Abstract
Background:
While obesity may be a risk factor for complications following total knee arthroplasty, data remain sparse on the impact of the degree of obesity on patient-reported outcomes following this procedure. Our objective was to determine the extent to which obesity level affects the trajectory of recovery as well as patient-reported pain, function, and satisfaction with surgery following total knee arthroplasty.
Methods:
We followed a cohort of patients who underwent total knee arthroplasty at 1 of 4 medical centers. Patients were ≥40 years of age with a primary diagnosis of osteoarthritis. We stratified patients into 5 groups according to the World Health Organization classification of body mass index (BMI). We assessed the association between BMI group and pain and function over the time intervals of 0 to 3, 3 to 6, and 6 to 24 months using a piecewise linear model. We also assessed the association between BMI group and patient-reported outcomes at 24 months. Multivariable models adjusted for age, sex, race, diabetes, musculoskeletal functional limitations index, pain medication use, and study site.
Results:
Of the 633 participants included in our analysis, 19% were normal weight (BMI of <25 kg/m2), 32% were overweight (BMI of 25 to 29.9 kg/m2), 27% were class-I obese (BMI of 30 to 34.9 kg/m2), 12% were class-II obese (BMI of 35 to 39.9 kg/m2), and 9% were class-III obese (BMI of ≥40 kg/m2). Study participants with a higher BMI had worse preoperative WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain and function scores and had greater improvement from baseline to 3 months. The mean change in pain and function from 3 to 6 and from 6 to 24 months was similar across all BMI groups. At 24 months, participants in all BMI groups had similar levels of pain, function, and satisfaction.
Conclusions:
Because of the differential trajectory of recovery in the first 3 months following total knee arthroplasty, the participants in the higher BMI groups were able to attain absolute pain and function scores similar to those in the nonobese and class-I obese groups. These data can help surgeons discuss expectations of pain relief and functional improvement with total knee arthroplasty candidates with higher BMI.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
Knee osteoarthritis is a prevalent, disabling joint disease that affects almost 4% of the global population1,2. Knee osteoarthritis is more prevalent in obese individuals, and increased body mass index (BMI) has been established as a risk factor for the disease3,4. The number of obese patients with advanced knee osteoarthritis is expected to increase in the coming decades as the prevalence of obesity among U.S. adults continues to rise5. Patients who develop advanced knee osteoarthritis are typically offered total knee arthroplasty, a cost-effective procedure for relieving pain and restoring function6,7. More than 660,000 total knee arthroplasty procedures were performed in 2014 in the U.S., totaling over $10 billion in hospital costs8.
Despite the overall success of total knee arthroplasty in improving pain and function, some patients experience complications and/or less improvement than expected; obese individuals may be at higher risk for such outcomes9-16 as well as for early component failure necessitating revision surgery17. Given that the majority of total knee arthroplasties are performed in obese individuals, it is imperative to understand the benefits these patients can expect from the procedure18. The pain and functional benefits of total knee arthroplasty among obese patients remain a topic of debate. Some authors have found that obesity is associated with worse improvement in functional outcomes, such as results of the timed up-and-go test, and patient-reported outcomes, such as pain19-21. Others have reported no association between obesity and these outcome measures22-24. The evidence is similarly mixed regarding the impact of class-III obesity (a BMI of ≥40 kg/m2 according to the World Health Organization [WHO] classification)25 on total knee arthroplasty outcomes13,14,26-29. While previous studies have evaluated the association between obesity and overall improvements following total knee arthroplasty, the patterns of recovery are less clear. These profiles of change, or trajectories, are important to illuminate in order to better understand the point in the recovery process at which outcomes diverge; this point presents a potent target for intervention. There remains a gap in our understanding of the extent to which the trajectory of recovery following total knee arthroplasty is influenced by BMI.
To address this question, we used patient-reported data from the Adding Value in Knee Arthroplasty (AViKA) studies and the Study of Total Knee Arthroplasty Responses (STARs)30-32 to measure patients’ function, pain, and satisfaction after total knee arthroplasty. Our objective was to assess the extent to which BMI category affects the trajectory of recovery over 24 months following total knee arthroplasty as well as the resulting patient-reported outcomes at 24 months.
Materials and Methods
Sample
Participants were enrolled in 1 of 3 studies assessing outcomes of total knee arthroplasty: the AViKA cohort study, the AViKA Care Navigator randomized controlled trial, and STARs30-32. Participants were enrolled at 4 medical centers: a tertiary academic medical center in Boston, Massachusetts; an academic medical center in New York City; and community orthopaedic practices in Baltimore, Maryland, and Fort Collins, Colorado. Included were English-speaking adults who lived in the community, were ≥40 years of age, and were undergoing total knee arthroplasty for a primary diagnosis of osteoarthritis. Exclusion criteria included diagnoses other than osteoarthritis (e.g., inflammatory arthritis), dementia, unicompartmental knee arthroplasty, and bilateral total knee arthroplasty. For our analysis, we included both arms of the Care Navigator randomized controlled trial, as the study did not find a difference in patient-reported outcomes, including pain and function, by treatment arm31.
