Abstract
Background:
The prevalence of obesity in the United States has increased in recent decades. The aim of this study was to evaluate the influence of obesity in patients undergoing primary total elbow arthroplasty.
Methods:
From 1987 to 2006, 723 primary semiconstrained, linked total elbow arthroplasties were performed in 654 patients. The average patient age (and standard deviation) at the time of surgery was 62.3 ± 13.7 years, with 550 total elbow arthroplasties (76%) performed in women. Total elbow arthroplasties were used to treat inflammatory conditions in patients undergoing 378 total elbow arthroplasties (52%) and to treat acute traumatic or posttraumatic conditions in patients undergoing 310 total elbow arthroplasties (43%). Patients were classified as non-obese (having a body mass index of <30 kg/m2) in 564 total elbow arthroplasties (78%) and as obese (having a body mass index of ≥30 kg/m2) in 159 total elbow arthroplasties (22%). The median duration of follow-up was 5.8 years (range, zero to twenty-five years). Survivorship of total elbow arthroplasty was estimated with use of the Kaplan-Meier method. The effect of obesity on risk of total elbow arthroplasty revision was estimated with use of Cox regression models, adjusting for age, sex, body mass index, and indication.
Results:
A total of 118 revisions (16%) were performed. The ten-year survival rate for total elbow arthroplasty revision for any reason was 86% (95% confidence interval, 82% to 89%) in non-obese patients compared with 70% (95% confidence interval, 60% to 79%) in obese patients (p < 0.05). The ten-year survival rate for total elbow arthroplasty revision for mechanical failure was 88% (95% confidence interval, 84% to 91%) in non-obese patients compared with 72% (95% confidence interval, 61% to 81%) in obese patients (p < 0.05). Severely obese patients (those with a body mass index of 35 to <40 kg/m2) had a significantly higher risk of total elbow arthroplasty revision for any reason (hazard ratio, 3.08 [95% confidence interval, 1.61 to 5.45]; p < 0.05) and mechanical failure (hazard ratio, 3.10 [95% confidence interval, 1.47 to 5.89]; p < 0.05) compared with non-obese patients.
Conclusions:
Obesity adversely influences the performance of elbow replacement after primary total elbow arthroplasty. Obese patients being considered for elbow replacement surgery should be counseled accordingly.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
Obesity has become epidemic, with more than 502 million people classified as obese in the world1. In the United States, from 1976 to 2004, obesity increased from 15.1% to 32.2% among adults twenty years of age and older2,3. The development of osteoarthritis in obese individuals includes both biomechanical and physiological mechanisms4,5. Although obesity is associated with the pathogenesis of osteoarthritis in the knee, its role remains less clear in the hip5.
The impact of obesity on the outcome of joint arthroplasty of the hip5-12, knee5,11-23, ankle24, and shoulder25-27 has been evaluated. Some public health systems recommend limiting arthroplasty services on the basis of body mass index (BMI)28. Current literature shows some uncertainty about the influence of obesity on outcome for total hip arthroplasty or total knee arthroplasty. Several authors have reported similar results for obese and non-obese patients6,10,18-21,23, whereas other authors have described obesity as having a negative influence on the outcome8,13-16,22. However, the effect of obesity on the outcome after total elbow arthroplasty has not been well studied.
The increased utilization of total elbow arthroplasty, especially for acute traumatic and posttraumatic conditions29, and the increasing rate of the obese population1-3,30 necessitate further investigation about the effect of obesity on the outcome of total elbow arthroplasty. The purpose of this study was to determine the influence of obesity on the outcome after primary total elbow arthroplasty.
Materials and Methods
Patient Demographic Characteristics
After institutional review board approval, the institutional joint registry31 was utilized to conduct a review of patients who underwent primary total elbow arthroplasty using a single implant design. A total of 723 primary semiconstrained, linked total elbow arthroplasties using the Coonrad/Morrey Total Elbow (Zimmer, Warsaw, Indiana) were performed in 654 patients from 1987 to 2006. Of those, 550 total elbow arthroplasties (76%) were performed in 494 women and 173 total elbow arthroplasties (24%) were performed in 160 men. The average patient age (and standard deviation) at the time of surgery was 62.3 ± 13.7 years (range, twenty-one to ninety-two years). Three hundred and seventy-eight total elbow arthroplasties (52%) in 317 patients were performed to treat inflammatory conditions. Another 310 total elbow arthroplasties (43%) in 307 patients were performed to treat acute traumatic or posttraumatic conditions, including 139 total elbow arthroplasties (138 patients) to treat bone fracture nonunion, 105 total elbow arthroplasties (104 patients) to treat posttraumatic arthritis, and sixty-six total elbow arthroplasties (sixty-five patients) to treat acute distal humeral fracture. The remaining indications included nineteen total elbow arthroplasties to treat primary osteoarthrosis, six total elbow arthroplasties to treat resection of neoplastic lesion, four total elbow arthroplasties to treat hemophilic arthropathy, three total elbow arthroplasties to treat septic arthropathy, two total elbow arthroplasties to treat Charcot neuropathic arthropathy, and one total elbow arthroplasty to treat crystal deposition arthropathy. Different surgeons performed the procedures, but one of the authors (B.F.M.) performed the majority (546 total elbow arthroplasties [76%]). All except one procedure used cemented prostheses. The average operative time (and standard deviation) was 148 ± 75 minutes. A tourniquet was applied for an average time (and standard deviation) of 88 ± 38 minutes.
