiple sclerosis: findings from a cohort study. Arch. Phys. Med. Rehabil 95 (3), 538–545. [DOI] [PubMed] [Google Scholar]
- Gunn H, Markevics S, Haas B, Marsden J, Freeman J, 2015. Systematic review: the effectiveness of interventions to reduce falls and improve balance in adults with multiple sclerosis. Arch. Phys. Med. Rehabil 96 (10), 1898–1912. [DOI] [PubMed] [Google Scholar]
- Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA, 2013. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys. Ther 93 (4), 504–513. [DOI] [PubMed] [Google Scholar]
- Hugos C, Frankel D, Tompkins SA, Cameron MH, 2016. Community delivery of a comprehensive fall prevention program improves balance and walking in people with MS: a retrospective observational study. Int. J. MS Care 18 (1), 42–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsaker A, Hargittai E, 2018. A review of internet use among older adults. NewMedica Soc. 20 (10), 3937–3954. [Google Scholar]
- Lejbkowicz I, Paperna T, Stein N, Dishon S, Miller A, 2010. Internet usage by patients with multiple sclerosis: implications to participatory medicine and personalized healthcare. Multip. Scler. Int 2010, 640749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrie RA, Salter AR, Tyry T, Fox RJ, Cutter GR, 2013. Preferred sources of health information in persons with multiple sclerosis: degree of trust and information sought. J. Med. Internet Res 15 (4), 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martini DN, Zeeboer E, Hildebrand A, Fling BW, Hugos CL, Cameron MH, 2018. ADSTEP: preliminary investigation of a multicomponent walking aid program in people with multiple sclerosis. Arch. Phys. Med. Rehabil 99 (10), 2050–2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda PN, Shumway-Cook A, Bamer AM, Johnson SL, Amtmann D, Kraft GH,2011. Falls in multiple sclerosis. Pm R. 3 (7), 624–632. [DOI] [PubMed] [Google Scholar]
- Nilsagard Y, Gunn HJ, Freeman J, et al. , 2015. Falls in people with MS – an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Multip. Scler. J 21 (1), 92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsagard Y, Lundholm C, Denison E, Gunnarsson LG, 2009. Predicting accidental falls in people with multiple sclerosis – a longitudinal study. Clin. Rehabil 23 (3), 259–269. [DOI] [PubMed] [Google Scholar]
- O’Connor S, Hanlon P, O’Donnell CA, Garcia S, Glanville J, Mair FS, 2016. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies. BMC Med. Inform. Decis. Mak 16 (1), 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallin MT, Culpepper WJ, Campbell JD, et al. , 2019. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 92(10), e1029–e1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woollacott MH, Shumway-Cook A, 1990. Changes in posture control across the life span–a systems approach. Phys. Ther 70 (12), 799–807. [DOI] [PubMed] [Google Scholar]