All participants completed a baseline questionnaire within 6 weeks prior to surgery and were evaluated at 3, 6, and 24 months postoperatively. The AViKA Care Navigator randomized controlled trial and STARs cohorts had an additional follow-up at 12 months. (While the primary end point of the Care Navigator randomized controlled trial was 6 months, patients were also evaluated at 12 and 24 months postoperatively.) Our analytic cohort consisted of participants who provided height and weight information on the baseline questionnaire and who completed ≥1 follow-up questionnaire. We also compared the baseline and clinical characteristics of participants who were included in our analytic cohort with those who were excluded.
All participants provided signed informed consent, and all 3 studies were approved by the Partners Healthcare institutional review board.
Data Elements
Outcomes
We measured pain and functional status with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). The WOMAC uses a 5-point Likert scale to assess pain according to 5 items and function according to 17 items. For ease of interpretation, these scores were converted to a scale of 0 to 100 (with 100 being the worst) by dividing the subscale score by the total possible score and multiplying by 100. We assessed the level of overall satisfaction with the surgery following total knee arthroplasty with the question, “How satisfied are you with the results of your knee replacement surgery?” Overall satisfaction was categorized as “very satisfied” or “not very satisfied” (which included “somewhat satisfied,” “somewhat dissatisfied,” and “very dissatisfied”).
Covariates
Our primary predictor was BMI group. BMI was calculated from height and weight that was self-reported on the preoperative patient questionnaire. We stratified BMI into 5 groups, on the basis of the WHO classification: BMI of <25.0 kg/m2 (normal weight), 25.0 to 29.9 kg/m2 (overweight), 30.0 to 34.9 kg/m2 (class-I obese), 35.0 to 39.9 kg/m2 (class-II obese), and ≥40.0 kg/m2 (class-III obese)25. Because of the small number of participants who were underweight (BMI of <18.5 kg/m2), those patients were included in the “normal weight” category (BMI of <25 kg/m2). We collected data regarding diabetes status, use of medication for knee pain (categorized as no use, occasional use, or almost daily use), and the musculoskeletal functional limitations index33. This index measures the aggregation of musculoskeletal problems in 6 anatomic regions that limit a patient’s ability to perform daily activities; it is scored on a scale of 0 to 12, with 12 being the worst. Demographic data included age, sex, education, race, study site, and surgeon.
Statistical Analysis
To investigate the association between time trend in WOMAC pain and function over 24 months and BMI group, we used a piecewise linear mixed-effects model. Piecewise linear models, also called spline models, work well to describe nonlinear longitudinal trends in which a mean response changes rapidly for some duration and more slowly thereafter (or vice versa)34. These models are thus well suited to describe total knee arthroplasty recovery, in which we expect rapid improvement over the first 3 to 6 months, followed by slower improvement35,36. Points at which the slope changes are referred to as “knots.” For pain and function separately, we evaluated 3 different models—1 knot at 3 months, 1 knot at 6 months, and knots at both 3 and 6 months—and selected the best-fit, most parsimonious model based on r2 and the Bayesian information criterion (BIC)34.
To investigate the association between the final WOMAC score at 24 months and BMI group, we used linear mixed-effects models. We modeled WOMAC pain and function separately. Linear mixed-effects models take into account all available data and thus allow for missing data; therefore, we included all participants in the analysis regardless of month-24 visit completion.
Finally, we used a mixed-effects logistic regression model to examine the effect of BMI group on patient satisfaction at 24 months. As a sensitivity analysis for missing 24-month data, we used a last observation carried forward (LOCF) approach by creating a satisfaction score based on the final satisfaction response recorded (that is, from 24 months if available; otherwise, from 12 months; otherwise, from 6 months; otherwise, satisfaction data missing).
All models were adjusted for age, sex, race, diabetes, musculoskeletal functional limitations index, pain medication use, and study site. We accounted for clustering by surgeon by including a random effect in the mixed model.
Results
Sample Description
Of 691 enrolled participants, 633 (92%) had baseline BMI data and completed ≥1 follow-up questionnaire. Fifty-eight participants were excluded: 16 on the basis of missing BMI data, 39 for missing all follow-up questionnaires, and 3 for missing both BMI data and all follow-up questionnaires. The excluded participants reported, on average, worse preoperative WOMAC scores for pain and function (mean [and standard deviation], 48.3 ± 19.2 and 50.4 ± 18.6, respectively) compared with those in the analytic cohort (40.8 ± 17.9 and 42.5 ± 17.0). The excluded participants were more likely to be using medication almost daily for knee pain (62% compared with 43%). There were also differences between the included and excluded groups with respect to race and study site (see Appendix). However, there did not appear to be an association between BMI group and exclusion due to missing all follow-up questionnaires.