At our institution, follow-up is conducted twice during the first year following surgery, after two and five years, and then every five years. Patients return for a routine assessment through clinical examination and radiographs by the treating physician. Patients who are unable to attend in person for a clinic visit are contacted by correspondence and/or telephone interview to complete an elbow evaluation questionnaire and to send radiographs26,31,32. The follow-up compliance is approximately 90% at ten years, 85% at fifteen years, and 80% at twenty years32,33. The duration of follow-up was calculated from the time of elbow replacement surgery until the most recent clinical evaluation with no additional revision surgery or until revision surgery with component exchange or removal. The median duration of follow-up for the study cohort was 5.8 years (range, zero to twenty-five years). Seventy-four patients (seventy-five elbows [10%]) did not reach a minimum of two years of follow-up. Of those, eighteen patients (eighteen elbows) underwent revision and thirty-one patients (thirty-two elbows) had died (thirteen patients during the first year and eighteen patients during the second year following surgery). The remaining twenty-five patients (twenty-five elbows) were completely lost to follow-up.
The BMI (weight in kilograms divided by height in meters squared) was obtained as part of the preoperative assessment. The World Health Organization (WHO) defines obesity as a BMI of ≥30 kg/m2. Furthermore, patients were categorized into moderate obesity (30 to <35 kg/m2), severe obesity (35 to <40 kg/m2), and very severe or morbid obesity (≥40 kg/m2)30. Five hundred and six patients undergoing 564 total elbow arthroplasties (78%) had a BMI of <30 kg/m2 and were categorized as non-obese, whereas 151 patients undergoing 159 total elbow arthroplasties (22%) had a BMI of ≥30 kg/m2 and were categorized as obese. There was a significant difference (p < 0.05) between the average BMI (and standard deviation) for non-obese patients (24.2 ± 3.4 kg/m2) and that for obese patients (35 ± 4.3 kg/m2) (see Appendix). There was also a significant difference (p < 0.05) between the average BMI (and standard deviation) for patients with inflammatory arthropathy (25.4 ± 5.5 kg/m2) and for patients with traumatic conditions (27.9 ± 6 kg/m2).
Patients’ records were retrospectively reviewed. We recorded complications, including bone fractures, extensor mechanism dysfunction, surgical wound complications, neurologic issues, and thromboembolic events, as well as ninety-day perioperative mortality. We also recorded additional operations, including revision arthroplasties with component exchange or removal, regardless of the location of the revision surgery. Revision arthroplasties were performed for deep infection or mechanical failure. Mechanical failure included component aseptic loosening34, periprosthetic bone fracture, component fracture, and/or bushings wear34,35.
Statistical Analysis
Unless otherwise specified, the data are expressed as the mean and the standard deviation for continuous variables and the number (percentage) for discrete variables. The means of BMI in patient cohorts classified on the basis of surgical indications in total elbow arthroplasty (inflammatory arthropathy, traumatic conditions, and others) were compared with use of one-way analysis of variance (ANOVA). Significant differences were analyzed further using the Tukey-Kramer honestly significant difference multiple comparisons procedure. The Kaplan-Meier method was used to estimate survival rates of total elbow arthroplasty with the end points of revision for any reason, revision for mechanical failure, and revision for component aseptic loosening36. An additional Wilcoxon test was used to compare Kaplan-Meier survival curves of total elbow arthroplasty between the non-obese and obese cohorts. Cox proportional-hazards regression models, adjusting for age, sex, and indication, were used to assess the effect of BMI on the risk of total elbow arthroplasty revision for the formerly described end points. All statistical tests were two-sided, and significance was set at p < 0.05.
Source of Funding
One author (Y.M.K.B.) received through his institution a grant (Grant No. UL1 TR000135) from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Funds were used to pay for statistical services. The authors’ institution receives royalties from Zimmer.