In the analytic cohort, the average age was 65.9 ± 8.5 years. Fifty-nine percent of the participants were female, and 93% were white. The average BMI was 30.8 ± 6.6 kg/m2 (Table I). On the basis of BMI, 120 (19%) of the participants were categorized as normal weight; 203 (32%), overweight; 174 (27%), class-I obese; 79 (12%), class-II obese; and 57 (9%), class-III obese. The normal-weight group included 2 participants with a BMI of <18.5 kg/m2. The mean musculoskeletal functional limitations index was 3.3 ± 2.1. Thirteen percent of the participants had diabetes, and 43% reported taking medication for knee pain almost every day. The overall mean preoperative WOMAC pain and function scores were 40.8 ± 17.9 and 42.5 ± 17.0, respectively.
TABLE I.
Baseline Characteristics*
| Group According to Baseline BMI in kg/m2 |
||||||
| Characteristic | Overall (N = 633) | <25 (N = 120) | 25-29.9 (N = 203) | 30-34.9 (N = 174) | 35-39.9 (N = 79) | ≥40 (N = 57) |
| WOMAC† | ||||||
| Function | 42.5 ± 17.0 | 34.7 ± 16.3 | 39.3 ± 15.8 | 45.8 ± 16.3 | 49.8 ± 16.4 | 50.5 ± 16.6 |
| Pain | 40.8 ± 17.9 | 33.7 ± 15.9 | 37.7 ± 15.6 | 43.2 ± 19.2 | 47.5 ± 18.6 | 49.7 ± 17.3 |
| Musculoskeletal functional limitations index‡ | 3.3 ± 2.1 | 2.9 ± 1.8 | 3.2 ± 2.1 | 3.4 ± 2.1 | 3.9 ± 2.2 | 3.8 ± 2.6 |
| BMI (kg/m2) | 30.8 ± 6.6 | 23.1 ± 1.7 | 27.6 ± 1.5 | 32.2 ± 1.4 | 37.4 ± 1.4 | 45.0 ± 5.6 |
| Age at surgery (yr) | 65.9 ± 8.5 | 68.0 ± 9.2 | 66.1 ± 8.6 | 66.5 ± 8.3 | 63.6 ± 8.0 | 62.6 ± 6.8 |
| Age group | ||||||
| <65 yr | 275 (43.4%) | 45 (37.5%) | 87 (42.9%) | 70 (40.2%) | 36 (45.6%) | 37 (64.9%) |
| ≥65 yr | 358 (56.6%) | 75 (62.5%) | 116 (57.1%) | 104 (59.8%) | 43 (54.4%) | 20 (35.1%) |
| Sex | ||||||
| Male | 258 (40.8%) | 37 (30.8%) | 107 (52.7%) | 78 (44.8%) | 20 (25.3%) | 16 (28.1%) |
| Female | 375 (59.2%) | 83 (69.2%) | 96 (47.3%) | 96 (55.2%) | 59 (74.7%) | 41 (71.9%) |
| Race | ||||||
| Non-white | 43 (7.0%) | 4 (3.3%) | 9 (4.6%) | 14 (8.2%) | 7 (9.5%) | 9 (16.1%) |
| White | 573 (93.0%) | 116 (96.7%) | 187 (95.4%) | 156 (91.8%) | 67 (90.5%) | 47 (83.9%) |
| Diabetes | ||||||
| No | 536 (87.4%) | 110 (94.8%) | 183 (92.9%) | 133 (80.6%) | 68 (86.1%) | 42 (75.0%) |
| Yes | 77 (12.6%) | 6 (5.2%) | 14 (7.1%) | 32 (19.4%) | 11 (13.9%) | 14 (25.0%) |
| Study center | ||||||
| MD | 88 (13.9%) | 24 (20.0%) | 28 (13.8%) | 22 (12.6%) | 8 (10.1%) | 6 (10.5%) |
| CO | 103 (16.3%) | 20 (16.7%) | 34 (16.7%) | 26 (14.9%) | 12 (15.2%) | 11 (19.3%) |
| NY | 54 (8.5%) | 9 (7.5%) | 17 (8.4%) | 13 (7.5%) | 8 (10.1%) | 7 (12.3%) |
| MA | 388 (61.3%) | 67 (55.8%) | 124 (61.1%) | 113 (64.9%) | 51 (64.6%) | 33 (57.9%) |
| Pain medication use for knee | ||||||
| No | 141 (22.4%) | 29 (24.2%) | 52 (25.7%) | 39 (22.5%) | 11 (14.1%) | 10 (17.9%) |
| Yes, occasionally | 215 (34.2%) | 46 (38.3%) | 65 (32.2%) | 62 (35.8%) | 26 (33.3%) | 16 (28.6%) |
| Yes, almost every day | 273 (43.4%) | 45 (37.5%) | 85 (42.1%) | 72 (41.6%) | 41 (52.6%) | 30 (53.6%) |
Continuous variables are presented as the mean and the standard deviation. Categorical variables are presented as the number, with the percentage in parentheses.
Scale of 0 to 100, with 100 being the worst.
Scale of 0 to 12, with 12 being the worst.
BMI Groups and Preoperative Characteristics
The BMI groups differed with respect to baseline characteristics. Heavier participants tended to be younger; the mean age at surgery ranged from 68.0 years in the normal-weight group to 62.6 years in the class-III obese group (Table I). Heavier participants were more likely to be female, to be non-white, and to have diabetes, and had, on average, greater musculoskeletal functional limitations.
The heavier BMI groups had, on average, worse preoperative WOMAC pain and function scores; the mean preoperative pain score ranged from 33.7 ± 15.9 in the normal-weight group to 49.7 ± 17.3 in the class-III obese group, and the mean preoperative function score ranged from 34.7 ± 16.3 in the normal-weight group to 50.5 ± 16.6 in the class-III obese group.
BMI Groups and Outcomes
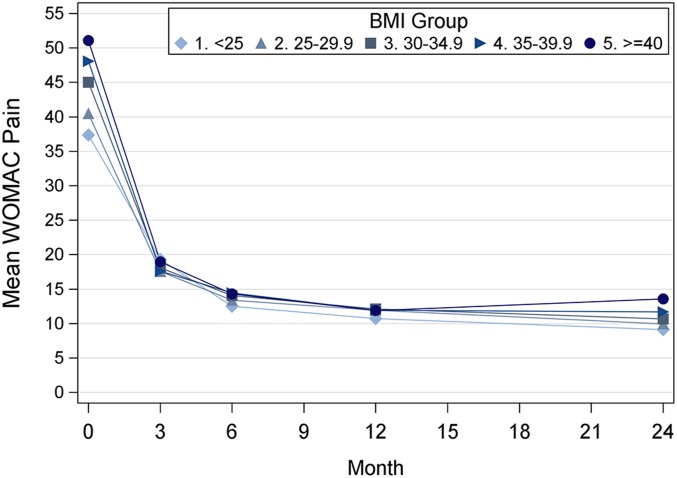
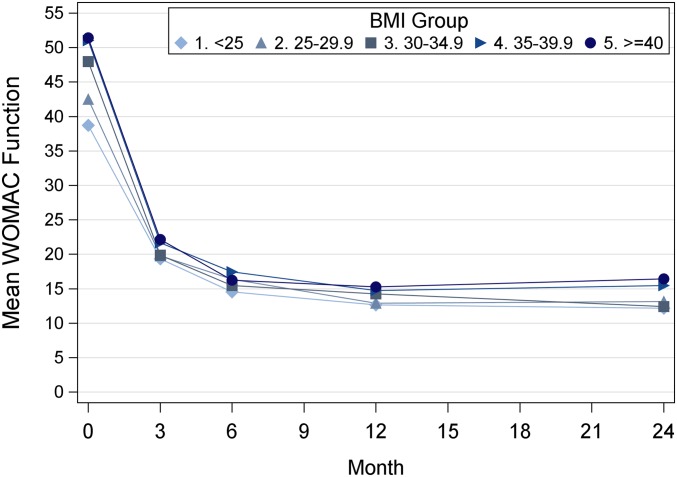
All BMI groups showed improvement in both pain (Fig. 1) and function (Fig. 2). The mean adjusted WOMAC pain and function scores at 24 months were 11.0 (standard error of the mean [SE], 1.3) and 13.9 (SE, 1.5), respectively.
Fig. 1.
Adjusted mean WOMAC pain scores by BMI group and time (baseline [preoperative] and 3, 6, 12, and 24 months). Each line represents a BMI group, from lighter to darker: normal weight (BMI of <25 kg/m2), overweight (BMI of 25 to 29.9 kg/m2), class-I obese (BMI of 30 to 34.9 kg/m2), class-II obese (BMI of 35 to 39.9 kg/m2), and class-III obese (BMI of ≥40 kg/m2). Adjusted means were computed from a linear mixed-effects model adjusting for age, sex, race, diabetes, musculoskeletal functional limitations index, pain medication use, and study site.
Fig. 2.
Adjusted mean WOMAC function scores by BMI group and time (baseline [preoperative] and 3, 6, 12, and 24 months). Each line represents a BMI group, from lighter to darker: normal weight (BMI of <25 kg/m2), overweight (BMI of 25 to 29.9 kg/m2), class-I obese (BMI of 30 to 34.9 kg/m2), class-II obese (BMI of 35 to 39.9 kg/m2), and class-III obese (BMI of ≥40 kg/m2). Adjusted means were computed from a linear mixed-effects model adjusting for age, sex, race, diabetes, musculoskeletal functional limitations index, pain medication use, and study site.