Results
Mortality and Complications
Seventy-four patients (seventy-five elbows [10%]) did not have a minimum of two years of follow-up. Of those, five patients (five elbows) died within ninety days following the surgery. Thus, the ninety-day mortality rate after total elbow arthroplasty was 0.76% for patients (five of 654 patients) and 0.69% for procedures (five of 723 procedures) in the study cohort, which was similar to previously reported rates37. The complications among non-obese and obese patients are described in Table I. The perioperative mortality rate and complications were comparable between non-obese and obese patients, except for the extensor mechanism dysfunction and the development of heterotrophic ossification, which was greater in obese patients.
TABLE I.
Complications After Total Elbow Arthroplasty
| Complications | Total Elbow Arthroplasties for Non-Obese Patients* (N = 564) | Total Elbow Arthroplasties for Obese Patients* (N = 159) |
| Surgical wound complications | 87 (15.4%) | 23 (14.5%) |
| Surgical wound complications that required additional operation with no component revision | 38 (6.7%) | 7 (4.4%) |
| Bone fractures | 43 (7.6%) | 12 (7.5%) |
| Humeral bone fracture | 27 (4.8%) | 10 (6.3%) |
| Ulnar bone fracture | 13 (2.3%) | 2 (1.3%) |
| Humeral and ulnar bone fracture | 3 (0.5%) | 0 (0%) |
| Neurologic issues | 25 (4.4%) | 5 (3.1%) |
| Thromboembolic events | 1 (0.2%) | 0 (0%) |
| Ninety-day perioperative mortality | 3 (0.5%) | 2 (1.3%) |
| Extensor mechanism dysfunctions | 16 (2.8%) | 9 (5.7%) |
| Ectopic bone and ossifications | 16 (2.8%) | 16 (10.1%) |
The values are given as the number of total elbow arthroplasties, with the percentage in parentheses.
Revision Surgical Procedures
A total of 118 total elbow arthroplasties (16%) had been revised at the most recent follow-up (Table II). The most common reason for revision was mechanical failure. Of the 118 revision total elbow arthroplasties, ninety-eight (83%) were revised for mechanical failure, including fifty-nine revised for component aseptic loosening. In addition, twenty total elbow arthroplasties (17%) were revised for deep infection. They were performed at a median of 2.3 years (range, 1.2 months to 19.9 years). Of 564 total elbow arthroplasties, eighty-three (15%) were revised in non-obese patients (sixty-seven for mechanical failure and sixteen for deep infection); and of 159 total elbow arthroplasties, thirty-five (22%) were revised in obese patients (thirty-one for mechanical failure and four for deep infection).
TABLE II.
Total Elbow Arthroplasty Failures*
| Failure Description | No. of Failures |
| Mechanical failure with revision surgical procedure | |
| Bushing exchange | 25 |
| Humeral component | |
| Aseptic loosening | 5 |
| Aseptic loosening and periprosthetic fracture | 4 |
| Component fracture | 3 |
| Aseptic loosening, component fracture, and periprosthetic fracture | 1 |
| Aseptic loosening and component fracture | 1 |
| Ulnar component | |
| Aseptic loosening | 20 |
| Aseptic loosening and periprosthetic fracture | 12 |
| Component fracture | 9 |
| Aseptic loosening, component fracture, and periprosthetic fracture | 5 |
| Aseptic loosening and component fracture | 4 |
| Malposition | 1 |
| Humeral and ulnar components | |
| Humeral and ulnar aseptic loosening | 3 |
| Humeral and ulnar aseptic loosening and ulnar periprosthetic fracture | 1 |
| Humeral and ulnar aseptic loosening and humeral periprosthetic fracture | 1 |
| Humeral and ulnar aseptic loosening and periprosthetic fracture | 1 |
| Ulnar aseptic loosening and humeral component fracture | 1 |
| Humeral and ulnar component fracture | 1 |
| Deep infection with revision surgical procedure | |
| Humeral and ulnar components (resection arthroplasty) | 18 |
| Humeral component | 1 |
| Ulnar component | 1 |
| Total no. of revision surgical procedures | 118 |
There were another five total elbow arthroplasties that showed mechanical failure on radiographs, but the patients who underwent these arthroplasties did not undergo revision surgery. With regard to mechanical failures, three elbows had ulnar component aseptic loosening, one elbow had ulnar component fracture, and one elbow had ulnar component aseptic loosening and component fracture.