The piecewise linear model identified 3 distinct pain-improvement periods: from baseline to 3 months (postoperative days 0 to 90), 3 to 6 months (days 90 to 183), and 6 to 24 months (days 183 to 730). For WOMAC pain, in the unadjusted model, patients improved, on average, by 25.0 points in the interval of baseline to 3 months (days 0 to 90), 4.9 points in the interval of 3 to 6 months (days 90 to 183), and 2.9 points in the interval of 6 to 24 months (days 183 to 730), which translates to 0.48 points per 3-month interval over months 6 to 24. On average, patients in the higher BMI groups experienced greater pain improvement during the interval of 0 to 3 months than did patients in the lower BMI groups (adjusted p < 0.0001). The mean adjusted change in pain for the interval of baseline to 3 months ranged from 18.1 points in the lowest BMI group (BMI of <25 kg/m2) to 32.2 points in the highest BMI group (BMI of ≥40 kg/m2) (Table II). During the intervals of 3 to 6 months and 6 to 24 months, all BMI groups experienced similar improvement in pain. We observed similar results for WOMAC function; the higher BMI groups experienced greater improvement in function from baseline to 3 months (adjusted p < 0.0001), while functional improvements did not differ by BMI group during the intervals of 3 to 6 months or 6 to 24 months.
TABLE II.
Trend Over Time by BMI Group: Results from Piecewise Linear Models
| Pain |
Function |
||||||
| Time Period | BMI (kg/m2) | Mean Change per 3-Mo. Interval | 95% CI | P Value | Mean Change per 3-Mo. Interval | 95% CI | P Value |
| Baseline to 3 mo. | <0.0001 | <0.0001 | |||||
| <25 | −18.1 | −21.7 to −14.5 | −19.5 | −22.7 to −16.3 | |||
| 25-29.9 | −23.0 | −25.8 to −20.1 | −23.0 | −25.5 to −20.5 | |||
| 30-34.9 | −26.9 | −30.0 to −23.9 | −28.2 | −30.9 to −25.5 | |||
| 35-39.9 | −30.6 | −35.0 to −26.2 | −29.6 | −33.5 to −25.7 | |||
| ≥40 | −32.2 | −37.5 to −27.0 | −29.4 | −34.1 to −24.7 | |||
| 3-6 mo. | 0.3096 | 0.7284 | |||||
| <25 | −6.9 | −9.3 to −4.6 | −5.0 | −7.0 to −3.1 | |||
| 25-29.9 | −4.2 | −6.0 to −2.4 | −4.0 | −5.5 to −2.4 | |||
| 30-34.9 | −4.2 | −6.2 to −2.2 | −4.4 | −6.1 to −2.8 | |||
| 35-39.9 | −3.5 | −6.2 to −0.7 | −4.7 | −7.0 to −2.4 | |||
| ≥40 | −5.0 | −8.3 to −1.7 | −6.1 | −8.9 to −3.3 | |||
| 6-24 mo. | 0.5936 | 0.5525 | |||||
| <25 | −0.5 | −0.9 to −0.2 | −0.3 | −0.7 to 0.1 | |||
| 25-29.9 | −0.6 | −0.9 to −0.3 | −0.4 | −0.7 to −0.1 | |||
| 30-34.9 | −0.5 | −0.9 to −0.2 | −0.5 | −0.9 to −0.2 | |||
| 35-39.9 | −0.4 | −0.9 to 0.1 | −0.2 | −0.7 to 0.3 | |||
| ≥40 | 0.0 | −0.6 to 0.5 | 0.1 | −0.5 to 0.7 | |||
At 24 months, the adjusted mean WOMAC pain score ranged from 9.1 (95% confidence interval [CI], 5.8 to 12.5) in the normal-weight group to 13.6 (95% CI, 9.4 to 17.7) in the class-III obese group (adjusted p = 0.2996). The mean adjusted WOMAC function score ranged from 12.2 (95% CI, 8.4 to 15.9) in the normal-weight group to 16.5 (95% CI, 11.9 to 21.0) in the class-III obese group (adjusted p = 0.2153). Eighty-one percent of the participants reported that they were “very satisfied” with the surgery: 80% in the normal-weight group, 80% in the overweight group, 82% in the class-I obese group, 80% in the class-II obese group, and 83% in the class-III obese group reported high satisfaction (adjusted p = 0.8246). Results were similar after using the LOCF approach for the 97 patients (15%) who were missing a satisfaction response at 24 months.
Discussion
From a cohort of >600 total knee arthroplasty patients, we assessed whether BMI group was associated with patient-reported outcomes, including the time trend of recovery. Our results showed that, while a higher BMI was associated with worse preoperative pain and function, by 24 months postoperatively, there were no significant differences in pain or function across the BMI groups. The piecewise linear model demonstrated that the higher BMI groups experienced greater improvement in the first 3 months postoperatively compared with the lower BMI groups, and afterward, the trend over time was similar across all BMI groups. Patients reported a similar level of high satisfaction across all BMI groups.
The findings of previous studies of obesity and recovery following total knee arthroplasty have been mixed, with some studies suggesting that obesity is associated with worse pain and function and lower satisfaction following total knee arthroplasty, and others finding no association, or even that obese patients are more likely to be satisfied with their surgery19-24,26,37,38. This variability may be due to differences in the health status of the cohorts or differences in the cutoffs used to define categories of obesity. Baker and colleagues found that a higher BMI (assessed in groups of BMI of <25, 25 to 39.9, and ≥40 kg/m2) was associated with worse baseline values for the Oxford Knee Score and EuroQol-5 Dimensions (EQ-5D) but that the average change from baseline to 6 months following total knee arthroplasty was similar across the BMI distribution39. Jiang et al. found that patients with a BMI of >35 kg/m2 started with worse Oxford Knee Score values compared with normal-weight patients and that differences between BMI groups persisted at 1, 5, and 10 years after total knee arthroplasty40. We also found that patients in the higher BMI groups had worse pain and function preoperatively, and we found that patients in the higher BMI groups had more change. The studies of both Baker et al. and Jiang et al. involved patients in the U.K., and the average baseline scores were substantially worse than in our study. It is possible that differences between the U.S. and U.K. health-care systems result in different indications for total knee arthroplasty; a recent review found that, in 2011, the U.S. had an incidence rate of 235 total knee arthroplasties per 100,000 population compared with 140 per 100,000 in the U.K41. We examined both short-term and long-term (up to 24-month) changes in pain and function, and our findings offer insight into the association between obesity and total knee arthroplasty recovery in a U.S. population with moderate pain and functional limitations prior to the procedure. It is also possible that, by using the 5-level WHO classification for BMI, we were better able to elucidate distinct patterns within each group.
A major strength of our study was the ability to evaluate different recovery periods following total knee arthroplasty. The recovery trend over time for total knee arthroplasty is nonlinear36, and our piecewise linear model uncovered 3 distinct recovery periods: baseline to 3 months (postoperative days 0 to 90), 3 to 6 months (days 90 to 183), and 6 to 24 months (days 183 to 730). This allowed us to assess the effect of the BMI group separately in early recovery and in later recovery. Participants in the higher BMI groups experienced greater improvement during the first 3 months postoperatively. In fact, the average change in pain among class-II and class-III obese participants over the first 3 postoperative months (30.6 and 32.2 points, respectively) was more than 40% greater than that for normal-weight participants (18.1 points). Improvements did not differ statistically by BMI group in the interval of 3 to 6 months or 6 to 24 months. All BMI groups experienced improvement in pain and function by 24 months. In particular, we noted that mean 24-month WOMAC scores differed at most by 4 to 5 points across the BMI groups, a difference that was neither significant nor regarded as clinically meaningful42,43.
Our analysis had several limitations. Eight percent of the participants were excluded from the analytic cohort, the majority because of missing follow-up questionnaires. Linear mixed-effects models take into account all available data and thus allow for missing data, and therefore, we included all patients who had at least 1 follow-up visit. While the excluded participants had worse preoperative pain and function (see Appendix), there did not appear to be an association between BMI group and exclusion due to missing follow-up questionnaires. The inclusion and exclusion criteria were not based on BMI value; however, BMI data were only available for those patients who completed a baseline questionnaire, and thus we cannot determine if study participation was associated with BMI. Bilateral and unicompartmental surgeries were excluded, limiting the generalizability of the results to unilateral total knee arthroplasty. Comorbidities were not assessed in a uniform manner across studies and thus could not be adjusted for, the exception being diabetes, which was similarly assessed across studies and, therefore, was included in our analysis. It is possible that differences in baseline comorbidities could explain some of the differences in baseline pain and function among the BMI groups. Finally, BMI calculations were based on self-reported height and weight, and BMI was missing for 3% of the cohort, who were excluded.
Overall, we found that participants across all BMI groups achieved similar outcomes with respect to self-reported pain, function, and satisfaction at 24 months following total knee arthroplasty. Because of the differential trajectory of recovery in the first 3 months postoperatively, participants in the class-II and class-III groups were able to reach absolute pain and function scores similar to those in the nonobese and class-I obese groups. We believe that our research contributes important data regarding the trajectory of patient-reported pain and functional recovery for obese patients after total knee arthroplasty; such research can provide critical insight as surgeons discuss the expectations of surgery with the growing numbers of total knee arthroplasty candidates with higher BMI.
Appendix
A table comparing the characteristics of participants included in, and excluded from, the analytic cohort is available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/E343).
Footnotes
Investigation performed at Brigham and Women’s Hospital, Boston, Massachusetts
A commentary by Craig J. Della Valle, MD, is linked to the online version of this article at jbjs.org.
Disclosure: This study was supported by funding from the National Institutes of Health (K24AR057827, P60AR047782). The funding source did not play a role in this investigation. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work and “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJS/E338).