Eighteen patients (eighteen total elbow arthroplasties) underwent revision within two years following surgery (median, 1.2 years [range, 0 to 1.9 years]). The indications for these revisions were deep infection in nine elbows, humeral component aseptic loosening in two elbows, ulnar component aseptic loosening in two elbows (including one with an additional periprosthetic ulnar bone fracture), ulnar component fracture in three elbows, ulnar component malposition in one elbow, and combined humeral and ulnar components aseptic loosening in one elbow. Additionally, five total elbow arthroplasties (three for non-obese patients and two for obese patients) had mechanical failure confirmed on radiographs, but these patients had not undergone revision surgery at the most recent follow-up.
Survivorship Analyses
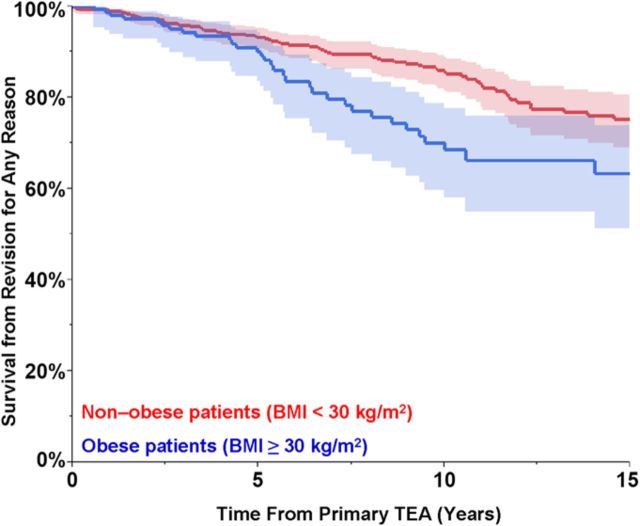
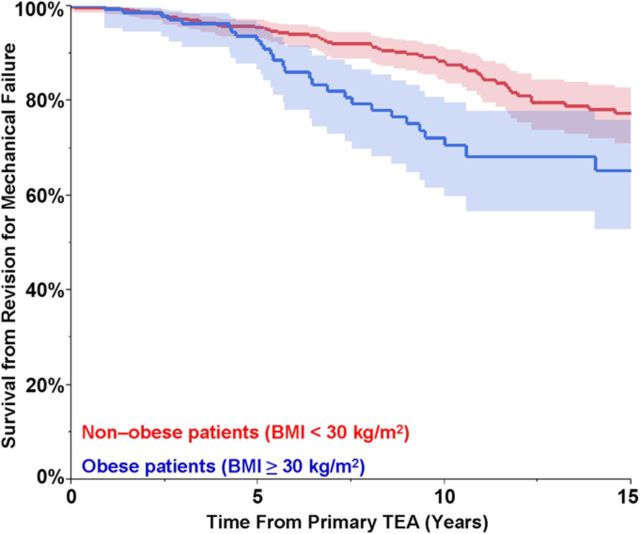
Table III summarizes the overall Kaplan-Meier survival estimates for different revision end points. Obese patients had a significantly lower survival rate (p < 0.05 for all) for total elbow arthroplasty revision for any reason, mechanical failure, or component aseptic loosening as end points compared with non-obese patients. However, the survival rate for total elbow arthroplasty revision for deep infection was comparable for obese and non-obese patients. The total elbow arthroplasty survival from revision for any reason was 86% (95% confidence interval [CI], 82% to 89%) at ten years and 75% (95% CI, 69% to 81%) at fifteen years for non-obese patients compared with 70% (95% CI, 60% to 79%) at ten years and 63% (95% CI, 51% to 74%) at fifteen years for obese patients, which was a significant difference (p < 0.05). Overall, nearly one-third of obese patients compared with one-quarter of non-obese patients underwent revision for different reasons at the fifteen-year follow-up (Fig. 1).
TABLE III.
Estimated Total Elbow Arthroplasty Survivorship for Different Revision End Points Based on BMI
| Revision End Points | Non-Obese Group* (BMI of <30 kg/m2) | Obese Group* (BMI of ≥30 kg/m2) |
| For any reason† | ||
| Survivorship at five years | 93% (91% to 95%) | 90% (83% to 94%) |
| Survivorship at ten years | 86% (82% to 89%) | 70% (60% to 79%) |
| Survivorship at fifteen years | 75% (69% to 81%) | 63% (51% to 74%) |
| For mechanical failure† | ||
| Survivorship at five years | 95% (93% to 97%) | 93% (87% to 96%) |
| Survivorship at ten years | 88% (84% to 91%) | 72% (61% to 81%) |
| Survivorship at fifteen years | 77% (71% to 83%) | 65% (53% to 76%) |
| For component aseptic loosening† | ||
| Survivorship at five years | 96% (94% to 98%) | 93% (87% to 97%) |
| Survivorship at ten years | 92% (89% to 95%) | 81% (70% to 88%) |
| Survivorship at fifteen years | 85% (80% to 90%) | 76% (64% to 85%) |
| For deep infection‡ | ||
| Survivorship at five years | 98% (96% to 99%) | 97% (92% to 99%) |
| Survivorship at ten years | 97% (95% to 98%) | 97% (92% to 99%) |
| Survivorship at fifteen years | 97% (95% to 98%) | 97% (92% to 99%) |
The values are given as the Kaplan-Meier survival estimate, with the 95% CI in parentheses.
These values were significant at p < 0.05.
These values were not significant at p > 0.05.
Kaplan-Meier curves for non-obese and obese patients, showing the survivorship estimates of primary total elbow arthroplasty (TEA) for the end points of revision for any reason (Fig. 1-A) and revision for mechanical failure (Fig. 1-B). The shaded area represents the 95% CI.
Fig. 1-A.
Fig. 1-B.
Similar trends of survival rates for total elbow arthroplasty revision for different end points were shown among total elbow arthroplasties performed for inflammatory or traumatic conditions in non-obese and obese patients at ten and fifteen years (see Appendix). The significant difference (p < 0.05 for all) was maintained between non-obese and obese patients for total elbow arthroplasty performed for inflammatory conditions (Table IV).
TABLE IV.
Estimated Total Elbow Arthroplasty Survivorship for Different Revision End Points Among Non-Obese and Obese Patients Based on Surgical Indication
| Revision End Points | Non-Obese Group* (BMI of <30 kg/m2) | Obese Group* (BMI of ≥30 kg/m2) |
| Inflammatory conditions | ||
| Revision for any reason† | ||
| Survivorship at five years | 98% (96% to 99%) | 93% (81% to 98%) |
| Survivorship at ten years | 94% (89% to 96%) | 78% (60% to 90%) |
| Survivorship at fifteen years | 82% (75% to 88%) | 78% (60% to 90%) |
| Revision for mechanical failure† | ||
| Survivorship at five years | 99% (97% to 100%) | 93% (81% to 98%) |
| Survivorship at ten years | 95% (90% to 97%) | 78% (60% to 90%) |
| Survivorship at fifteen years | 83% (75% to 89%) | 78% (60% to 90%) |
| Traumatic conditions | ||
| Revision for any reason‡ | ||
| Survivorship at five years | 85% (79% to 90%) | 87% (78% to 93%) |
| Survivorship at ten years | 72% (63% to 79%) | 65% (52% to 77%) |
| Survivorship at fifteen years | 61% (50% to 71%) | 54% (39% to 69%) |
| Revision for mechanical failure‡ | ||
| Survivorship at five years | 89% (83% to 93%) | 92% (83% to 96%) |
| Survivorship at ten years | 76% (67% to 83%) | 69% (55% to 80%) |
| Survivorship at fifteen years | 64% (52% to 74%) | 57% (41% to 72%) |
The values are given as the Kaplan-Meier survival estimate, with the 95% CI in parentheses.
These values were significant at p < 0.05.
These values were not significant at p > 0.05.
Cox Proportional-Hazards Regression Models
Table V lists the adjusted hazard ratios for different total elbow arthroplasty revision end points based on the BMI category. Severely obese patients (those with a BMI of 35 to <40 kg/m2) demonstrated a significantly higher risk (p < 0.05) of total elbow arthroplasty revision for any reason (hazard ratio, 3.08 [95% CI, 1.61 to 5.45]) and revision for mechanical failure (hazard ratio, 3.10 [95% CI, 1.47 to 5.89]) compared with non-obese patients.
TABLE V.
Adjusted Hazard Ratios* for Total Elbow Arthroplasty Revision at Different End Points
| BMI Group | Revision for Any Reason† | Revision for Mechanical Failure† |
| Non-obese | 1.00 (reference) | 1.00 (reference) |
| Moderately obese | 1.03 (0.6 to 1.68) | 1.23 (0.7 to 2.06) |
| Severely obese‡ | 3.08 (1.61 to 5.45) | 3.1 (1.47 to 5.89) |
| Morbidly obese | 0.71 (0.17 to 1.9) | 0.88 (0.21 to 2.37) |
The model also included the parameters of age, sex, and surgical indication.
The values are given as the hazard ratio, with the 95% CI in parentheses.
The difference was significant at p < 0.05.