References
- 1.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 Study. Ann Rheum Dis. 2014. July;73(7):1323-30. Epub 2014 Feb 19. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2009. May 1;58(16):421-6. [PubMed] [Google Scholar]
- 3.Lee R, Kean WF. Obesity and knee osteoarthritis. Inflammopharmacology. 2012. April;20(2):53-8. Epub 2012 Jan 12. [DOI] [PubMed] [Google Scholar]
- 4.Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010. January;18(1):24-33. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Fryar CD, Flegal KM, Centers for Disease Control and Prevention. Prevalence of obesity among adults and youth: United States, 2011-2014. 2015. https://www.cdc.gov/nchs/products/databriefs/db219.htm. Accessed 2017 May 12.
- 6.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009. June 22;169(12):1113-21, discussion :1121-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones CA, Beaupre LA, Johnston DW, Suarez-Almazor ME. Total joint arthroplasties: current concepts of patient outcomes after surgery. Rheum Dis Clin North Am. 2007. February;33(1):71-86. [DOI] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. 2014. http://hcupnet.ahrq.gov/. Accessed 2016 December 20. [DOI] [PubMed]
- 9.Abdel MP, Ast MP, Lee YY, Lyman S, González Della Valle A. All-cause in-hospital complications and urinary tract infections increased in obese patients undergoing total knee arthroplasty. J Arthroplasty. 2014. July;29(7):1430-4. Epub 2014 Feb 12. [DOI] [PubMed] [Google Scholar]
- 10.Abdel MP, Bonadurer GF, 3rd, Jennings MT, Hanssen AD. Increased aseptic tibial failures in patients with a BMI ≥35 and well-aligned total knee arthroplasties. J Arthroplasty. 2015. December;30(12):2181-4. Epub 2015 Jul 2. [DOI] [PubMed] [Google Scholar]
- 11.Alvi HM, Mednick RE, Krishnan V, Kwasny MJ, Beal MD, Manning DW. The effect of BMI on 30 day outcomes following total joint arthroplasty. J Arthroplasty. 2015. July;30(7):1113-7. Epub 2015 Feb 7. [DOI] [PubMed] [Google Scholar]
- 12.Friedman RJ, Hess S, Berkowitz SD, Homering M. Complication rates after hip or knee arthroplasty in morbidly obese patients. Clin Orthop Relat Res. 2013. October;471(10):3358-66. Epub 2013 May 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Samson AJ, Mercer GE, Campbell DG. Total knee replacement in the morbidly obese: a literature review. ANZ J Surg. 2010. September;80(9):595-9. Epub 2010 Aug 19. [DOI] [PubMed] [Google Scholar]
- 14.McElroy MJ, Pivec R, Issa K, Harwin SF, Mont MA. The effects of obesity and morbid obesity on outcomes in TKA. J Knee Surg. 2013. April;26(2):83-8. Epub 2013 Mar 11. [DOI] [PubMed] [Google Scholar]
- 15.Ward DT, Metz LN, Horst PK, Kim HT, Kuo AC. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplasty. 2015. September;30(9)(Suppl):42-6. Epub 2015 Jun 3. [DOI] [PubMed] [Google Scholar]
- 16.Adhikary SD, Liu WM, Memtsoudis SG, Davis CM, 3rd, Liu J. Body mass index more than 45 kg/m(2) as a cutoff point is associated with dramatically increased postoperative complications in total knee arthroplasty and total hip arthroplasty. J Arthroplast. 2016. April;31(4):749-53. Epub 2015 Nov 10. [DOI] [PubMed] [Google Scholar]
- 17.Kerkhoffs GM, Servien E, Dunn W, Dahm D, Bramer JA, Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am. 2012. October 17;94(20):1839-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fehring TK, Odum SM, Griffin WL, Mason JB, McCoy TH. The obesity epidemic: its effect on total joint arthroplasty. J Arthroplasty. 2007. September;22(6)(Suppl 2):71-6. Epub 2007 Jul 26. [DOI] [PubMed] [Google Scholar]
- 19.Naylor JM, Harmer AR, Heard RC. Severe other joint disease and obesity independently influence recovery after joint replacement surgery: an observational study. Aust J Physiother. 2008;54(1):57-64. [DOI] [PubMed] [Google Scholar]
- 20.Jones CA, Cox V, Jhangri GS, Suarez-Almazor ME. Delineating the impact of obesity and its relationship on recovery after total joint arthroplasties. Osteoarthritis Cartilage. 2012. June;20(6):511-8. Epub 2012 Mar 3. [DOI] [PubMed] [Google Scholar]
- 21.Vincent HK, Vincent KR. Obesity and inpatient rehabilitation outcomes following knee arthroplasty: a multicenter study. Obesity (Silver Spring). 2008. January;16(1):130-6. [DOI] [PubMed] [Google Scholar]
- 22.Papakostidou I, Dailiana ZH, Papapolychroniou T, Liaropoulos L, Zintzaras E, Karachalios TS, Malizos KN. Factors affecting the quality of life after total knee arthroplasties: a prospective study. BMC Musculoskelet Disord. 2012. June 29;13(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stevens-Lapsley JE, Petterson SC, Mizner RL, Snyder-Mackler L. Impact of body mass index on functional performance after total knee arthroplasty. J Arthroplasty. 2010. October;25(7):1104-9. Epub 2009 Oct 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deshmukh RG, Hayes JH, Pinder IM. Does body weight influence outcome after total knee arthroplasty? A 1-year analysis. J Arthroplasty. 2002. April;17(3):315-9. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed 2016 November 11.