Table VI lists the age, sex, BMI, and indication-adjusted hazard ratios for different total elbow arthroplasty revision end points. The increased risk of total elbow arthroplasty revision for any reason or total elbow arthroplasty revision for mechanical failure was not statistically detectable with each additional unit of BMI. Men had a significantly higher risk (p < 0.05 for both) of total elbow arthroplasty revision for any reason (hazard ratio, 1.79 [95% CI, 1.19 to 2.65]) and revision for mechanical failure (hazard ratio, 1.74 [95% CI, 1.11 to 2.67]) compared with women. Each additional year of age at surgery was significantly associated (p < 0.05 for both) with a 2% decline in the risk of total elbow arthroplasty revision for any reason or for mechanical failure (Table VI). The performance of total elbow arthroplasty for acute traumatic or posttraumatic conditions was significantly lower (p < 0.05) compared with total elbow arthroplasty performed for inflammatory conditions, as shown in Table VI.
TABLE VI.
Age, Sex, BMI, and Indication-Adjusted Hazard Ratios for Total Elbow Arthroplasty Revision at Different End Points
| Variable | Revision for Any Reason* | Revision for Mechanical Failure* |
| Age per year increase† | 0.98 (0.96 to 0.99) | 0.98 (0.97 to 0.99) |
| Men compared with women† | 1.79 (1.19 to 2.65) | 1.74 (1.11 to 2.67) |
| BMI per unit increase | 1.02 (0.99 to 1.05) | 1.03 (0.99 to 1.06) |
| Indications | ||
| Inflammatory conditions | 1.00 (reference) | 1.00 (reference) |
| Traumatic conditions† | 3.48 (2.34 to 5.27) | 3.37 (2.19 to 5.28) |
| Other‡ | 0.95 (0.28 to 2.48) | 0.57 (0.09 to 1.96) |
The values are given as the hazard ratio, with the 95% CI in parentheses.
These values were significant at p < 0.05.
Other includes primary osteoarthrosis, resection of neoplastic lesion, hemophilic arthropathy, history of septic arthropathy, Charcot neuropathic arthropathy, and crystal deposition arthropathy.
Discussion
Obesity has reached epidemic proportions1-3,30. Joint replacement can be challenging in obese patients because of longer operative time, difficult surgical technique, more complications, and possibly a negative effect on implant longevity. The impact of obesity on joint replacement has been extensively analyzed for total hip arthroplasty5-12 and total knee arthroplasty5,11-23. However, the effect of obesity on total elbow arthroplasty is largely unknown.
In this study, obesity adversely affected the longevity of total elbow arthroplasty. Despite the poor implant longevity among obese patients, their rate of perioperative mortality and complications were comparable with those of non-obese patients, although there were higher percentages of extensor mechanism dysfunction and heterotrophic ossification among obese patients.
There is a paucity of published data about the influence of obesity on joint arthroplasty of the upper extremity25-27. Singh et al.26 reported about risk factors of humeral head revision in 1431 shoulders. They concluded that obesity and young age are associated with a higher revision rate. Beck et al.27 also found a higher complication rate of reverse total shoulder arthroplasty in obese patients compared with normal-weight patients at a minimum of a two-year follow-up. They noted that obesity may be associated with a low rate of radiographic scapular notching.
Studies published about the effect of obesity on joint arthroplasty of the lower extremity have provided conflicting evidence. This conflict could be attributed to differences in patient-related, operative-related, or research-related factors, including differences in patient population, patient activity, mechanical loading, operative indication, operative technique, surgeon experience, and implants. Several studies have shown that obesity does not affect the clinical outcomes, complications, and the implant durability of total hip arthroplasty6,10 and total knee arthroplasty18-21,23. However, other studies have shown that obesity adversely influences the clinical outcomes, complications, and prosthesis longevity of total hip arthroplasty8 and total knee arthroplasty13-16. Additionally, a number of authors have also reported that obesity only adversely affects the clinical outcomes with no impact on complications or implant revisions of total hip arthroplasty9,12 and total knee arthroplasty12,17,22 (see Appendix).
This study had several limitations. The experience of a single institution may not be generalizable. Despite a high compliance rate of follow-up at our institution, some patients may have undergone revision surgery at other institutions without being available for our joint registry. Given the nature of the study design, the analysis was not adjusted for other potential parameters. Also, some parameters affecting the outcome may not have been detected during the analysis because of inadequate power and inadequate or biased sampling, leading to a type-II error. We performed a retrospective record review, multiple surgeons were involved, and patients were not matched with a control cohort. We did not report patient outcomes for satisfaction and function. Because patient function and activity level were not collected, we did not correlate them with the study findings. However, Barlow and colleagues38 reported that higher-demand activities following total elbow arthroplasty are associated with male patients and a preoperative diagnosis of fracture or nonunion. The strengths of the current study included the use of a single implant design, the large number of elbows included, and the intermediate to long-term follow-up.