- 26.Dewan A, Bertolusso R, Karastinos A, Conditt M, Noble PC, Parsley BS. Implant durability and knee function after total knee arthroplasty in the morbidly obese patient. J Arthroplasty. 2009. September;24(6)(Suppl):89-94: 94.e1-3. Epub 2009 Jul 2. [DOI] [PubMed] [Google Scholar]
- 27.Franklin PD, Rosal MC. Can knee arthroplasty play a role in weight management in knee osteoarthritis? Arthritis Care Res (Hoboken). 2013. May;65(5):667-8. [DOI] [PubMed] [Google Scholar]
- 28.Rajgopal V, Bourne RB, Chesworth BM, MacDonald SJ, McCalden RW, Rorabeck CH. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008. September;23(6):795-800. Epub 2008 Mar 4. [DOI] [PubMed] [Google Scholar]
- 29.Dowsey MM, Liew D, Stoney JD, Choong PF. The impact of pre-operative obesity on weight change and outcome in total knee replacement: a prospective study of 529 consecutive patients. J Bone Joint Surg Br. 2010. April;92(4):513-20. [DOI] [PubMed] [Google Scholar]
- 30.Losina E, Collins JE, Daigle ME, Donnell-Fink LA, Prokopetz JJ, Strnad D, Lerner V, Rome BN, Ghazinouri R, Skoniecki DJ, Katz JN, Wright J. The AViKA (Adding Value in Knee Arthroplasty) postoperative care navigation trial: rationale and design features. BMC Musculoskelet Disord. 2013. October 12;14:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Losina E, Collins JE, Wright J, Daigle ME, Donnell-Fink LA, Strnad D, Usiskin IM, Yang HY, Lerner V, Katz JN. Postoperative care navigation for total knee arthroplasty patients: a randomized controlled trial. Arthritis Care Res (Hoboken). 2016. September;68(9):1252-9. Epub 2016 Jul 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dave AJ, Selzer F, Losina E, Klara KM, Collins JE, Usiskin I, Band P, Dalury DF, Iorio R, Kindsfater K, Katz JN. Is there an association between whole-body pain with osteoarthritis-related knee pain, pain catastrophizing, and mental health? Clin Orthop Relat Res. 2015. December;473(12):3894-902. Epub 2015 Oct 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Katz JN, Wright EA, Baron JA, Losina E. Development and validation of an index of musculoskeletal functional limitations. BMC Musculoskelet Disord. 2009. June 6;10:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. 2nd ed. Hoboken: Wiley; 2011.
- 35.Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD. Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplasty. 2006. June;21(4):559-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kennedy DM, Stratford PW, Riddle DL, Hanna SE, Gollish JD. Assessing recovery and establishing prognosis following total knee arthroplasty. Phys Ther. 2008. January;88(1):22-32. Epub 2007 Nov 6. [DOI] [PubMed] [Google Scholar]
- 37.Rodriguez-Merchan EC. Review article: Outcome of total knee arthroplasty in obese patients. J Orthop Surg (Hong Kong). 2015. April;23(1):107-10. [DOI] [PubMed] [Google Scholar]
- 38.Núñez M, Lozano L, Núñez E, Segur JM, Sastre S, Maculé F, Ortega R, Suso S. Total knee replacement and health-related quality of life: factors influencing long-term outcomes. Arthritis Rheum. 2009. August 15;61(8):1062-9. [DOI] [PubMed] [Google Scholar]
- 39.Baker P, Muthumayandi K, Gerrand C, Kleim B, Bettinson K, Deehan D. Influence of body mass index (BMI) on functional improvements at 3 years following total knee replacement: a retrospective cohort study. PLoS One. 2013;8(3):e59079 Epub 2013 Mar 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiang Y, Sanchez-Santos MT, Judge AD, Murray DW, Arden NK. Predictors of patient-reported pain and functional outcomes over 10 years after primary total knee arthroplasty: a prospective cohort study. J Arthroplasty. 2017. January;32(1):92-100.e2. Epub 2016 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pabinger C, Lothaller H, Geissler A. Utilization rates of knee-arthroplasty in OECD countries. Osteoarthritis Cartilage. 2015. October;23(10):1664-73. [DOI] [PubMed] [Google Scholar]
- 42.Ehrich EW, Davies GM, Watson DJ, Bolognese JA, Seidenberg BC, Bellamy N. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities Osteoarthritis Index questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000. November;27(11):2635-41. [PubMed] [Google Scholar]
- 43.Lingard EA, Katz JN, Wright EA, Sledge CB; Kinemax Outcomes Group. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004. October;86(10):2179-86. [DOI] [PubMed] [Google Scholar]