To our knowledge, this is the only study to date that shows that primary total elbow arthroplasty carries a substantially higher risk of failure in obese patients compared with non-obese patients. Patients with a high BMI being considered for elbow replacement surgery should be counseled accordingly.
Appendix
Figures showing the Kaplan-Meier curves for non-obese and obese patients for the survivorship estimates of primary total elbow arthroplasty for various end points and tables showing patient demographic characteristics and studies published about the effect of obesity on shoulder, hip, and knee arthroplasties are available with the online version of this article as a data supplement at jbjs.org.
Acknowledgments
Note: We thank Ross A. Dierkhising, MS, for support in the statistical analyses conducted in this study and Youlonda Loechler, BS, for providing the study cohort.
Investigation performed at the Department of Orthopedic Surgery, Mayo Clinic, Rochester, Minnesota
Disclaimer: The contents of the article are solely the responsibility of the authors and do not necessarily represent the official view of the National Institutes of Health.
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Finucane MM Stevens GA Cowan MJ Danaei G Lin JK Paciorek CJ Singh GM Gutierrez HR Lu Y Bahalim AN Farzadfar F Riley LM Ezzati M; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index). National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011 Feb 12;377(9765):557-67. Epub 2011 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL Carroll MD Curtin LR McDowell MA Tabak CJ Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006 Apr 5;295(13):1549-55. [DOI] [PubMed] [Google Scholar]
- 3.Wang Y Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6-28. Epub 2007 May 17. [DOI] [PubMed] [Google Scholar]
- 4.Pottie P Presle N Terlain B Netter P Mainard D Berenbaum F. Obesity and osteoarthritis: more complex than predicted! Ann Rheum Dis. 2006 Nov;65(11):1403-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Workgroup of the American Association of Hip and Knee Surgeons Evidence Based Committee. Obesity and total joint arthroplasty: a literature based review. J Arthroplasty. 2013 May;28(5):714-21. Epub 2013 Mar 19. [DOI] [PubMed] [Google Scholar]
- 6.Andrew JG Palan J Kurup HV Gibson P Murray DW Beard DJ. Obesity in total hip replacement. J Bone Joint Surg Br. 2008 Apr;90(4):424-9. [DOI] [PubMed] [Google Scholar]
- 7.Horan F. Obesity and joint replacement. J Bone Joint Surg Br. 2006 Oct;88(10):1269-71. [DOI] [PubMed] [Google Scholar]
- 8.Chee YH Teoh KH Sabnis BM Ballantyne JA Brenkel IJ. Total hip replacement in morbidly obese patients with osteoarthritis: results of a prospectively matched study. J Bone Joint Surg Br. 2010 Aug;92(8):1066-71. [DOI] [PubMed] [Google Scholar]
- 9.Jackson MP Sexton SA Yeung E Walter WL Walter WK Zicat BA. The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J Bone Joint Surg Br. 2009 Oct;91(10):1296-300. [DOI] [PubMed] [Google Scholar]
- 10.McLaughlin JR Lee KR. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Joint Surg Br. 2006 Oct;88(10):1286-92. [DOI] [PubMed] [Google Scholar]
- 11.Wendelboe AM Hegmann KT Biggs JJ Cox CM Portmann AJ Gildea JH Gren LH Lyon JL. Relationships between body mass indices and surgical replacements of knee and hip joints. Am J Prev Med. 2003 Nov;25(4):290-5. [DOI] [PubMed] [Google Scholar]
- 12.Yeung E Jackson M Sexton S Walter W Zicat B Walter W. The effect of obesity on the outcome of hip and knee arthroplasty. Int Orthop. 2011 Jun;35(6):929-34. Epub 2010 May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foran JR Mont MA Rajadhyaksha AD Jones LC Etienne G Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004 Oct;19(7):817-24. [DOI] [PubMed] [Google Scholar]
- 14.Kerkhoffs GM Servien E Dunn W Dahm D Bramer JA Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am. 2012 Oct 17;94(20):1839-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foran JR Mont MA Etienne G Jones LC Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am. 2004 Aug;86(8):1609-15. [DOI] [PubMed] [Google Scholar]
- 16.Amin AK Clayton RA Patton JT Gaston M Cook RE Brenkel IJ. Total knee replacement in morbidly obese patients. Results of a prospective, matched study. J Bone Joint Surg Br. 2006 Oct;88(10):1321-6. [DOI] [PubMed] [Google Scholar]
- 17.Jackson MP Sexton SA Walter WL Walter WK Zicat BA. The impact of obesity on the mid-term outcome of cementless total knee replacement. J Bone Joint Surg Br. 2009 Aug;91(8):1044-8. [DOI] [PubMed] [Google Scholar]
- 18.Spicer DD Pomeroy DL Badenhausen WE Schaper LA Jr Curry JI Suthers KE Smith MW. Body mass index as a predictor of outcome in total knee replacement. Int Orthop. 2001;25(4):246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mont MA Mathur SK Krackow KA Loewy JW Hungerford DS. Cementless total knee arthroplasty in obese patients. A comparison with a matched control group. J Arthroplasty. 1996 Feb;11(2):153-6. [DOI] [PubMed] [Google Scholar]
- 20.Amin AK Patton JT Cook RE Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg Br. 2006 Mar;88(3):335-40. [DOI] [PubMed] [Google Scholar]
- 21.Stevens-Lapsley JE Petterson SC Mizner RL Snyder-Mackler L. Impact of body mass index on functional performance after total knee arthroplasty. J Arthroplasty. 2010 Oct;25(7):1104-9. Epub 2009 Oct 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins RA Walmsley PJ Amin AK Brenkel IJ Clayton RA. Does obesity influence clinical outcome at nine years following total knee replacement? J Bone Joint Surg Br. 2012 Oct;94(10):1351-5. [DOI] [PubMed] [Google Scholar]
- 23.Singh JA Gabriel SE Lewallen DG. Higher body mass index is not associated with worse pain outcomes after primary or revision total knee arthroplasty. J Arthroplasty. 2011 Apr;26(3):366-374.e1. Epub 2010 Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker JF Perera A Lui DF Stephens MM. The effect of body mass index on outcomes after total ankle replacement. Ir Med J. 2009 Jun;102(6):188-90. [PubMed] [Google Scholar]
- 25.Linberg CJ Sperling JW Schleck CD Cofield RH. Shoulder arthroplasty in morbidly obese patients. J Shoulder Elbow Surg. 2009 Nov-Dec;18(6):903-6. Epub 2009 May 22. [DOI] [PubMed] [Google Scholar]
- 26.Singh JA Sperling JW Cofield RH. Risk factors for revision surgery after humeral head replacement: 1,431 shoulders over 3 decades. J Shoulder Elbow Surg. 2012 Aug;21(8):1039-44. Epub 2011 Oct 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beck JD Irgit KS Andreychik CM Maloney PJ Tang X Harter GD. Reverse total shoulder arthroplasty in obese patients. J Hand Surg Am. 2013 May;38(5):965-70. Epub 2013 Apr 6. [DOI] [PubMed] [Google Scholar]
- 28.Coombes R. Rationing of joint replacements raises fears of further cuts. BMJ. 2005 Dec 3;331(7528):1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gay DM Lyman S Do H Hotchkiss RN Marx RG Daluiski A. Indications and reoperation rates for total elbow arthroplasty: an analysis of trends in New York State. J Bone Joint Surg Am. 2012 Jan 18;94(2):110-7. [DOI] [PubMed] [Google Scholar]
- 30.[No author listed]. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1-253. [PubMed]
- 31.Berry DJ Kessler M Morrey BF. Maintaining a hip registry for 25 years. Mayo Clinic experience. Clin Orthop Relat Res. 1997 Nov;(344):61-8. [DOI] [PubMed] [Google Scholar]
- 32.Berry DJ von Knoch M Schleck CD Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005 Nov;87(11):2456-63. [DOI] [PubMed] [Google Scholar]
- 33.Kremers HM Howard JL Loechler Y Schleck CD Harmsen WS Berry DJ Cabanela ME Hanssen AD Pagnano MW Trousdale RT Lewallen DG. Comparative long-term survivorship of uncemented acetabular components in revision total hip arthroplasty. J Bone Joint Surg Am. 2012 Jun 20;94(12):e82. [DOI] [PubMed] [Google Scholar]
- 34.Ramsey ML Adams RA Morrey BF. Instability of the elbow treated with semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 1999 Jan;81(1):38-47. [DOI] [PubMed] [Google Scholar]
- 35.Lee BP Adams RA Morrey BF. Polyethylene wear after total elbow arthroplasty. J Bone Joint Surg Am. 2005 May;87(5):1080-7. [DOI] [PubMed] [Google Scholar]
- 36.Kaplan EL Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457-81. [Google Scholar]
- 37.Sanchez-Sotelo J Sperling JW Morrey BF. Ninety-day mortality after total elbow arthroplasty. J Bone Joint Surg Am. 2007 Jul;89(7):1449-51. [DOI] [PubMed] [Google Scholar]
- 38.Barlow JD Morrey BF O’Driscoll SW Steinmann SP Sanchez-Sotelo J. Activities after total elbow arthroplasty. J Shoulder Elbow Surg. 2013 Jun;22(6):787-91. Epub 2013 Mar 13. [DOI] [PubMed] [Google Scholar]